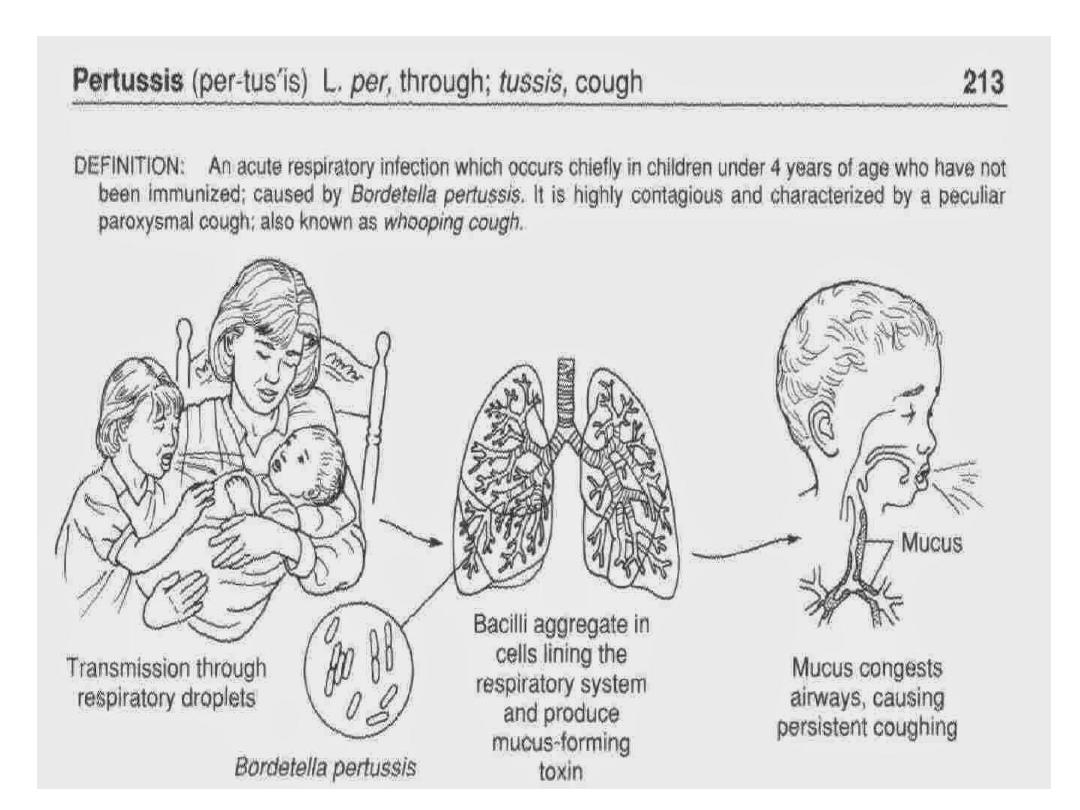
It is an acute, highly infectious disease of the respiratory
tract, caused by Bordetella pertussis. Common among young
children, transmitted by droplet infection. Clinically
characterized by mild fever, attacks of cough with a
characteristic whoop, due to sharp indrawing of breath,
terminated by vomiting.
Attack rate is about 70 to 80 percent and the case fatality rate
is 5 to 15 percent. Chinese call it a ‘Hundred day cough.’
The causative agent is Bordetella pertussis. It is a gram
negative, Cocco-bacillus. They produce an exotoxin
(pertussigen). Capsulated, phase 1 strain results in severe
clinical illness. Bordetella parapertussis often affects older
children but results in minor illness. The toxin is not only an
important virulence factor but also acts as a mediator for
attachment to the respiratory cells.
• Host
Under five children are most susceptible, and the disease is
most severe below 6 months of age. Disease occurs more
frequently and seriously among female children. There are
only clinical cases and no subclinical cases/ carriers.
• Environment
Overcrowding and low socioeconomic status paly important
role in transmission.
Pertussis is a very contagious disease only found in
humans. It is spread from person to person. People
with pertussis usually spread the disease to another
person by coughing or sneezing or when spending a
lot of time near one another where you share breathing
space. Many babies who get pertussis are infected by
older siblings, parents, or caregivers who might not
even know they have the disease.
Incubation period = 7–14 days
Stage 1: Catarrhal stage (2 weeks). Insidious onset of cold, running
nose, watering of eyes, mild fever, irritating cough that worsens at
night.
Stage 2: Paroxysmal stage (2– 4 weeks). Intense bouts of cough in
quick succession with apnea and deep inspiration with a
characteristic ‘whoop’ like sound.
Communicable period:
Maximum infectivity is during the first week of the illness (i.e.
Catarrhal stage) and lasts for about another 3 weeks during the
paroxysmal stage. Patient considered no longer contagious after 5
days of treatment with erythromycin, clarithromycin or
azithromycin.
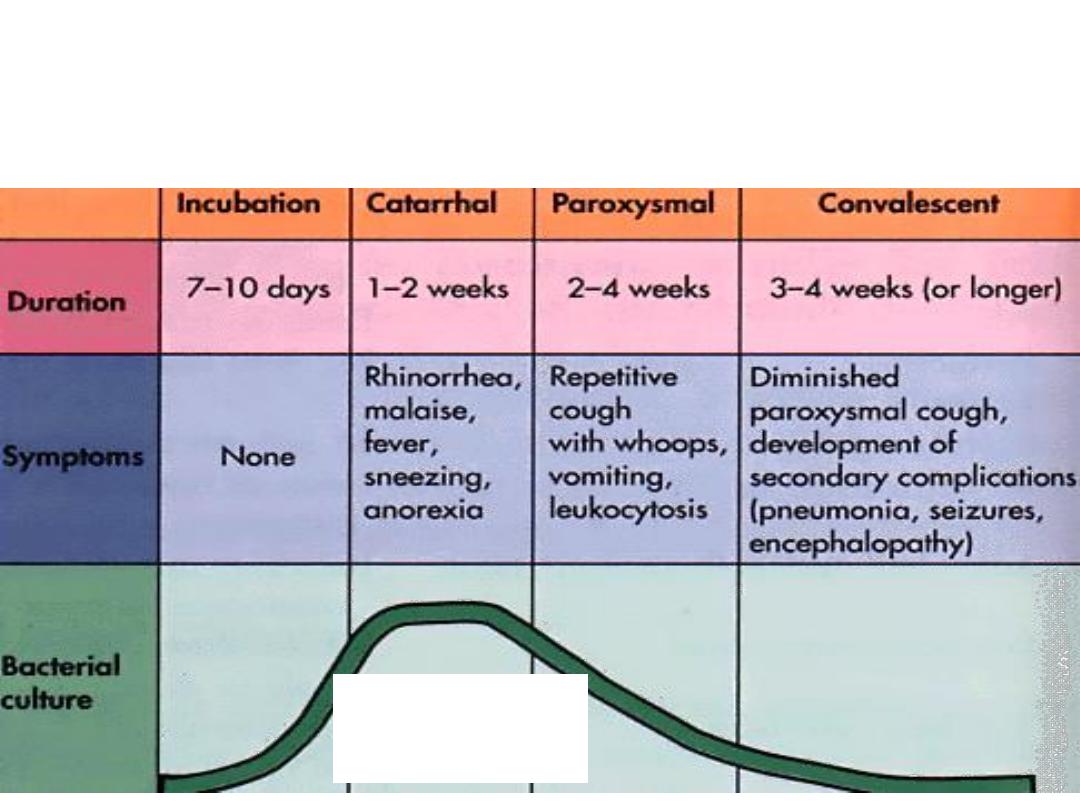
Clinical Progression of Pertussis
Most infectious, but
generally not yet
diagnosed
1. Pressure effects: subconjunctival hemorrhage,
hematemesis, epistaxis.
2. Dehydration and exertion.
3. Bronchitis, emphysema, bronchiectasis,
bronchopneumonia.
4. Convulsion and coma (encephalitis).
Pertussis is one of the most lethal diseases in children
who have not been immunized, or are malnourished.
Diagnosis
1. Signs and symptoms
2. Physical examination
3. Laboratory test which involves taking a
sample of mucus (with a swab or syringe filled
with saline) from the back of the throat through
the nose.
4. Blood test.
Treatment
1. Maintenance of hydration, good nursing care and
continued feeding.
2. Erythromycin 30–50 mg/kg oral daily (in 4 divided
doses) × 10 days.
Erythromycin, clarithromycin and azithromycin can
shortened the period of communicability but do not
reduce symptoms severity or duration unless given
before paroxysmal stage.

