1
Therapeutic drug monitoring (TDM)
Therapeutic drug monitoring (TDM): is the measurement of the serum level of the
drug and the coordination of this serum level with the therapeutic range.
Criteria for therapeutic drug monitoring (TDM):
There are a number of criteria which should be fulfilled before TDM is
considered:
1- The drug has narrow therapeutic index ( therapeutic range) the quantity
required to be effective is not far removed from the quantity that causes
significant side effects and/or signs of toxicity or, where therapeutic drug
levels do not differ greatly from levels associated with serious toxicity .
2- Good concentration response relationship.
3- Significant consequences from toxicity.
4- There is a large variability in pharmacokinetic parameters values among
patients.
5- Ready available assay method.
6- Patient have impaired clearance of drug with narrow therapeutic range are
candidate for drug monitoring.
7- Drugs whose toxicity is difficult to distinguish from a patients underlying
disease may require monitoring.
8- Desired therapeutic effect difficult.
In the absence of these criteria, the only indication for TDM is to monitor
compliance or to confirm toxicity.
Drug commonly monitored in hospitals:
1- Antibiotics : aminoglycosides , vancomycin
2- Cardiovascular agents: digoxin, lidocaine, procainamide and N-Acetyl
procainamide, quinidine.
3- Anticonvulsants: phenytoin, carbamazepine, valproic acid, phenobarbital,
primidone, ethosuximide.
4- Immunosuppressants: cyclosporine, tacrolimus.
5- Other drugs: lithium, theophylline.
2
Source of errors in TDM:
Common potential sources of error (in decreasing order of like hood) are:
1- Administration times not recorded accurately.
2- Dose administration error.
3- Blood drawn at incorrect time.
4- Blood drawn before steady-state.
5- Blood drawing from wrong site.
6- Lab assay error.
7- Pharmacy dispending error.
There are two major sources of variability between individual patients in drug
response. These are variation in the relationship between:
- Dose and plasma concentration (pharmacokinetic variability)
- Drug concentration at the receptor and the response (pharmacodynamics
variability).
By adjusting doses to maintain plasma drug concentration within a target range,
variability in the pharmacokinetic phase of drug action is greatly reduced.
The major sources of pharmacokinetic variability are shown in Table below:
Table 1
The major sources of pharmacokinetic variability
Compliance
Age : neonates, children, elderly
Physiology: gender, pregnancy
Disease : hepatic, renal, cardiovascular, respiratory
Drug interactions
Environmental influences on drug metabolism
Genetic polymorphisms of drug metabolism
3
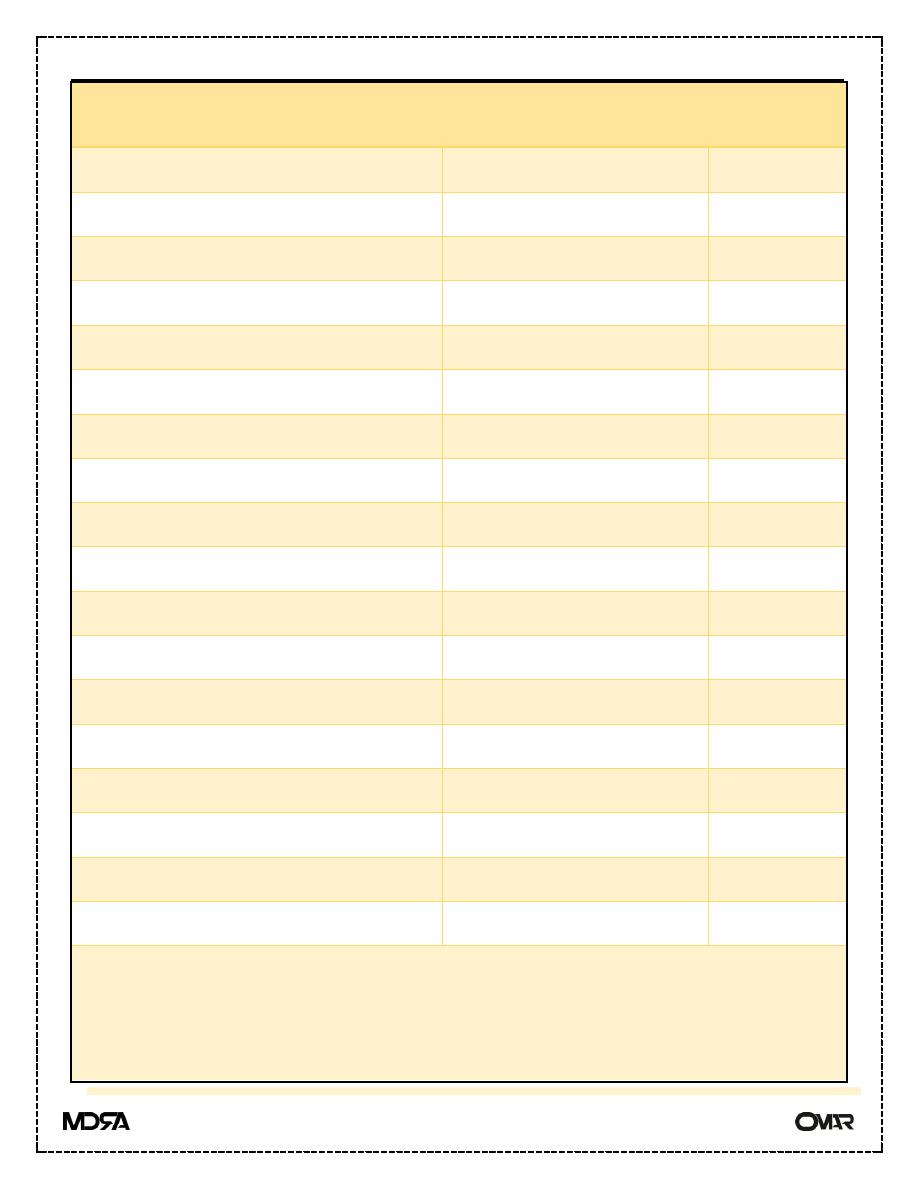
Table2
Drugs commonly monitored
Drug
Therapeutic range mg/L Toxic
Digoxin
0.5-1.5
4
<2.4
4
Amiodarone
1.0-2.5
Lignocaine
1.5-5
1
<5.0
1
Quinidine
2.0-6.0
1
<10
1
Flecainide
0.2-0.9
Mexilitine
0.5-2.5
Salicylate
150-300
Perhexiline
0.15-0.6
Theophylline
10-20
<20
Phenytoin
10.20
1
<20
1
Carbamazepine
4.0-12
1
<12
1
Sodium valproate
50-100
<100
1
Phenobarbitone
15-40
Gentamicin, tobramycin, netilmicin Trough >2
2
; peak< 5
<12
Amikacin
Trough >5
2
peak< 15
<25
Vancomycin
Trough >10; peak< 20-40
lithium
0.6-1.5
3
<2.0
1
(1)
Microgram/L
(2)
For 8-hourly dosing
(3)
mmol/L
(4)
nanogram/ml
