Infectious disease lecture 9-10
Fever‘Fever’ implies an elevated core body temperature > 38.0 °C, i.e. above the normal daily variation.
Fever is a response to cytokines and acute phase proteins and is a common manifestation of infection, although it also occurs in other conditions.
• Documentation of fever. ‘Feeling hot’ or sweaty is not synonymous with
fever. Body temperature must be documented: > 38.0 °C is a fever.
Axillary and aural measurement is less accurate than oral or rectal.
• Rigors. Shivering (followed by excessive sweating) implies a rapid
rise in body temperature but rarely gives a clue to aetiology.
• Night sweats. These are characteristic of several infections (e.g. tuberculosis (TB), infective endocarditis), but sweating from any cause is worse at night.
• Excessive sweating. Alcohol, anxiety, thyrotoxicosis, diabetes mellitus, acromegaly, lymphoma and excessive environmental heat all cause sweating without temperature elevation.
• Recurrent fever. There are various causes of recurrent fever, e.g. Borrelia recurrentis, bacterial abscess.
• Accompanying features
Headache. Severe headache and photophobia, although characteristic of meningitis, may accompany other infections.
Delirium. Mental confusion during fever is more common in young children or the elderly.
Muscle pain. Myalgia may occur with viral infections, such as influenza, and with septicaemia including meningococcal sepsis.
Shock. Shock may accompany severe infections and sepsis.
Pyrexia of unknown origin (PUO)
PUO is defined as a temperature persistently above 38.0 °C for more than 3 weeks, without diagnosis despite initial investigation during 3 days of inpatient care or after more than two outpatient visits. Subsets of PUO
are described by medical setting: HIV-related, immunedeficient or nosocomial. Up to one-third of cases of PUO
Sepsis
describes patients with signs of the systemic inflammatory response syndrome (SIRS: two of temperature > 38 °C or < 36 °C, pulse rate > 90 beats per minute, respiratory rate > 20 per minute or PCO2 < 4.3 kPa (32.5 mmHg), and white blood cell count > 12 or < 4 × 109/L) and evidence of infection.
Septic shock describes sepsis plus hypotension (systolic blood pressure
< 90 mmHg systolic or a fall of > 40 mmHg from baseline that is not responsive to fluid challenge or due to another cause). It may be complicated by multi-organ failure and requires intensive care unit admission.
History-taking in suspected infectious disease (ID)
Presenting complaint
• Diverse manifestations of ID make accurate assessment of features and duration critical; e.g. fever and cough lasting for 2 days imply an acute respiratory tract infection and for 2 months suggest TB
Review of systems
• Must be comprehensive
Past medical history
• Define the ‘host’ and likelihood of infection(s)
• Include surgical and dental procedures involving prosthetic materials
• Document previous infections
Medication history
• Include non-prescription drugs, use of antimicrobials and immunosuppressive drugs
Allergy history
• Especially to antimicrobials, noting the allergic manifestation (e.g. rash versus anaphylaxis)
Family and contact history
• Note infections and their time course
• Sensitively explore exposure to key infections, e.g. TB and human
immunodeficiency virus (HIV)-1
Travel history
• Include countries visited and where previously resident (relevant to exposure and likely vaccination)
Occupation
• e.g. Anthrax in leather tannery workers
Animal exposures
• Include pets, e.g. dog exposure and hydatid disease
Dietary history
• Consider undercooked meats, shellfish, unpasteurised dairy products or well water
• Establish who else was exposed, e.g. to potential food-borne diarrhoea
History of intravenous drug injection or receipt of blood products
• Risks for blood-borne viruses, such as HIV-1 and hepatitis B and C viruses (HBV and HCV)
Vaccination history and use of prophylactic medicines
• Consider occupation- or age-related vaccines
• In a traveller or infection-predisposed patient, establish compliance with
prophylactic treatments
Skin lesions in infectious diseases
