Endocrinology Dr Yasameen
Alsaffar
Lec 1
Introduction
Endocrinology concerns the synthesis, secretion and action of
hormones. These are chemical messengers released from endocrine
glands that coordinate the activities of many different cells.
Endocrine diseases can therefore affect multiple organs and systems.
Some endocrine disorders are common, particularly those of the
thyroid, parathyroid glands, reproductive system and β cells of the
pancreas.
Functional anatomy and physiology
Some endocrine glands, such as the parathyroids and pancreas,
respond directly to metabolic signals, but most are controlled by
hormones released from the pituitary gland. Anterior pituitary
hormone secretion is controlled in turn by substances produced in
the hypothalamus and released into portal blood, which drains
directly down the pituitary stalk. Posterior pituitary hormones are
synthesised in the hypothalamus and transported down nerve axons,
to be released from the posterior pituitary. Hormone release in the
hypothalamus and pituitary is regulated by numerous stimuli and
through feedback control by hormones produced by the target
glands (thyroid, adrenal cortex and gonads). These integrated
endocrine systems are called ‘axes’.
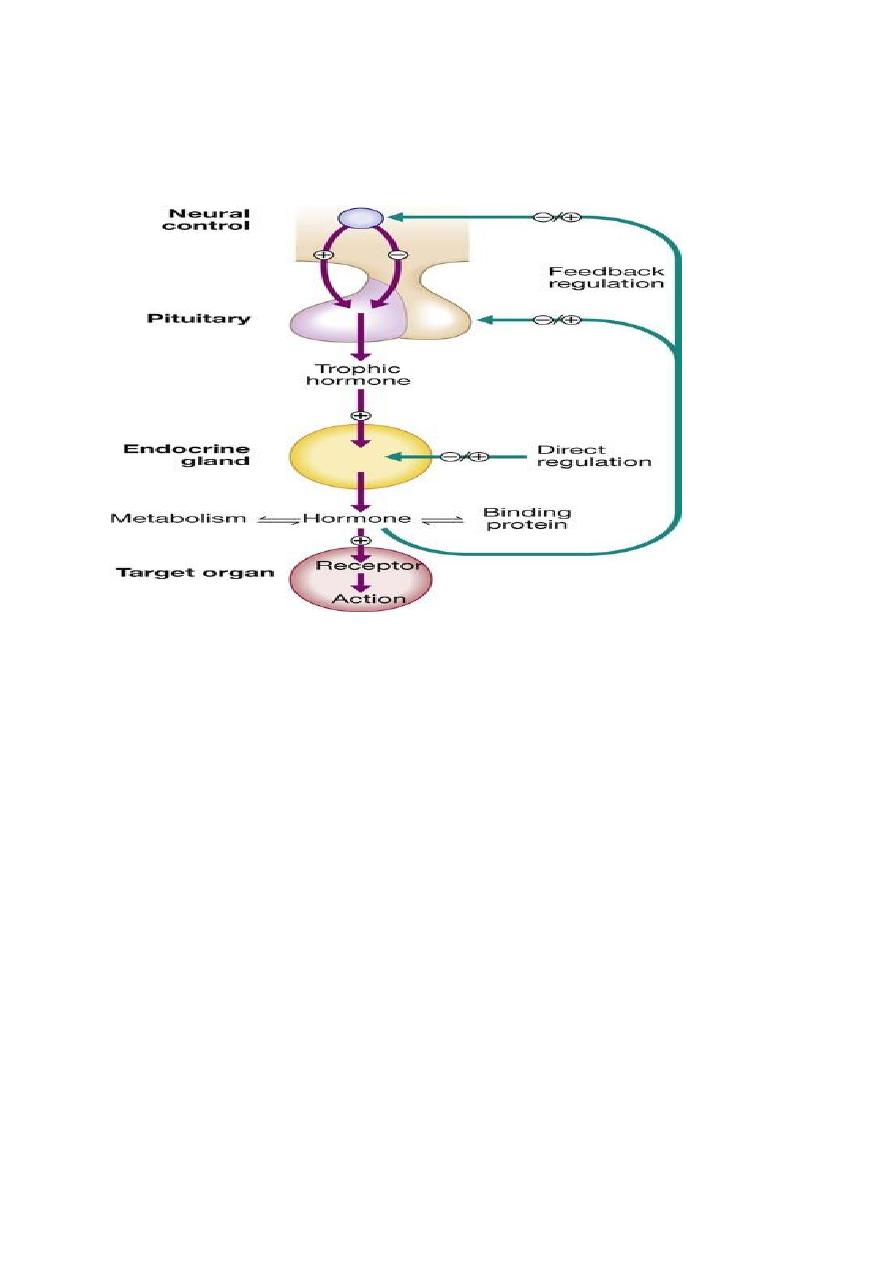
A wide variety of molecules can act as hormones, including peptides
such as insulin and growth hormone, glycoproteins such as thyroid-
stimulating hormone, and amines such as noradrenaline
(norepinephrine). The biological effects of hormones are mediated
by binding to receptors. Many receptors are located on the cell
surface.
