Neurological
Examination;

Introduction
Select appropriate questions to elicit from the
patient with a neurological complaint during a
patient interview
Differentiate “normal” from “abnormal”
findings on neurological examination
Identify common causes of various cranial
nerve palsies
Determine location of neurological lesion
Differentiate amongst the various movement
disorders

Differentiate atrophy and hypertrophy.
Differentiate between spasticity, rigidity, and flaccidity,
and identify common causes of each.
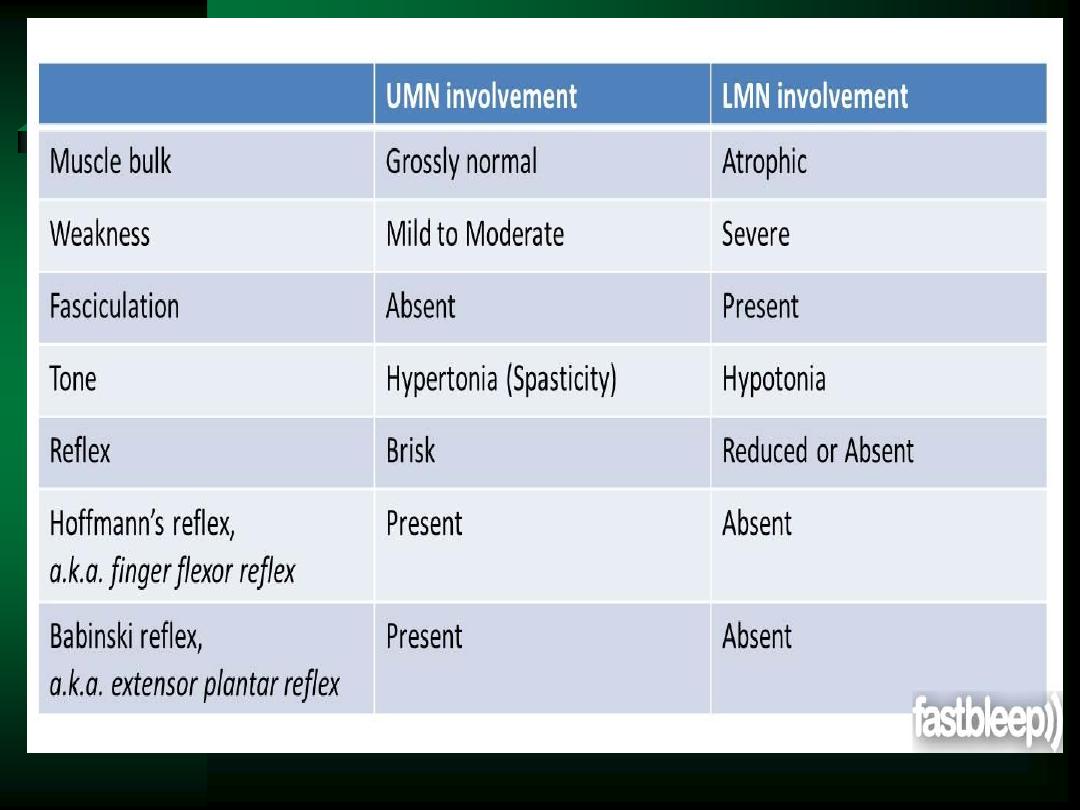
Differentiate upper motor neuron lesions from lower
motor neuron lesions.
Differentiate CNS disorders from PNS disorders, and
identify location of the lesion & common causes.

TERMS
Paresis – slight or incomplete paralysis
Paralysis (plegia) – loss or impairment of
motor function
Hemiparesis
Hemiplegia
Paraplegia
Quadriplegia

Atrophy – a decrease in size
Hypertrophy
– enlargement of an organ or part due to an increase in size of its
constituent cells
Spasticity – hypertonicity with increased DTRs
Rigidity – stiffness or inflexibility
Flaccidity – loss of tone with diminished DTRs
.

FOCUS
Mental status
Cranial nerves
Motor function
Reflexes
Sensory status
Coordination and balance

HISTORY
Chief complaint
Headache?
Vertigo?
Visual disturbance?
Tremors or dyskinesias?
Weakness?
Paresthesias?
Loss of consciousness?

Alertness
Attention
Orientation
– Person, Place, Time, & Situation
Cognitive function
Perception
– Illusions =
misinterpretations of real external stimuli
– Hallucinations =
subjective sensory perceptions in the absence of stimuli
Judgment
Memory
– Short-term & long-term
Speech
– Rate & rhythm
– Spontaneity
– Fluency
– Simple vs. complex
MENTAL STATUS

Testing Cognitive Function
*
*
*
Information & vocabulary
– Common
Calculating
– Simple math
– Word problems
Abstract thinking
– Proverbs
– Similarities/differences
Construction
– Copy figures of increasing difficulty (i.e. circle, clock)
LANGUAGE
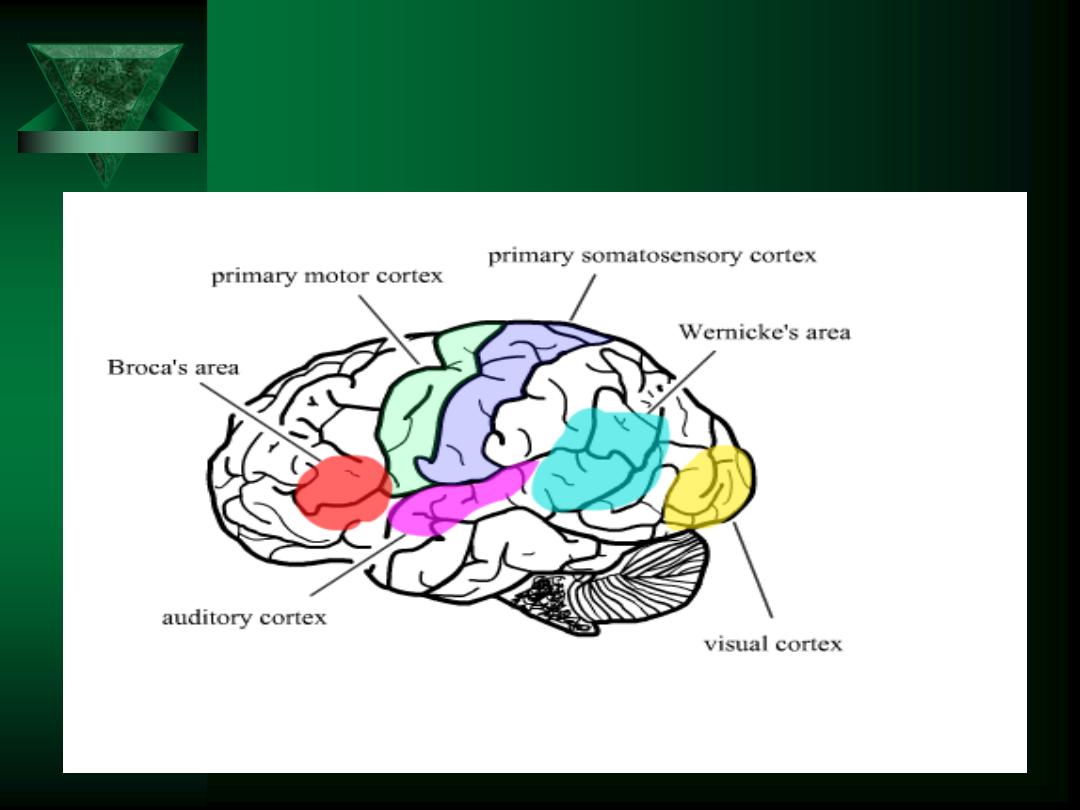
Cerebrum
Frontal - Conceptualization, motor ability
and judgment, thought process, emotions.
Parietal – Interpretation of sensory
information, ability to recognize body parts.
Temporal – memory storage, integration of
auditory stimuli.
Occipital – Visual Center.

Cerebellum
Cerebellum- Keeps person oriented
in space, balance. Doesn’t initiate
movement but coordinates it
Controls skeletal muscles
Controls voluntary movements

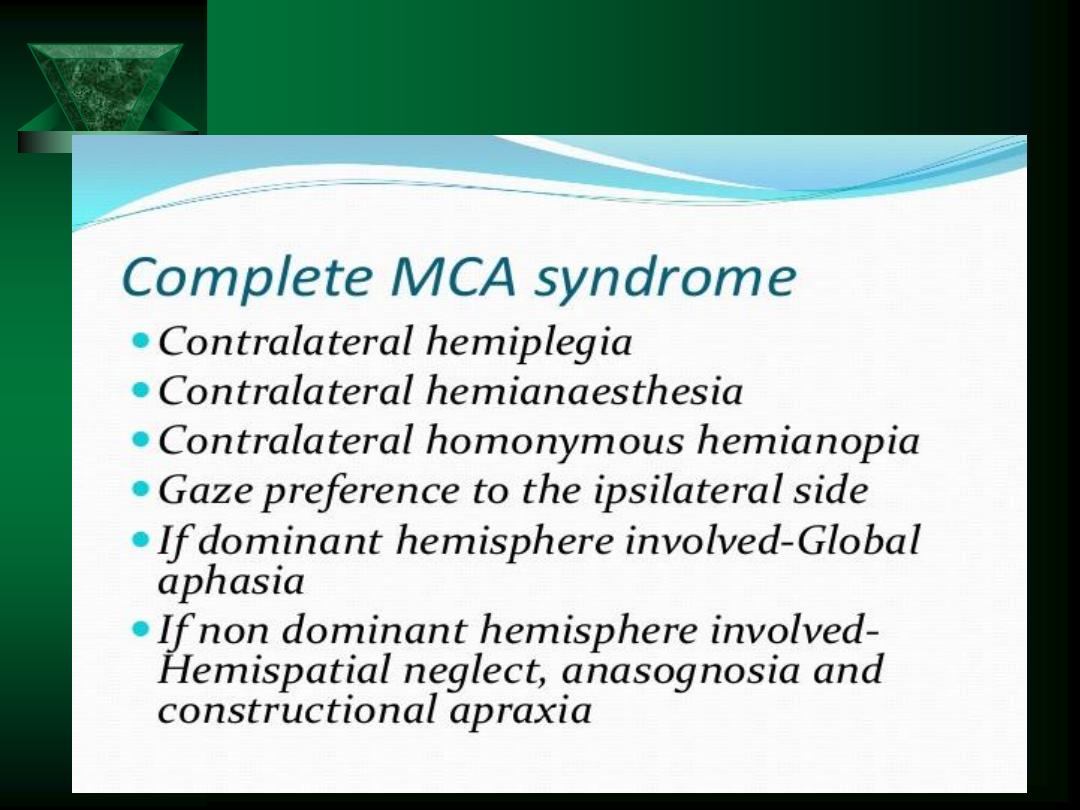
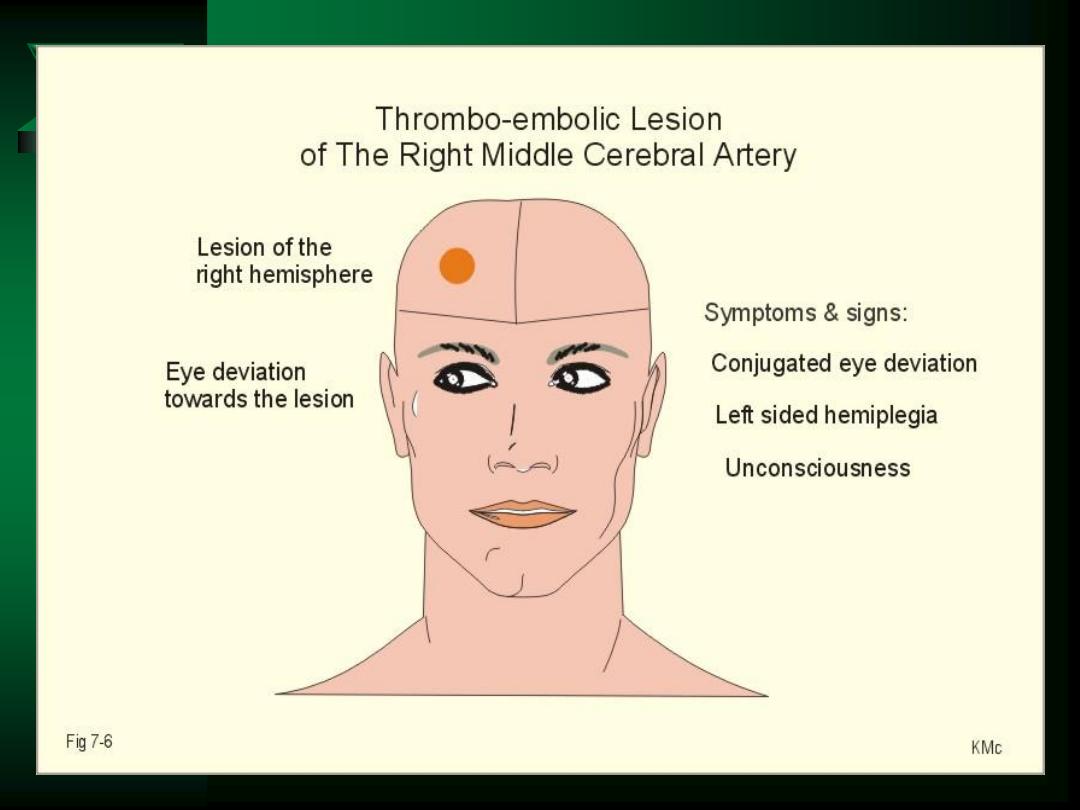
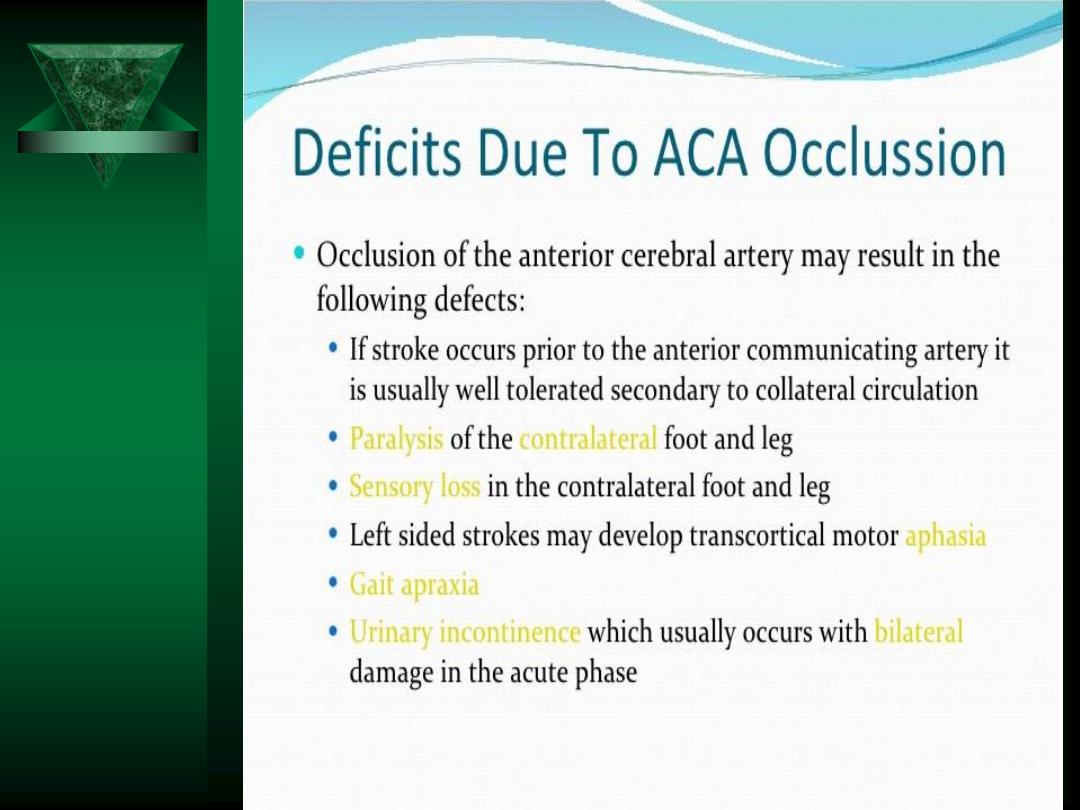
Localization
Cerebrum
– Impaired intellect, memory, higher brain function
Brain stem
– unconsciousness
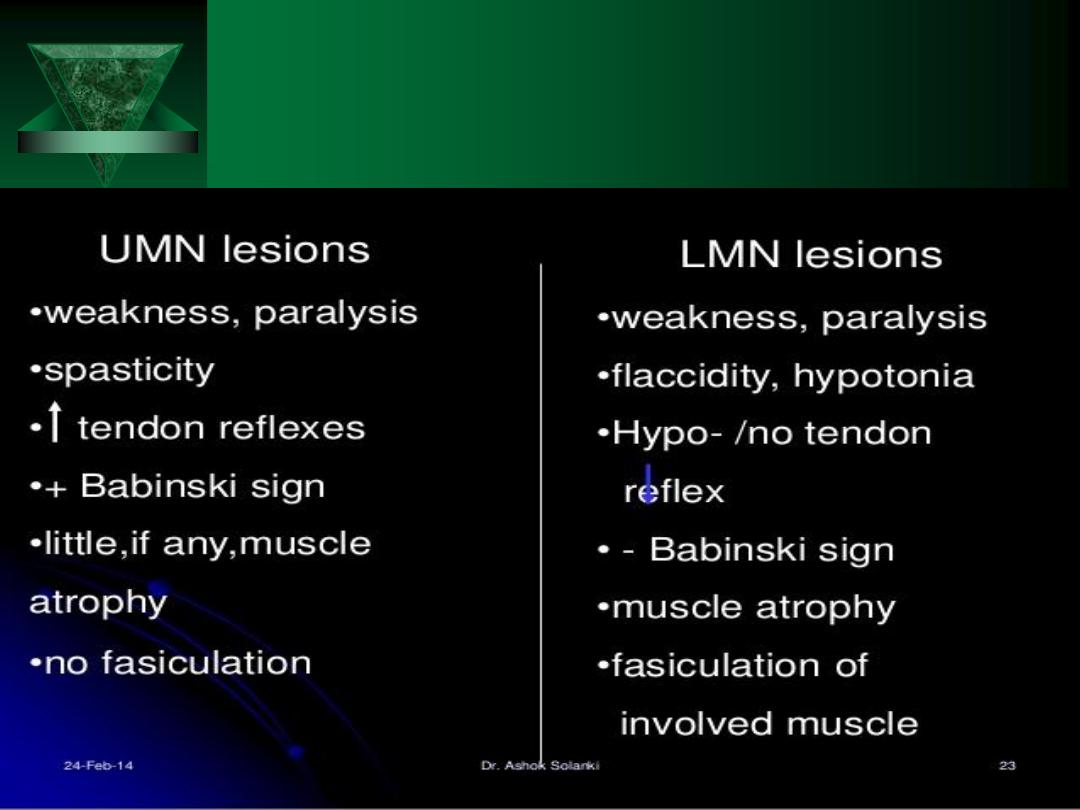
LMN
– paralysis with loss of DTRs
– muscle atrophy with fasciculation
LMN + anesthesia
– peripheral nerve or spinal root
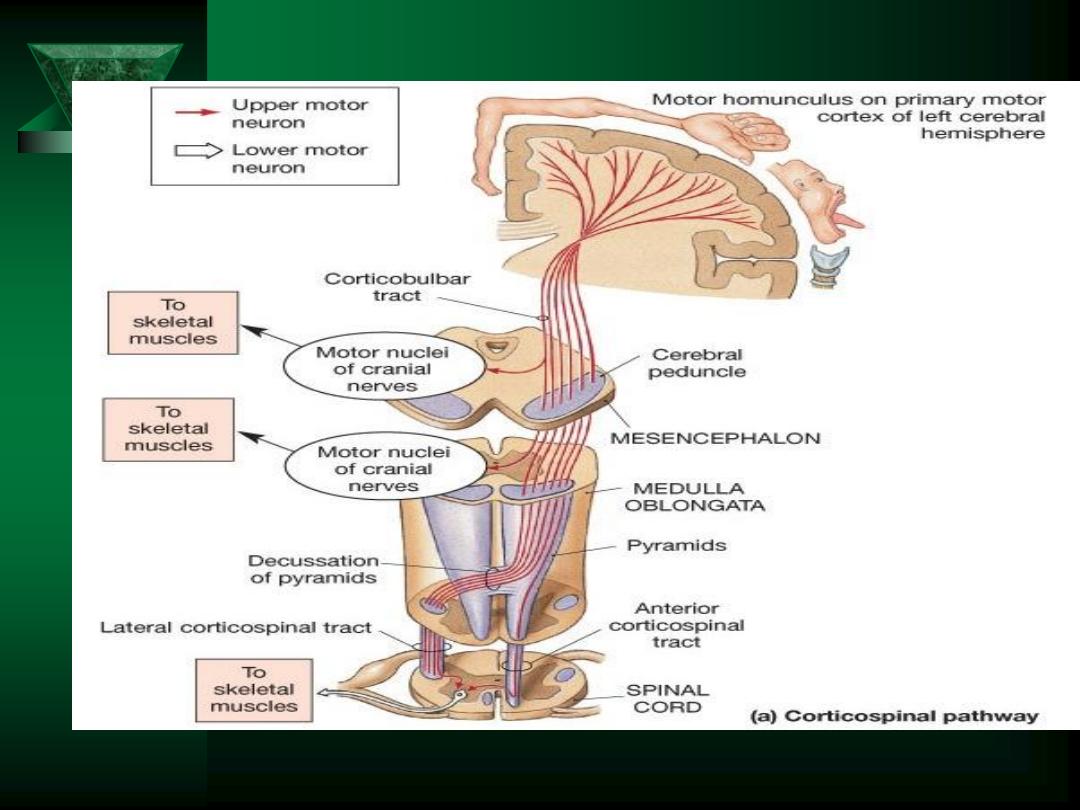
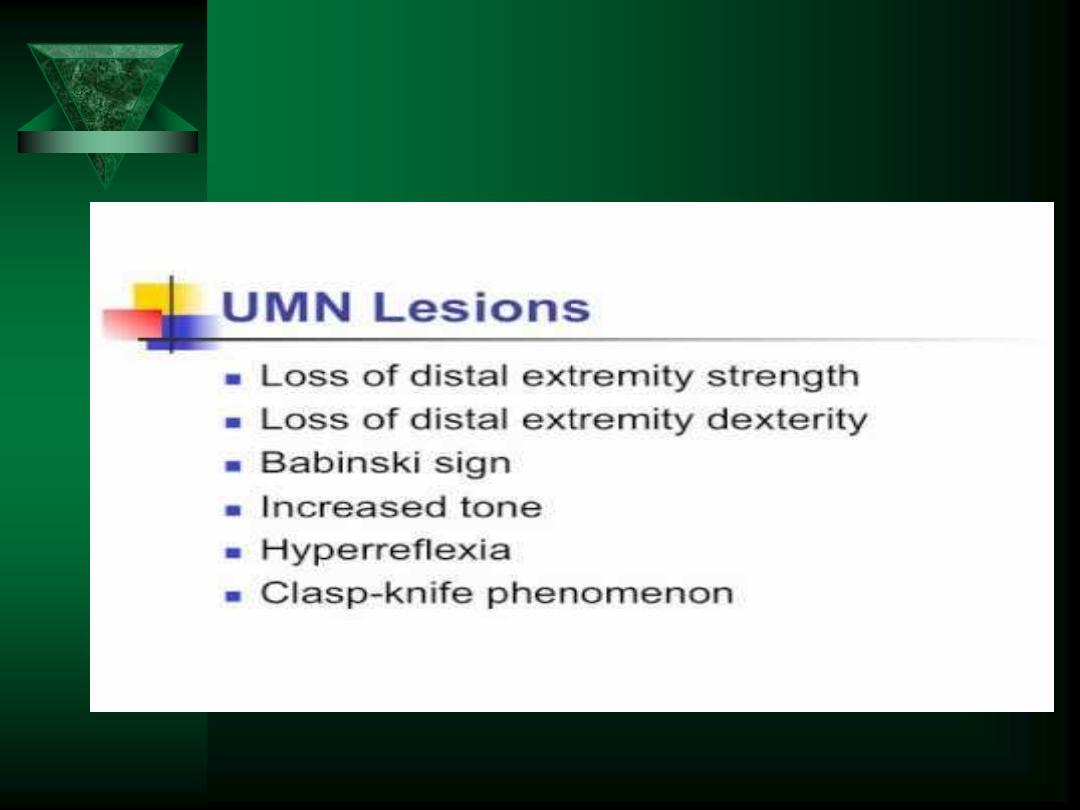
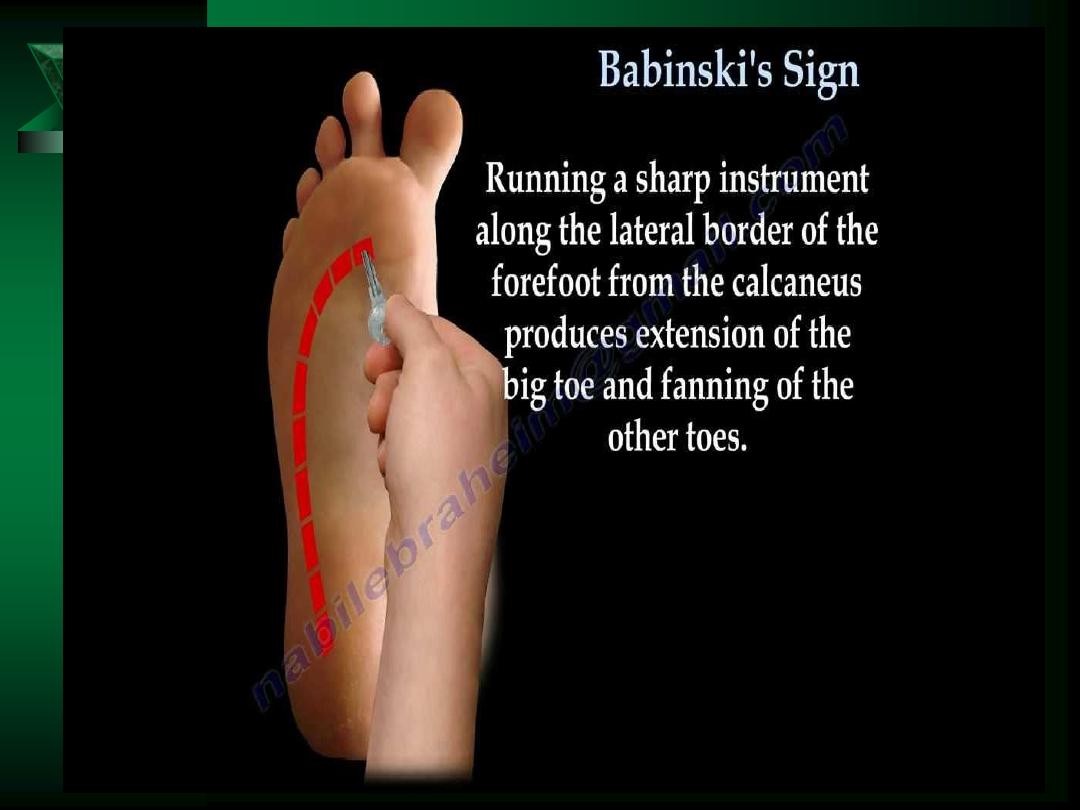
UMN
– involves whole muscle groups
– increased or spastic muscle tone
– +/- paralysis with DTR accentuation
– Positive Babinski

