[
1
]
Medicine
THE IMMUNE SYSTEMLec. 1
HOST DEFENCE
Whether the organisms invade and cause disease is determined by the balance of the
pathogenicity of the organism (i.e. the virulence factors that it has ) and the integrity of
the host defence mechanisms..
The immune system protect the host from pathogens while minimising damage to self
tissue.
The immune system not only protects against infection, but can lead to autoimmune
diseases.
so Dysfunction or deficiency of the immune response leads to a wide variety of diseases,
involving every organ system in the body.
Immunity is often divided into two types
1. termed innate and
2. adaptive (acquired or specific), although in practice these overlap and interlink
1. INNATE IMMUNITY
Innate immunity provides the immediately active, first line, non-specific host defence
mechanisms. It includes
A- physical (e.g. epithelial cells,skin and mucous membrane,coughreflex,mucociliary
Ciliary paralysis (smoking, primary ciliarydyskinesis syndromes),Increased mucus
production (asthma) ,washing,tear,saliva,urine)
B- chemical (e.g. 'natural' antimicrobial substances like defenses at surface barriers eg.
Gastric acid secreation)
C- Biological Colonization resistance provided by nonpathogenic commensal
Organisims of skin and gut

[
2
]
Innate immune mechanisms
These are directly activated by infectious agents, tissue damage or tumours) consist of
1. Cellular such as phagocytic cells (neutrophils, and monocytes in the blood;
macrophages including dendritic cells in tissues, natural killer cell, eosinophils, mast
cells and basophils)
2. humoral components (e.g. complement, acute-phase reactants, cytokines).
Initiation of the inflammatory response:
Phagocytosiss
Phagocytes ('eating cells') are specialised cells which ingest and kill microorganisms,.
They include
neutrophils, monocytes and macrophages
,
and are particularly important
for defence against bacterial and fungal infections
neutrophils travel within the blood They are short-lived cells with a half-life of 6 hours. A
series of events leads to the recruitment and activation of these cells at the site of tissue
damage.
Cell recruitment:
Recruitment of cells of the immune system (phagocytes and lymphocytes) to tissue sites
involves
1. cellular adhesion molecules (CAM) ). The main ones are the a-intercellular adhesion
molecules (ICAM), b-integrins,and c-selectins Adhesion molecules associate with