Control
A. Controlling the patient:
1. Early detection of cases (the best chances of detection of
bacteria in nasal wash is at the first stage of disease, i.e. 2
weeks after onset of symptoms).
2. Isolation until clinically considered non infective by culture
(at least 3 weeks in untreated patients or 5 days after
erythromycin treatment)
3. Treatment.
B. Breaking the chain
Disinfection of fomites of all cases.
Control
C. Active immunization:
There are two kinds of vaccines
• Whole cell killed vaccine (wP) which can
cause the same neurologic complications as the
pertussis bacillus.
• Acellular vaccine (aP).
Both vaccines are safe but both local and
transient systemic reactions are less commonly
associated with a cellular vaccine than whole
cell vaccine.
Control
Adverse effects of vaccine include local redness
and swelling, fever and agitation which often
occur after use of (wP) in about (1 to each 2-10),
prolong crying and febrile seizures are rare (1 in
2000).
Pertussis vaccines are highly effective and save
many infant lives every year. Although
protection lasts only a few years, those few
years include the preschool age, which the time
of greatest risk from pertussis.
Control
The recommended pertussis vaccine for babies and
children is called DTP or DTaP. This is a combination
vaccine that protects children against 3 diseases:
diphtheria, tetanus, and pertussis. For maximum
protection against pertussis, children need 5 shots.
Parents can also help protect their children by
keeping them away, as much as possible, from
anyone who has cold symptoms or is coughing.
D. Management of contacts of a case
For all contacts of a case, provide the following:
1. Inadequately immunized contacts less than 7 years may
excluded from the school for 21 days after last exposure or
until received 5 days of appropriate antibiotics.
2. Prophylactic erythromycin (7 days course) is recommended
regardless immunization status or age for households where
there is a child less than 1 year of age.
Management of contacts of a case
Prophylactic antibiotics is especially recommended for
children below 1 year and pregnant women in last 3
weeks of pregnancy because risk of transmission to
newborn.
3. Booster dose of DPT.
4. Ring immunization (protecting a child by
vaccinating his playmates, so that he is surrounded by
immune individuals).