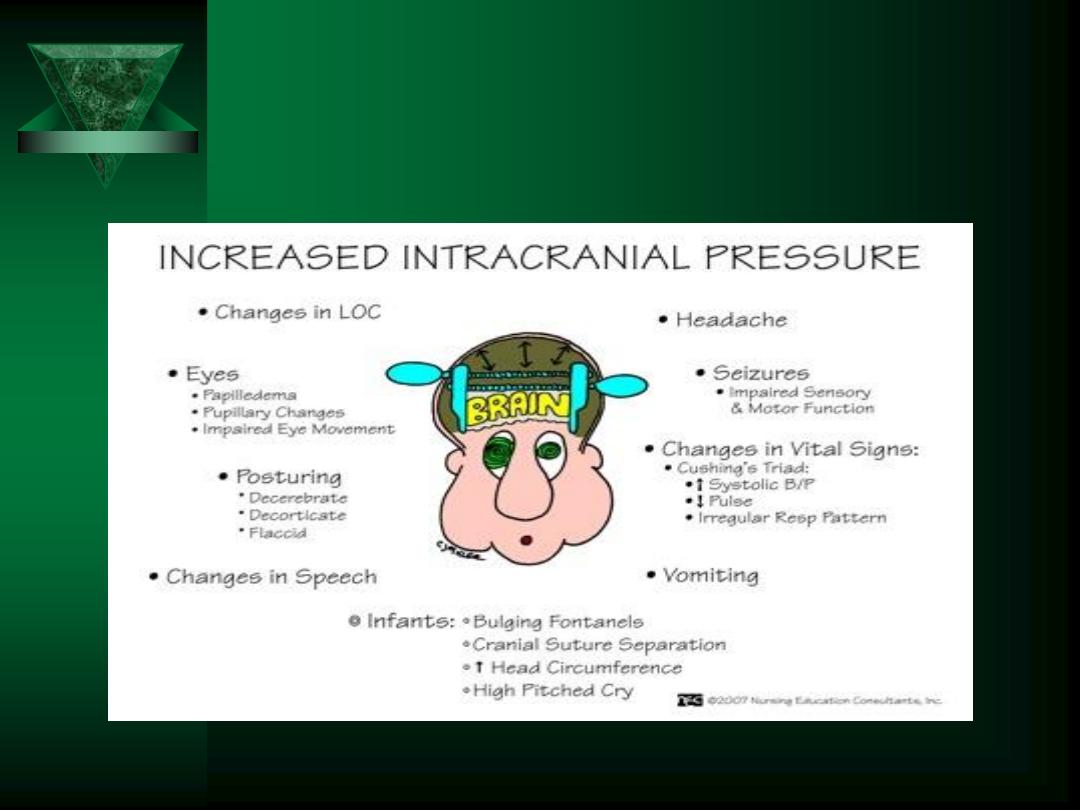
HEADACHE
Symptom! (not a disease)
Most important diagnostic clue
is a steady,
bilateral, nonthrobbing pain that is worse in
the a.m.
– May awaken patient
– Worse with VALSALVA

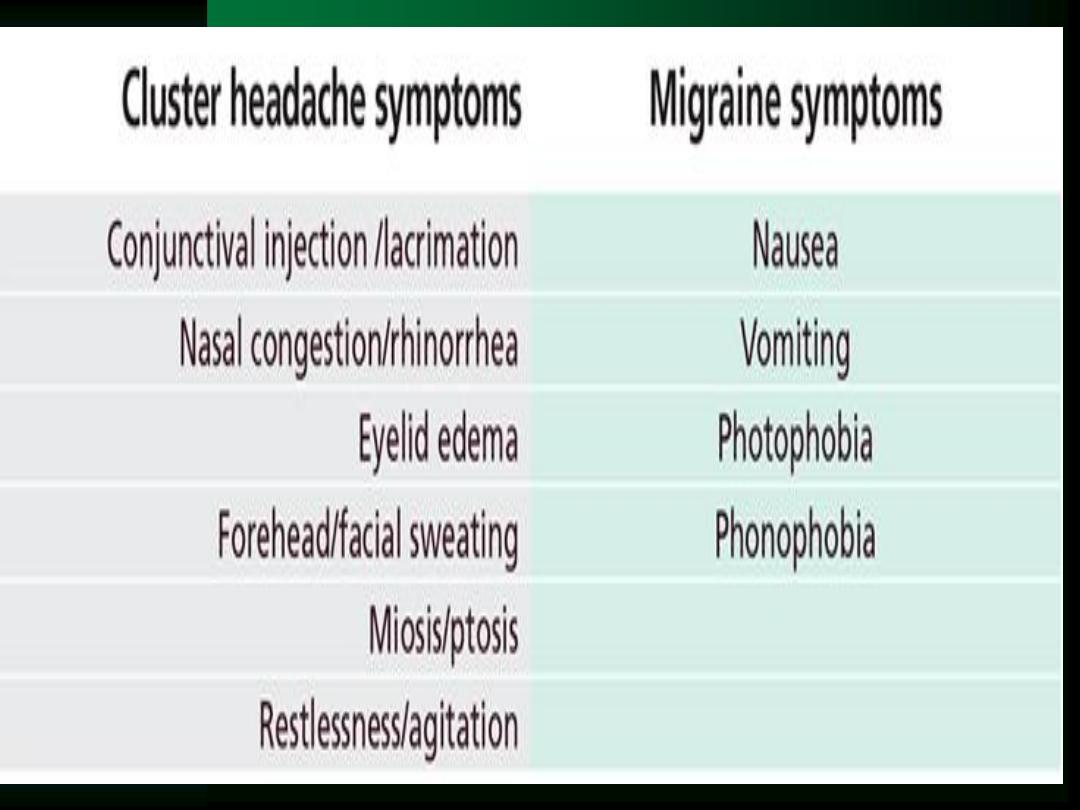
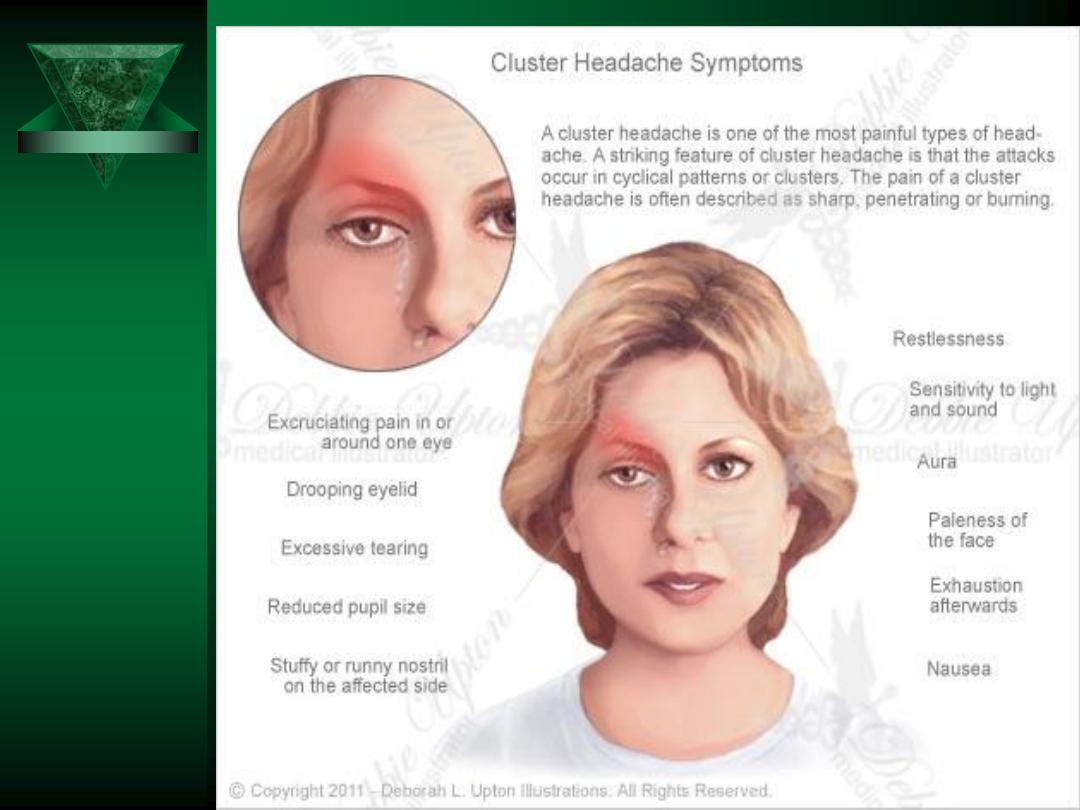
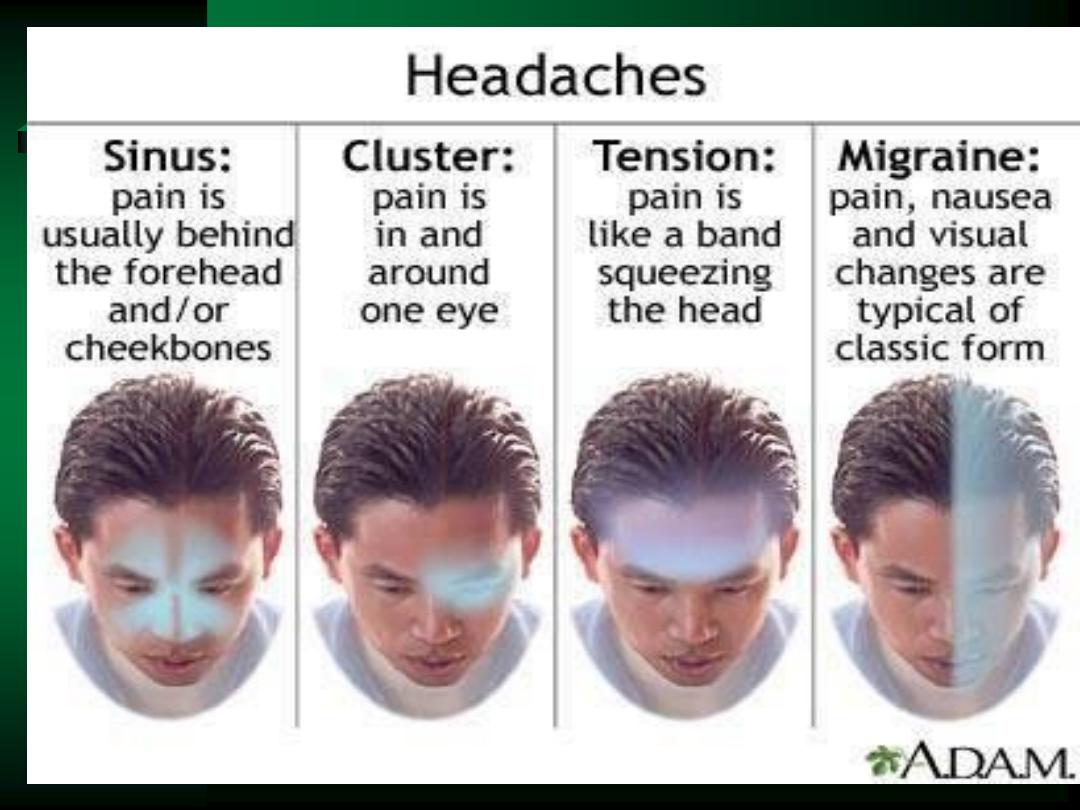
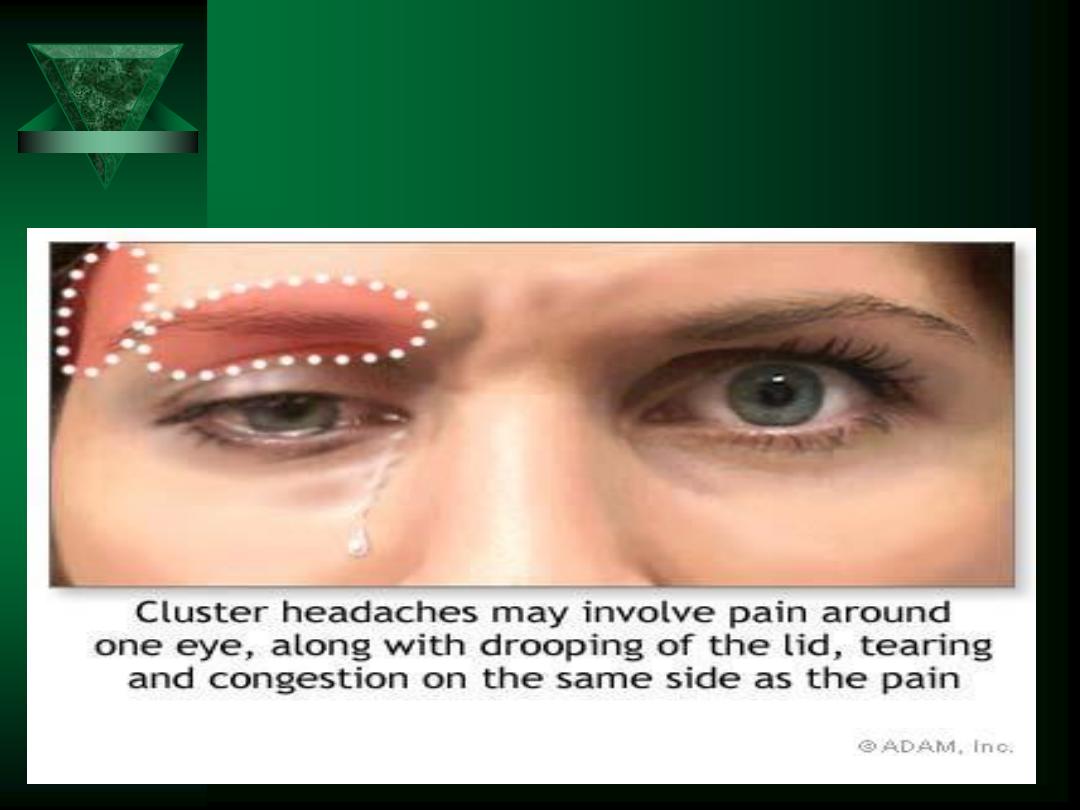
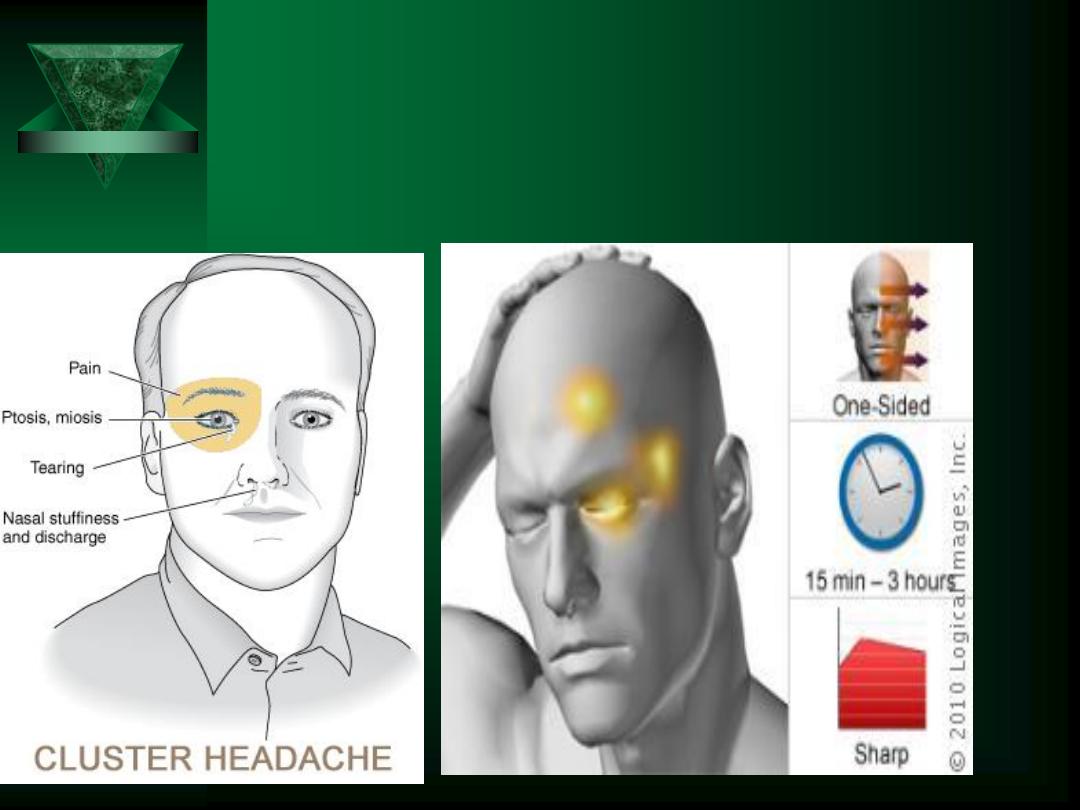
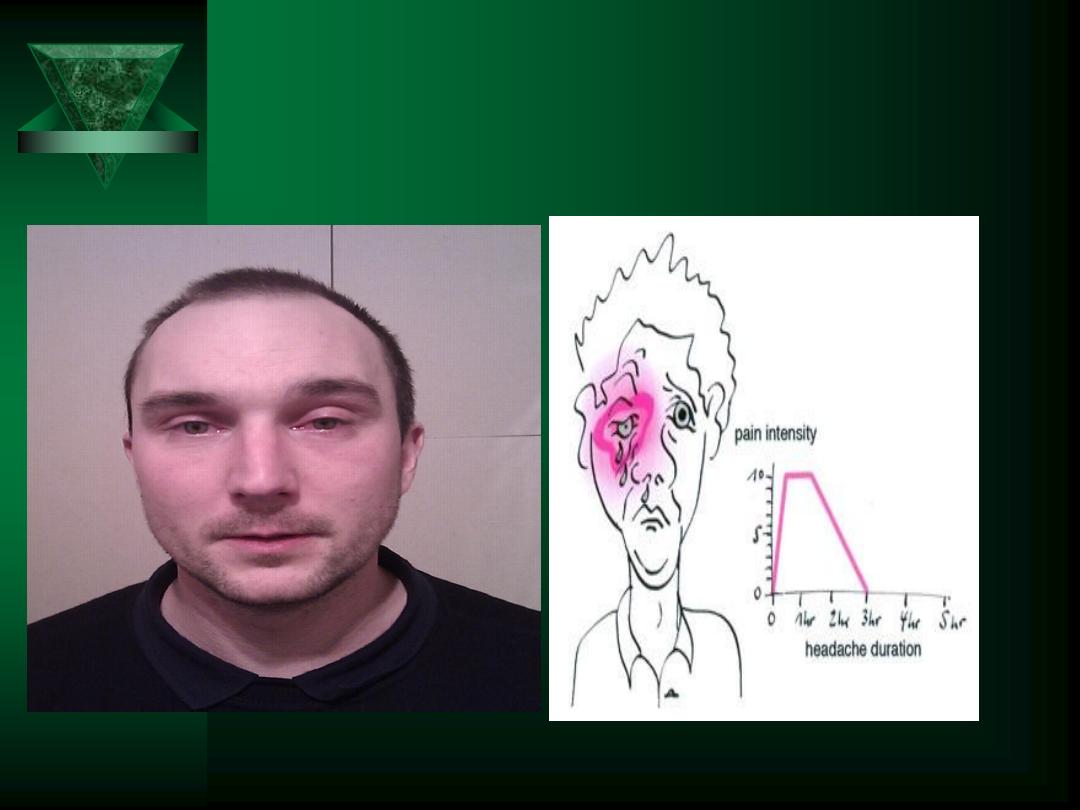
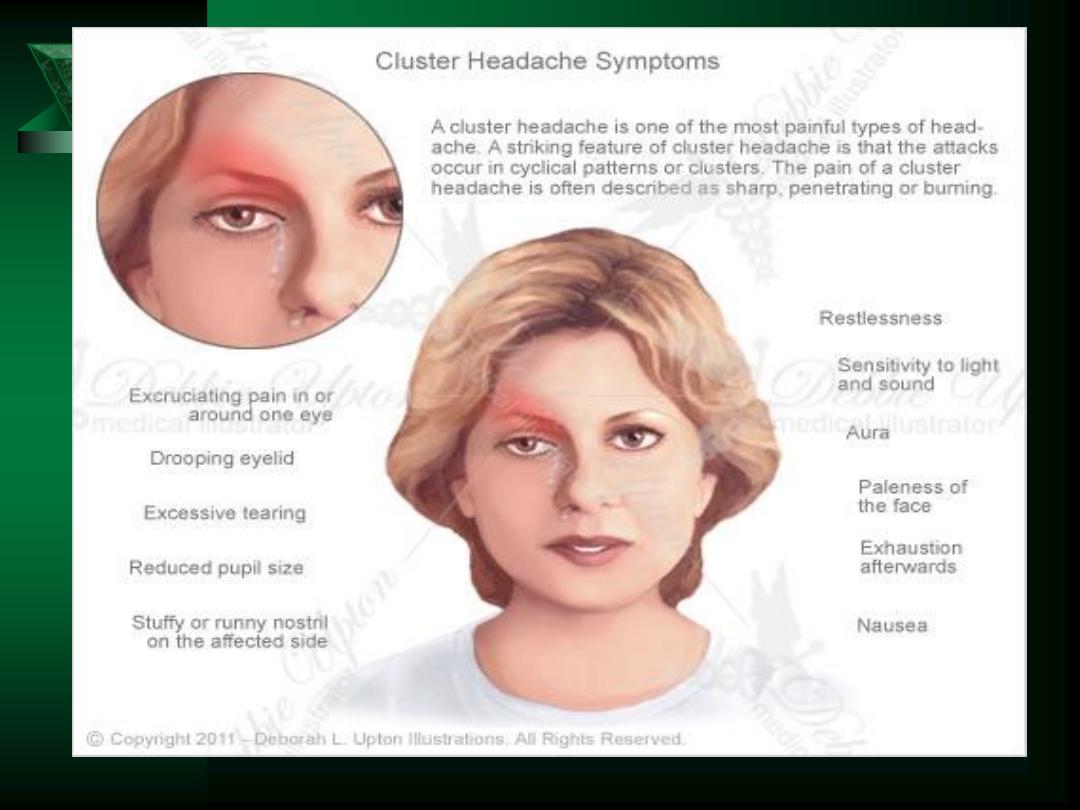
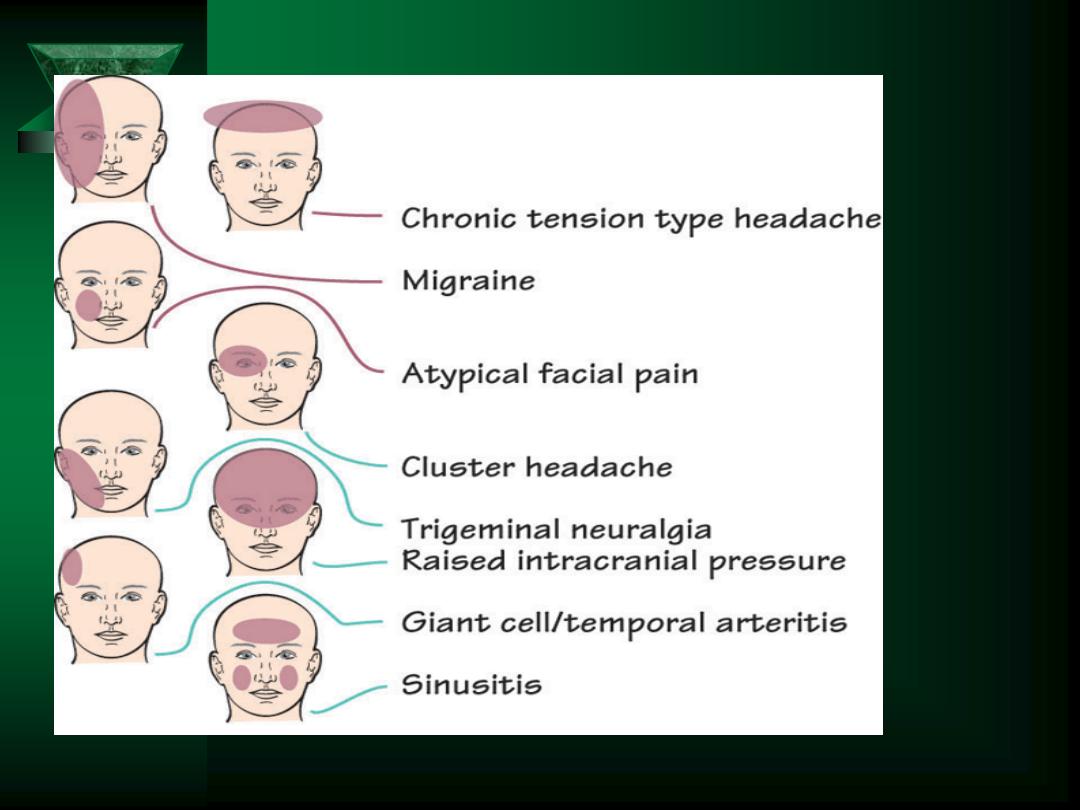
Types of Headaches
Tension
Sinus
Migraine
– Classic
– Common
– Complicated
– Cluster
Temporal Arteritis
ICP
Subarachnoid hemorrhage
Infection
Ocular
Trigeminal neuralgia (Tic
doloureaux)
TMJ syndrome
Toxic

Headache History
Location
– Unilateral ~ migraine
– Periorbital ~ glaucoma/uveitis
– Parietal/Occipital ~ tension
– Neck ~ meningitis or Subarachnoid hemorrhage
Quality
– “Throbbing” ~ vascular
– “Intermittent jabbing” ~ Trigeminal neuralgia
– “Pressure” ~ sinus
Radiation?
Severity
Timing
– Constant vs. intermittent
– Worse in a.m. or p.m.
Worst headache ever?????

