Blood vesselspathology
Lecturer Dr. ZAHRAA MARWANLEC. 1
Mechanisms Of Diseases Due ToVascular Pathology:
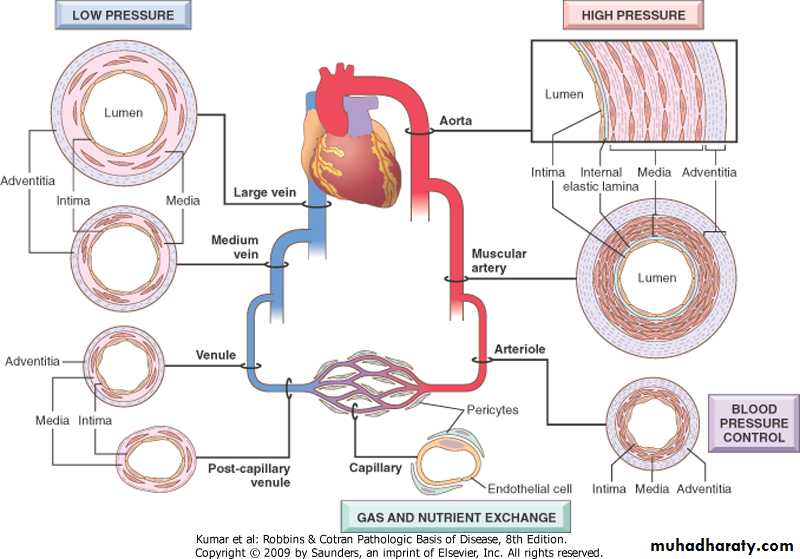
Vascular disease develops through two principal mechanisms:Narrowing or complete obstruction of the lumen
Weakening of the vessels wall leading to dilation or ruptureConstituents Of The blood vessels Wall
Endothelial cellsSmooth muscle cells
Extracellular matrix, (elastin, collagen, glycosoaminoglycans)
these constituents form 3 layers:
-Intima
-Media
-Adventitia
Vessels
Arteries
Veins
Lymphatics
Types Of Arteries Based On Their Size And Structure
• Large or elastic arteries• Medium-sized or muscular arteries
• Small arteries (less than 2mm in diameter)
• Arterioles
Functions
Elastic arteries: recoil of the wall during diastole, propel blood through the peripheral vascular system. (e.g., aorta, arch vessels, iliac and pulmonary arteries).Muscular arteries and arterioles: regulate regional blood flow and blood pressure by changes in lumen size, controlled by:
• - Autonomic nervous system
• - Local metabolic factors and cellular
• interactions
• Capillaries: serve exchange of diffusible substances between blood and tissue
The venous system: collectively, has a large capacity, approximately 2/3 of all blood is in veins.
Lymphatics: serve as drainage system for returning interstitial tissue fluid and inflammatory cells to the blood
Regional specializations of the vasculature
Congenital Anomalies
.Mostly are important in surgery during which an unexpected vessel can be injured..The anomalies are rarely symptomatic except in the coronary tree.
Arterio-Venous Fistulae
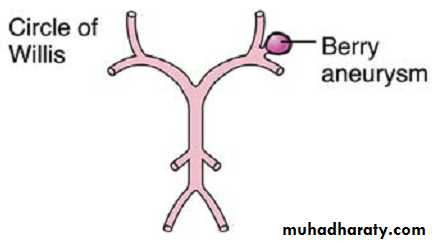
Abnormal communications between arteries and veins *Causes: -Developmental defects -Produced from 1. Rupture of an arterial aneurysm into adjacent vein 2. Penetrating injuries 3. Inflammatory necrosis of adjacent vessels*Clinical significance: -may short circuit blood -may ruptureBerry Aneurysms
• Saccular congenital of unknown etiology• Cigarette smoking and hypertension are predisposing factors
• Most frequent at the 5th decade
• Slightly more common in females
• They occur where the arterial media is
• congenitally attenuated
•
Berry Aneurysms
Clinical features:.Rupture> subarachnoid hemorrhage,Probability of rupture depends on:
-size of the lesion
-acute increase in intracranial pressure
acute feature -generalized vasospasm of non- involved blood vessels>ischemia
late squeal -meningeal fibrosis
Arteriosclerosis
Means: hardening of the arteries, it is a generic term reflecting arterial wall thickening and loss of elasticity.1 - Atherosclerosis.
2 - Monckeberg medial calcific sclerosis.