cytoskeletal components to cause cytoskeletal reorganization, resulting in migration
and spreading, allowing the cells to move
2. Chemoattractants Cells move towards the site of inflammation in response to
chemoattractants (chemicals which attract cells) at sites of infection or tissue
damage.
The cells pass between endothelial cells into the tissues by the formation of foot-like
processes (pseudopodia) that push through the intercellular spaces; this process is
called diapedesis. The cells continue to move along the chemoattractant gradient to the
site of infection ).
[
3
]
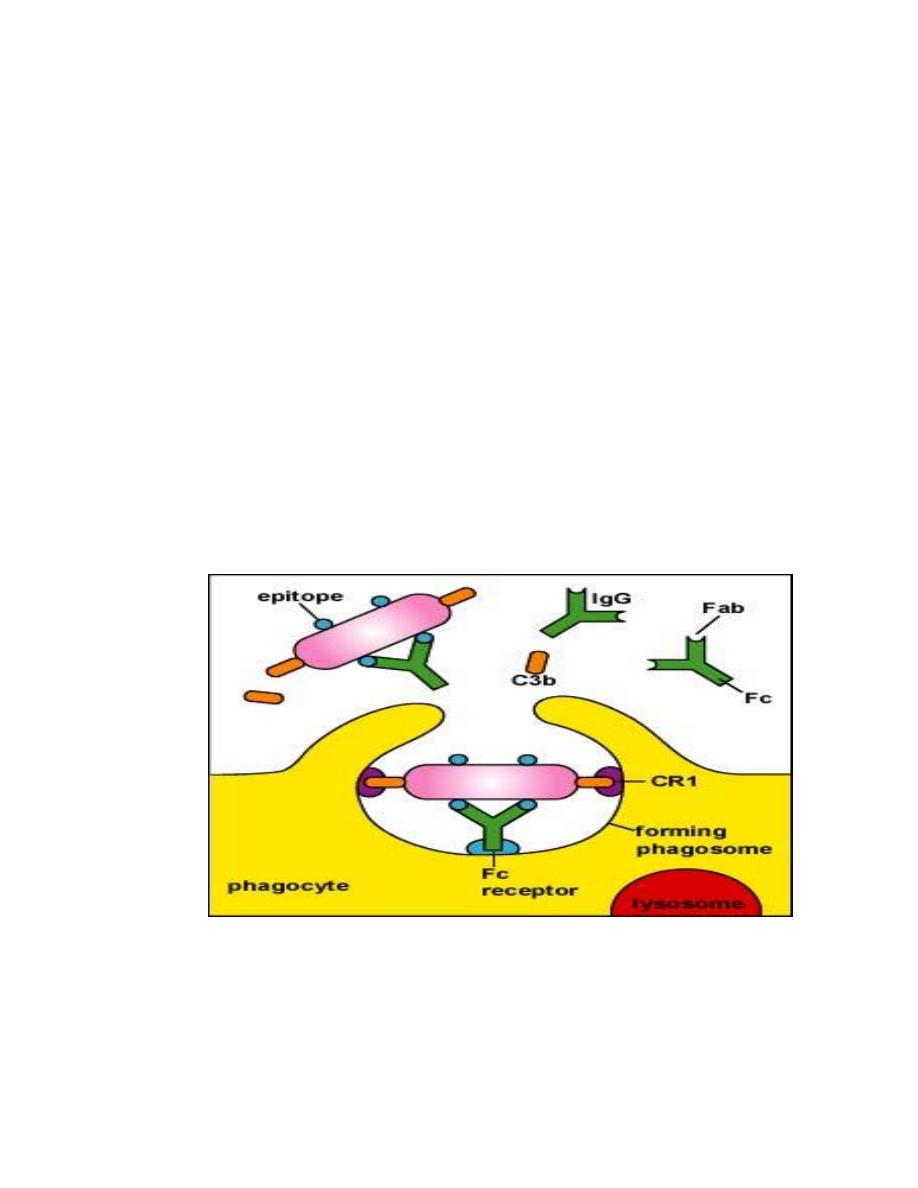
Once the neutrophils have been recruited, phagocytosis (ingestion) and intracellular
killing of microbes begins. Phagocytosis occurs by the formation of pseudopodia
(projections of cytoplasmic membrane) around the organism or particle to be
ingested ). Owing to the fluidity of the cell membrane, the tips eventually fuse to
form a membrane-bound vesicle called a phagosome. This fuses with the neutrophil
cytoplasmic granules, lysosom ) to form a phagolysosome. Within this localized
environment, killing occurs
Ingestion and killing of organisms is much more effective if the particle is first coated
or opsonized ('made ready to eat') with a-
specific antibody , b-acute phase protein
and c-complement.
This is because neutrophils have receptors for the Fc portion of
antibody molecules (FcR), and complement (CR). Binding of cell-surface receptors to
complement and antibody on the particle both increases the strength of adhesion
and causes transduction of intracellular signals, which activate the cell to promote
phagocytic and killing activity.
Opsonins
include acute phase proteins such as C-reactive protein (CRP), antibodies
and complement. They bind both to the pathogen and to phagocyte receptors, acting
as a bridge between the two to facilitate phagocytosis (.
Monocytes and macrophages
Monocytes are the precursors of tissue macrophages
. They are produced in the bone
marrow and exported to the circulation, where they constitute about 5% of leucocytes.
From the blood stream, they migrate to peripheral tissues where they differentiate into
tissue macrophages and reside for long periods.

[
4
]
Specialised populations of tissue macrophages
include Kupffer cells in the liver, alveolar
macrophages in the lung, mesangial cells in the kidney, and microglial cells in the brain.