HEADACHE HISTORY
Associated Sx’s
– Visual disturbance
– Vertigo
– N/V
– Dysesthesias
– Aura
Past medical history
Family history
Current medication/drug use
Suspect an extracranial etiology if pain is the only
symptom

REFLEXES
Corneal
Pharyngeal
Biceps
Triceps
Brachioradialis
Abdominal
Patellar (knee jerk)
Achilles (ankle jerk)
Babinski
– Positive suggests UMN lesion

Cranial Nerves
I
- Olfactory
II
- Optic
III - Oculomotor
IV - Trochlear
V
- Trigeminal
VI - Abducens
VII - Facial
VIII - Vestibulocochlear (Acoustic)
IX - Glossopharyngeal
X
- Vagus
XI - Accessory
XII - Hypoglossal

Cranial Nerve II
Responsible for vision
Test visual acuity!!!!
Pupillary size
– Swinging-flashlight test
Visual fields
– Peripheral vision
– Test by confrontation
Fundoscopic examination
– Papilledema

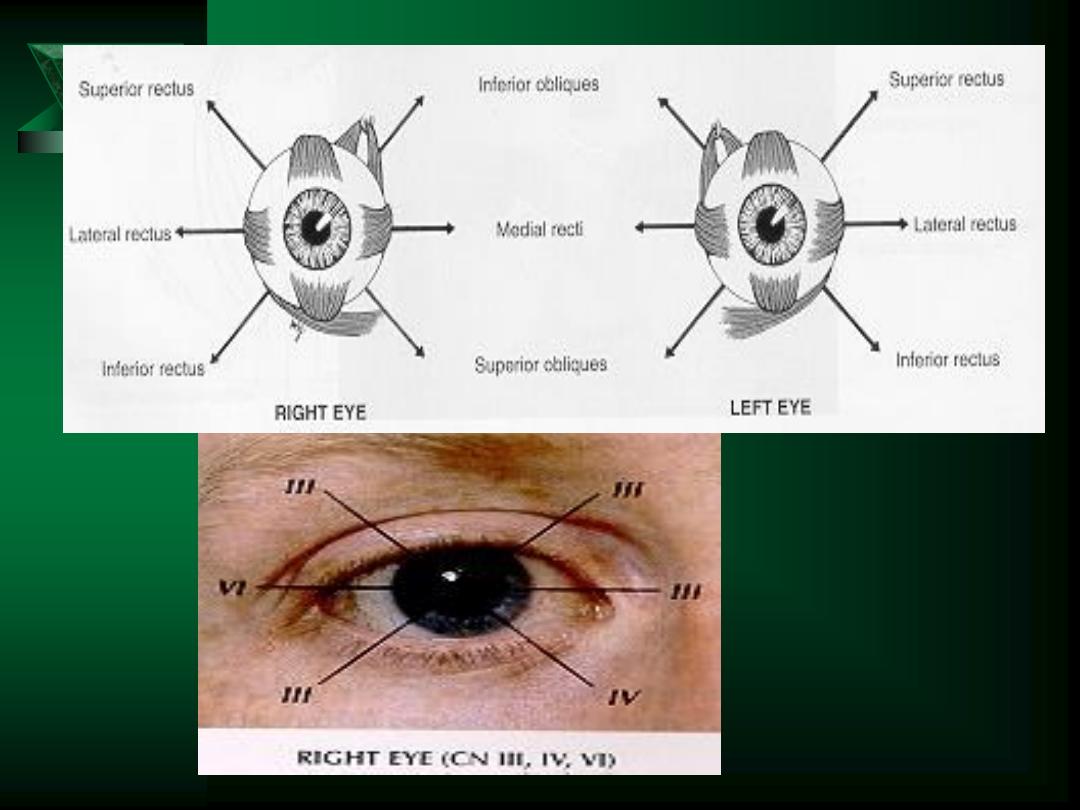
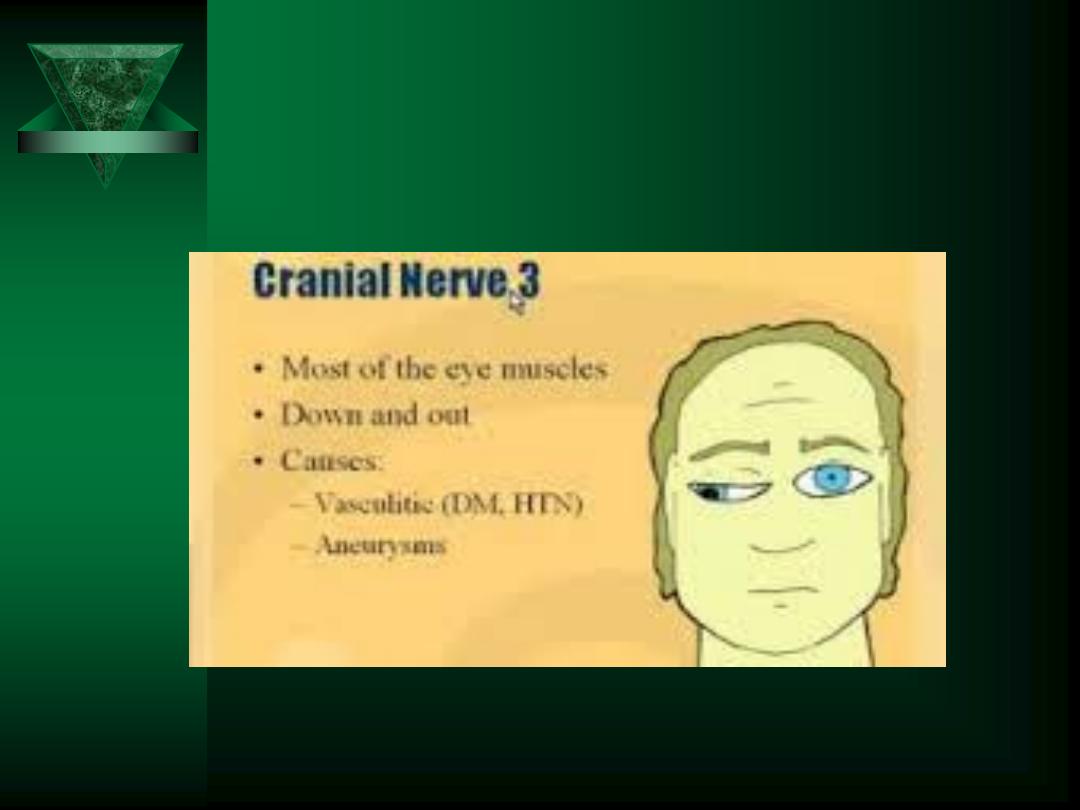
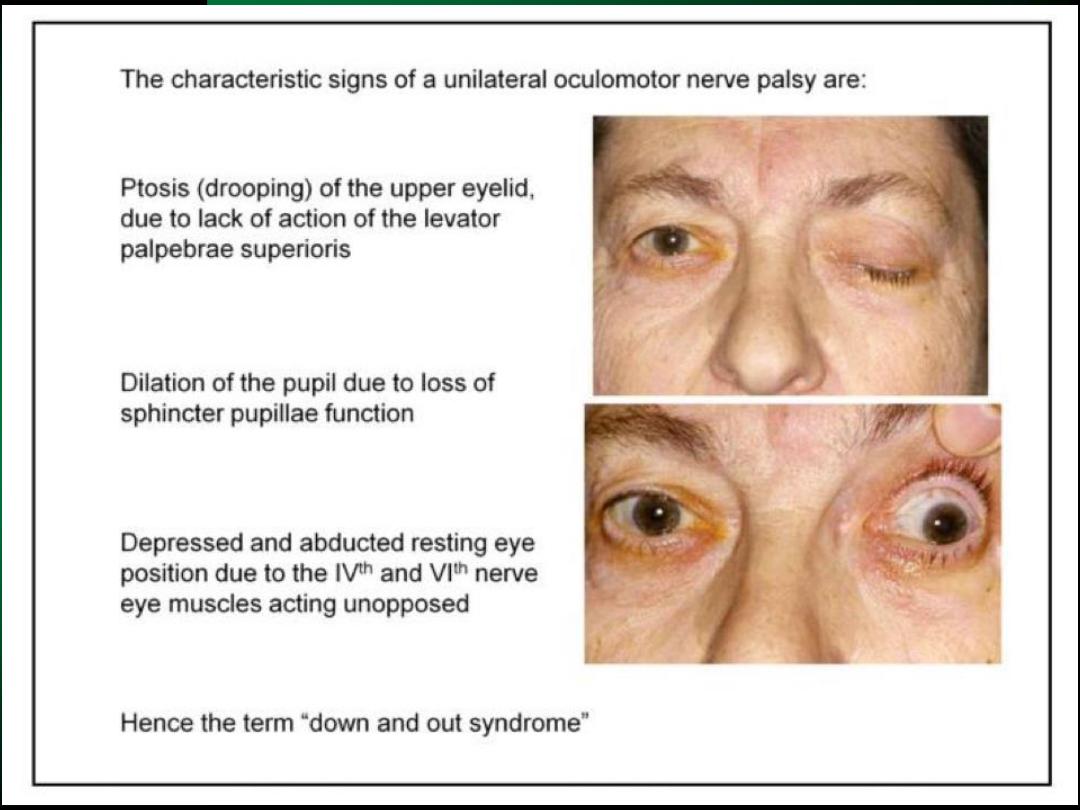
Cranial Nerves III, IV, VI
CN III involved in:
Pupillary reflex
Opening of the eyelids
Most extraocular movements
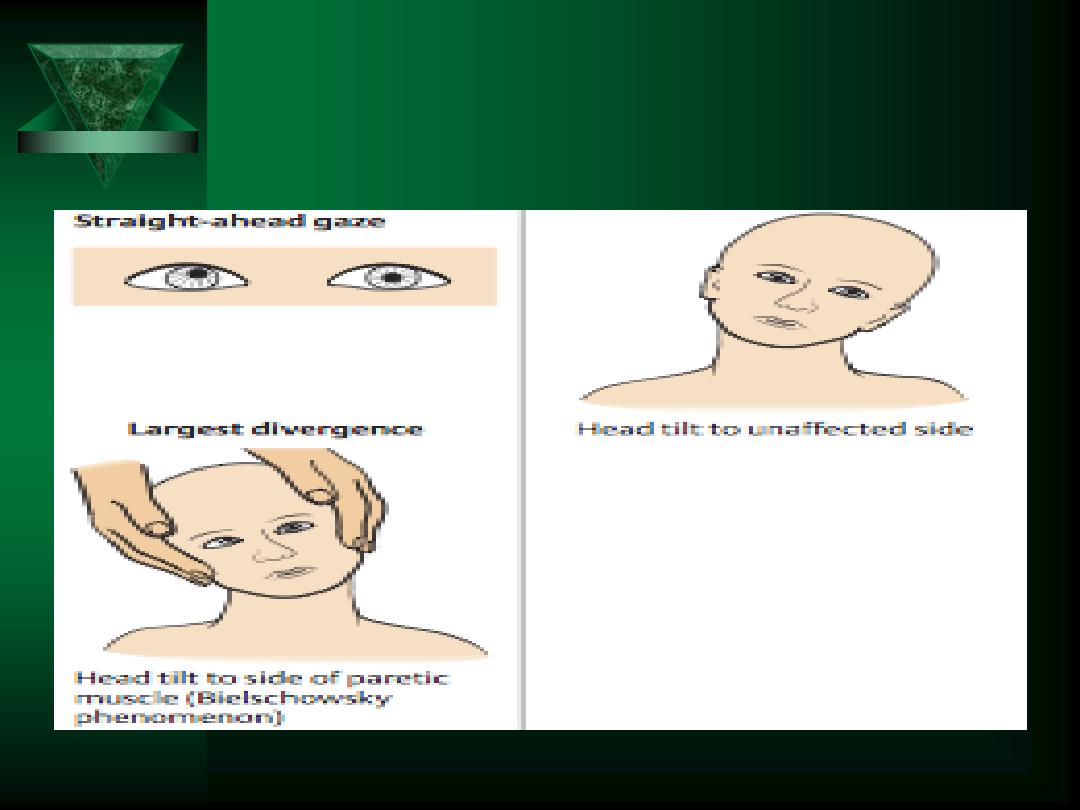
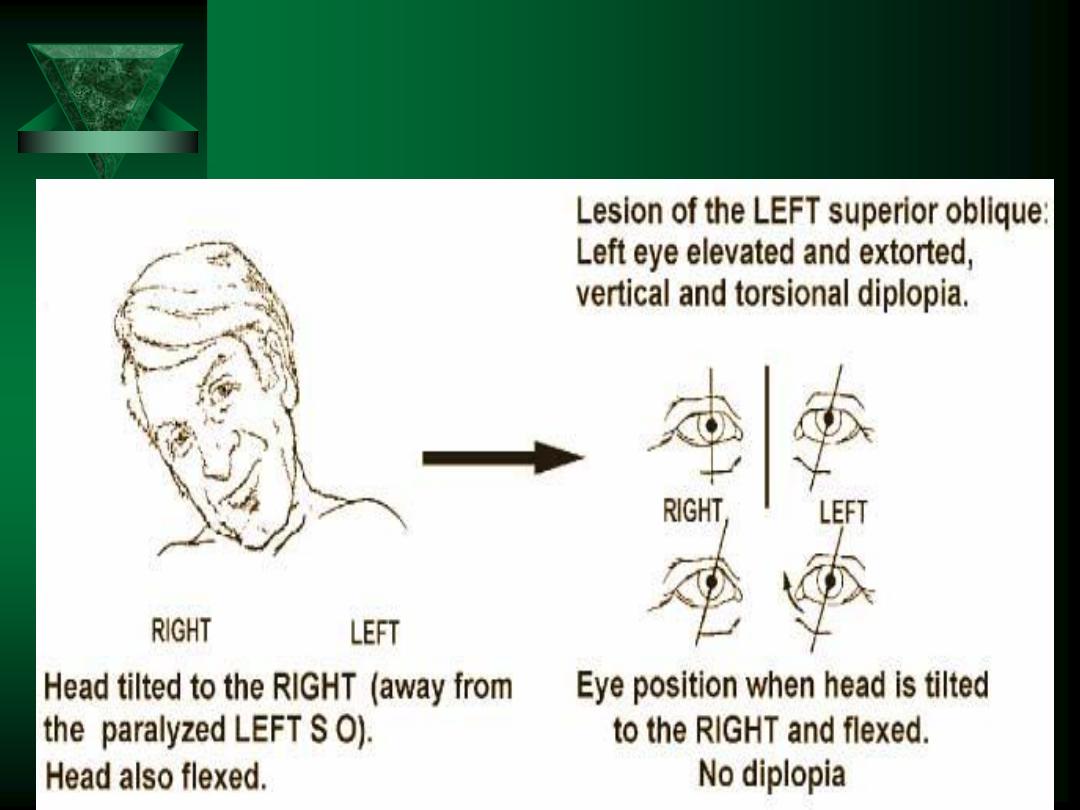
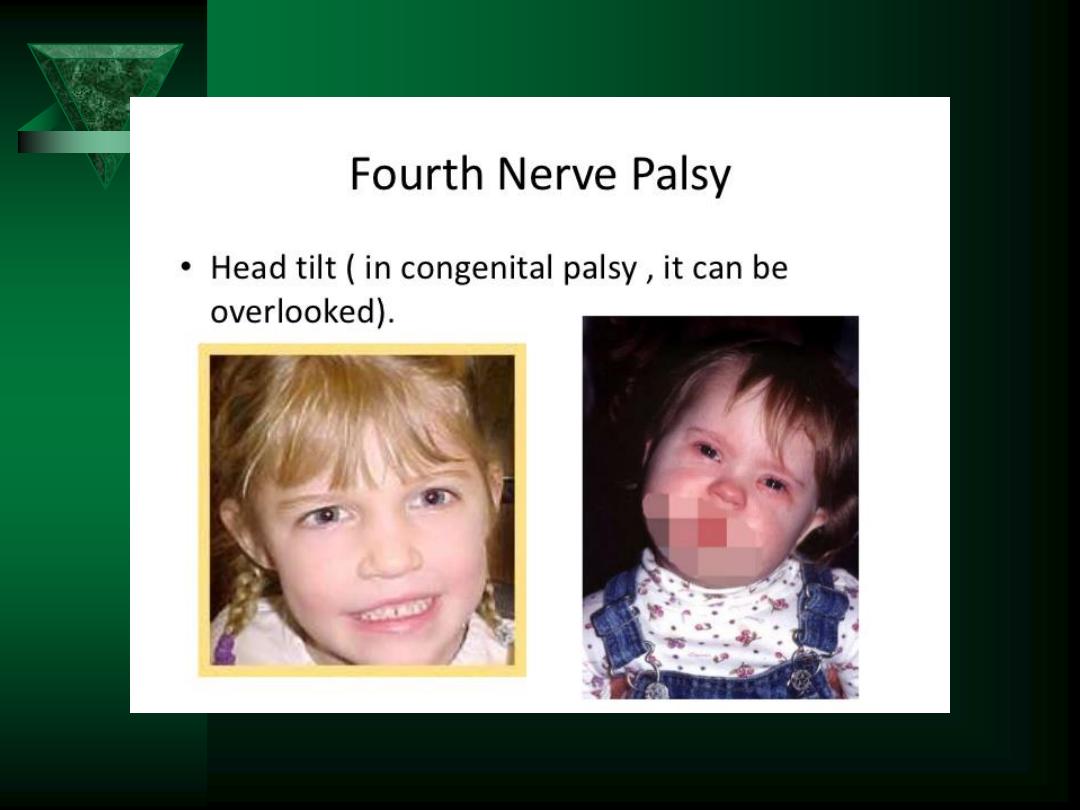
CN IV
provides downward/inward eye movement
CN VI
provides lateral eye movement


3
rd
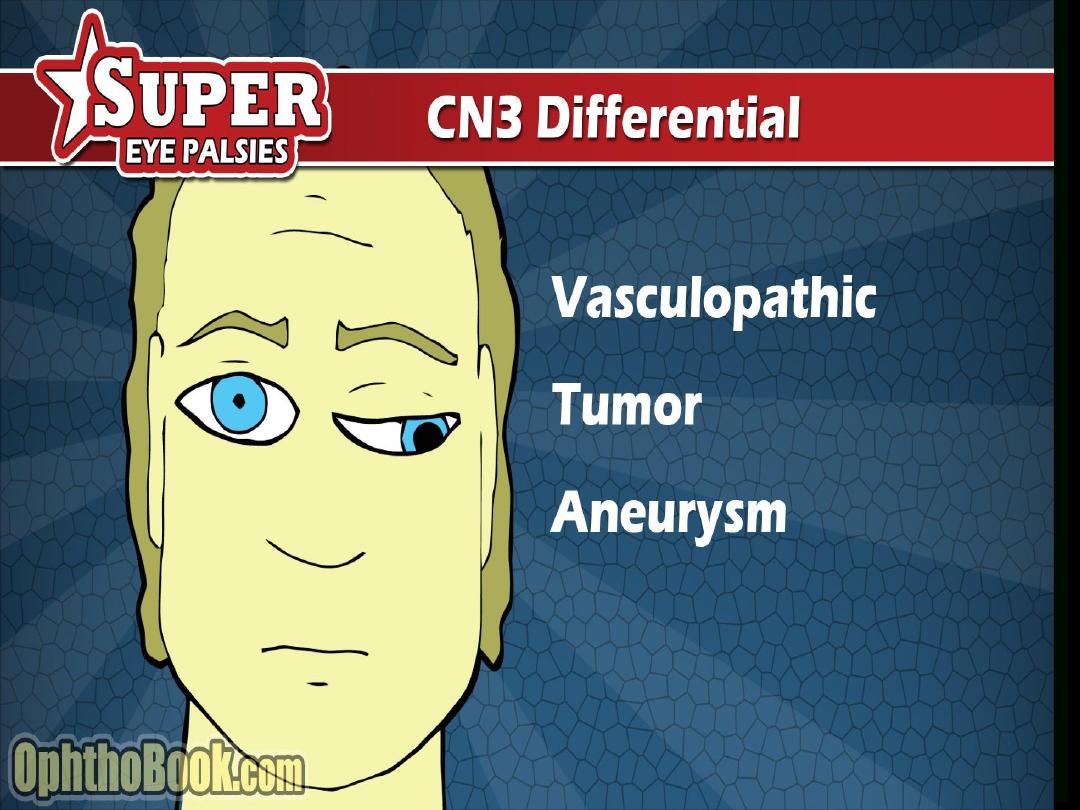
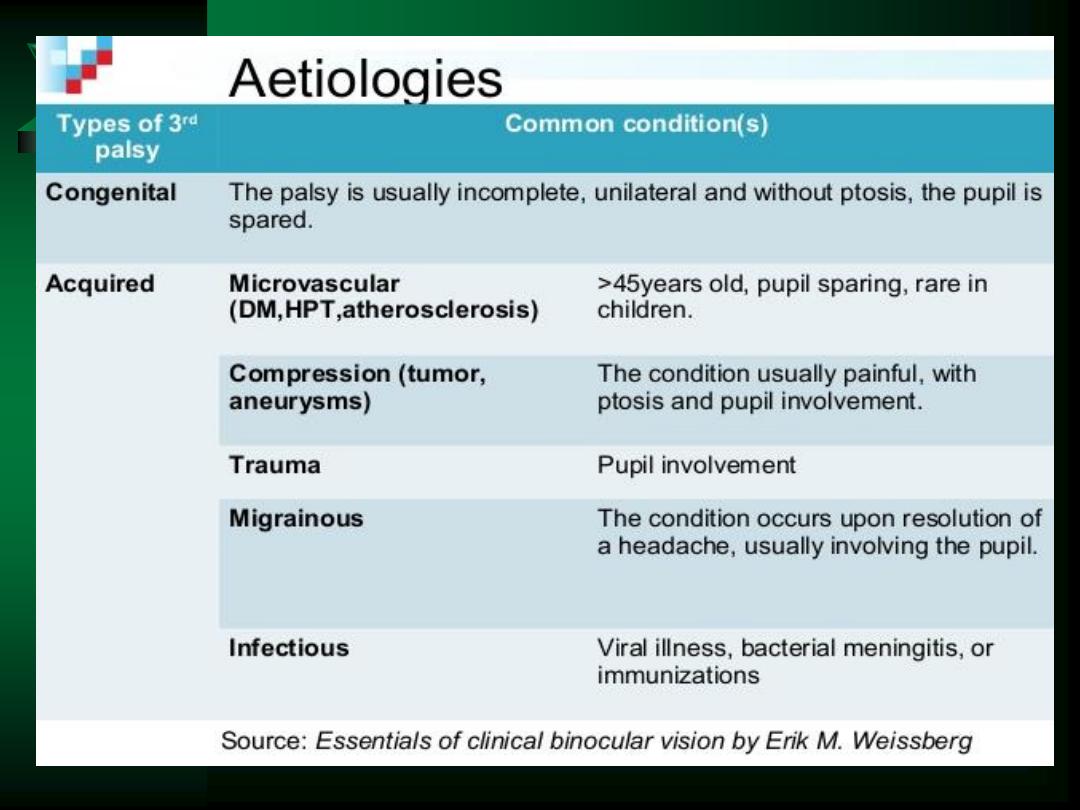
CN Palsy

3
rd
cn

3
rd
CN Palsy

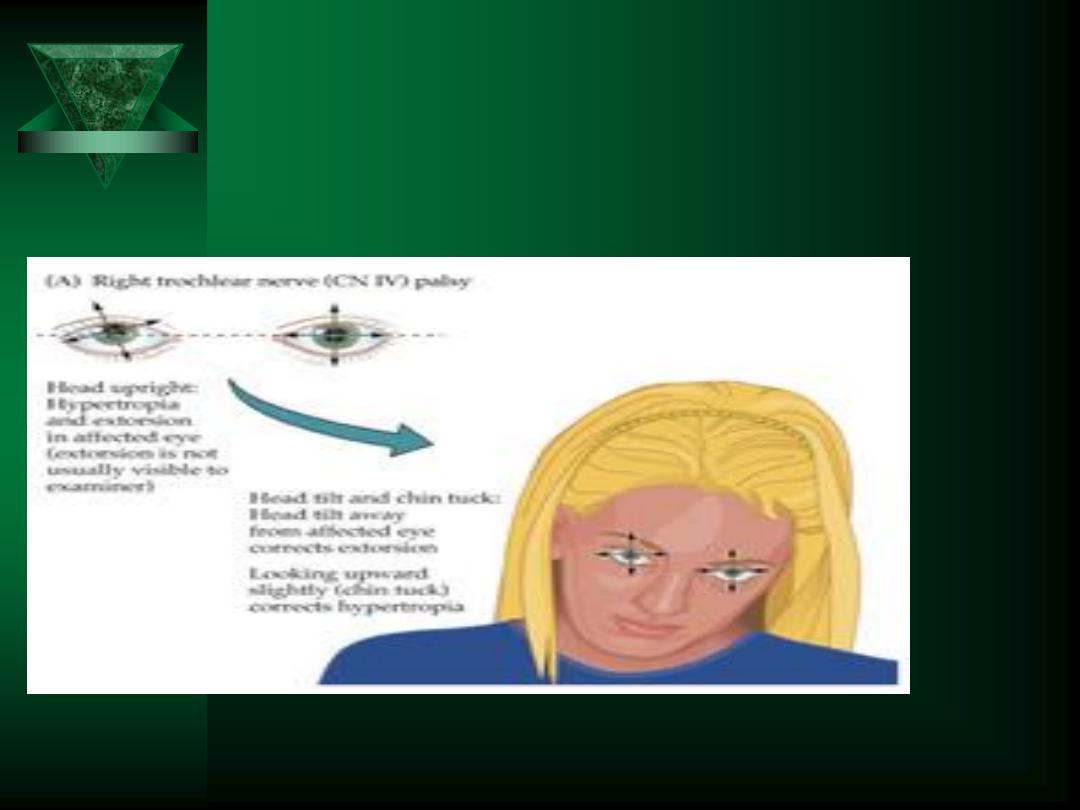
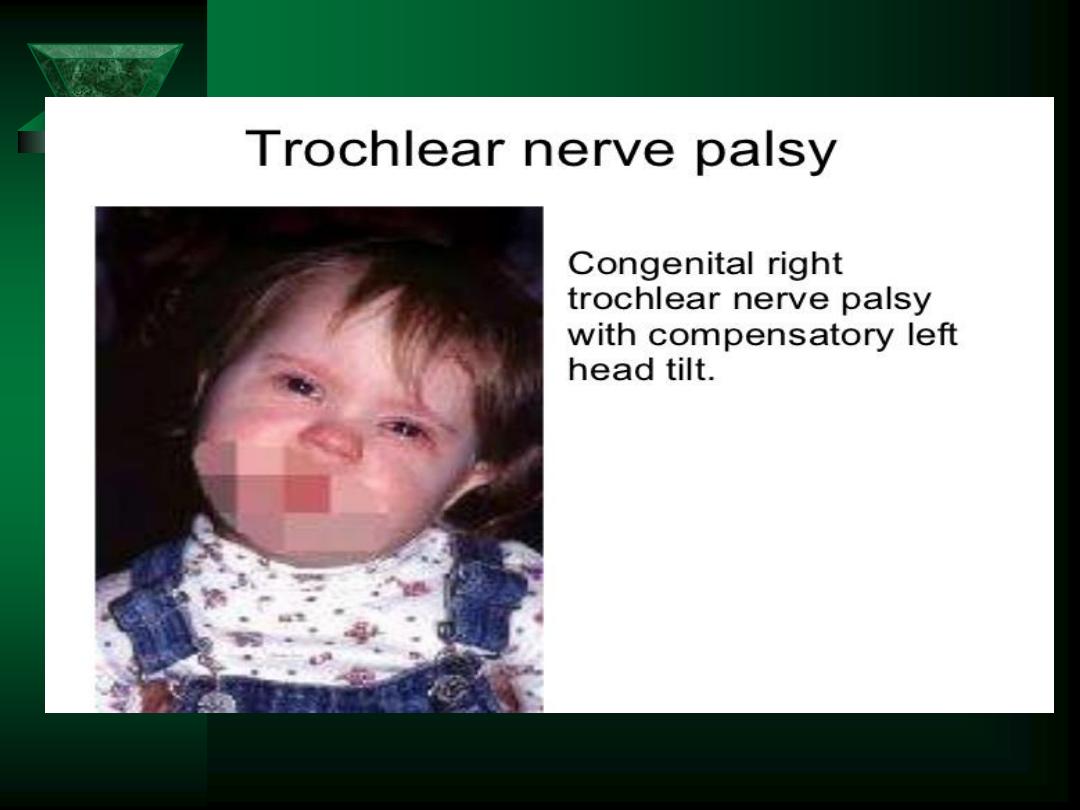
trochlear