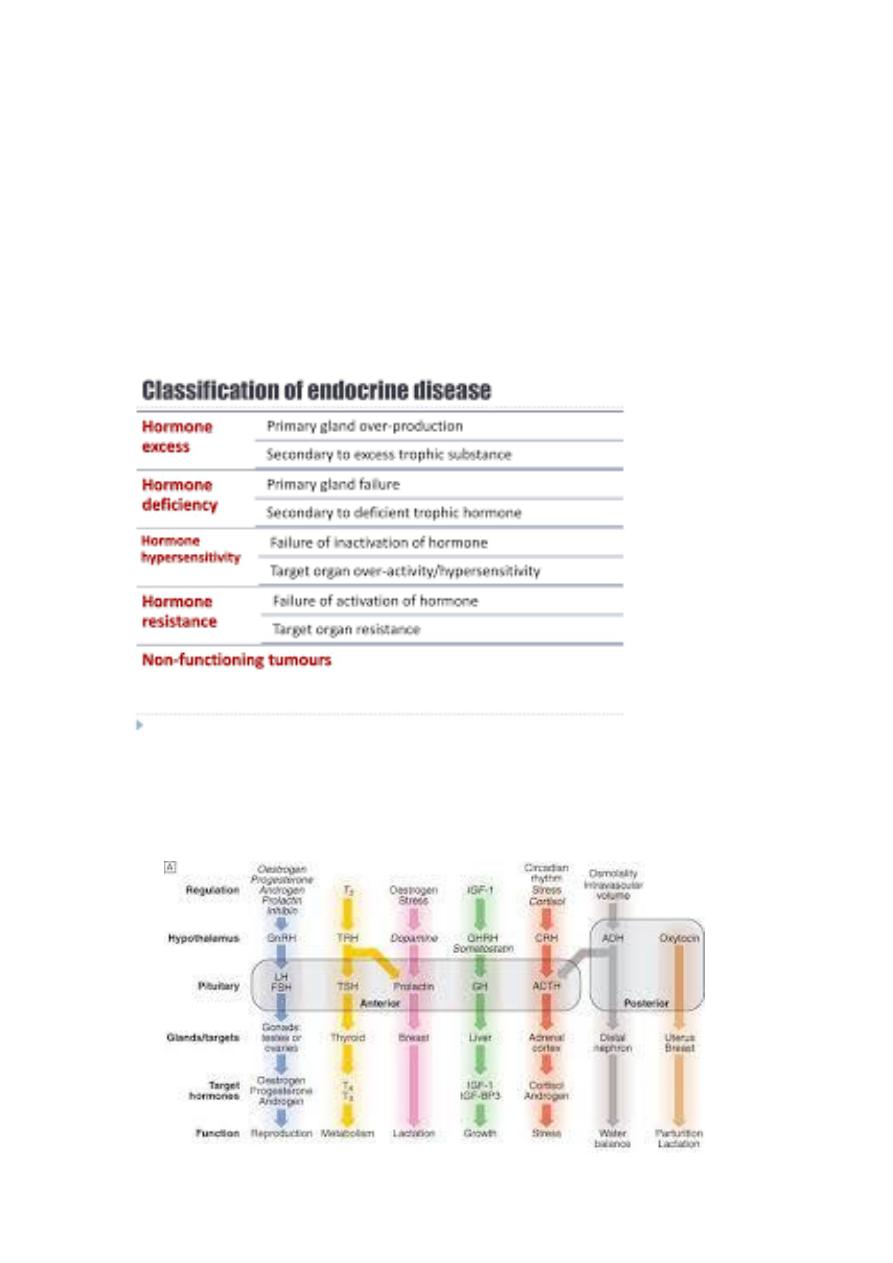
Endocrine pathology
For each endocrine axis or major gland, diseases can be classified as
Pathology arising within the gland is often called ‘primary’ disease
(e.g. primary hypothyroidism in Hashimoto’s thyroiditis), while
abnormal stimulation of the gland is often called ‘secondary’ disease
(e.g. secondary hypothyroidism in patients with a pituitary tumour
and thyroid-stimulating hormone
deficiency). Some pathological
processes can affect multiple endocrine glands these may have a
genetic basis (such as organ-specific autoimmune endocrine
disorders and the multiple endocrine neoplasia (MEN) syndromes) or
be a consequence of therapy for another disease (e.g. following
treatment of childhood cancer with chemotherapy and/or
radiotherapy).
Classification

The principal endocrine ‘axes’. Some major endocrine glands are not controlled by the
pituitary. These include the parathyroid glands (regulated by calcium concentrations, p.
661), the adrenal zona glomerulosa (regulated by the renin–angiotensin system, p. 665) and