• Diffuse erythema, e.g. Streptococcal toxicm shock syndrome
• Migrating erythema, e.g. enlarging rash of erythema migrans in Lyme disease
• Purpuric or petechial rashes, e.g. Meningoccal sepsis
• Macular or papular rashes, e.g. primary infection with HIV
• Vesicular or blistering rash, e.g. Shingles
• Nodules or plaques, e.g. Kaposi’s sarcoma
• Erythema nodosum e.g. mycoplasma pneumonia
Morphological description of skin lesions
Atrophy Thinning of the skin
Papule Small palpable, circumscribed lesion (<0.5 cm)
Nodule Large papule (>0.5 cm)
Macule Flat, circumscribed non-palpable lesion
Plaque Large flat-topped, elevated, palpable lesion
Vesicle A small fluid-filled blister
Bulla A large fluid-filled blister
Petechia* Pinpoint-sized macule of blood in the skin
Purpura Larger macule or papule of blood in the skin which does not
blanch on pressure
Ecchymosis Large confluent area of purpura (‘bruise’)
Erosion Denuded area of skin (partial epidermal loss)
Crusted Dried serum or exudate on the skin
Pustule Yellowish white pus-filled lesion
Excoriation Scratch mark
Scaly Visible flaking and shedding of surface skin
Fissure Deep linear crack or crevice (often in thickened skin)
Telangiectasia Abnormal visible dilatation of blood vessels
Lichenified Thickened epidermis with prominent normal skin markings
Ulcer Deeper denuded area of skin (full epidermal and dermal loss)
Weal Itchy raised ‘nettle rash’-like swelling due to dermal oedema
Presenting Problems in
Musculoskeletal Disease Important MSK symptoms
Pain
• Usage pain: worse on use, relieved by rest (mechanical strain, damage)
• Rest pain: worse after rest, improved by movement (inflammation)
• Night or ‘bone’ pain: mostly at night, poorly related to movement (bone origin)
Stiffness
• Subjective feeling of inability to move freely
• Duration and severity of early morning and inactivity stiffness that can be ‘worn off’ suggest degree of inflammation
Weakness
• Consider primary or secondary muscle abnormality
Swelling
• Fluid
• Soft tissue
• Bone
Deformity
• Joint
• Bone
Non-specific symptoms of systemic illness
• Weight loss ± reduction in appetite
• Fatigability, poor concentration
• Sweats and chills, particularly at night
• Feeling ill, low, irritable
Arthralgia Pain in a joint without sign of inflammation.
Myalgia pain in the muscle
Arthritis is inflammation of the joint(swelling, redness, hotness and tender)
Monoarthritis is inflammation of single joint.
May be the presentation of what subsequently evolves into
oligo- or polyarthritis.
Oligoarthritis affects 2–4 joints or joint groups (the wrist has many joints but counts as a single site). By far the most common cause is Osteoarthritis , which causes non-inflammatory symptoms that usually affect just one or a few sites at any one time, even though asymptomatic multiple joint Osteoarthritis may be apparent on examination.
Polyarthritis is defined as the involvement of five or more joints or joint groups. Features helpful in determining the cause are:
• symmetry
• involvement of the upper and/or lower limbs
• involvement of large and/or small joints
• periarticular involvement
• extra-articular features .
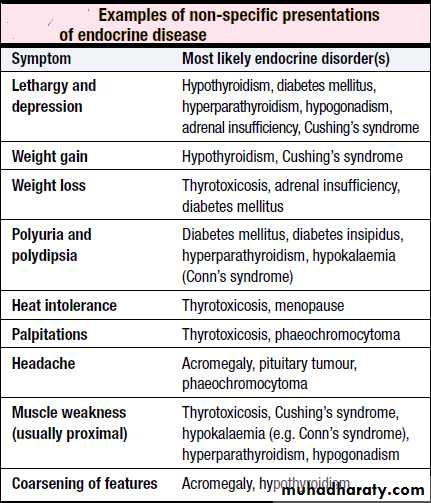
Endocrine disease
INTRODUCTION
The endocrine system consists of glands that exert their actions at distant parts of the body via the production of biologically active hormones secreted into the bloodstream.
Unlike the neurological system, which produces an immediate response, the endocrine system typically has a slower and longer lasting effect on the body.
A full general examination is essential to endocrine assessment because endocrine disorders affect all organ systems. Weight, height, body mass index (BMI), blood pressure and general habitus should all be documented, together with presence or absence of specific signs of deficiency or excess of individual hormone axes (signs of hyper- or hypothyroidism, acromegaly, Cushing’s).
In people with suspected pituitary disease, visual fields and adjacent cranial nerves should be assessed clinically. In thyroid disease, presence of goitre or thyroid eye disease