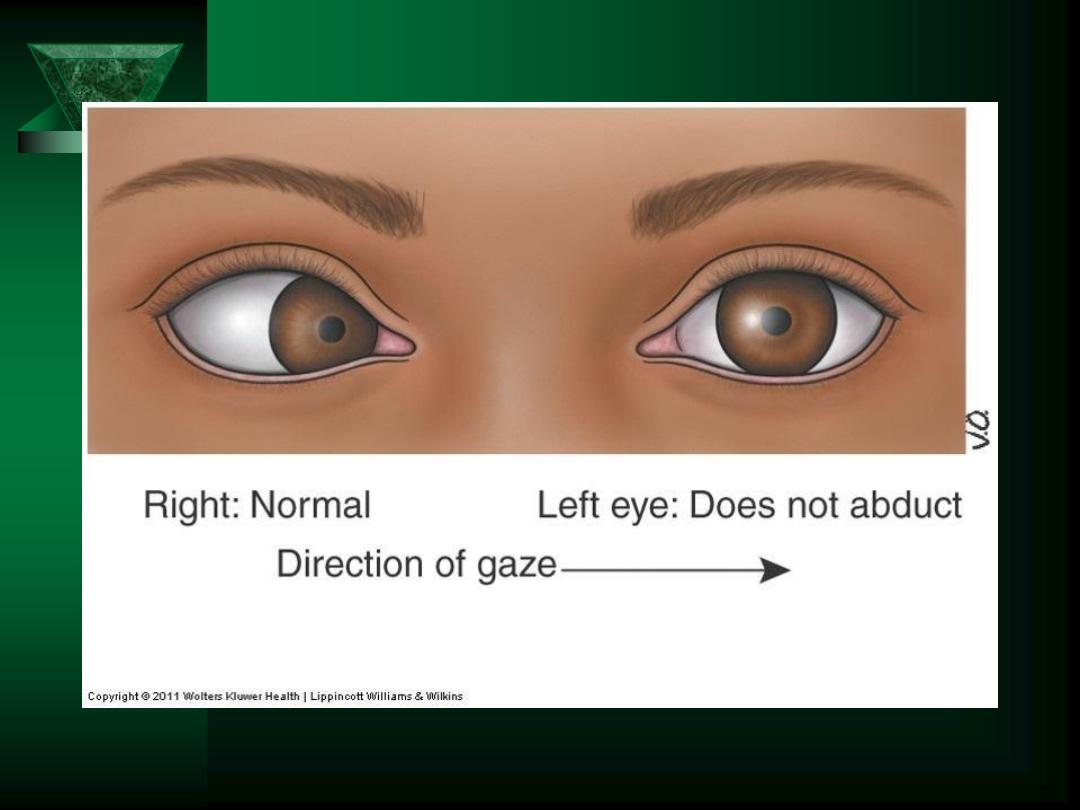
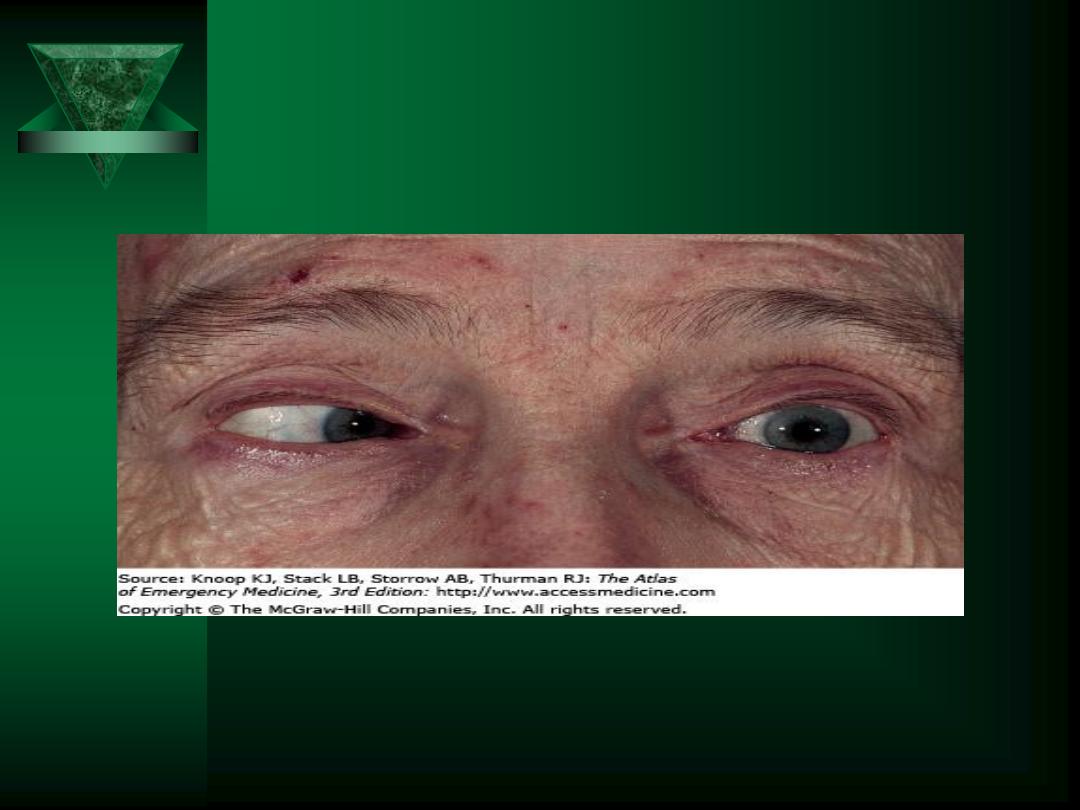
6
th
CN Palsy
6
th
CN Palsy



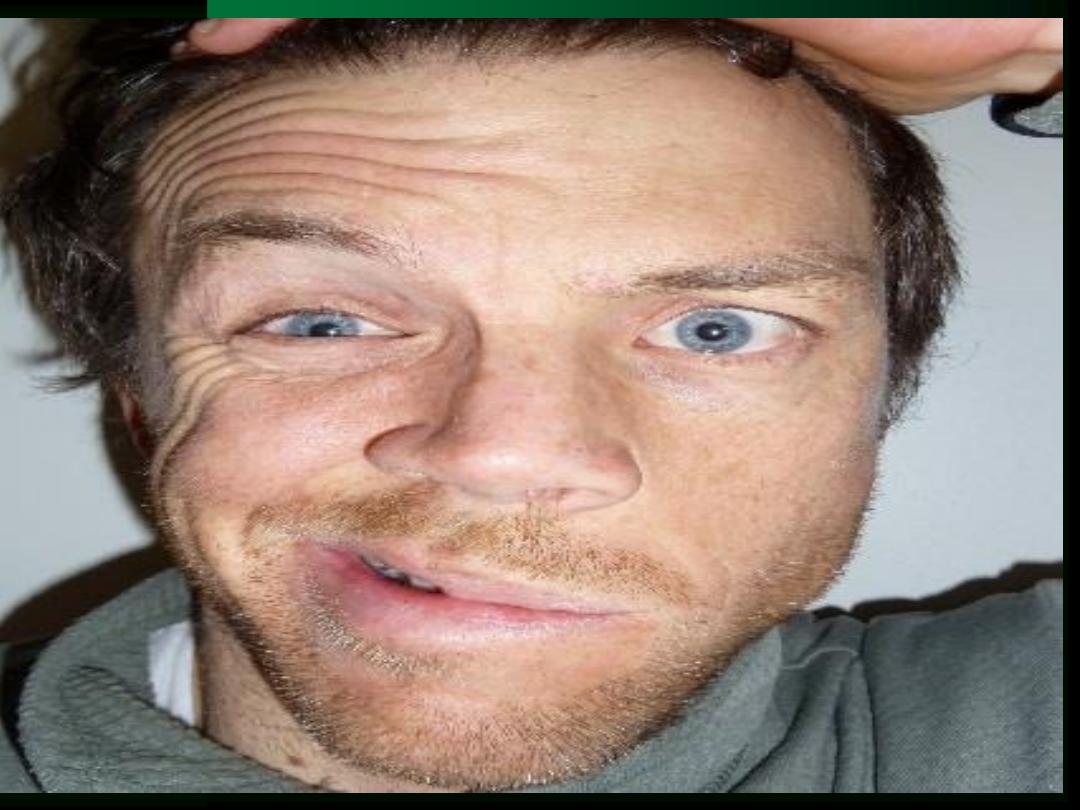




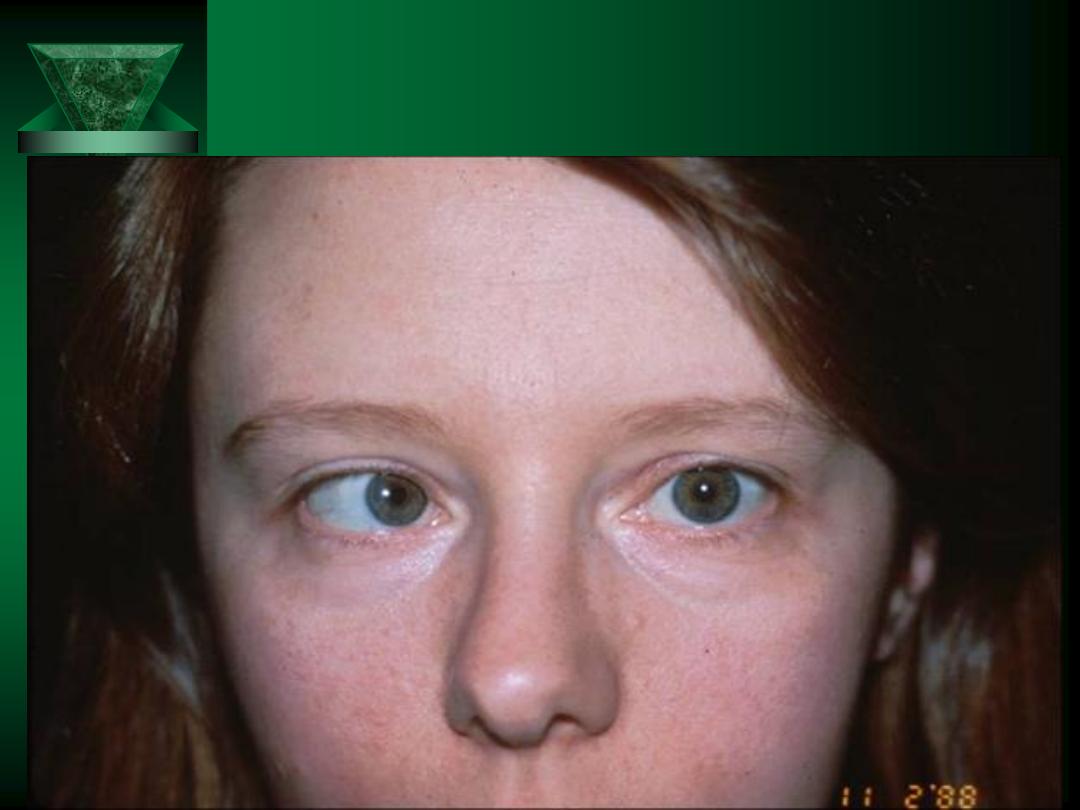
BILATERAL BELLs

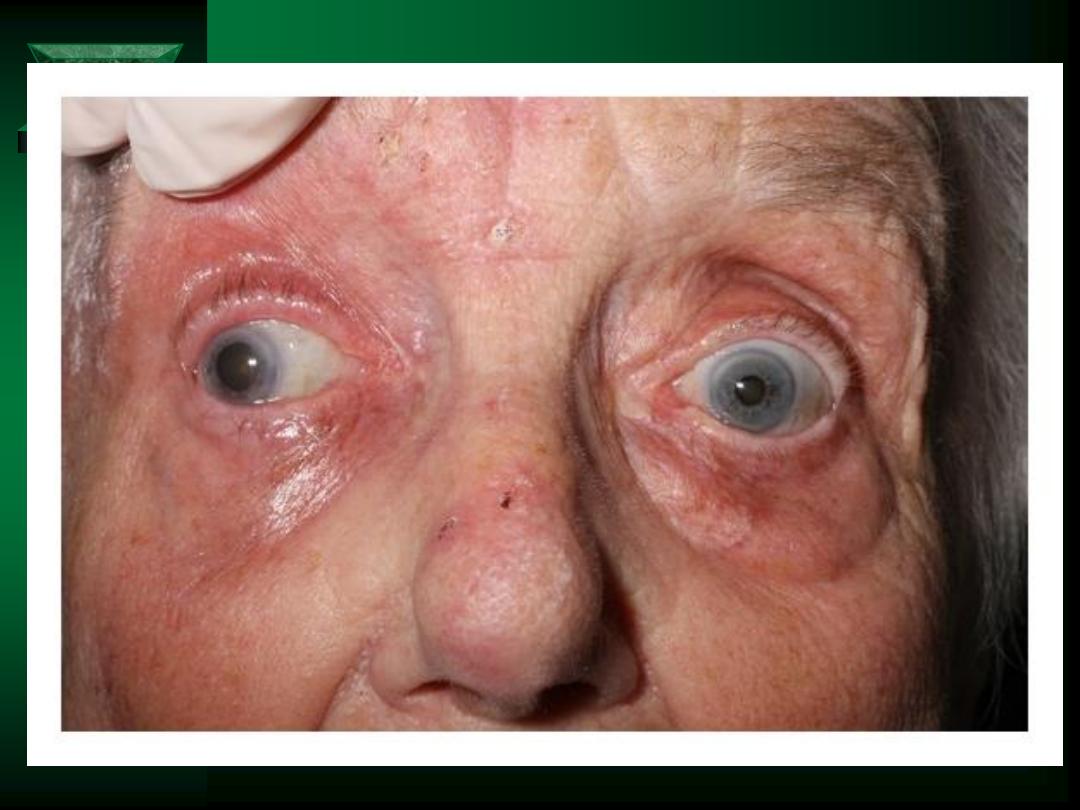
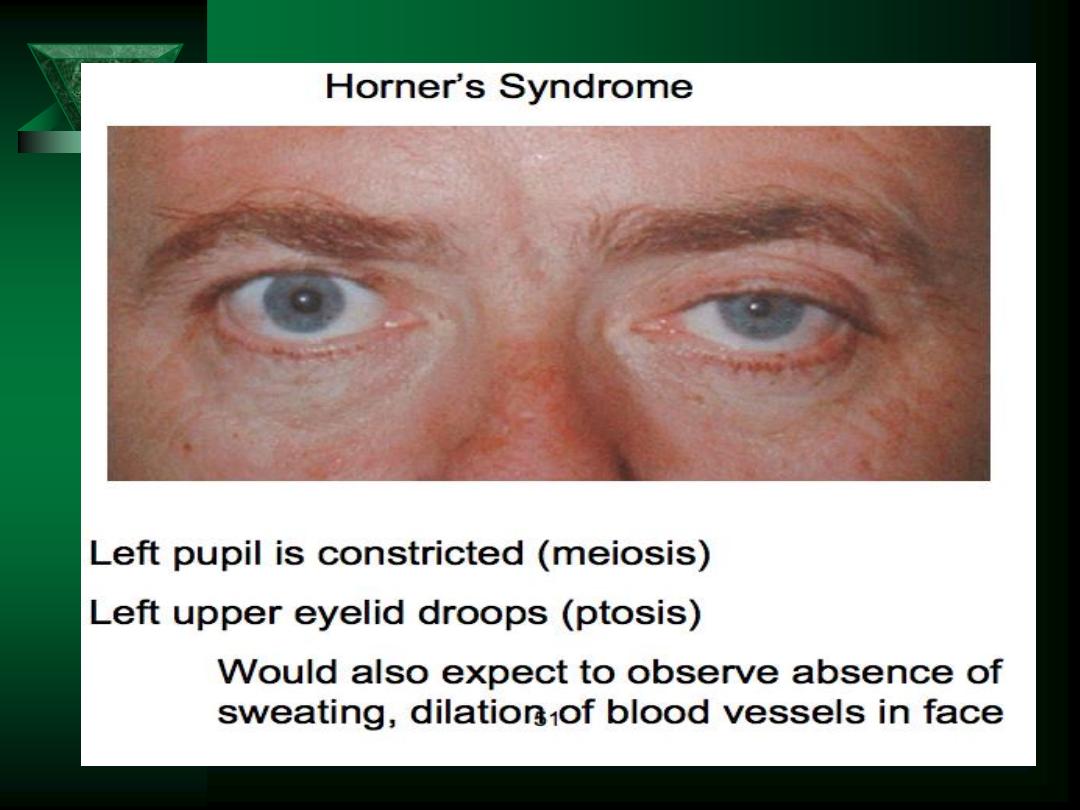
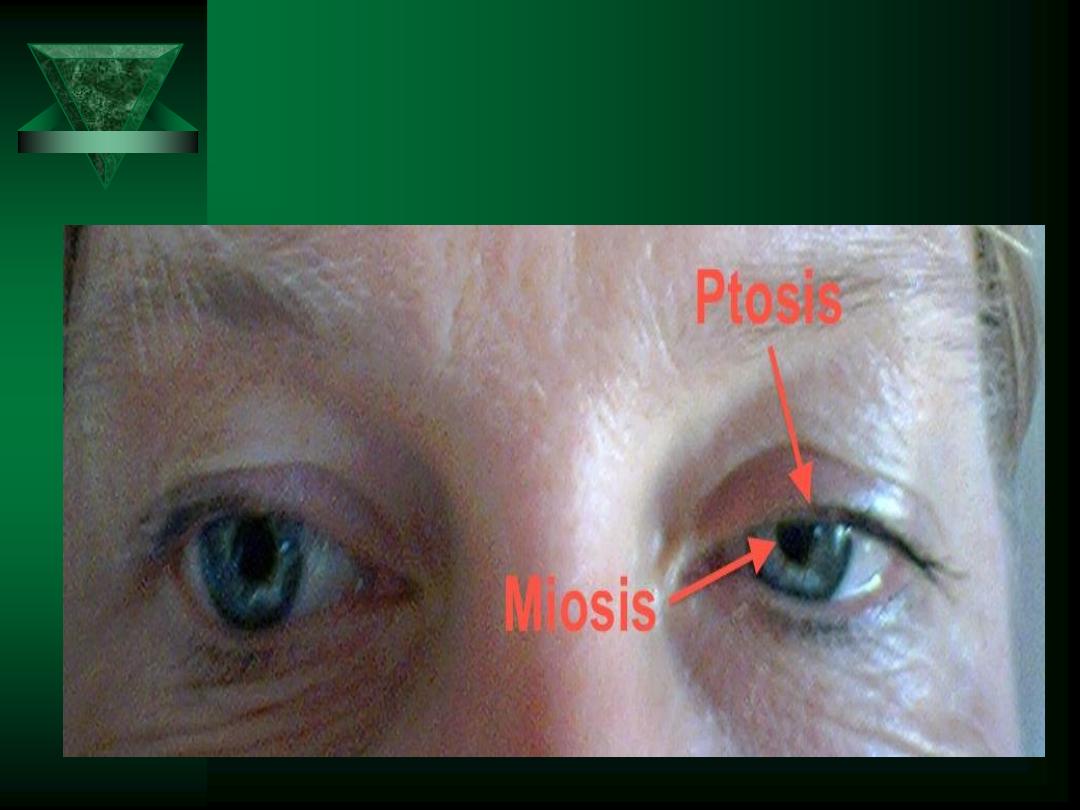
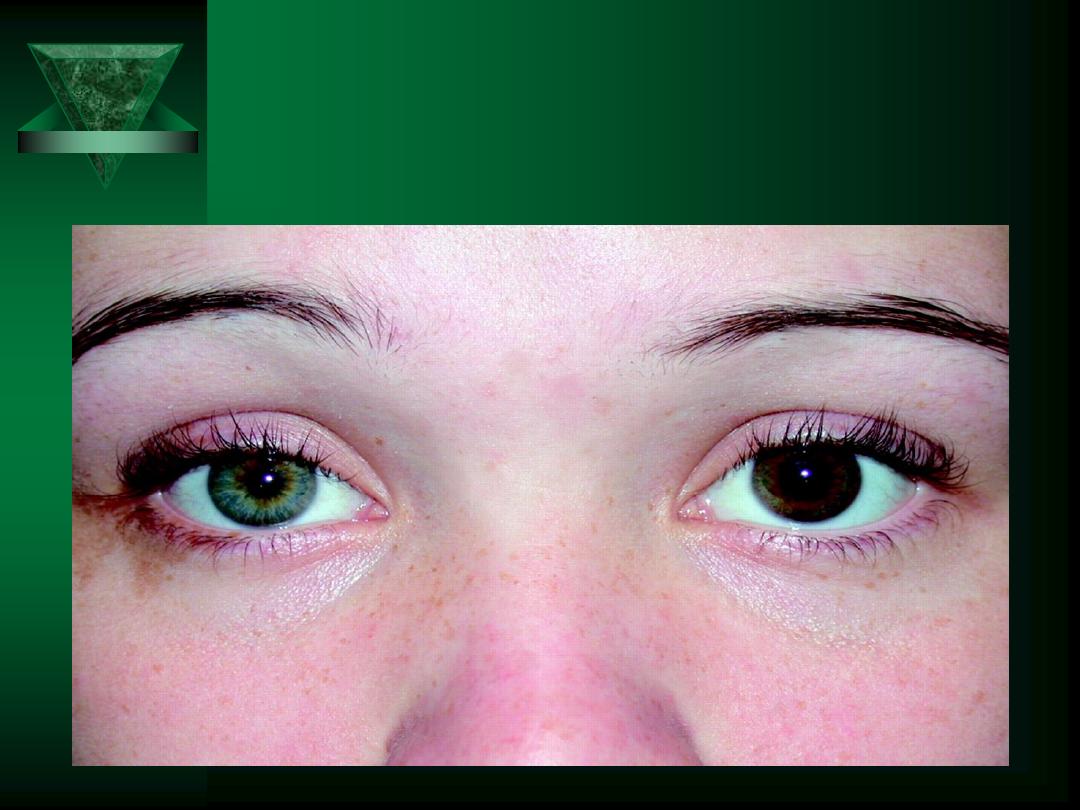
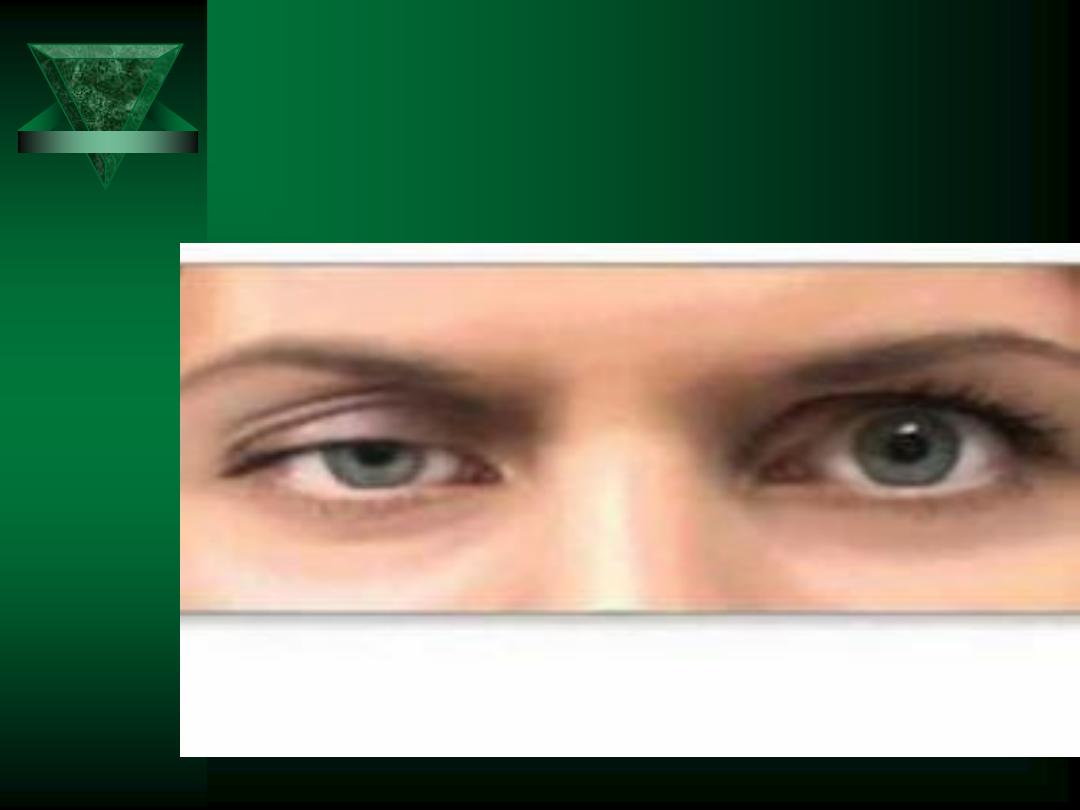
Pupil Abnormalities
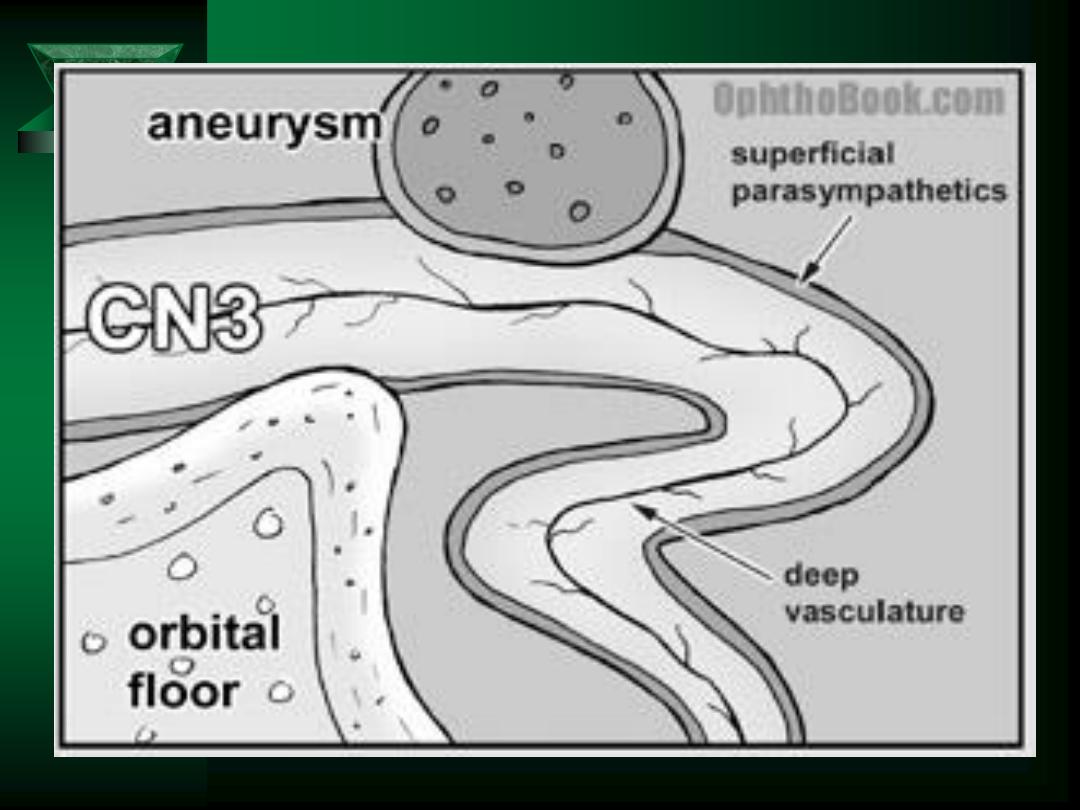
Asymmetry of pupil size of >1mm suggests CN
III compression
Bilateral dilation suggests anoxia or drug affect
Unilateral constriction is seen with sympathetic
dysfunction (Horner syndrome) or in carotid
artery dissection
Bilateral constriction is seen with:
– Pontine hemorrhage
– Drugs (opiates, Clonidine)
– Toxins (organophosphates)

Horner syndrome


Cranial Nerve V
Sensory
– Ophthalmic branch (sensory)
• Cornea, conjunctiva, ciliary body, nasal cavity, sinuses, skin of
eyebrows/forehead/nose
– Maxillary branch (sensory)
• Side of nose, lower eyelid, upper lip
– Mandibular branch (mixed)
• Sensory – skin of temporal region, auricles, lower lip/face, anterior 2/3 of
tongue, mandibular gums/teeth
• Motor - innervates the muscles of mastication
Cerebral lesion causes contralateral paresthesia
Most lesions affect all 3 branches

Varicella zoster reactivated in the
Ophthalmic branch of the 5
th
CN.