3 - Arteiolosclerosis:Hyaline
Hyperplastic
Atherosclerosis
Atherosclerosis is characterized by intimal lesions called atheromas (or atheromatous or atherosclerotic plaques) that affect the vascular lumen and can rupture to cause sudden occlusion.The most common arteries involved in descending order: -Aorta -Coronary -Popliteal -Internal carotid -Vessels of circle of willis
Risk factors including: age, gender( male), obesity smoking, DM, lack of exercise, hypertension, hyperlipidemia, type A personality (impatient, workaholic)
Risk factors
• I- Major factors• - Non modifiable
• (Constitutional)
• (age, gender, genetic)
• - Modifiable
• - Hyperlipidemia
• - Hypertension
• - Smoking
• - Diabetes mellitus
• - Inflammation
• II- Other minor factors .lack of exercise .stressful life .obesity .hyperhomocystinemia .lipoprotein a
Hyperlipidemia
Specifically hypercholesterolemia; even in the absence of other risk factors, it is sufficient to initiate lesion development.The major component of serum cholesterol associated with increased risk is low-density lipoprotein (LDL) cholesterol (“bad cholesterol”).
In contrast, high-density lipoprotein (HDL) is the complex that mobilizes cholesterol from the periphery (including atheromas) and transports it to the liver for excretion. Consequently, higher levels of HDL (“good cholesterol”) correlate with reduced risk.
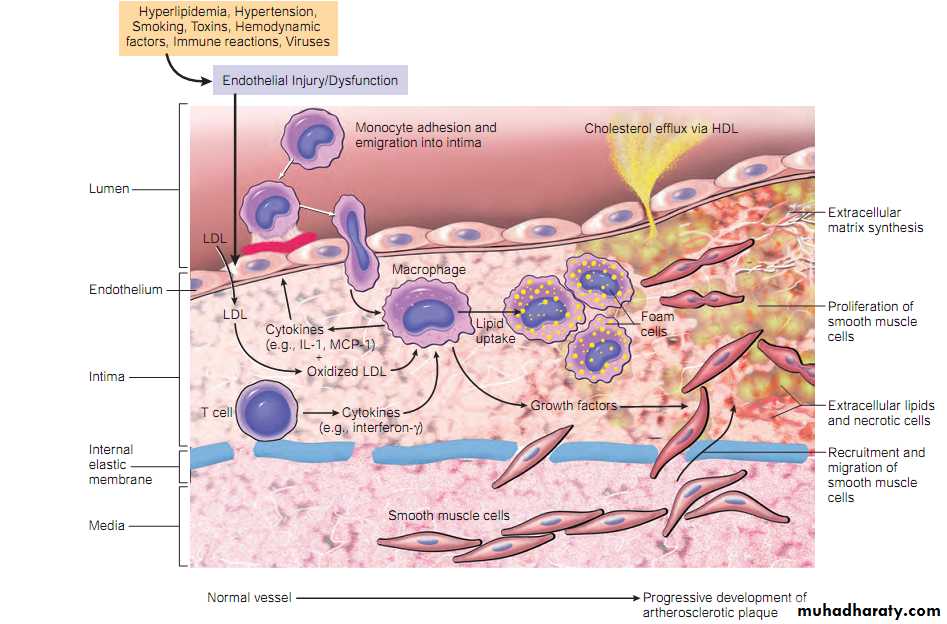
Pathogenesis
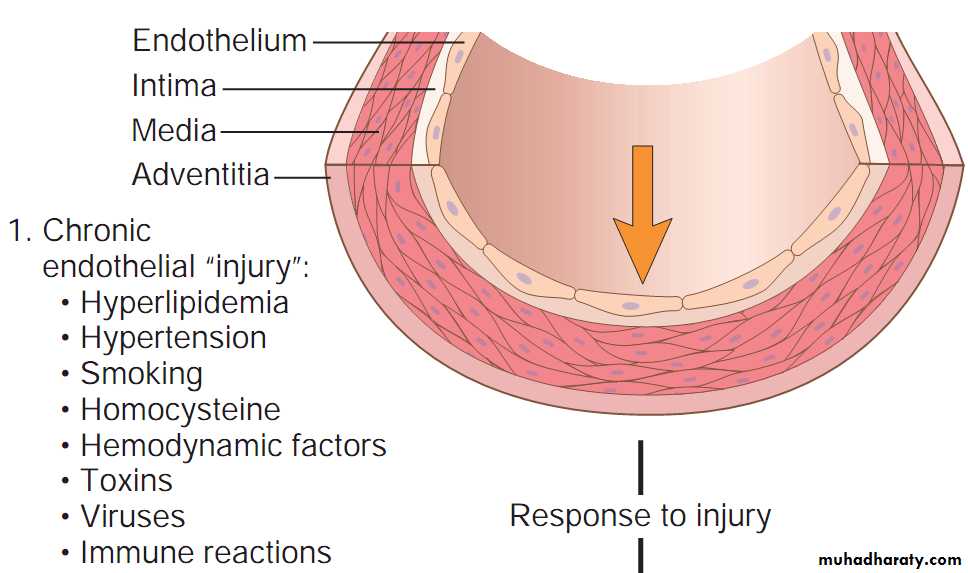
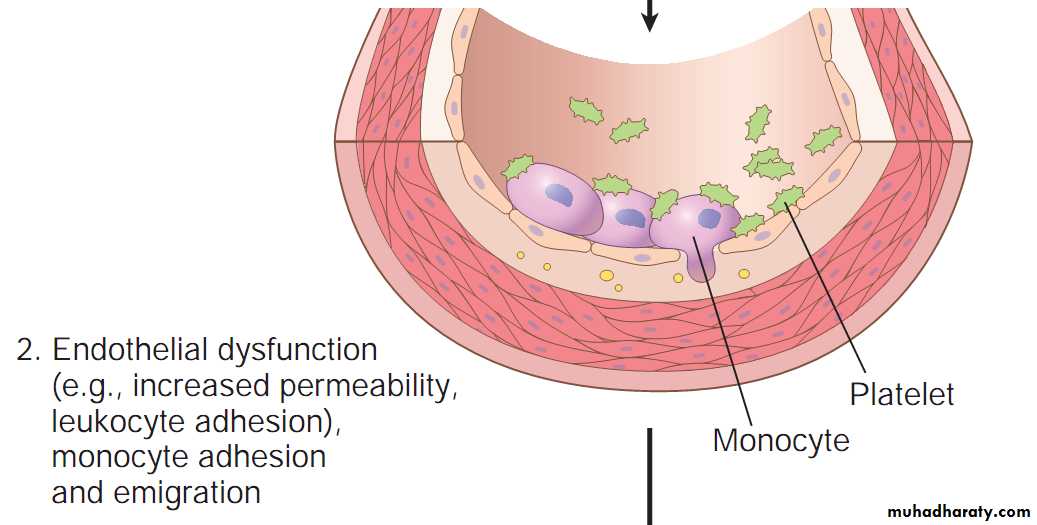
I- Response to injury hypothesis
• Endothelial injury and dysfunction: causing increased vascular permeability, leukocyte adhesion, and thrombosis
• Accumulation of lipoproteins (mainly LDL and its oxidized forms) in the vessel wall
• Monocyte adhesion to the endothelium, followed by migration into the intima and transformation into macrophages and foam cells
• Platelet adhesion
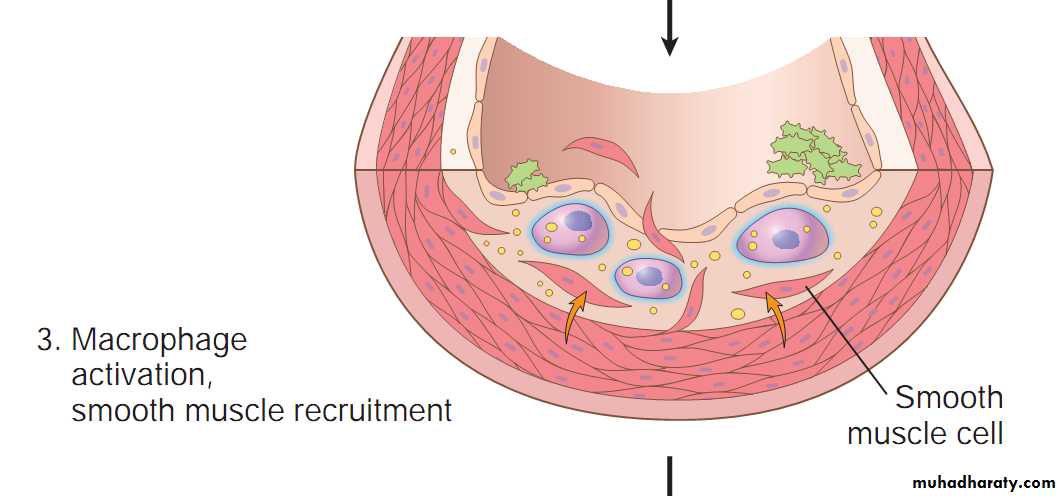
• Factor release from activated platelets, macrophages, and vascular wall cells, inducing smooth muscle cell recruitment, either from the media or from circulating precursors
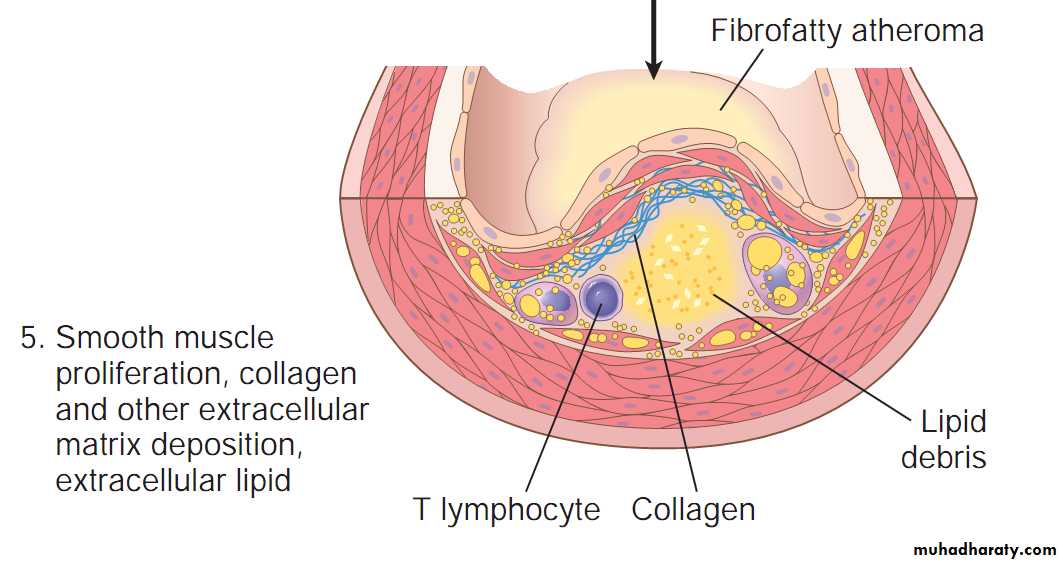
• Smooth muscle cell proliferation, extracellular matrix production, and recruitment of T cells.