Macrophages, like neutrophils, are capable of phagocytosis and killing of
microorganisms . Unlike neutrophils, macrophages do not die after killing pathogens
Eosinophils in host defence :
eosinophils are most commonly associated with allergic disease, . Eosinophils have
receptors for IgE which is the major antiparasite antibody, particularly against
nematodes. Eosinophils bind IgE via the FcεR, and toxic metabolites are released from
the eosinophil granules directly onto the parasite surface
Mast cells and basophils :
Mast cell function appears to be in the initiation of inflammatory responses (increased
vascular permeability, bronchoconstriction) by the release (following degranulation) of
pro-inflammatory mediators such as histamine, leukotrienes, platelet-activating factor
(PAF), prostaglandins and some cytokines (e.g. IL-4). Basophils are morphologically
similar to mast cells but are found in very small numbers in the blood.
Dendritic cells/Langerhans' cells
These are derived from the lymphoid and myeloid cell lines; dendritic cells in the skin
are called Langerhans' cells. Their major function is to present antigen to T cells when
stimulated. Dendritic cells link innate immunity to the adaptive immune system by
being the only cell that can activate native T cells to initiate an adaptive immune
response
Natural killer (NK) cells
These non-phagocytic cells have the morphology of lymphocytes but do not bear the
markers for T or B cells. They are distinguished by the presence of numerous
cytoplasmic granules. They have non-specific antiviral and antitumour activity, causing
lysis of cells with which they react
[
5
]
Cytokines are small soluble intercellular messengers that exert their effect by binding
to specific receptors on target cells.. Cytokines are produced by any cell. Their
biological effect varies according to the cytokine and the cell involved ,
Function: signal certain cell populations to activate, divide or home in on a particular
site in the body.
Cytokines include:
1. Interleukins produced by and signal between white cells.
2. Chemokines have a chemoattractant function.
3. Colony-stimulating factors cause differentiation and proliferation of stem cells.
4. Tumour necrosis factors. TFN-α increases phagocyte function.
5. Interferons : interferons are antiviral agents produced mainly by fibroblasts
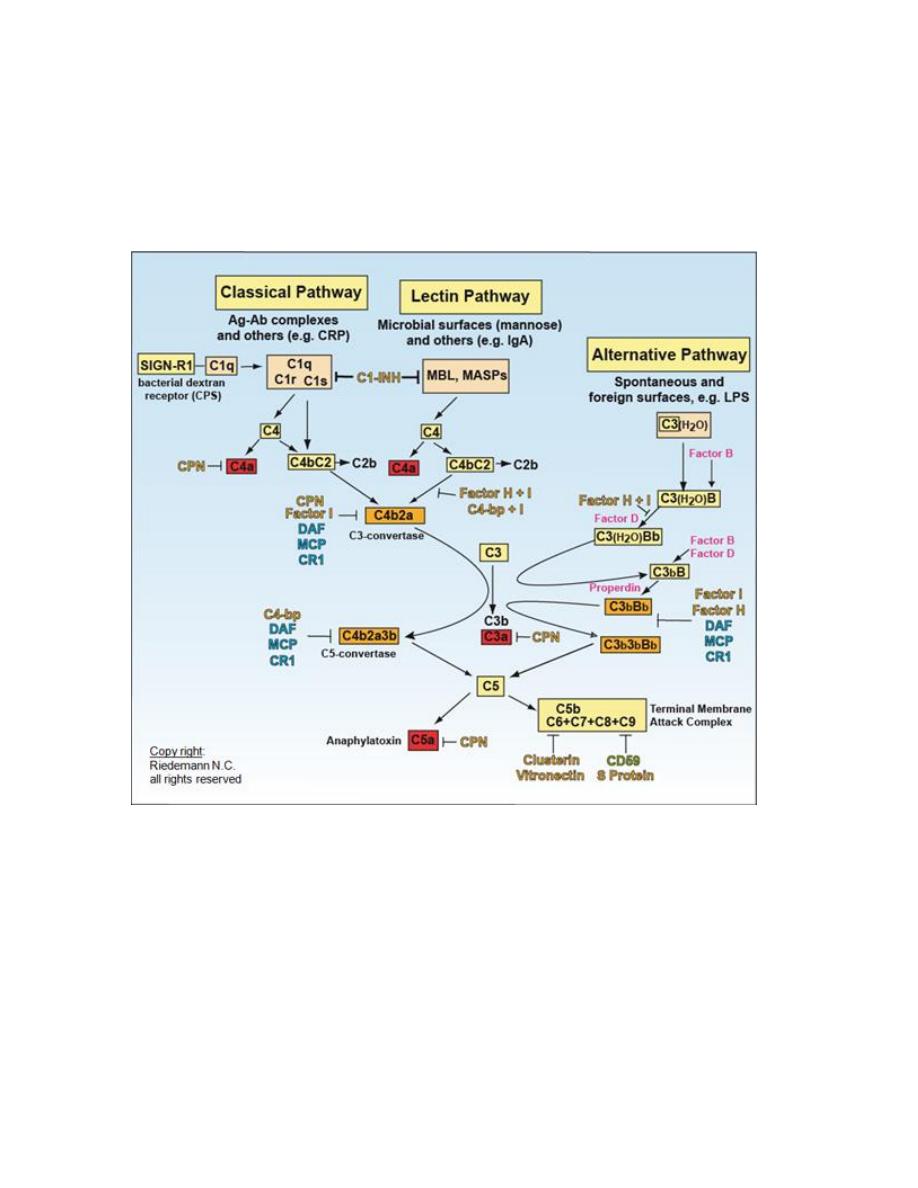
Complement
The complement system comprises a series of at least 20 glycoproteins that are
activated in a cascade sequence, with proenzymes that undergo sequential proteolytic
cleavage to their active forms. It is a major part of the innate immune system