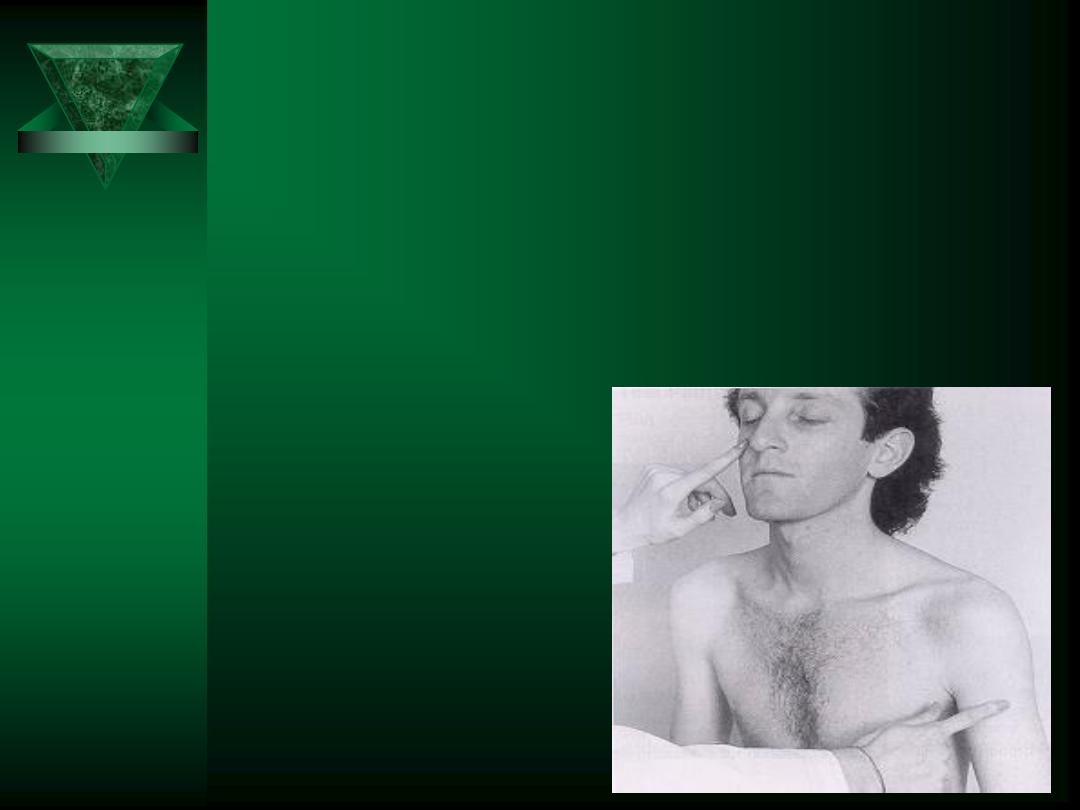
Cranial Nerve V Testing
Inspect for tremor of the lips, involuntary
chewing movements, and trismus
Compare muscle tension bilaterally with
teeth clenched
Test tactile perception
Test sharp-dull discrimination
Test temperature perception
Test corneal reflex
– Tests V & VII directly and VII consensually

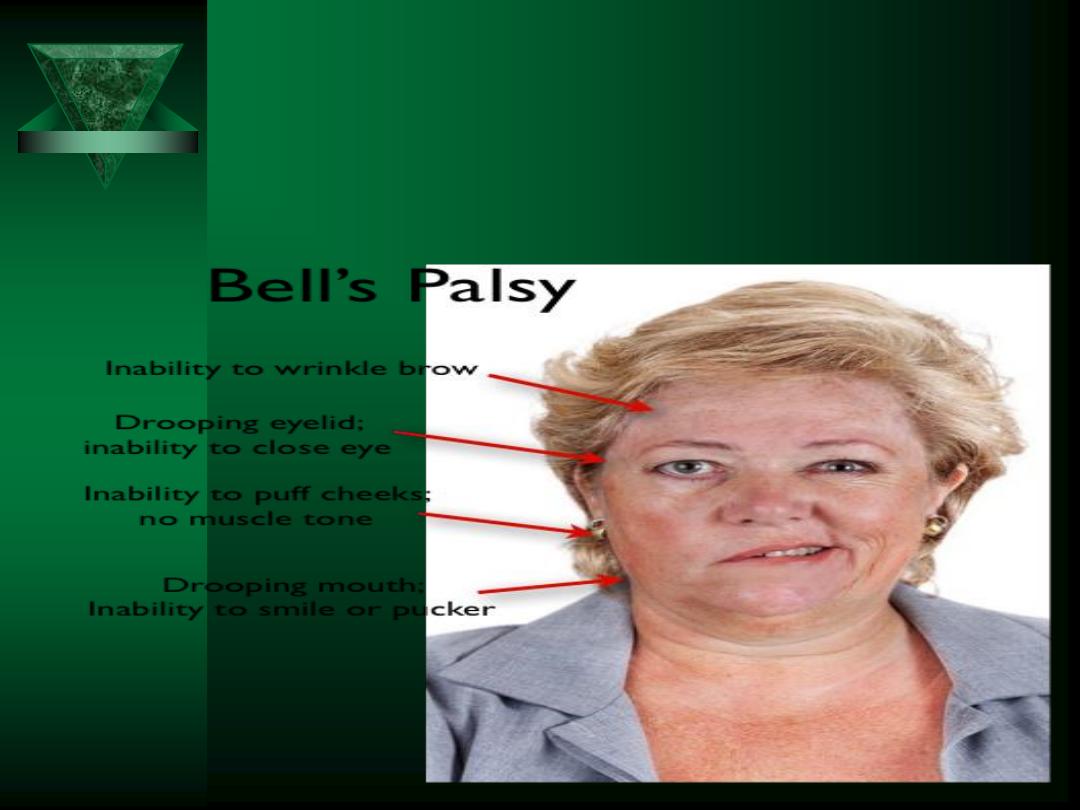
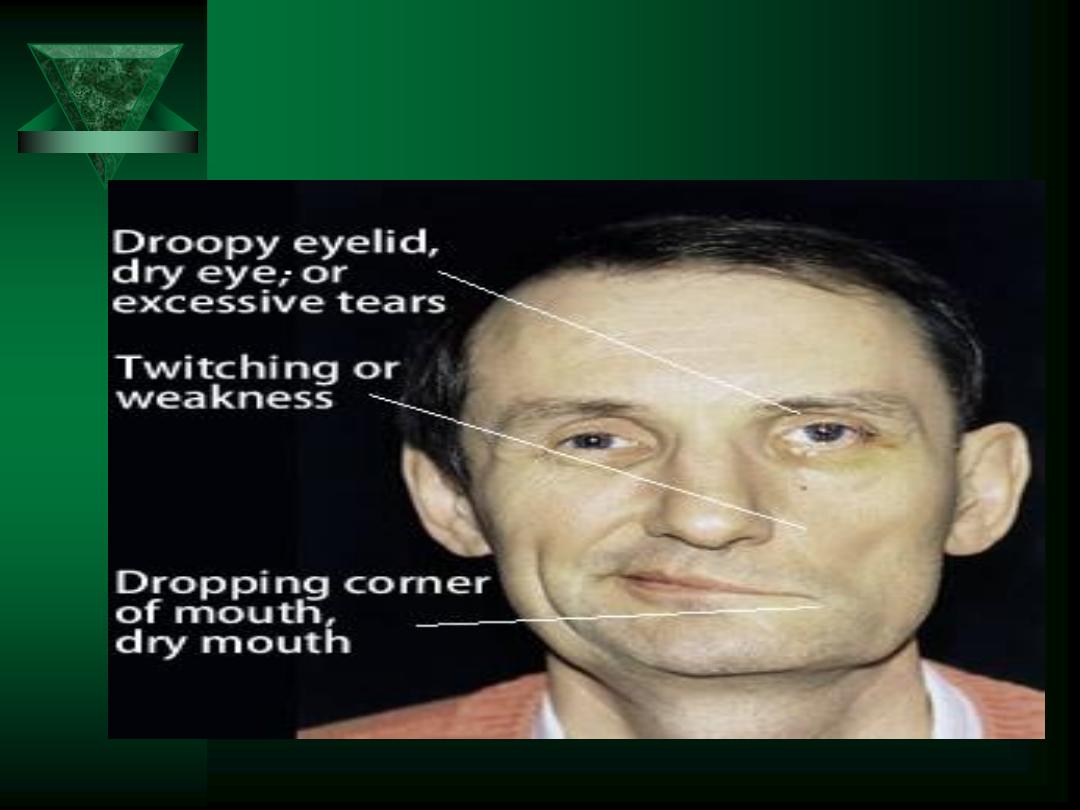
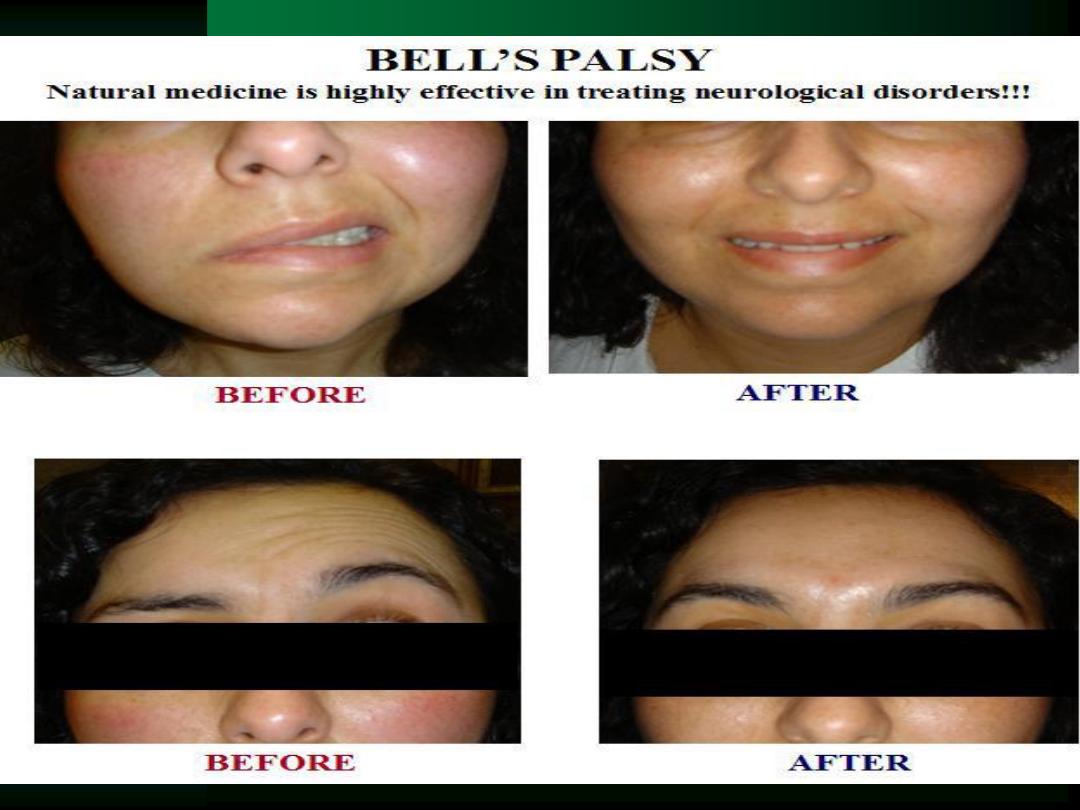
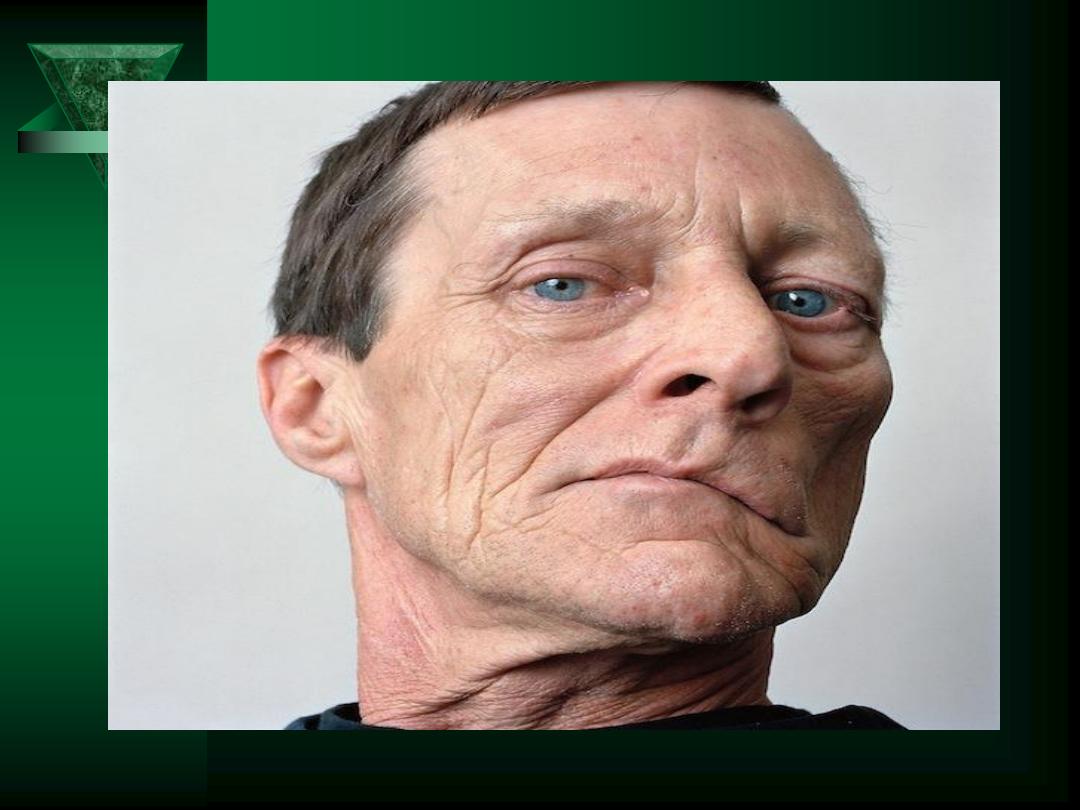
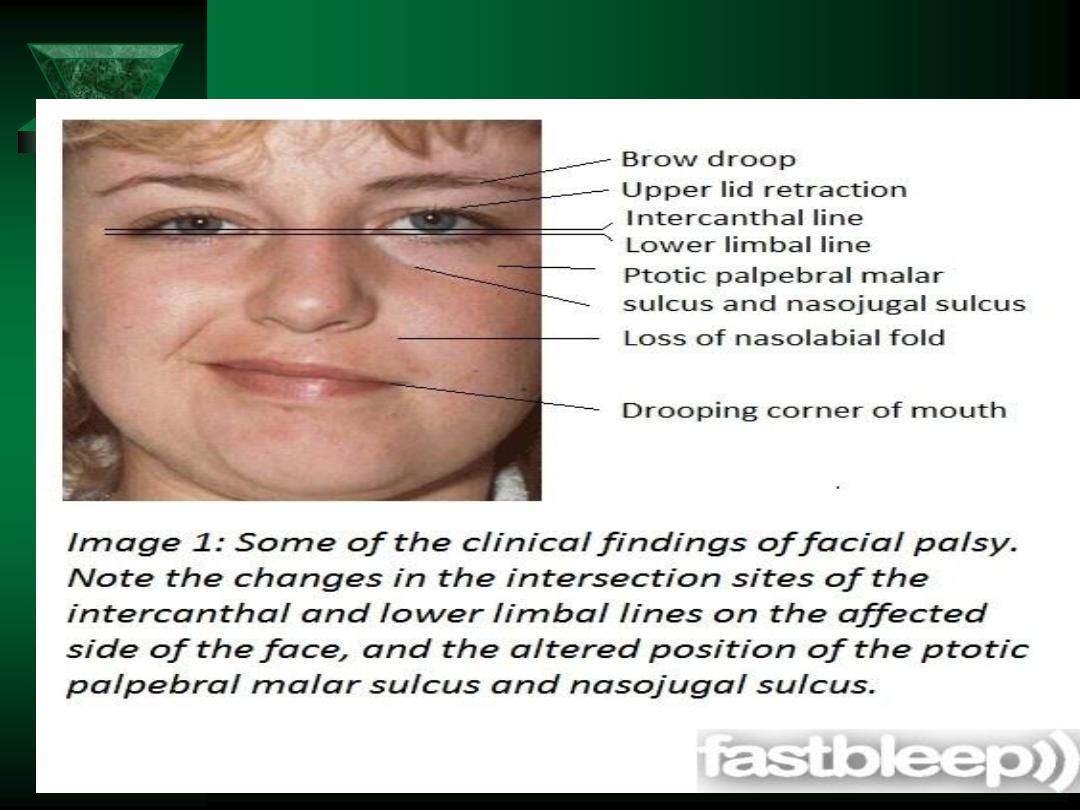
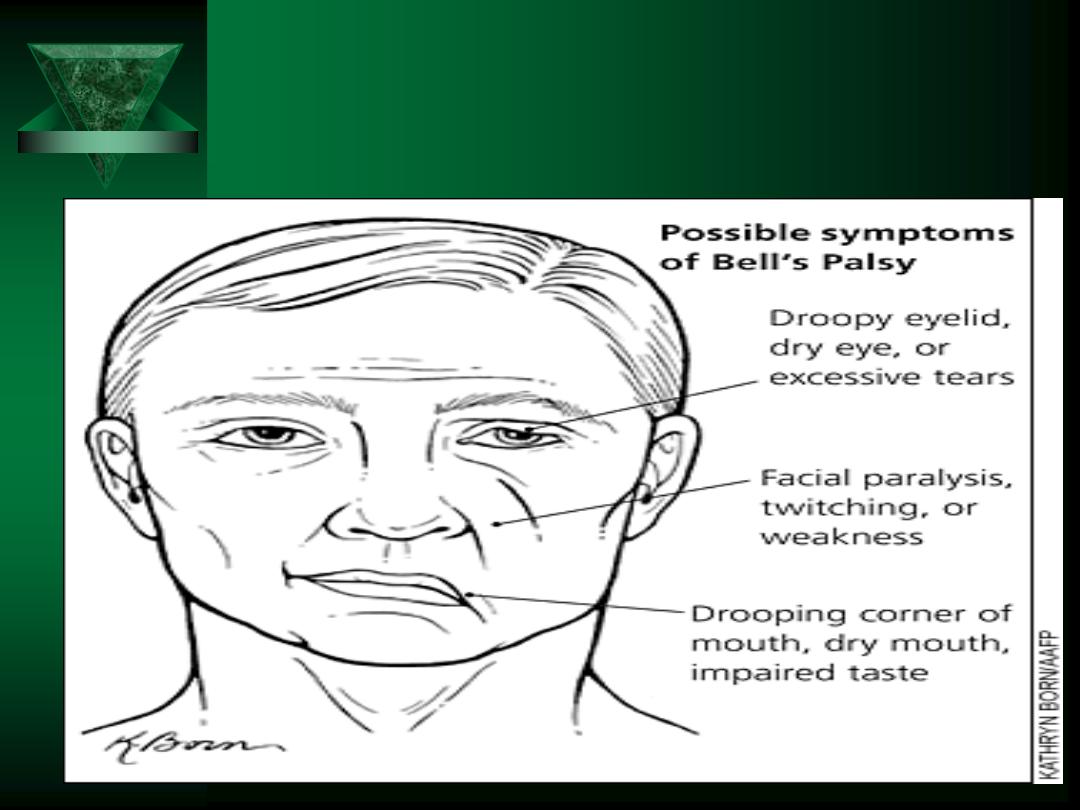
Cranial Nerve VII
Motor
– Muscles of the face, scalp, and ears
Autonomic
– Vasodilation
– Secretion of submaxillary/sublingual glands
Sensory
– Taste in anterior 2/3 of tongue
– Ear canal/postauricular
Palsies can occur secondary to:
– Polio, ALS, MS, tumors, syphilis, Lyme disease,
Guillain-Barré Syndrome

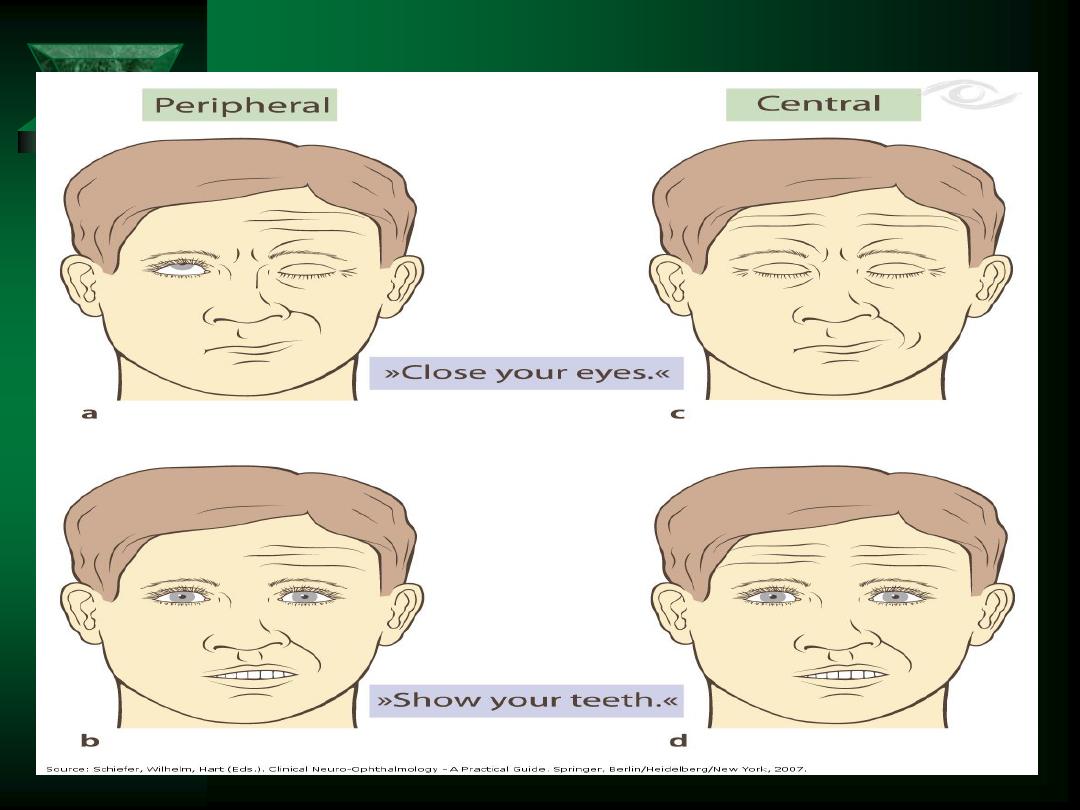
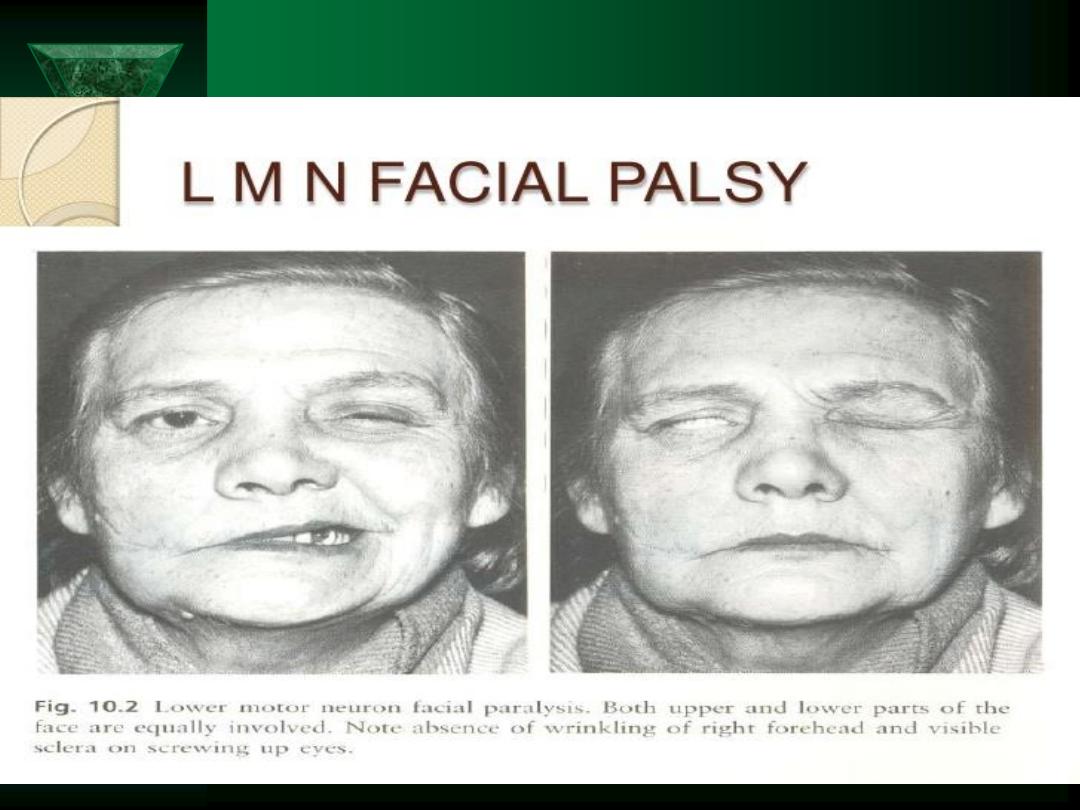
Cranial Nerve VII
Inspect for flaccid paralysis
Differentiate UMN vs. LMN
– Elevate eyebrows
– Close eyes
– Show teeth
– Whistle
– Smile
**Central lesions causes contralateral
paralysis to lower half of face (below the
eyes)