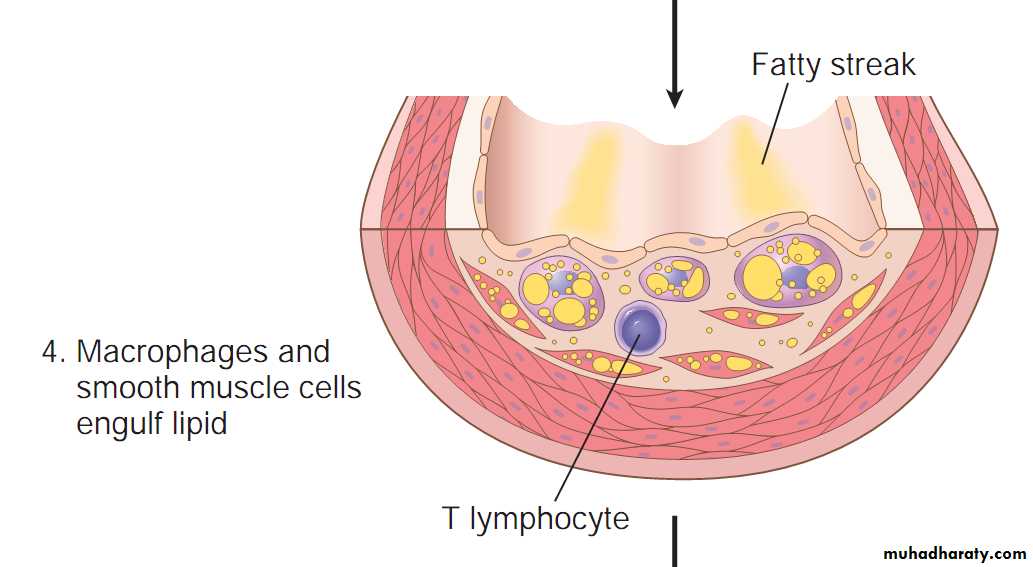
• Lipid accumulation both extracellularly and within cells (macrophages and smooth muscle cell)
Sequence of cellular interactions in atherosclerosis
Evolution of arterial wall changes in response to injury hypothesis
II- Other hypotheses: -Oligoclonality of lesion -Infection
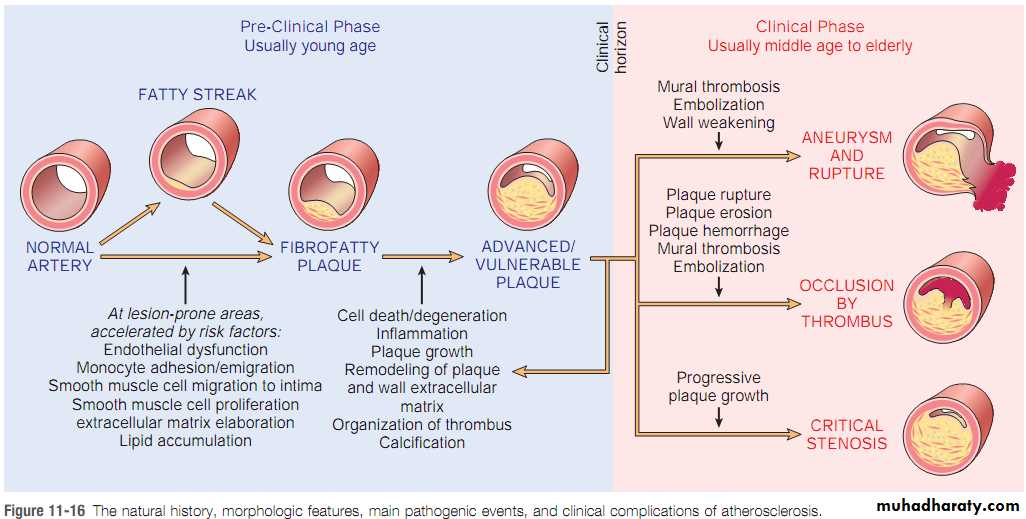
Natural history and consequences:The lesion is divided into 6 types:
1- Fat dots
2- Fatty Streaks
3- Intermediate
4- Atheroma or Atherosclerotic Plaque. The key features of these lesions are intimal thickening and lipid accumulation. 5- fibroatheroma (or atheroma with thick fibrous capsule)
6- complicated atheroma
Morphology :
Raised focal lesion within the intima with soft yellow core of lipid (mainly cholesterol and cholesterol esters), covered by firm fibrous cap.