leprosy
Leprosy is a chronic disease caused by a bacillus
Mycobacterium leprae.
M. leprae multiplies slowly and the incubation period of
disease, on average, is 5 years.
In some cases, symptoms may occur within 1 year but can
also take as long as 20 years to occur.
The disease mainly affects the skin, the peripheral nerves,
mucosa of the upper respiratory tract, and also the eyes.
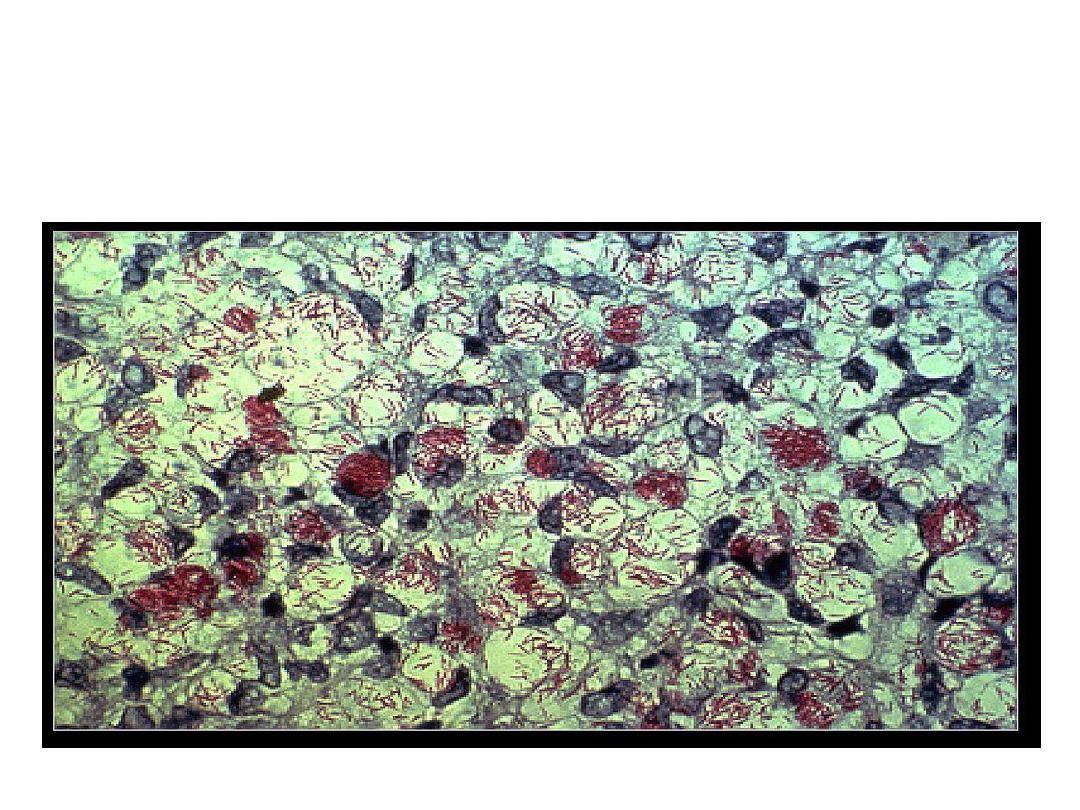
M. Leprae an acid-fast bacterium, M. leprae appears red
when a Ziehl-Neelsen stain is used