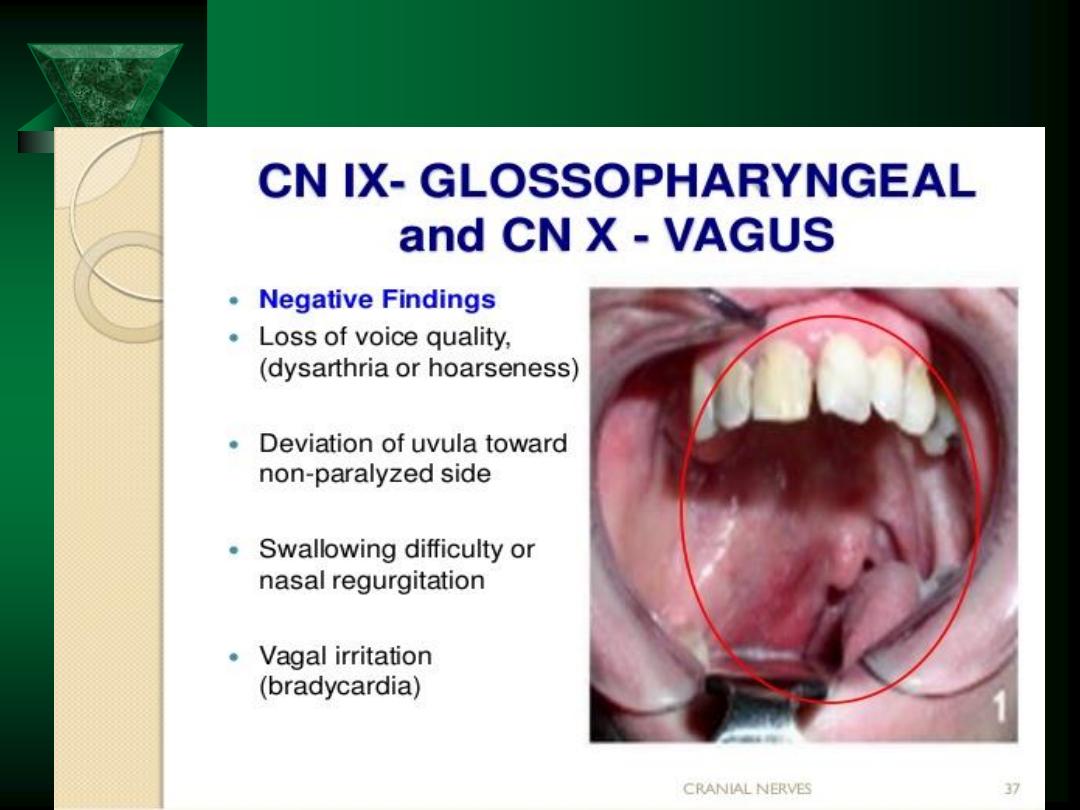
Cranial Nerve IX
Motor
– Muscles of the pharynx
Autonomic
– Vasodilation
Sensory
– Taste in posterior 1/3 of tongue
– Pharynx, tonsils, fauces, TM, posterior ear canal
Test for
– Elevation of the uvula
– Gag reflex
– Mucosal anesthesia

Motor, autonomic, and sensory functions
Palate, pharynx, larynx, neck, thorax, and abdomen
Branches to:
Pharynx
Larynx
Esophagus
Heart
Bronchioles
Stomach
Liver
Celiac
Perform indirect examination of the vocal cords
Lesion causes
:
Hoarseness/aphonia
Dyspnea/stridor
Cranial Nerve X

Cranial Nerve XI
Provides motor to
– SCM
– upper Trapezius
Testing:
– Have patient shrug against resistance
– Head rotation and movement against resistance
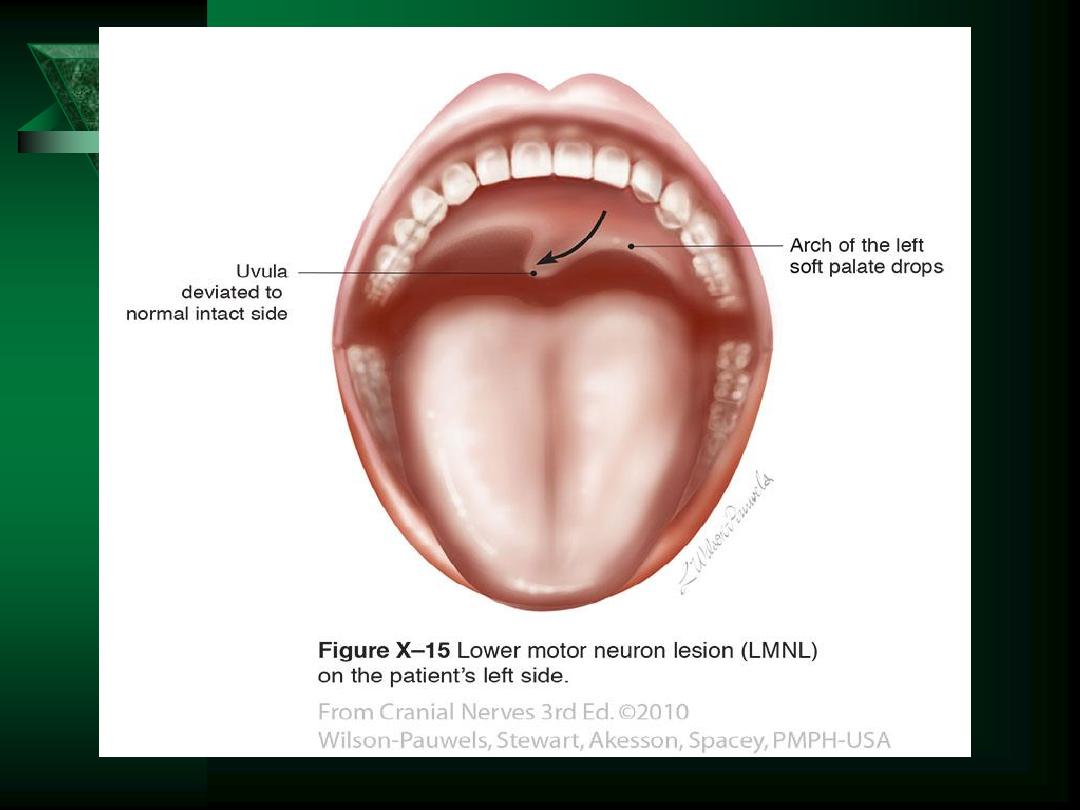

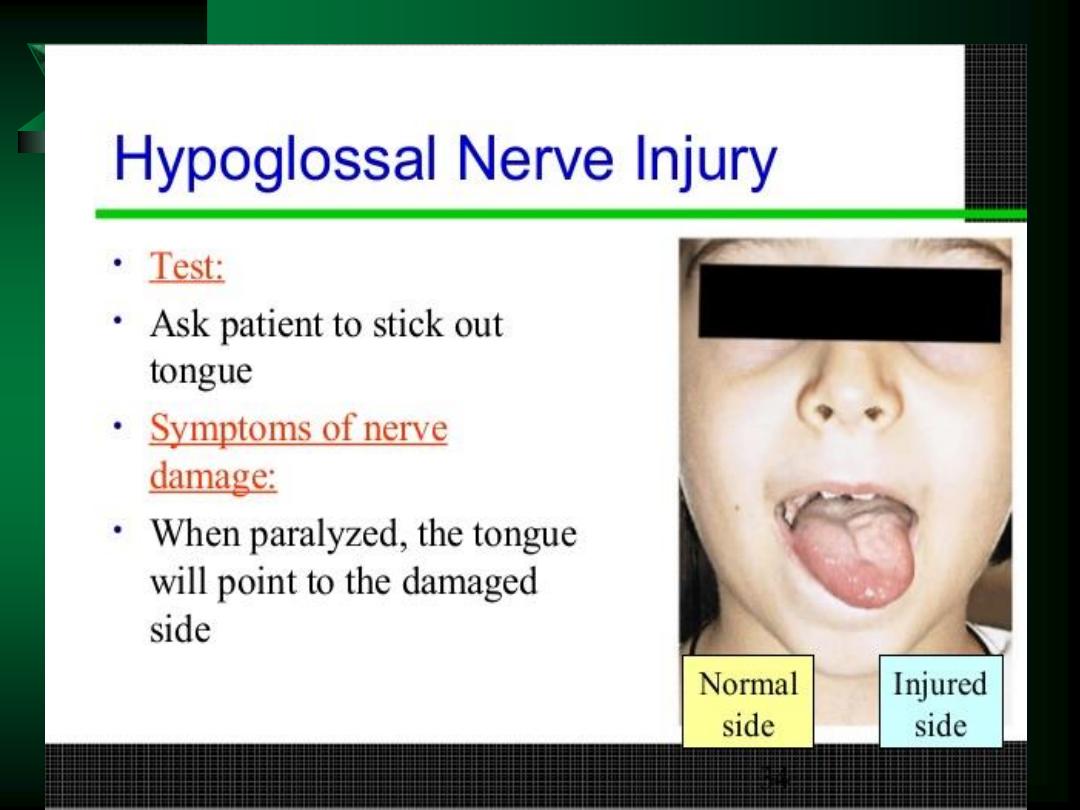
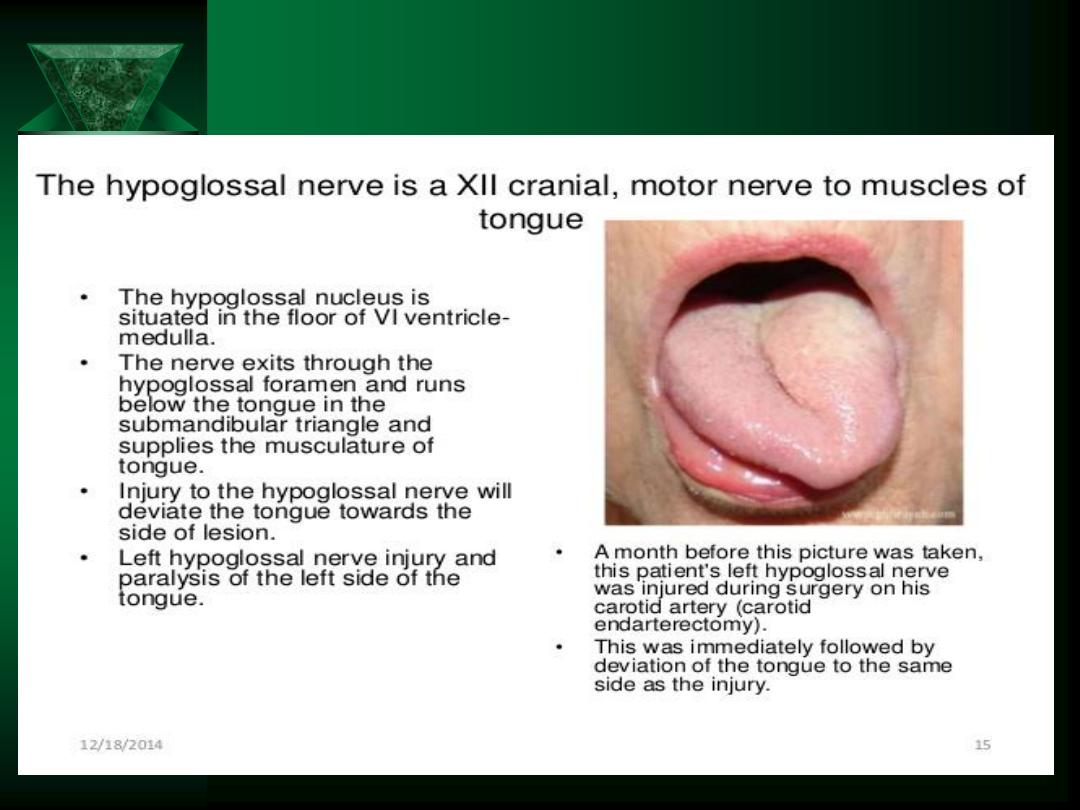
Cranial Nerve XII
Motor to tongue
Testing:
– Tongue movement
• Midline
• Tremors
• Involuntary
– Atrophy
– Lingual speech
Paralysis causes deviation to the weak side
1
Up-to-Date

Deviation to the affected side,wasting, and
fasciculations.

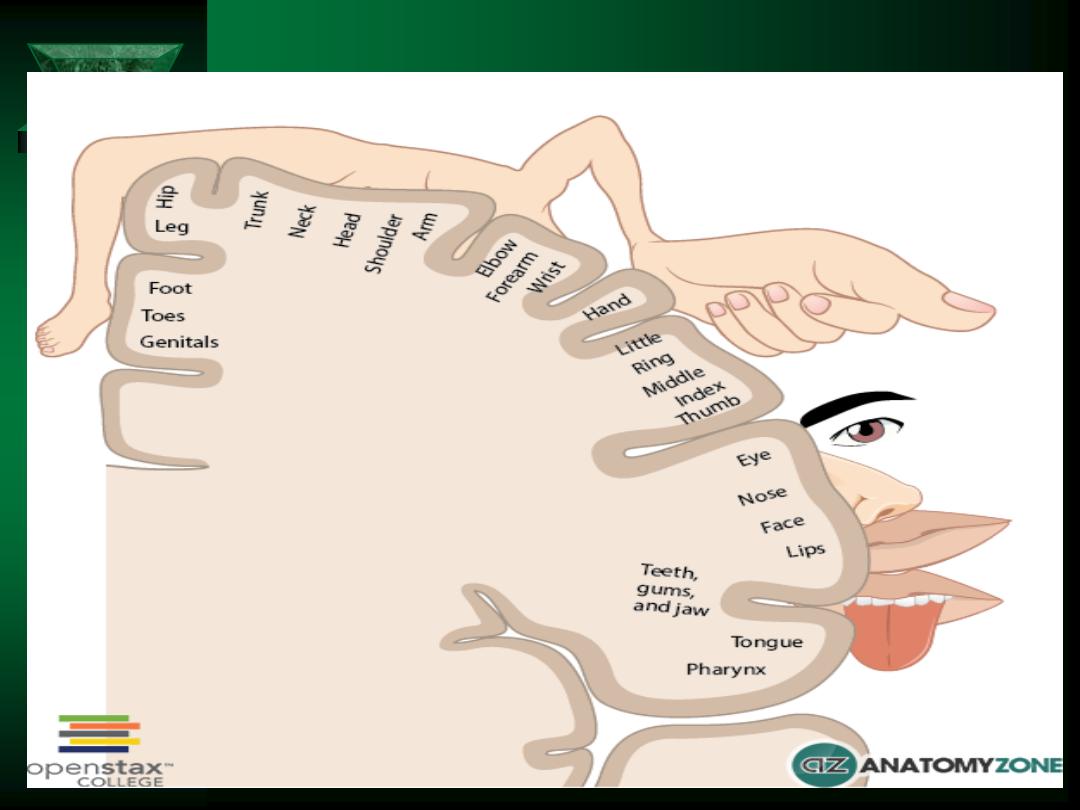
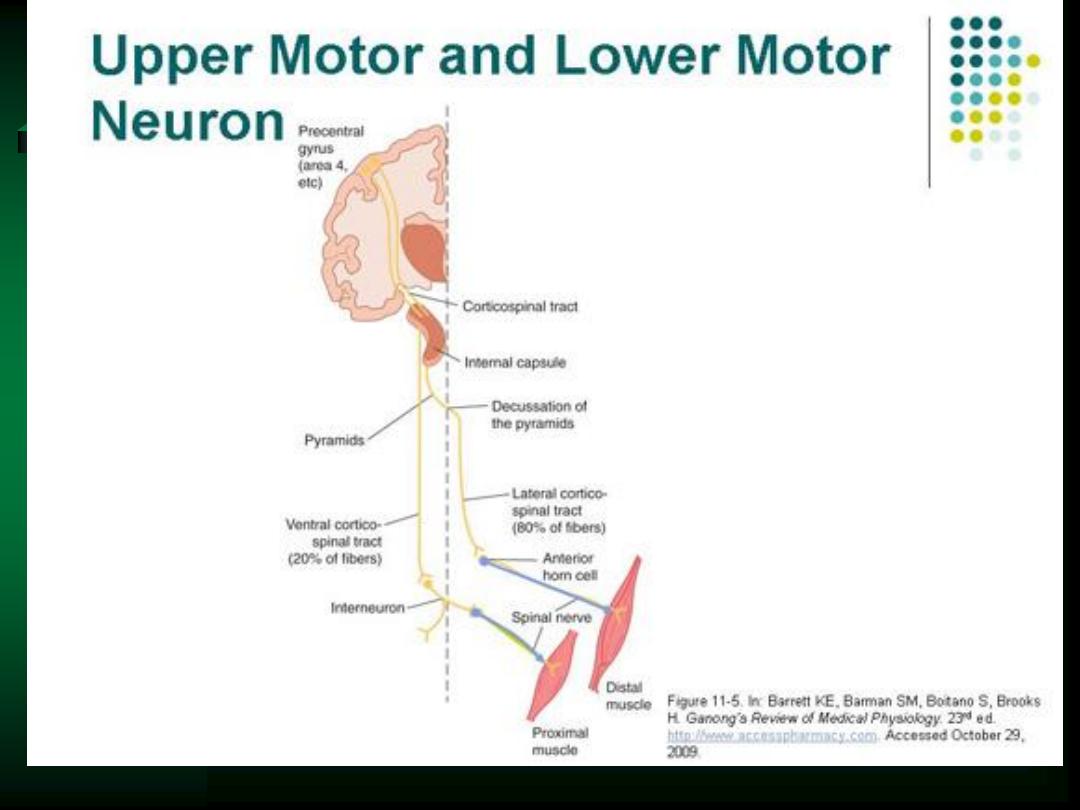
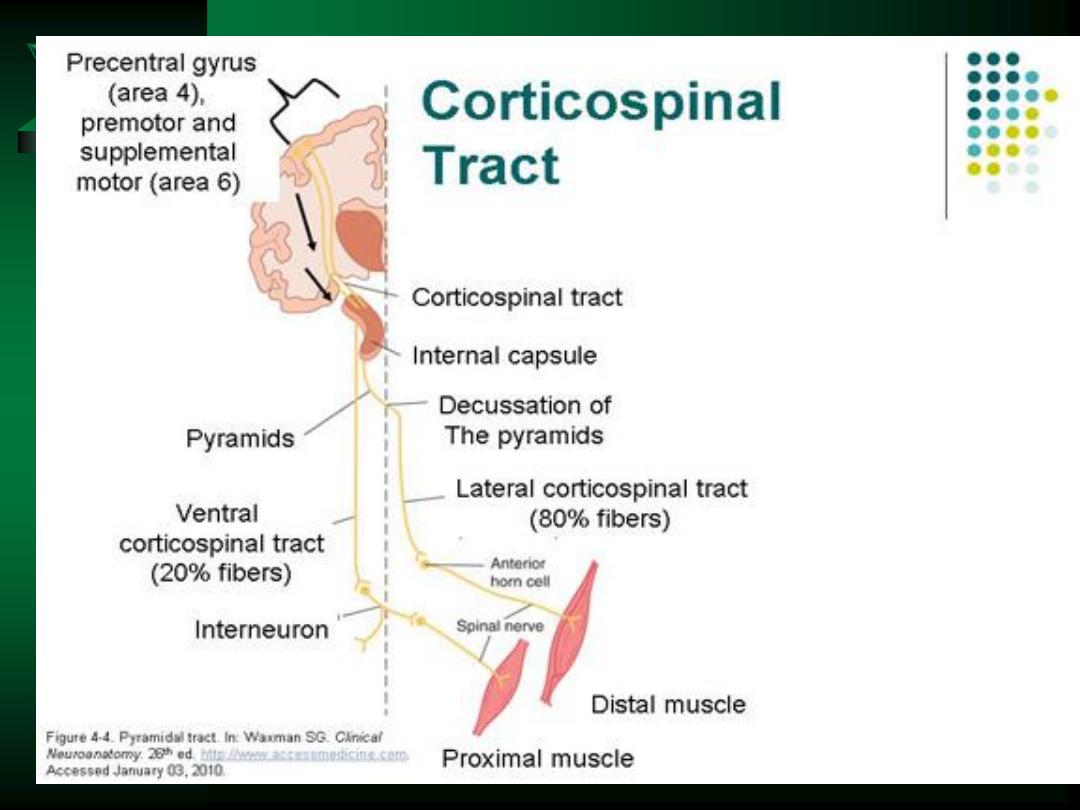
Motor Function
UMNs
– Transmit impulses from cortical nerve bodies to:
• motor nuclei in brainstem (CNs)
• Anterior horn cells of spinal cord
LMNs
– Transmit impulses from anterior horn cells through
anterior root into peripheral nerves
– Terminate at the neuromuscular junction

Motor Function
Inspection
Symmetry
Muscle bulk; size and contours; flat or concave; unilateral or bilateral; proximal
or distal
Atrophy
Palpation
Muscle tone
Percussion
Fasciculations
Check motor strength
Body position (during movement and at rest)
Involuntary movements
Location, quality, rate, rhythm, amplitude and relation to posture, activity,
fatigue, or emotions
If an abnormality exists:
Identify muscle(s) involved
Central vs. peripheral?
Learn muscle innervations

Motor Function
Muscle tone
– Slight residual tension in normal relaxed muscle
– Feel muscle’s resistance to passive stretch
Muscle strength
– Wide variance - stronger dominant side
– Test by asking patient to actively resist movement
– If muscles too weak - test against gravity only or eliminate
gravity
– If patient fails to move, watch or feel for weak contraction
Suspect decreased resistance?
– Hold forearm and shake hand loosely
Resistance increased?
– Varies or persists throughout movement
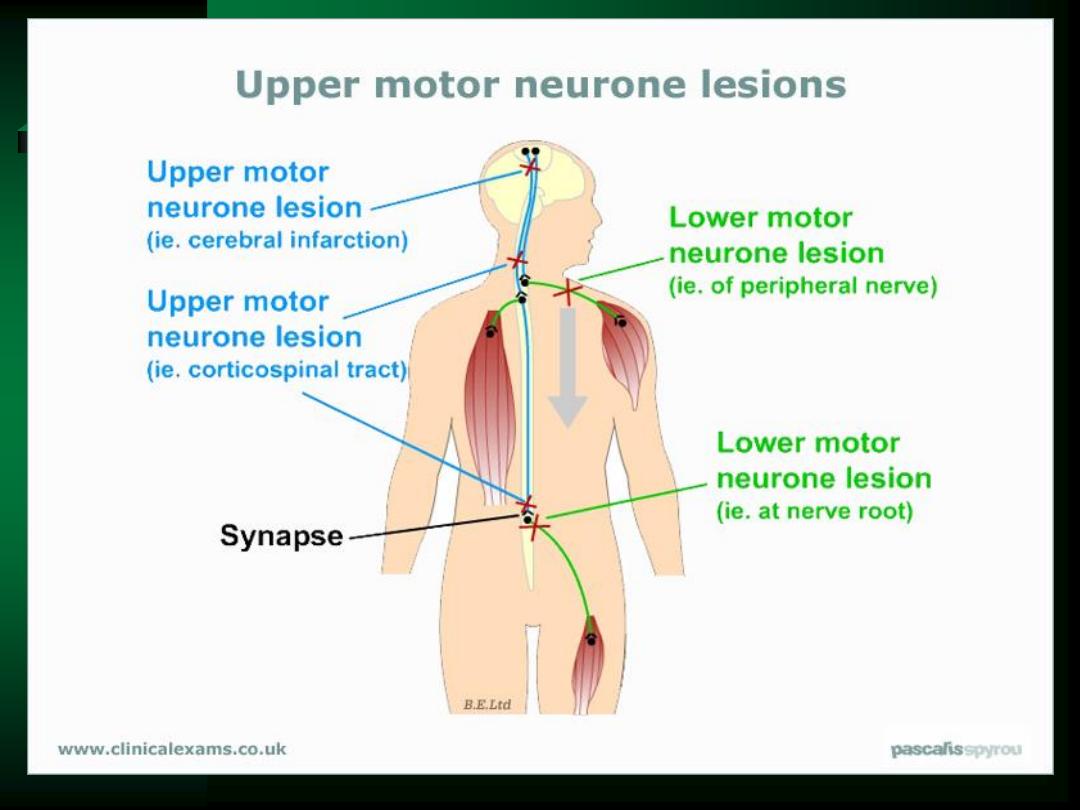

Motor Function
Always compare symmetry
Note any atrophy
Check muscle tone against resistance
– Cogwheel rigidity = jerky, released in degrees
– UMN paralysis = spasticity (increased tone)
– LMN paralysis = hypotonia
Test muscle strength
– Grade 0 to 5
Grading Muscular Response
Grade
Muscular Response
0
No contraction detected
1
Barely detectable flicker or trace of contraction
2
Active movement with gravity eliminated
3
Active movement against gravity
4
Active movement against gravity and some
resistance
5
Active movement against resistance without
evident fatigue -
“Normal”

BILATERAL CARPAL TUNNEL SYNDROME

Sensory Function
Fatigues quickly
– Efficiency
– Special attention to areas of:
• Symptomology
• Motor or reflex abnormalities
• Trophic changes
– Confirm with repeat testing!!
Patterns of testing:
– Symmetrical
– Distal vs. proximal: scattered stimuli

Sensory Function Testing
Look for abnormality
– map out boundaries in detail
Source of lesion
Distribution of sensory abnormalities
and kinds of sensations affected
+/- motor/reflex abnormality
Demonstrate to patient before testing

Spinothalamic Tract
Pain
and
temperature
Crude touch
(light touch without localization)
Fibers cross & pass upward into thalamus

Pain Sensation
Sharp safety pin or other tool
Demonstrate sharp & dull
Test by:
– Alternating sharp & dull w/ pt’s eyes closed
Ask patient:
– Sharp or dull?
– Does this feel same as this?
– Lightest pressure needed - do not draw blood

TEMPERATURE
Often omitted if pain sensation normal
Two test tubes
filled with hot & cold water
or tuning fork heated or cooled by water

Light Touch
Wisp of cotton
Touch lightly - avoid pressure
Ask patient:
– To respond when touch is felt
– Compare one area with another
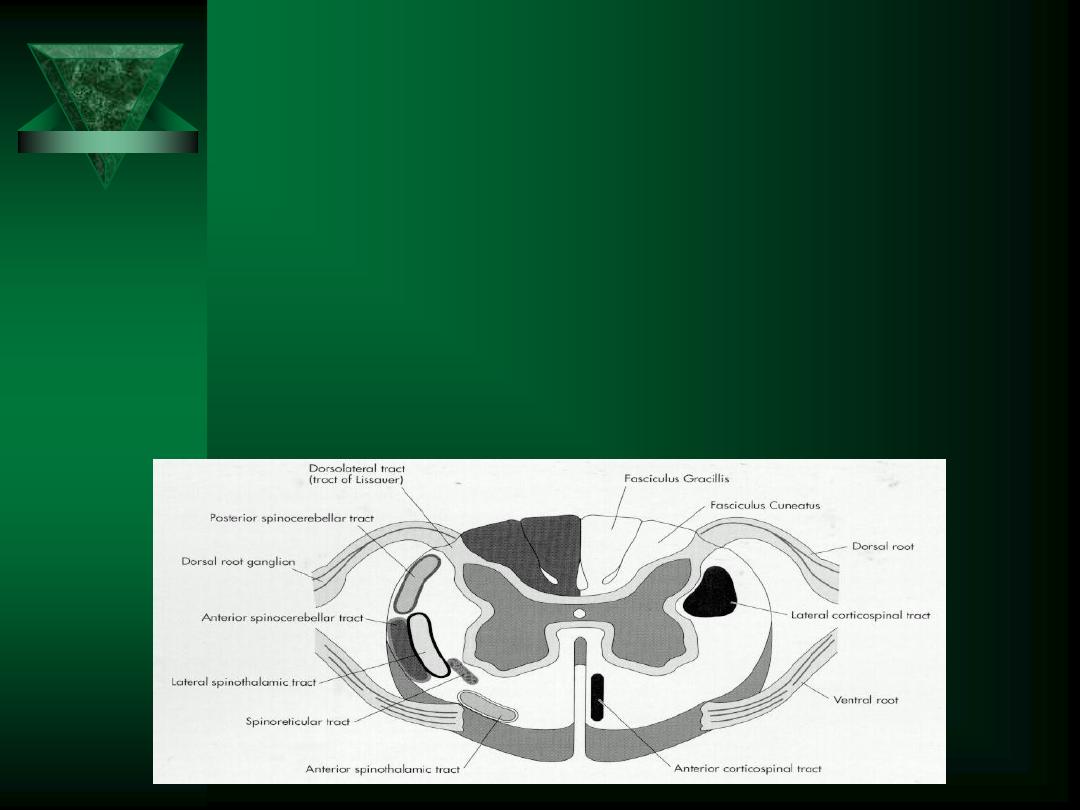
Posterior Columns
Position
and
vibration
Fine touch
Synapse in medulla, cross & continue on to thalamus
Proprioception
Grasp toe by sides - pull away from other toes
Demonstrate “up” & “down”