Size range is 0.3-several centimeters, at first patchy in which later on becomes more numerous and diffuse
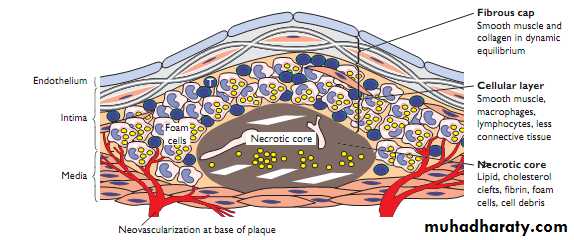
Components:
Cells: (smooth muscle, macrophages• and other leukocytes (T lymphocutes))
Extracellular matrix, (collagen, elastic fibers and proteoglycans)
Iintracellular and extracellular lipid
The key components of atheromatous plaque.
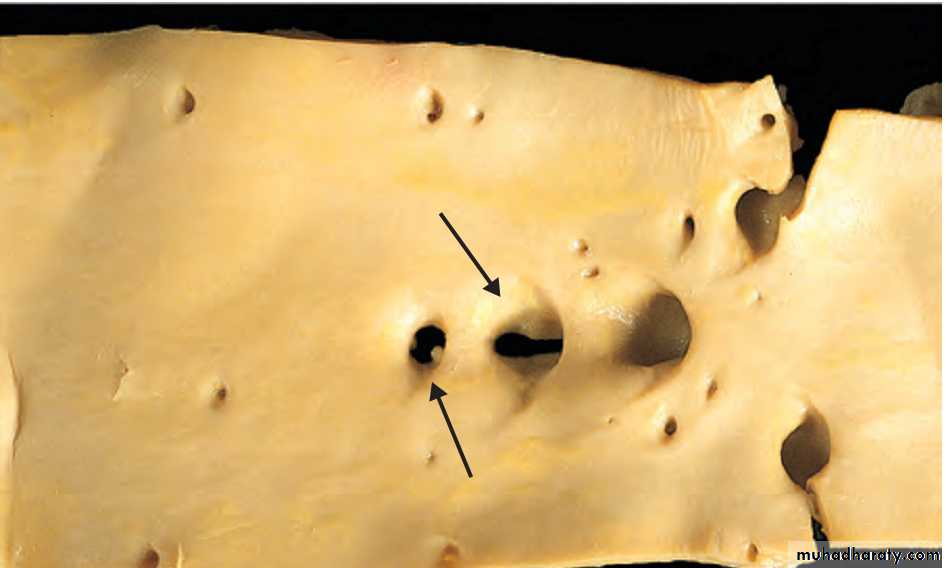
Aorta; Fat streaks
Aorta with fatty streaks, mainly near the ostia of branch vessels.Fatty streak in an experimental hypercholesterolemic rabbit, demonstrating intimal, macrophage-derived foam cells
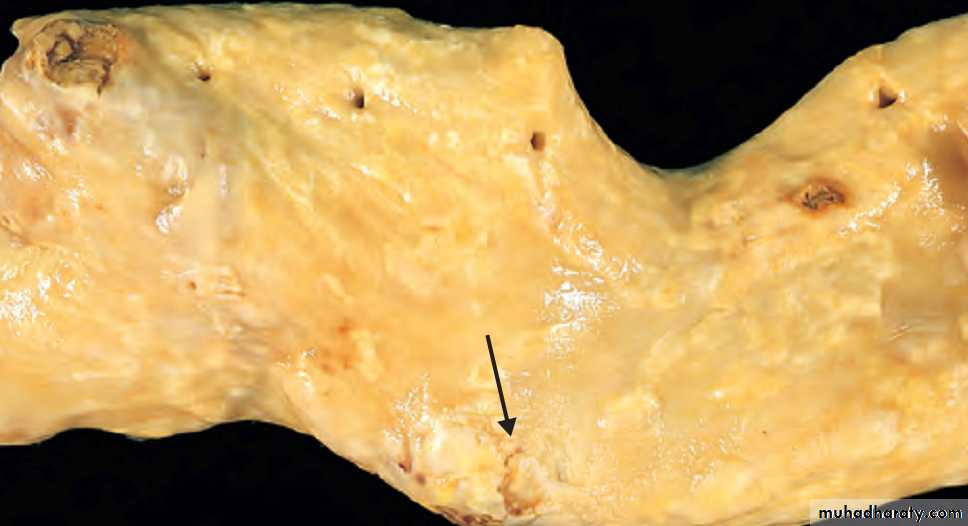
Aorta, mild atherosclerosis
composed of fibrous plaques, one denoted by the arrow.