leprosy
Leprosy is curable with multidrug therapy
(MDT).
Although not highly infectious, leprosy is
transmitted via droplets, from the nose and
mouth, during close and frequent contacts with
untreated cases.
Untreated, leprosy can cause progressive and
permanent damage to the skin, nerves, limbs, and
eyes.
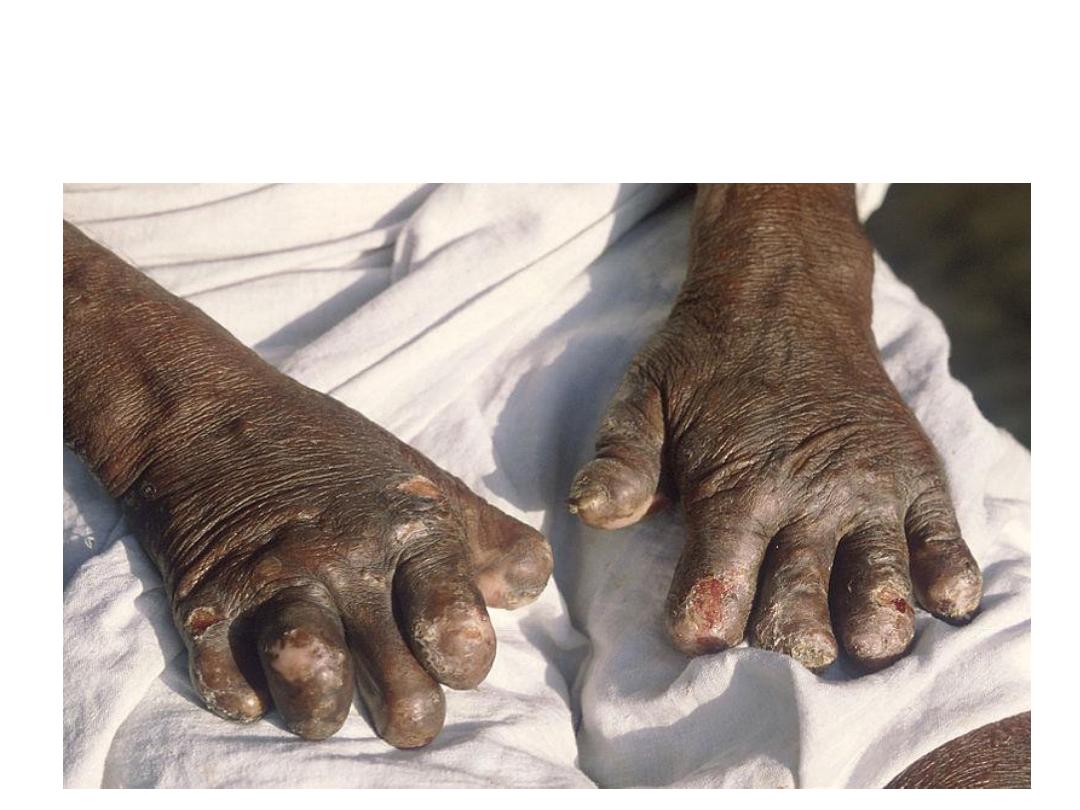
Hands deformed by leprosy

Control
1. Strengthening patient and community
awareness of leprosy.
2. Promoting early case detection through active
case-finding in areas of higher endemicity.
3. Ensuring adherence to treatment, including
working towards improved treatment regimens.
4. Improving prevention and management of
disabilities.

Control
5. Strengthening surveillance for antimicrobial
resistance including laboratory network.
6. Promoting innovative approaches for training,
referrals, and sustaining expertise in leprosy.
7. Promoting interventions for the prevention of
infection and disease.
8. Ensuring political commitment and adequate
resources for leprosy programs.

Control
9. Promoting social inclusion by addressing all forms of
discrimination and stigma.
10. Empowering persons affected by leprosy and
strengthening their capacity to participate actively in
leprosy services.
11. Involving communities in action for improvement of
leprosy services.
12. Promoting access to social and financial support
services, for example to facilitate income generation for
persons affected by leprosy and their families.

Control
13. Supporting community-based rehabilitation
for people with leprosy-related disabilities.
14. Working towards abolishing discriminatory
laws and promoting policies facilitating inclusion
of persons affected by leprosy.