Vibratory Sense
128 or 256 Hz Tuning fork
If impaired, proceed proximally
Tactile Localization
Have pt close eyes
Touch pt on R cheek & L arm
Ask patient where touch was felt

Discriminative Sensations
Stereognosis, graphesthesia, two-point
discrimination
Test ability of sensory cortex to correlate,
analyze, & interpret sensations
Dependent on touch & position sense
Screen first with stereognosis - proceed to
other methods if indicated
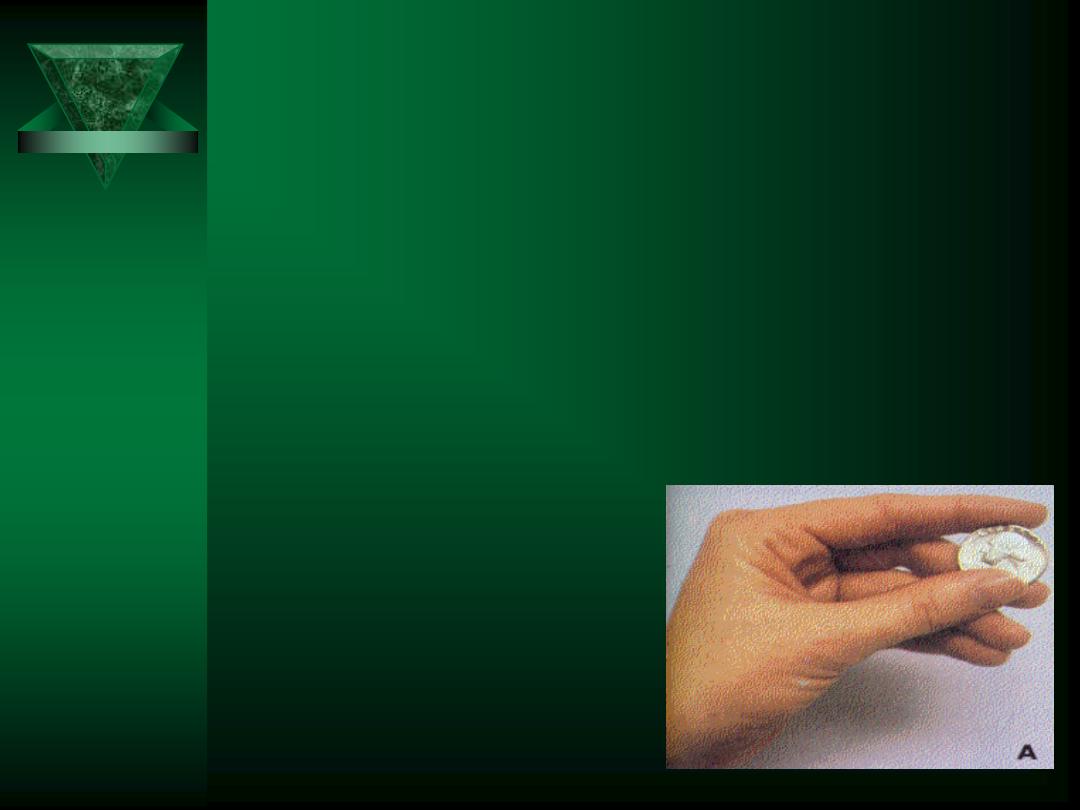
Stereognosis
Ability to identify an object by feeling it
Place familiar object in patient’s hand & ask
patient to identify it
Normally patient manipulates it skillfully &
identifies it correctly
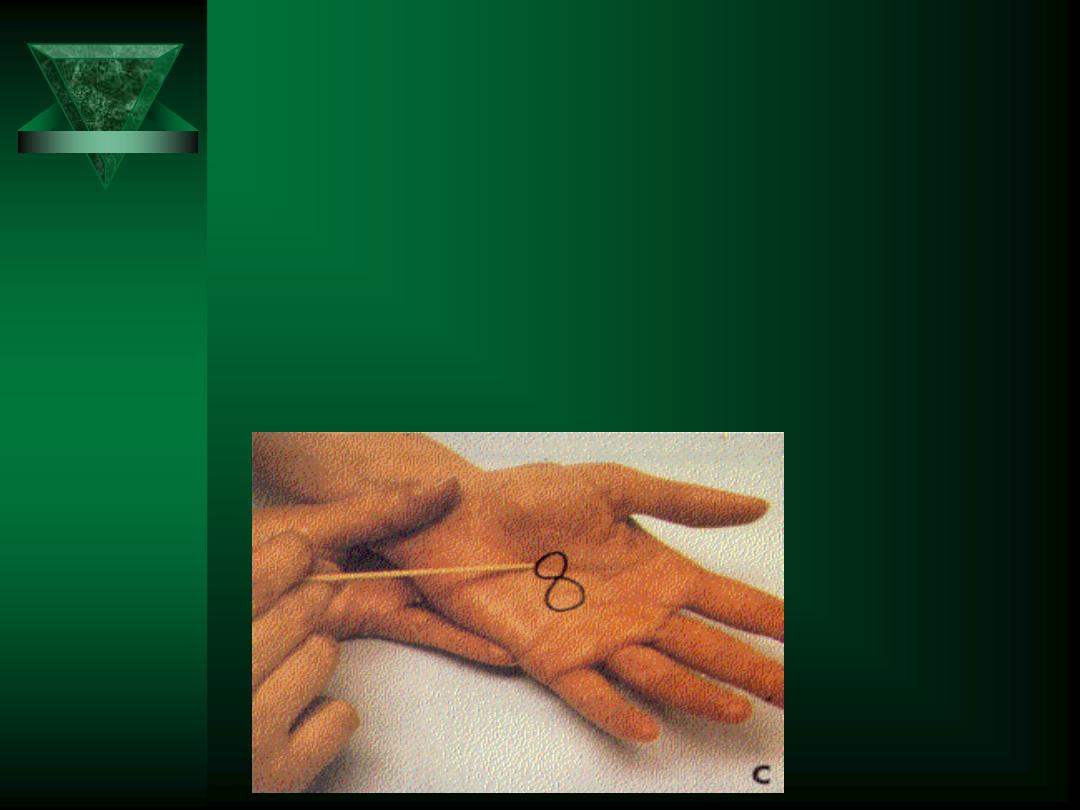
Graphesthesia
Perform if inability to manipulate object
Ability to identify numbers written in hand
Use patient’s orientation

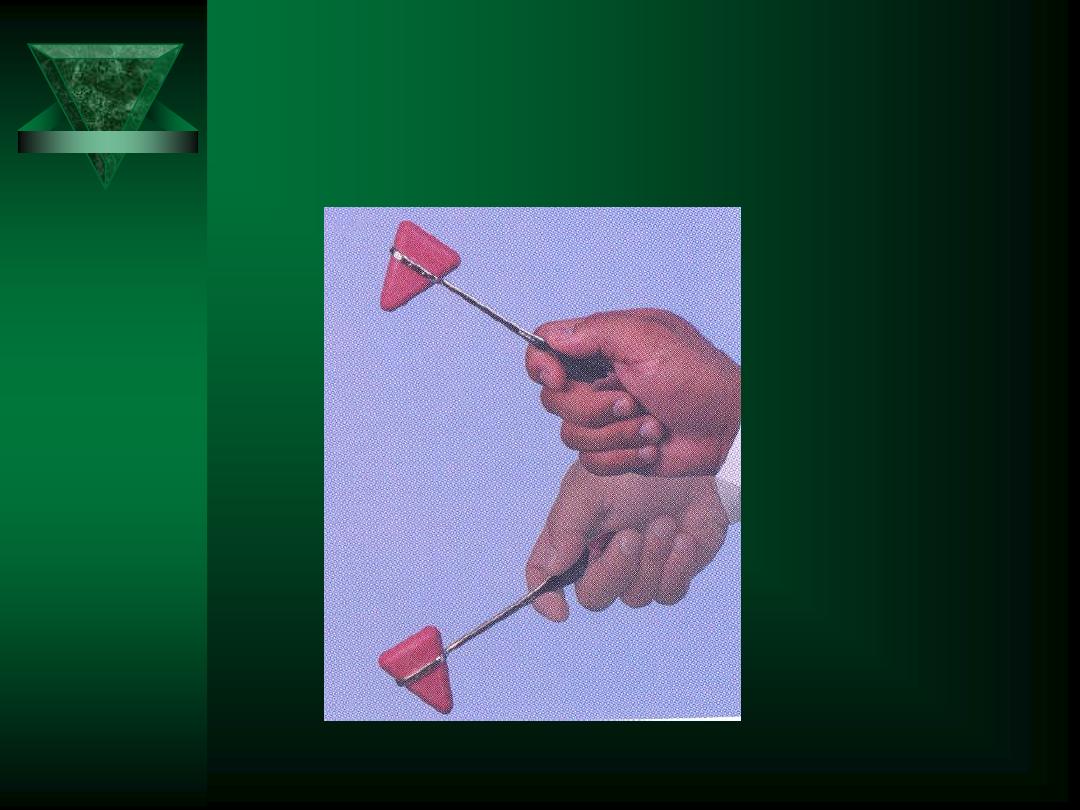
Two-Point Discrimination
Touch two places
simultaneously
Alternate stimuli
Avoid pain
Determine distance

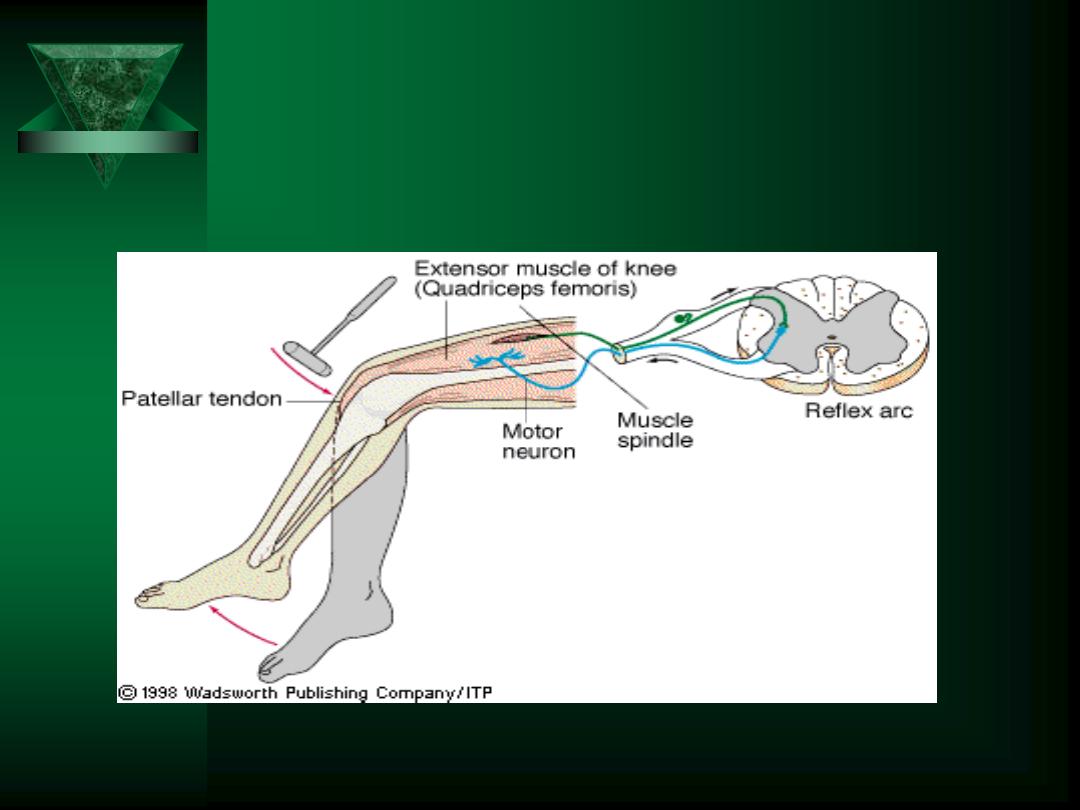
Spinal Reflexes: DTRs
Segmental levels of DTRs:
– Supinator reflex
C5, 6
– Biceps reflex
C5, 6
– Triceps reflex
C6, 7
– Abdominal reflexes - upper
T8, 9, 10
–
- lower
T 10, 11, 12
– Knee (Patellar)
L2, 3, 4
– Plantar responses
L5, S1
– Achilles reflex
S1 primarily

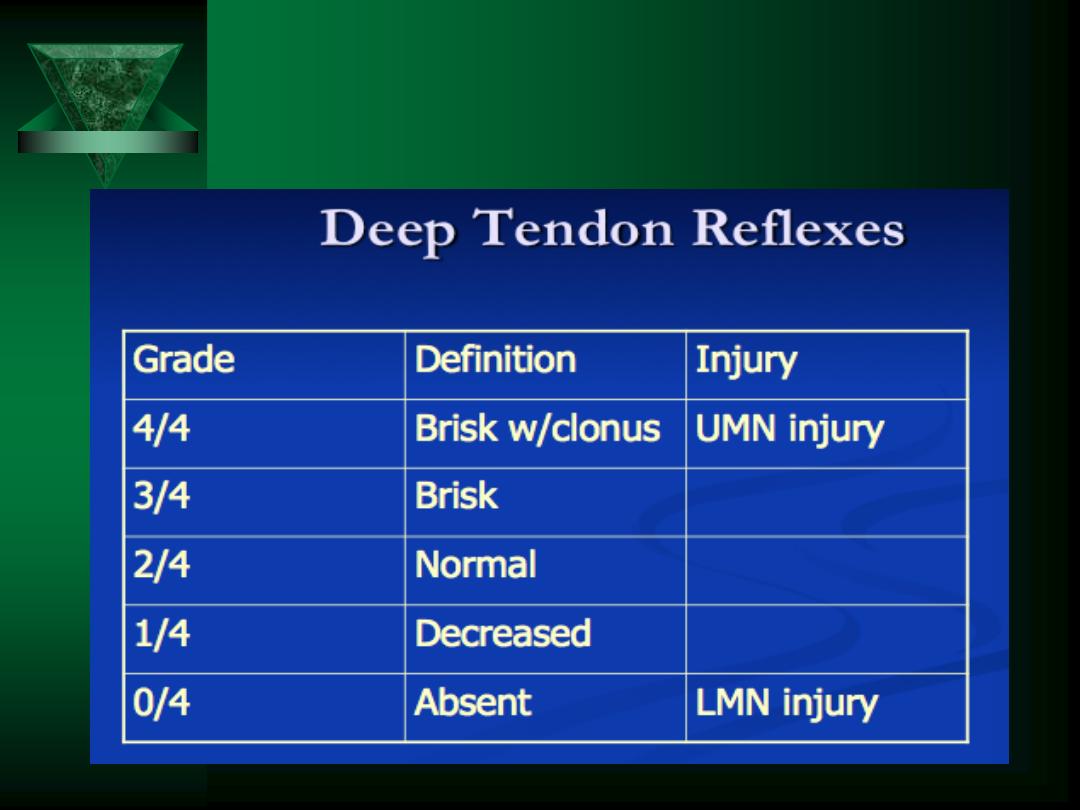
Deep Tendon Reflexes:
Grading
Grade
DTR Response
4+
Very brisk, hyperactive, with
clonus
3+
Brisker than average, slightly
hyperreflexic
2+
Average, expected response;
normal
1+
Somewhat diminished, low
normal
0
No response, absent
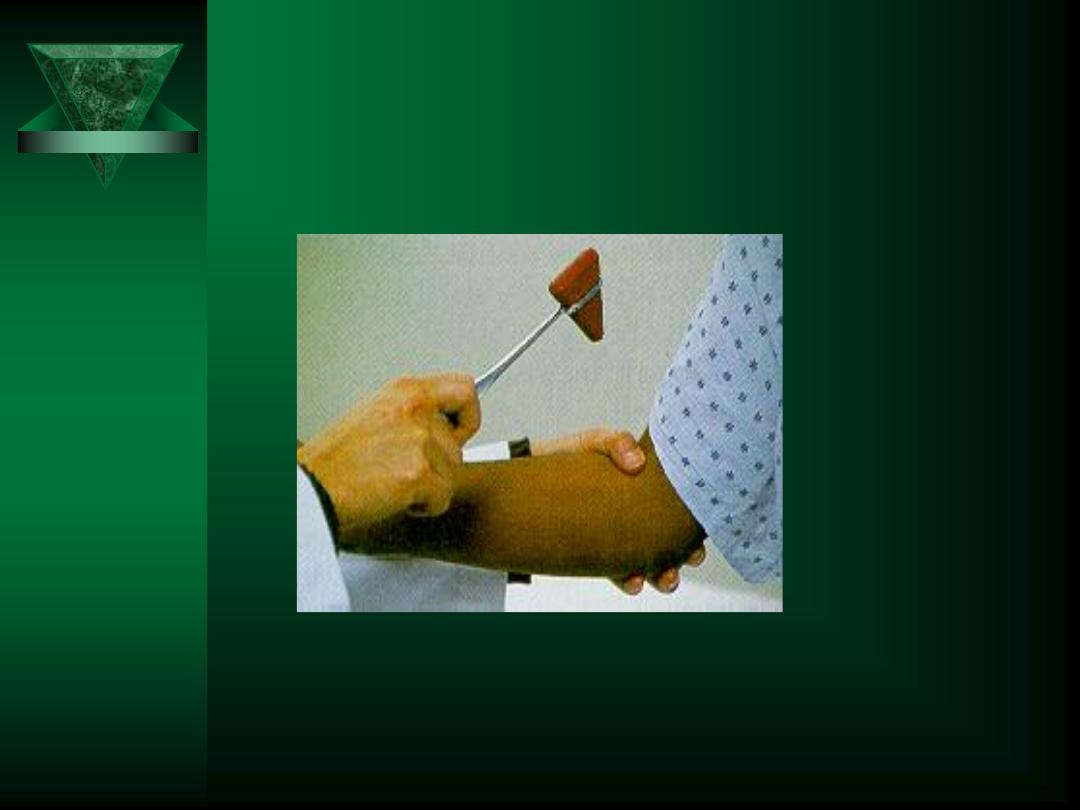
Reflex Hammer - Incorrect
Usage
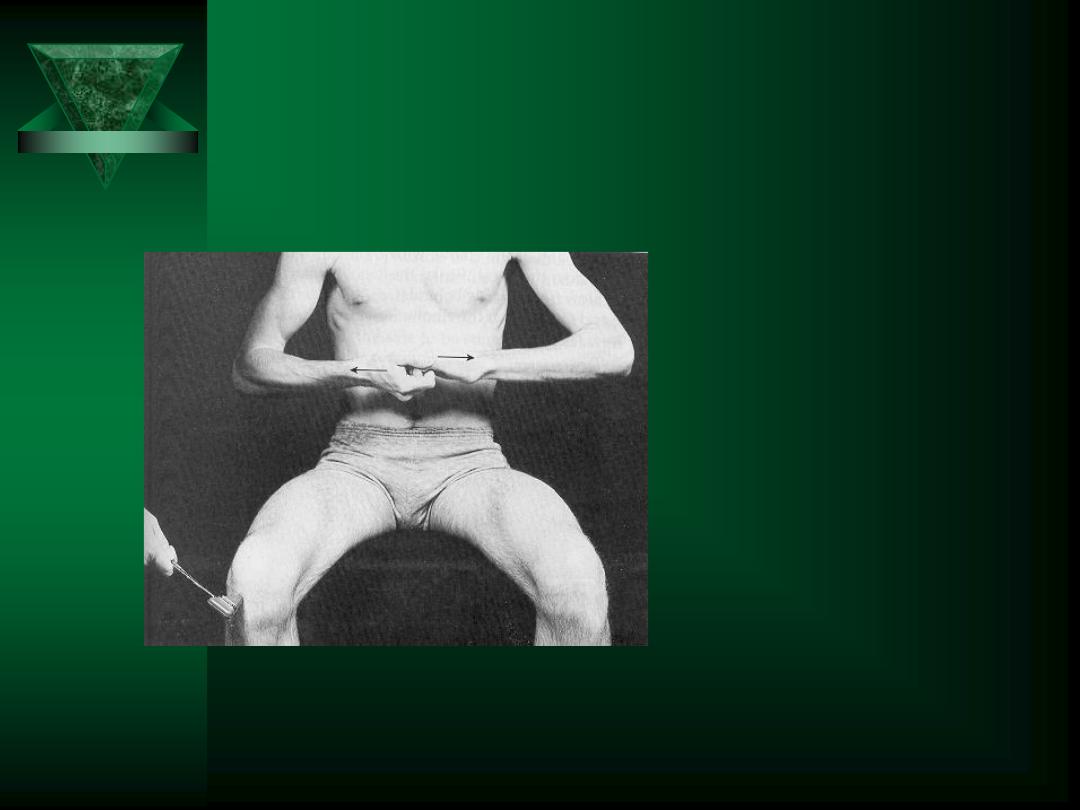
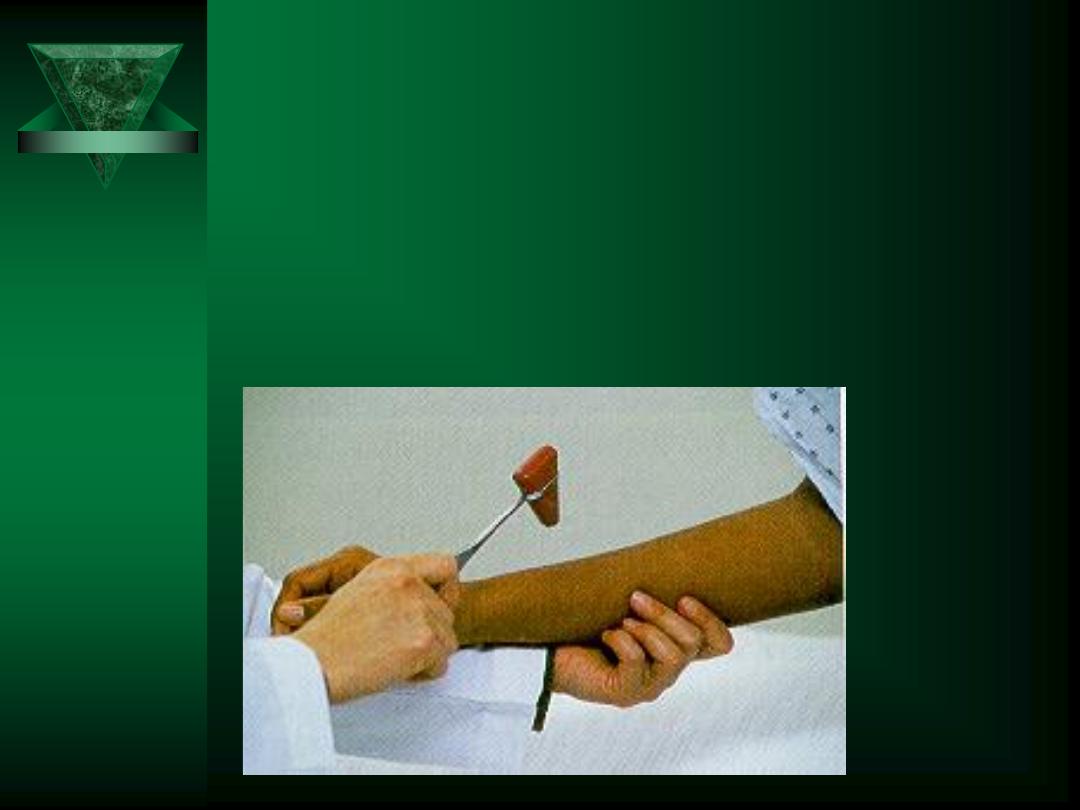
Jendrassik’s Maneuver
Reinforcement
technique
Upper extremities
– clench teeth
– squeeze thigh
Lower extremities
– lock fingers and pull
one against the other
Biceps Reflex
C5,C6
Elbow Flexion

Triceps Reflex
C6, C7, C8
Elbow Extension
Brachioradialis Reflex
C5, C6
Forearm semiflexion/semipronation
(
NO
wrist/hand flexion)

Patellar Reflex
L2, L3, L4
Knee Extension

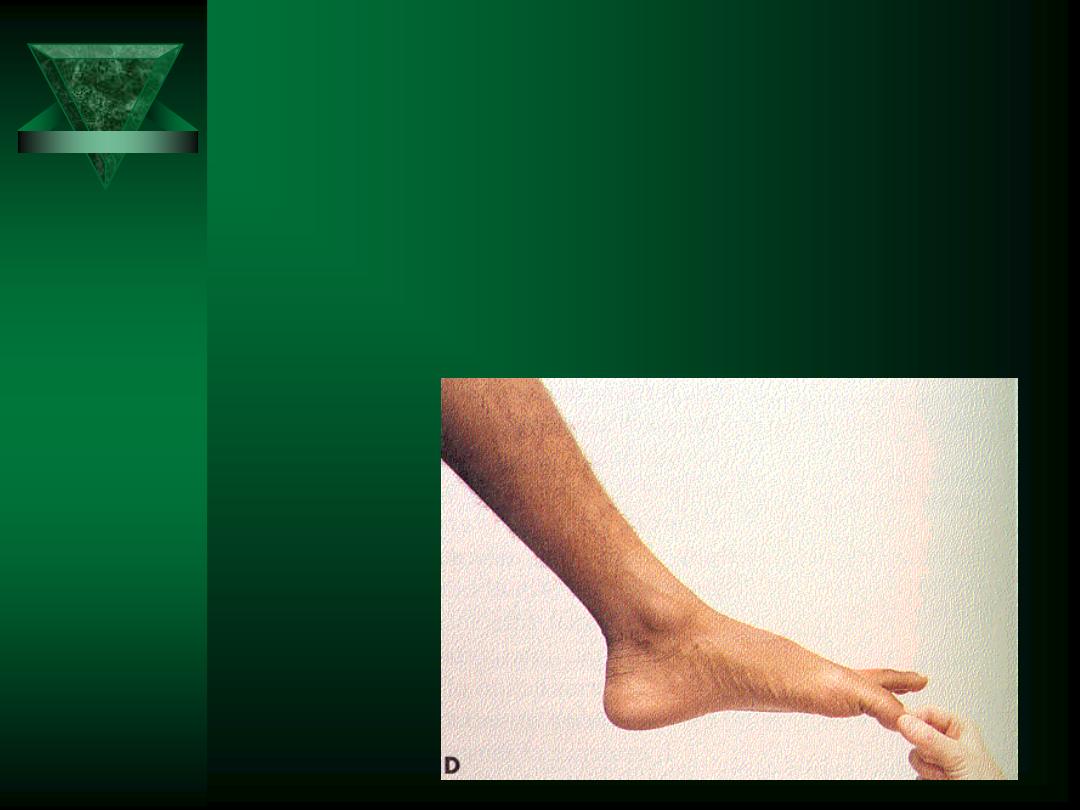
Achilles Reflex
S1, S2
Ankle Plantar Flexion