Aorta ; severe diffuse atherosclerosis
complicated lesions, including an ulcerated plaque , and a lesion with overlying thrombus.Atherosclerosis
Complications:1. Rupture, ulceration, and erosion of the luminal surface of atheromatous plaques exposes highly thrombogenic substances and induces thrombus formation.2. Hemorrhage in to plaque. (Rupture of the overlying fibrous cap or of the thin-walled vessels in the areas of neovascularization can cause intra-plaque hemorrhage; the resulting hematoma may cause rapid plaque expansion or plaque rupture).3. Atheroembolism (Ruptured plaque can discharge debris into the blood, producing microemboli composed of plaque contents).
4. Aneurysm formation. (Atherosclerosis-induced pressure or ischemic atrophy of the underlying media, with loss of elastic tissue, causes structural weakening that can lead to aneurysmal dilation and rupture).
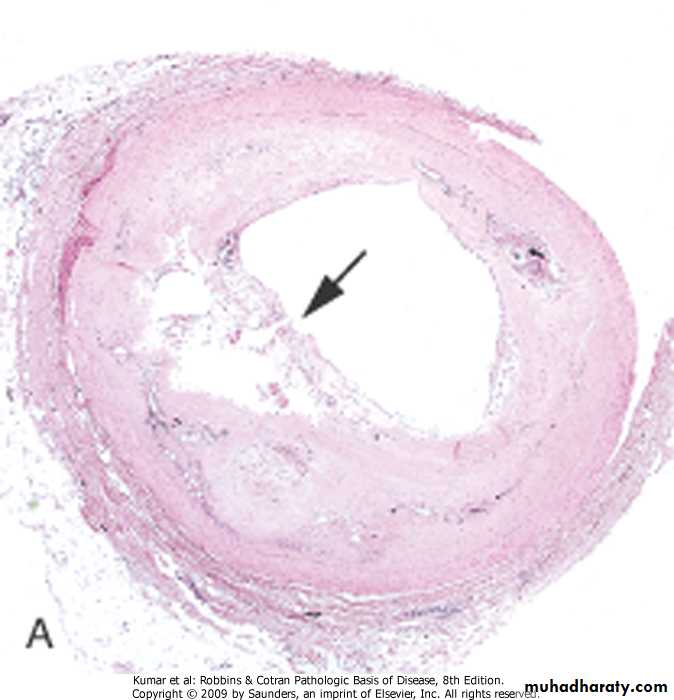
Coronary artery, plaque rupture, without superimposed thrombus, in a patient who died suddenly
s plaque
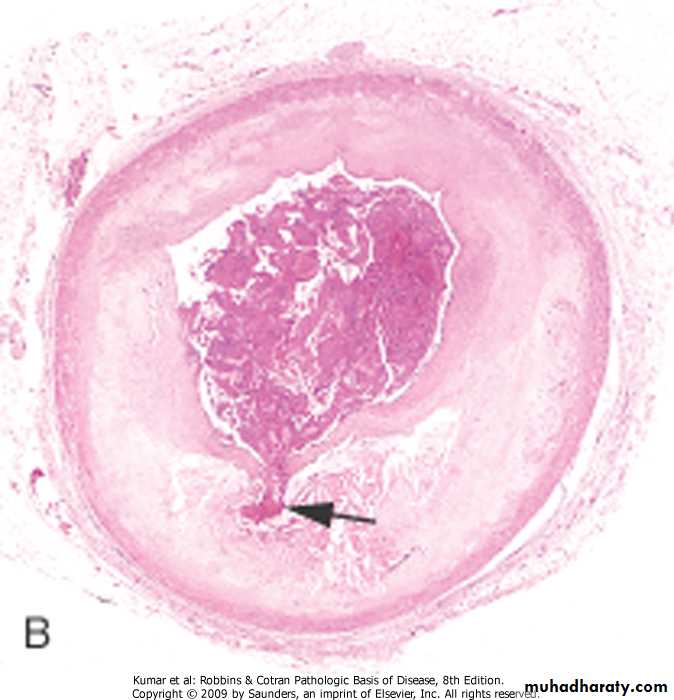
Coronary artery, thrombus overlying complicated atheroma (Acute coronary thrombosis superimposed on an atherosclerotic plaque with focal disruption of the fibrous cap)Atherosclerosis, natural history, morphology, pathogentic events, complications
Major clinical consequences of atherosclerosis
Myocardial infarction (heart attack)Cerebral infarction (stroke),
Aortic aneurysms
Peripheral vascular disease (gangrene of the legs)
Bowel ischemia
Hypertensive vascular disease
• Multifactorial disorder, (genetic &• environmental)
• Defined as: sustained elevation of blood pressure above 140/90 mmHg
• .Types:
• -Essential (idiopathic) 95%
• -Secondary 5% to
• .renal disease
• .endocrine abnormality
• .cardiovascular disorder
• .neurogenic cause
Regulation of normal blood pressure
Blood pressure is controlled by:
1. Cardiac output
2. Peripheral vascular resistance*Morphology -Atherosclerosis -Hyaline arteriolosclerosis -Hyperplastic arteriolosclerosis
AtherosclerosisHypertension accelerates atherogenesis
Causes degenerative changes in the walls, can lead to aortic dissection and cerebrovascular hemorrhage.