the endocrine pancreas. Italics show negative regulation. (ACTH = adrenocorticotrophic
hormone; CRH = corticotrophin-releasing hormone; FSH = folliclestimulating hormone; GH =
growth hormone; GHRH = growth hormone-releasing hormone; GnRH = gonadotrophin-
releasing hormone; IGF-1 = insulin-like growth factor-1; IGF-BP3 = IGF-binding protein-3; LH
= luteinising hormone: T3 = triiodothyronine; T4 = thyroxine; TRH = thyrotrophin-releasing
hormone; TSH = thyroid-stimulating hormone; vasopressin = antidiuretic hormone (ADH))
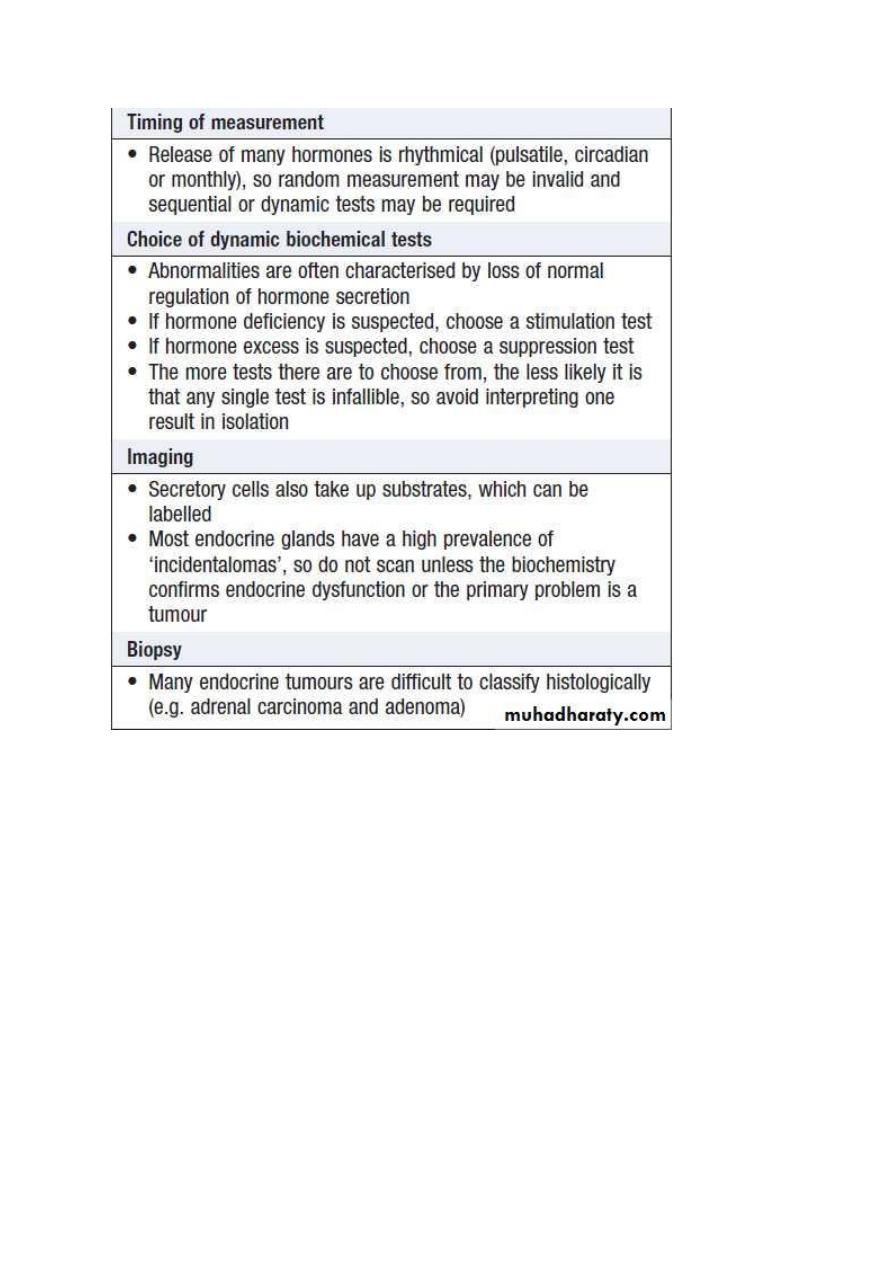
Investigation of endocrine disease
Biochemical investigations play a central role in endocrinology. Most
hormones can be measured in blood but the circumstances in which
the sample is taken are often crucial, especially for hormones with
pulsatile secretion, such as growth hormone; those that show diurnal
variation, such as cortisol; or those that demonstrate monthly
variation, such as oestrogen or progesterone. Some hormones are
labile and need special collection, handling and processing
requirements, e.g. collection in a special tube and/or rapid
transportation to the laboratory on ice. Local protocols for hormone
measurement should be carefully followed. Other investigations,
such as imaging and biopsy, are more frequently reserved for
patients who present with a tumour.
Examples of non-specific presentations of endocrine disease
Symptom
Most likely endocrine disorder(s)
1. Lethargy and depression Hypothyroidism, diabetes mellitus,
hyperparathyroidism, hypogonadism, adrenal insufficiency and
Cushing’s syndrome.
2. Weight gain Hypothyroidism, Cushing’s syndrome

3. Weight loss Thyrotoxicosis, adrenal insufficiency, diabetes
mellitus.
4. Polyuria and polydipsia Diabetes mellitus, diabetes insipidus,
hyperparathyroidism, hypokalaemia (Conn’s syndrome)
5. Heat intolerance Thyrotoxicosis, menopause
6. Palpitation Thyrotoxicosis, phaeochromocytoma
7. Headache Acromegaly, pituitary tumour, phaeochromocytoma
Muscle weakness (usually proximal) Thyrotoxicosis, Cushing’s
syndrome, hypokalaemia (e.g. Conn’s syndrome),
hyperparathyroidism, hypogonadism
8. Coarsening of features Acromegaly, hypothyroidism
Thank you