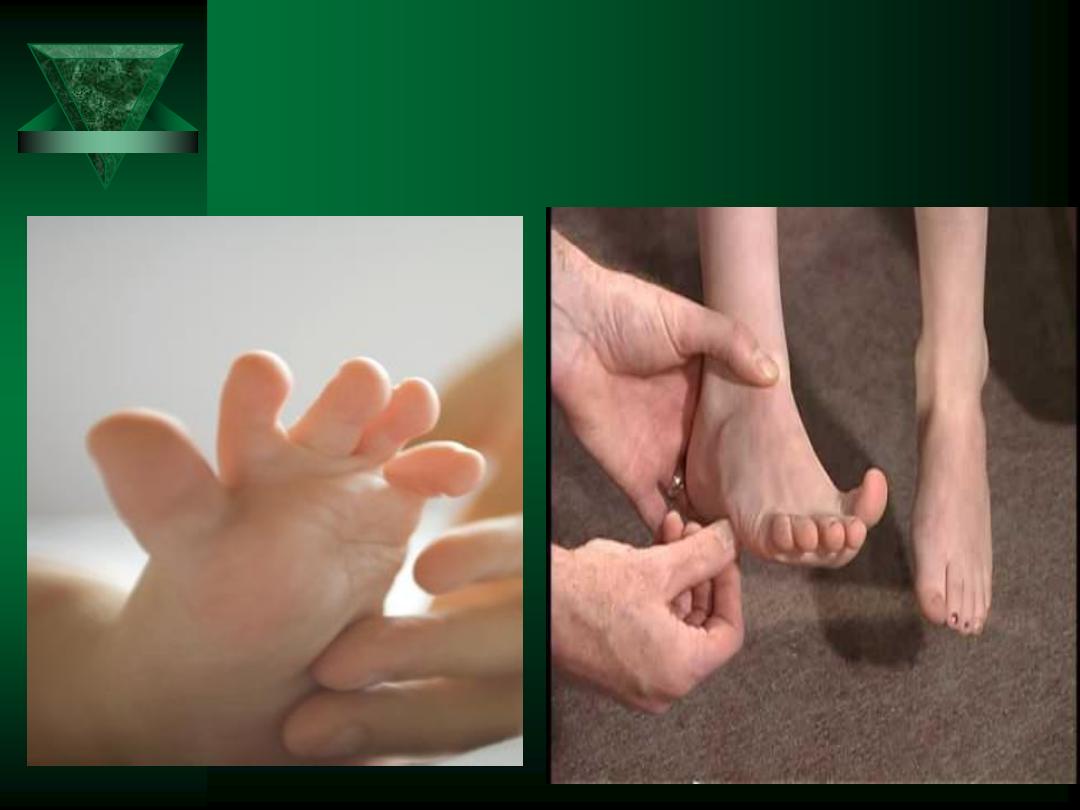
Plantar Reflex
L5, S1, S2
Babinski Sign


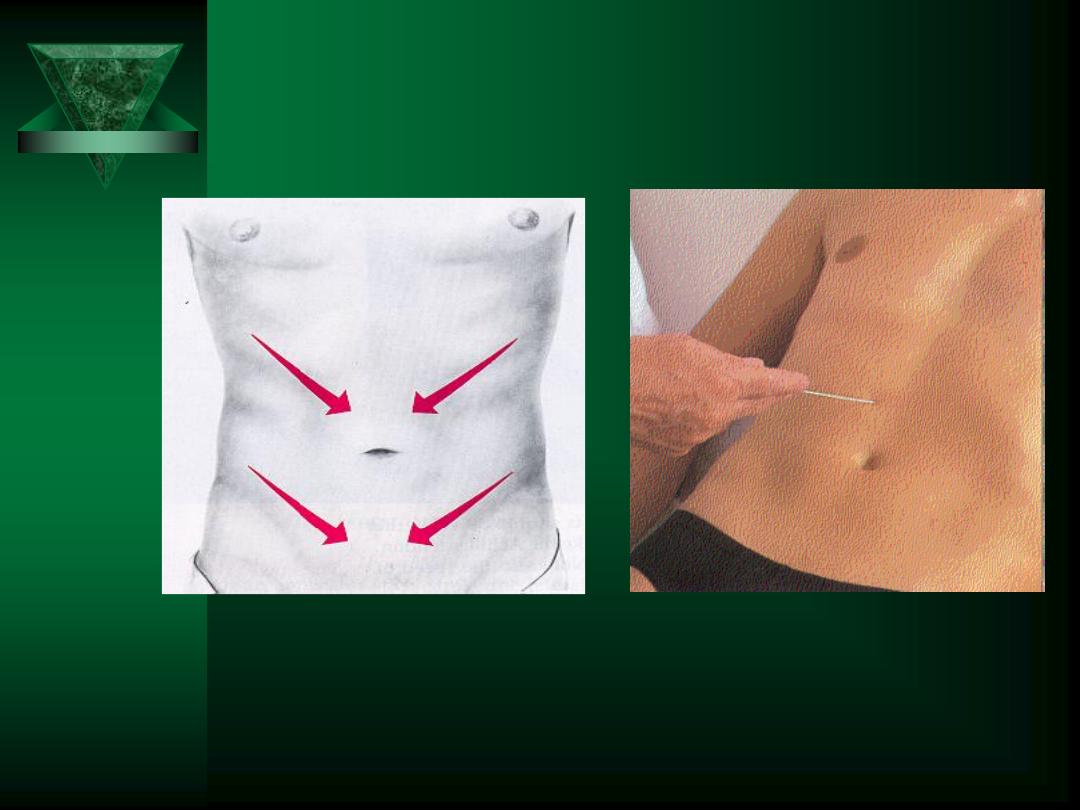
Abdominal Reflexes
T8, T9, T10:
ABOVE
umbilicus
T10, T11, T12:
BELOW
umbilicus

Anal Reflex
Superficial reflex
Loss of anal reflex suggests lesion of S2,3,4
reflex arc
Possible lesion of cauda equina

Clonus
Rhythmic Oscillation
Flexion/Extension
UMN Lesion

Cerebellar Function
Requires
integration of:
Motor system
Cerebellar
system
Vestibular
system
Sensory system
Assessed by:
Rapid alternating
movements
Finger-to-Nose /
Heel-to-Knee Test
Romberg’s Test
Gait
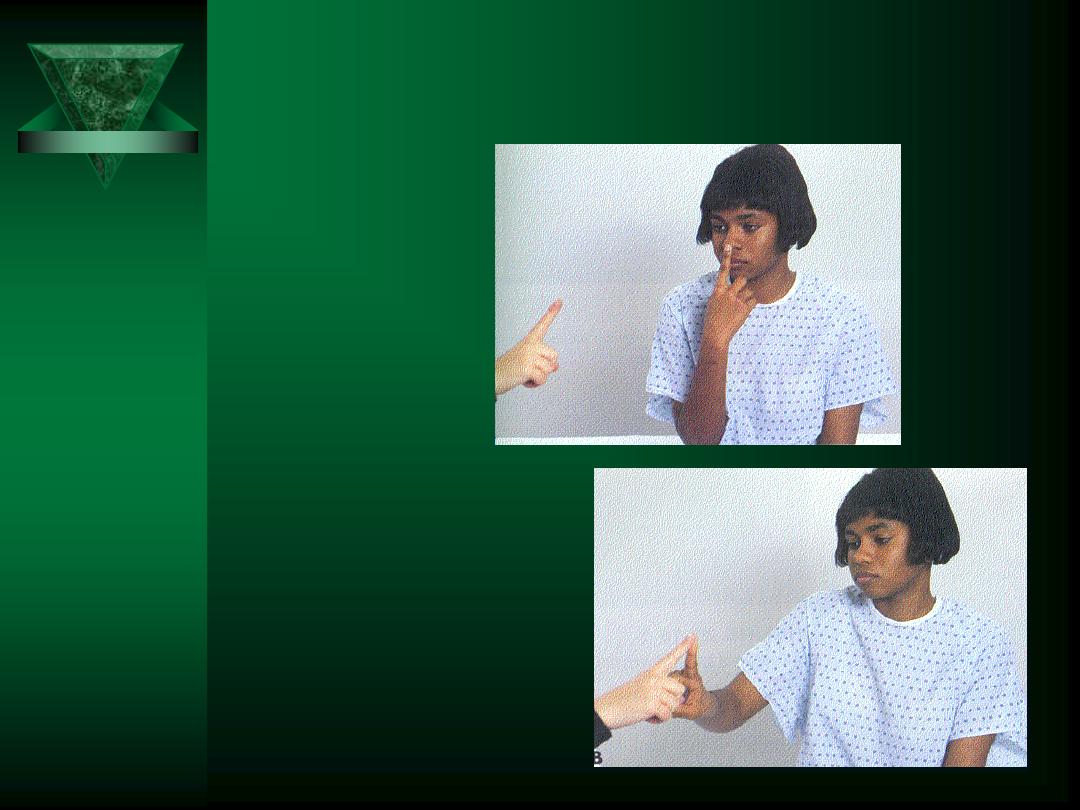
Finger-to-Nose Test
Finger-to-nose
with moving
target
Stationary
finger-to-nose
with eyes closed
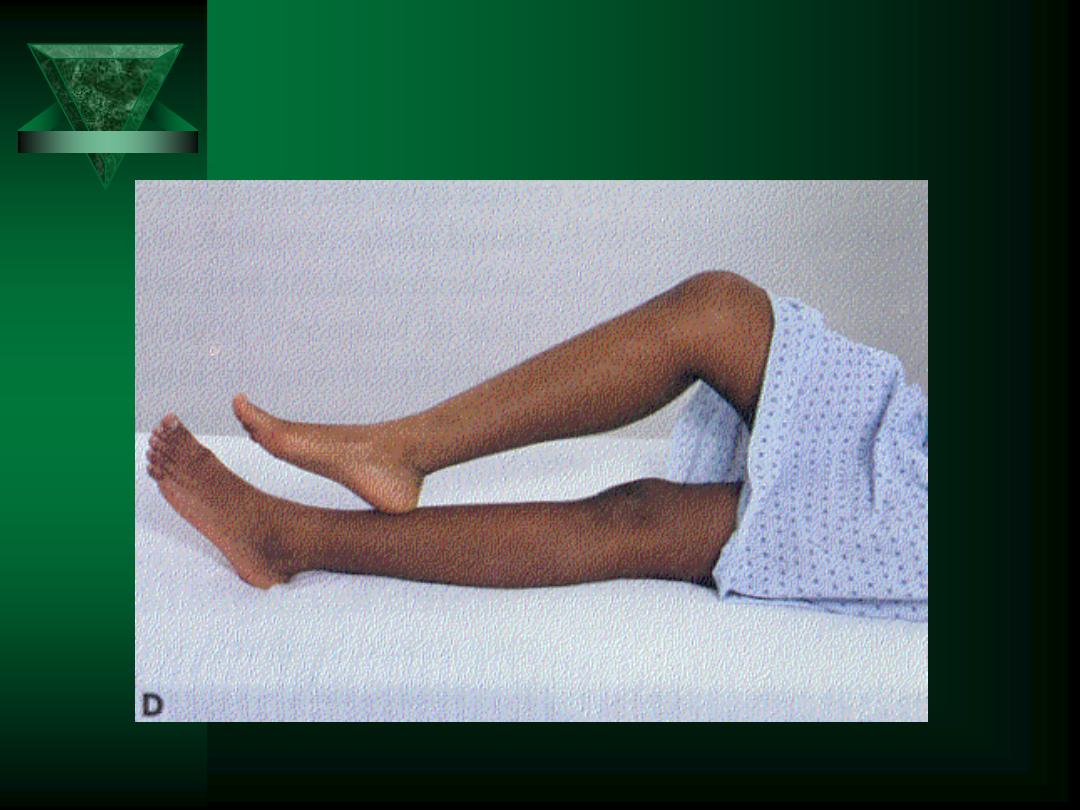
Heel-to-Knee Test

Rapid Alternating Movements
First with hands
Repeat with feet
Diadochokinesia = ability to perform RAM
Dysdiadochokinesis = slow, irregular, clumsy
movements
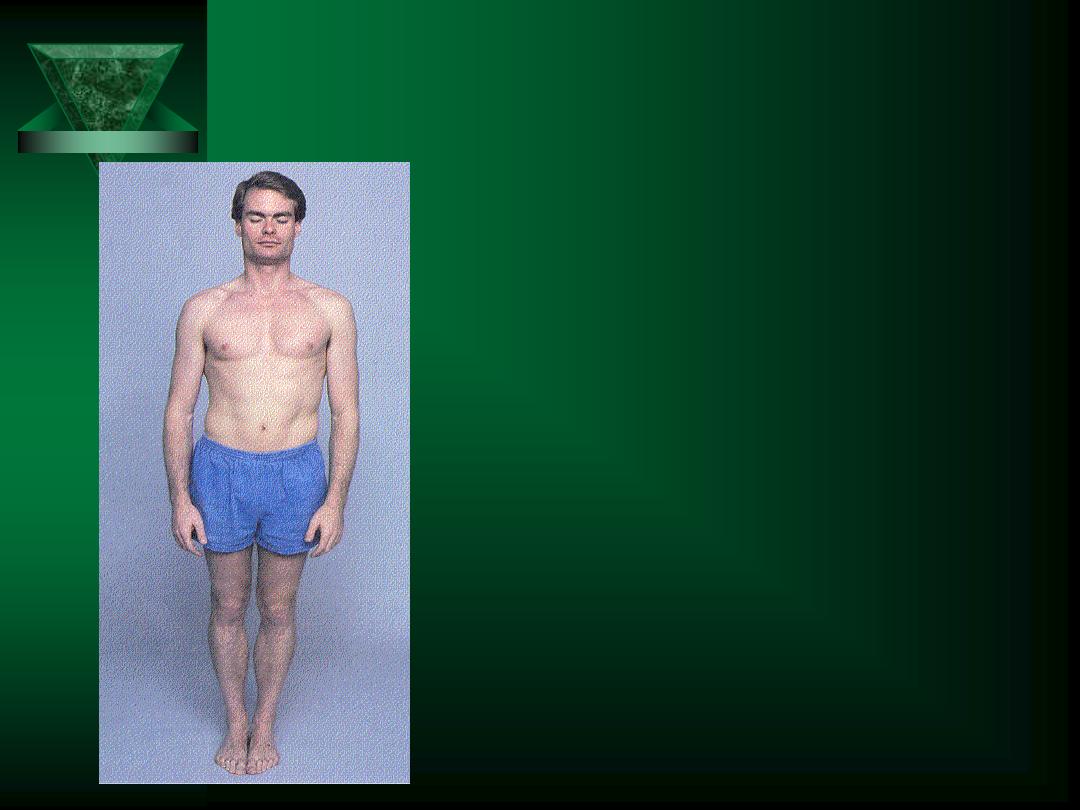
Station, Stance & Romberg’s Test
Station & Stance
– Pt stand with feet together
– First, eyes open
Romberg Test
– Then, close eyes
– If okay with eyes open, but sways
w/ eyes closed = + Romberg
– Mainly tests position sense
• Vision can compensate for loss of
position sense

Pronator Drift
Often performed in
conjunction with
Romberg test
Pronator drift
– Muscular strength
– Coordination
– Position sense
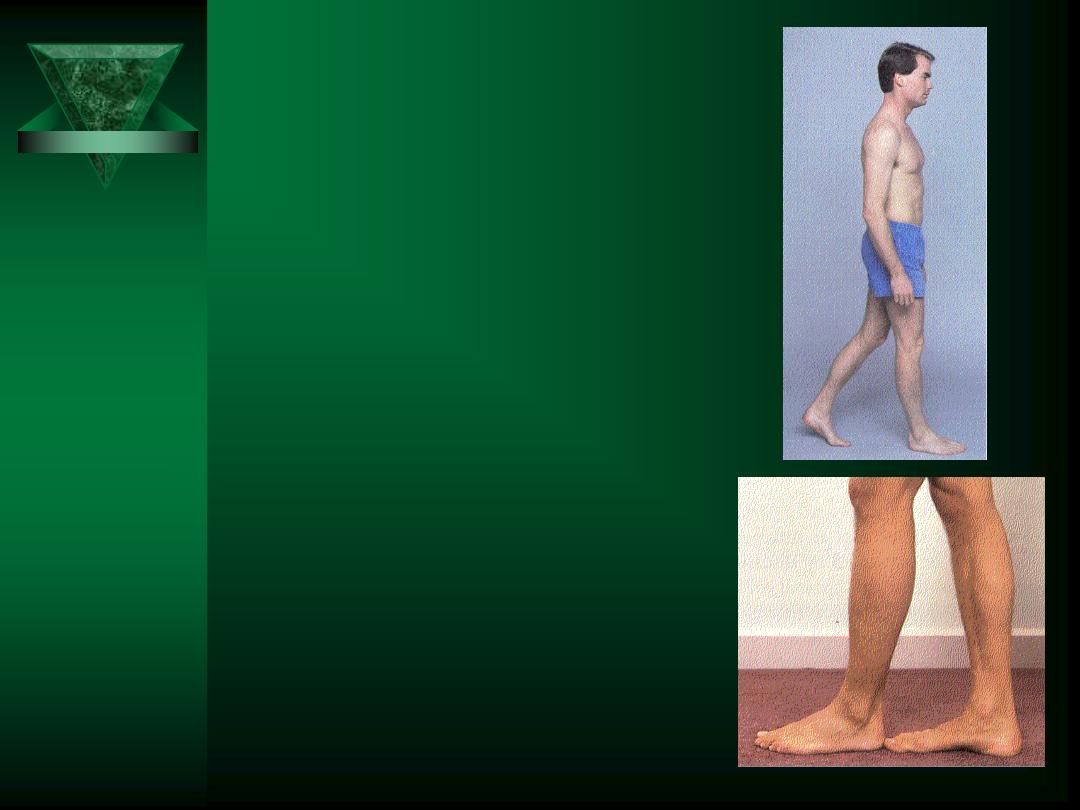
Gait
Walk across room, turn and
walk back
Tandem walking
Heel & toe walking
Hop in place
Shallow knee bend
Rising from sitting position
or stepping up on stool

Meningeal Irritation
Occur with meningitis & subarachnoid
hemorrhage
Brudzinski’s Sign
– Flex the head
– Marked pain in the neck
– Patient flexes hip and BLE
Kernig’s Sign
– Pain when raising a straightened LE

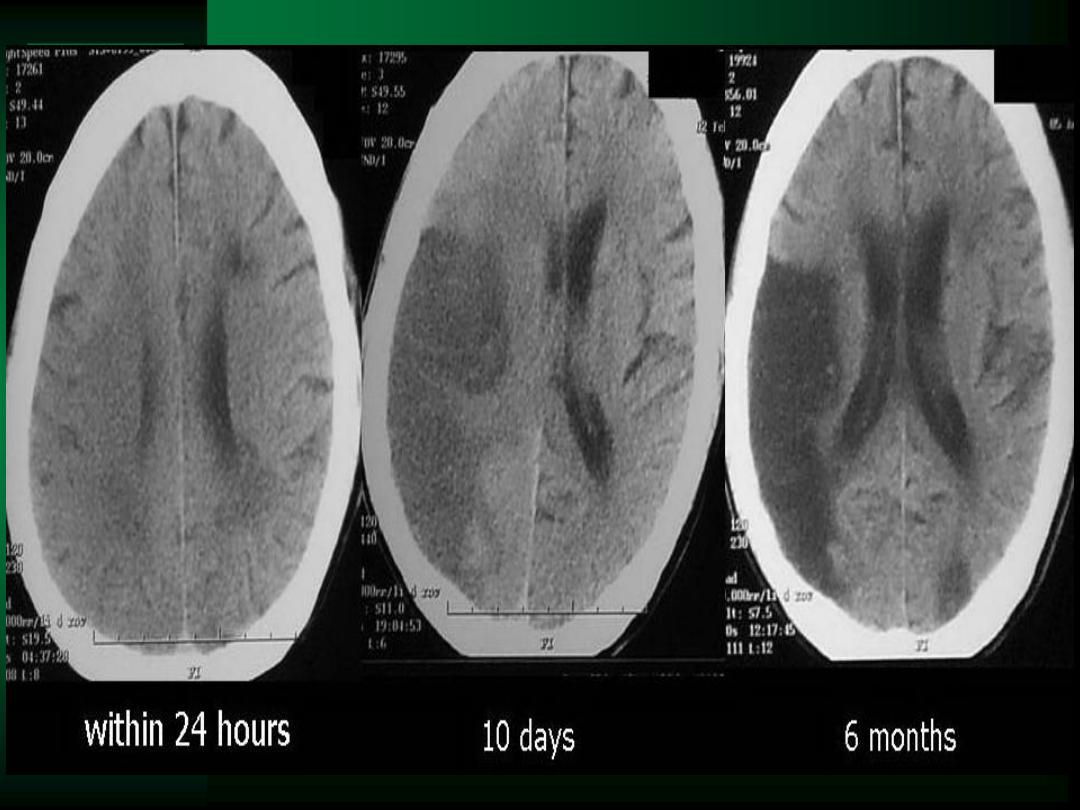
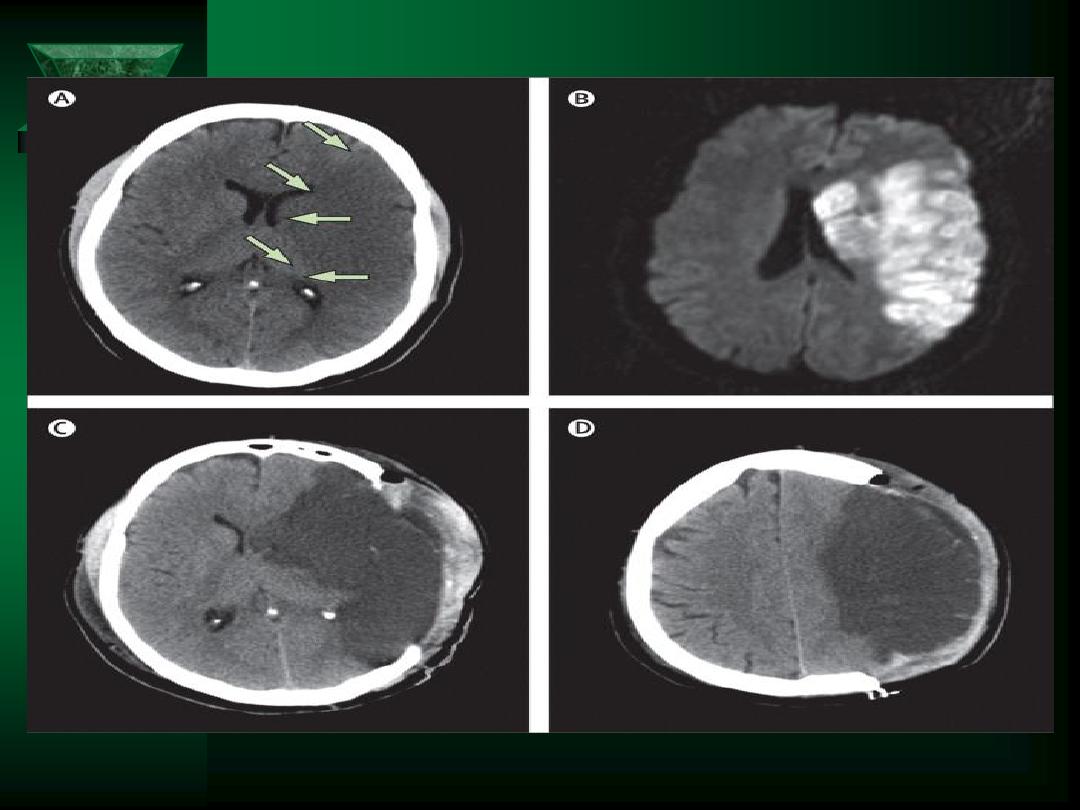
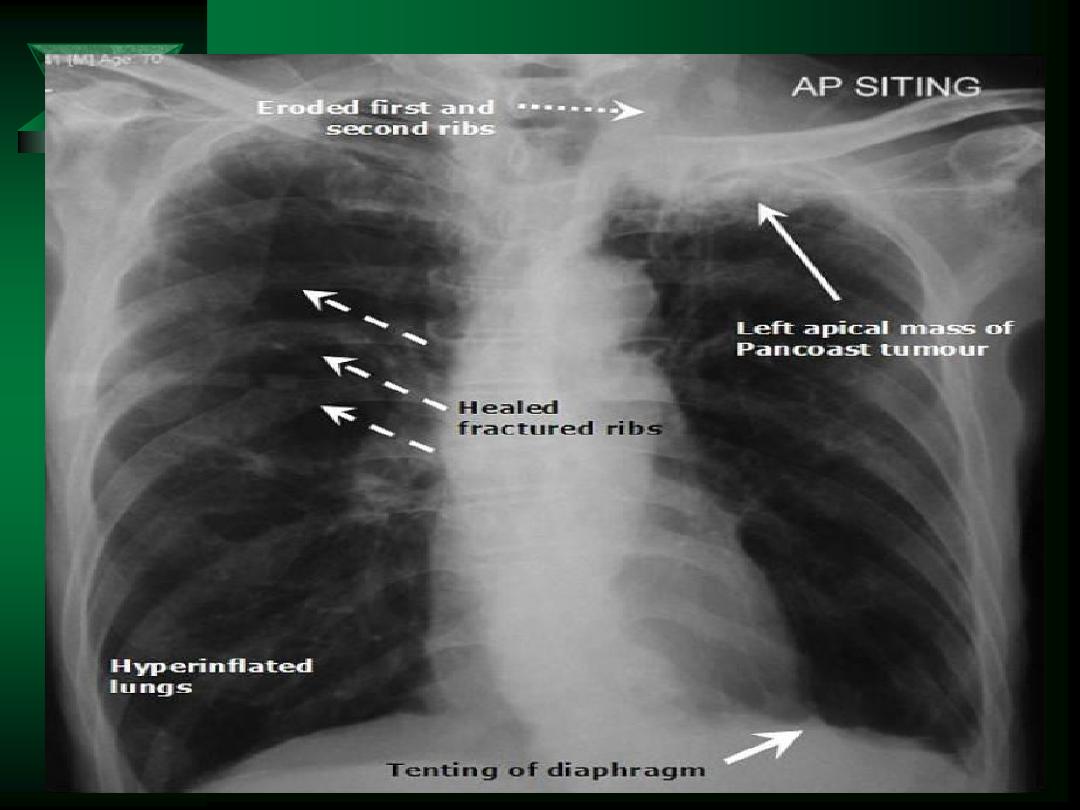
Lab/X-ray
CBC, CMP, U/A
Specific drug levels
Plain films of the spine
CT of the brain & head
MRI of the brain & spine
– Greater resolution then CT for soft tissue/plaques
Angiography
CSF exam
EEG
EMG & NCT
PET/SPECT

CSF
Obtained through lumbar puncture
Indications:
– Suspected CNS infection (i.e. syphilis)
– Suspected subarachnoid hemorrhage
Contraindicated if cerebral mass/lesion is
suspected
Measure opening pressure
Obtain samples for cell counts, glucose,
protein level, and cultures