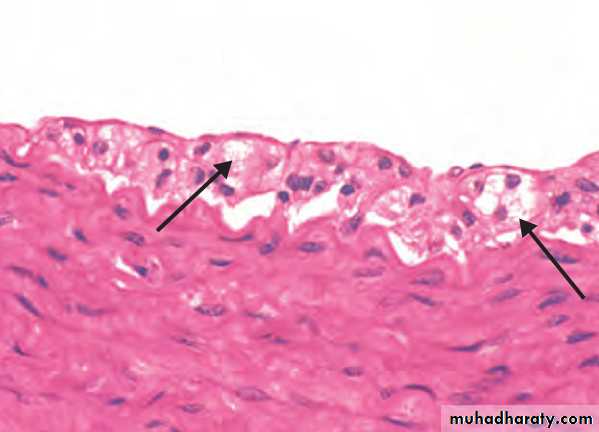
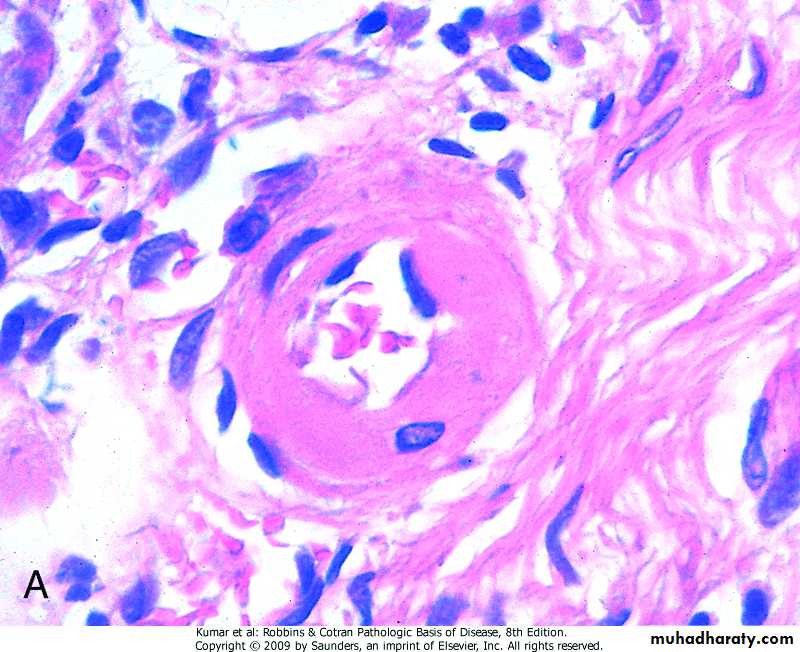
Hyaline arteriolosclerosis
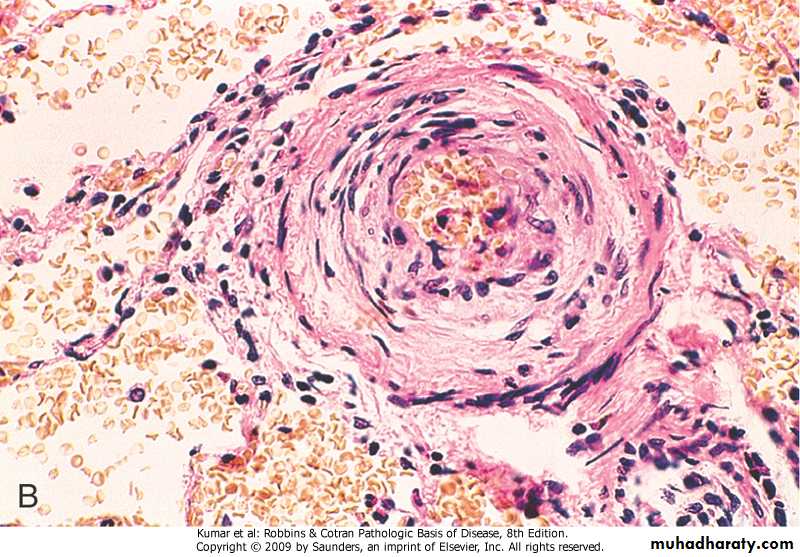
Associated with benign hypertension. It is marked by homogeneous, pink hyaline thickening of the arteriolar walls, and luminal narrowing caused by leakage of plasma components across injured endothelial cells. ( Hyaline arteriolosclerosis)Hyperplastic arteriolosclerosis
Typical of severe hypertension. “onionskin,” concentric, laminated thickening of arteriolar walls and luminal narrowing . The laminations consist of smooth muscle cells and thickened, reduplicated basement membrane. (Hyperplastic arteriolosclerosis)Aneurysm
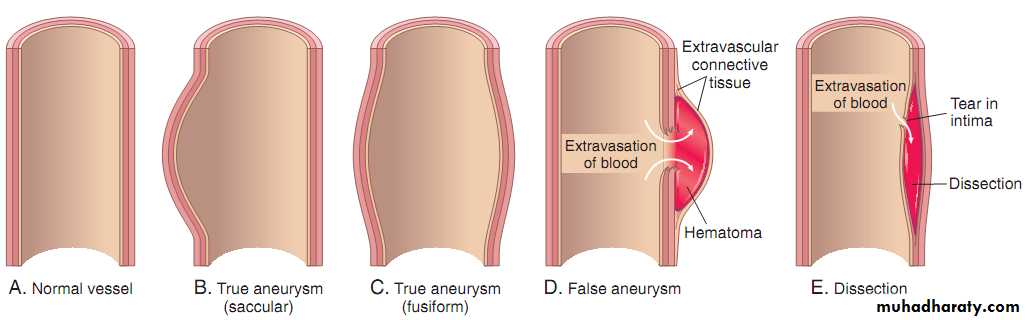
Localized abnormal dilation (saccularor fusiform) of blood vessels or the wall
of the heart.
Classified into:
-True
-False
Aneurysms.
(A) Normal vessel. (B) True aneurysm, saccular type. The wall bulges outward and may be attenuated but is otherwise intact. (C) True aneurysm, fusiform type. There is circumferential dilation of the vessel. (D) False aneurysm. The wall is ruptured, creating a collection of blood (hematoma) bounded externally by adherent extravascular tissues. (E) Dissection. Blood has entered the wall of the vessel and separated (dissected) the layers.Causes of aneurysm: - Atherosclerosis