Complement pathway.
Three main pathways of complement activation exist, termed the classical, alternative
and mannan-binding lectin (MBL) pathway.
The complement pathways are triggered by different factors:
¡
Classical pathway
by antigen-antibody immune complexes, apoptotic cells, C-
reactive protein bound to ligand and certain viruses and bacteria.
¡
Alternative pathway
by bacterial endotoxin, fungal cell walls, viruses and tumour
cells.
¡
Mannan-binding lectin (MBL) pathway
is activated by microbes with terminal
mannose groups
[
6
]
Complement activation is focused at cell membranes. Host cells are protected from
complement-mediated lysis by
inhibitory surface molecules
, for example decay
accelerating factor (DAF). Most organisms lack any protective molecules and are
therefore susceptible to complement.
Functions of complement:
A.
Anti-infective function
:
1. opsonization by C3b and C4b
2. chemotaxis - attraction of phagocytes by chemoattractant activation products
3. activation of leucocytes by anaphylatoxins (C5a, C3a and C4a); via receptors on
leucocytes
4. lysis of bacteria and cells (C5b-C9).

[
7
]
B.
Interplay between innate and adaptive immune system
. Immunomodulation of B-
cell responses to specific antigen through binding of complement receptors on B-cell
surface, thus augmenting antibody responses and immunological memory.
C.
Clearance of:
- immune complexes (C1q, C3 and C4)
- apoptotic cells (C1q, C3 and C4).
ADAPTIVE (SPECIFIC OR ACQUIRED) IMMUNITY
Consist of
-
cellular(T –lymphocyteand B- lymphocyte
)
1-
-
humeral (AntibodY
)
2-
Antigen-specific receptor:
.
Innate immunity is a rapid non-specific response
whereas in adaptive immunity The characters of this response are:
1. the use of antigen-specific receptors on T lymphocytes (T-cell receptor, TCR) and B
lymphocytes to direct the response.(response is very focused)
2. The response takes time to develop so that it cannot provide immediate protection
on first meeting an antigen.
3. the development of memory CELL so that subsequent exposure leads to a more rapid
response
4. Phagocytes only recognize extracellular organisms, mostly bacteria. In contrast,
T cells are able to combat intracellular infections, such as viruses, bacteria
(mycobacteria, legionella, listeria, brucella, salmonella), many fungi and protozoa.
B CEL immunoglobulin producing cell,identified by present of I.G on their surface.
These cells comprise approximately 25% of lymphocytes. B cells divide and are activated
to become plasma cells which secrete large amounts of antibody.
Sara Abdulbasit