- Hypertension - Congenital - Trauma - Infection …syphilis - InflammationMost important
Pathogenesis of aneurysm:Inadequate or abnormal connective tissue synthesis:
Marfan syndrome: defective synthesis of the scaffolding protein Fibrillin
Ehlers-Danlos syndrome: Defective type III collagen synthesis
Excessive connective tissue degradation: such as by macrophages in atherosclerotic plaque.
Loss of smooth muscle cells or change in the smooth muscle cell synthetic phenotype: Atherosclerotic thickening of the intima can cause ischemia of the inner media
Abdominal Aortic Aneurysm (AAA)
Rare <50 yrs
> in malesPositioned between renal arteries
origin and bifurcation of aorta
Either saccular or fusiform
Up to 15cm in diameter and 25cm in length
Abdominal aortic aneurysm
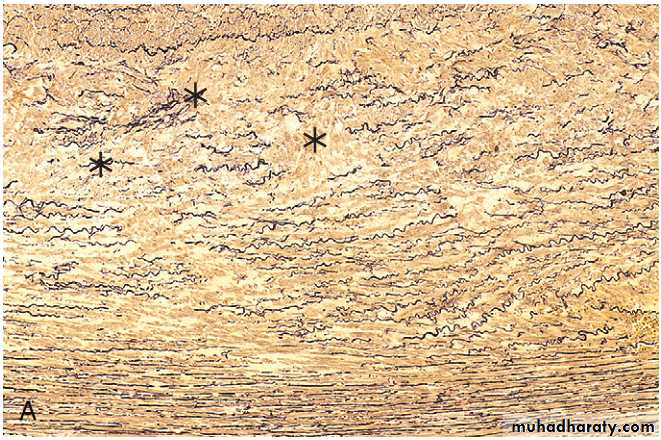
Aorta, cystic medial degeneration with loss of elastin
* Clinical course:
. Rupture (related to size). Obstruction of blood vessels
. Embolism
. Pressure on adjacent structures
. Abdominal mass
THANK YOU