LEC 1:
.ا
م
.
د
.
حسن
الجميلي
Liver and biliary tract disease
Introduction:
Liver cells
Hepatocytes comprise 80% of liver cells. The
remaining 20% are the endothelial cells
lining the sinusoids ,epithelial cells lining the
intrahepatic bile ducts, cells of the immune
system (including macrophages (Kupffer
cells)

Hepatic function
1-Carbohydrate, amino acid and lipid metabolism
•Amino acids from dietary proteins are used for synthesis of
plasma proteins, including albumin.The liver produces 8–14 g of
albumin per day..
• Following a meal, more than half of the glucose absorbed is taken
up by the liver and stored as glycogen --preventing hyperglycaemia.
During fasting, glycogen is broken down to release glucose
(gluconeogenesis), thereby preventing hypoglycaemia
• The liver plays a central role in lipid metabolism, producing VLDL
and further metabolising LDL &HDL .Dysregulation of lipid
metabolism is thought to have a critical role in the pathogenesis of
NAFLD.

2-Clotting factors
The liver produces key proteins that are involved
in the coagulation cascade. Reduced clotting
factor synthesis is an important and easily
accessible biomarker of liver function in the
setting of liver injury.
Prothrombin time (PT or INR) is therefore one of
the most important clinical tools available for the
assessment of hepatocyte function.
.

3-Storage of vitamins and minerals
Vitamins A, D and B12 are stored by the liver in large
amounts, while others, such as vitamin K and folate, are
stored in smaller amounts and disappear rapidly if dietary
intake is reduced.
The liver is also able to metabolise vitamins to more
active compounds, e.g. 7-dehydrocholesterol to 25(OH)
vitamin D.
Vitamin K is a fat-soluble vitamin and so the inability to
absorb fat soluble vitamins, as occurs in biliary
obstruction, results in a coagulopathy.
The liver stores minerals such as iron, in ferritin and
haemosiderin, and copper, which is excreted in bile.

4-Immune regulation
Approximately 9% of the normal liver is
composed of immune cells . Kupffer cells
derived from blood monocytes, the liver
macrophages and natural killer (NK)cells, as
well as ‘classical’ B and T cells
. They remove aged and damaged red blood
cells, bacteria, viruses, antigen–antibody
complexes and endotoxin
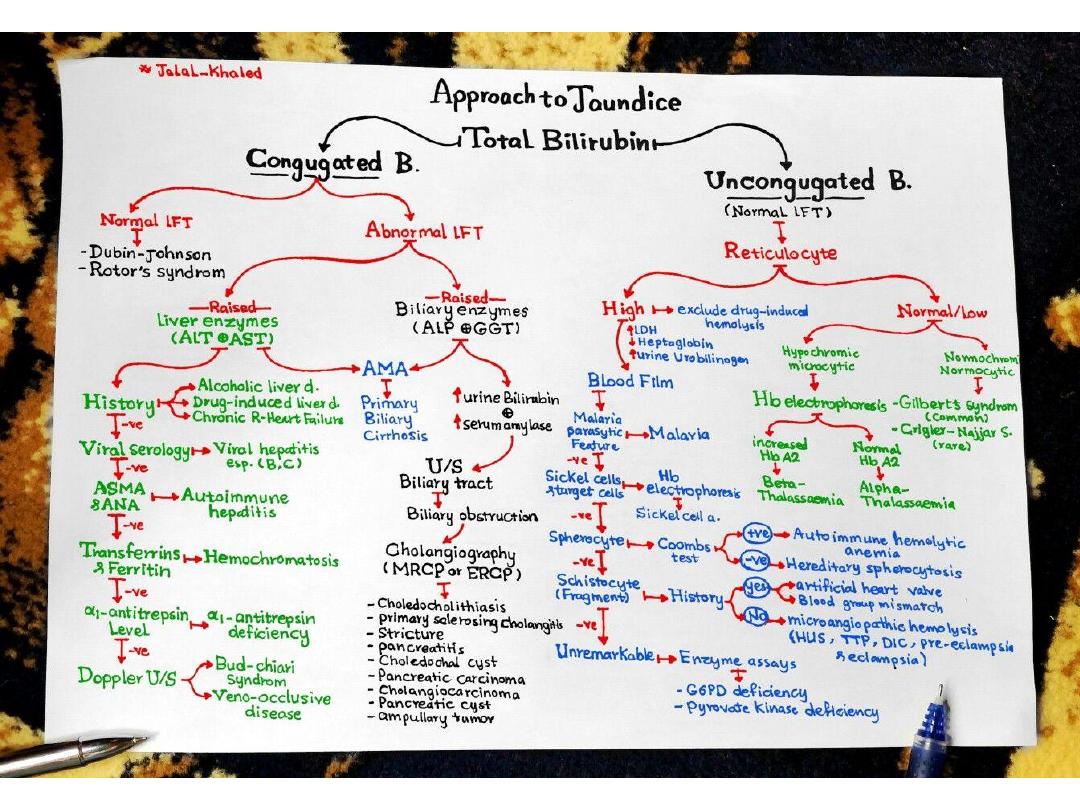
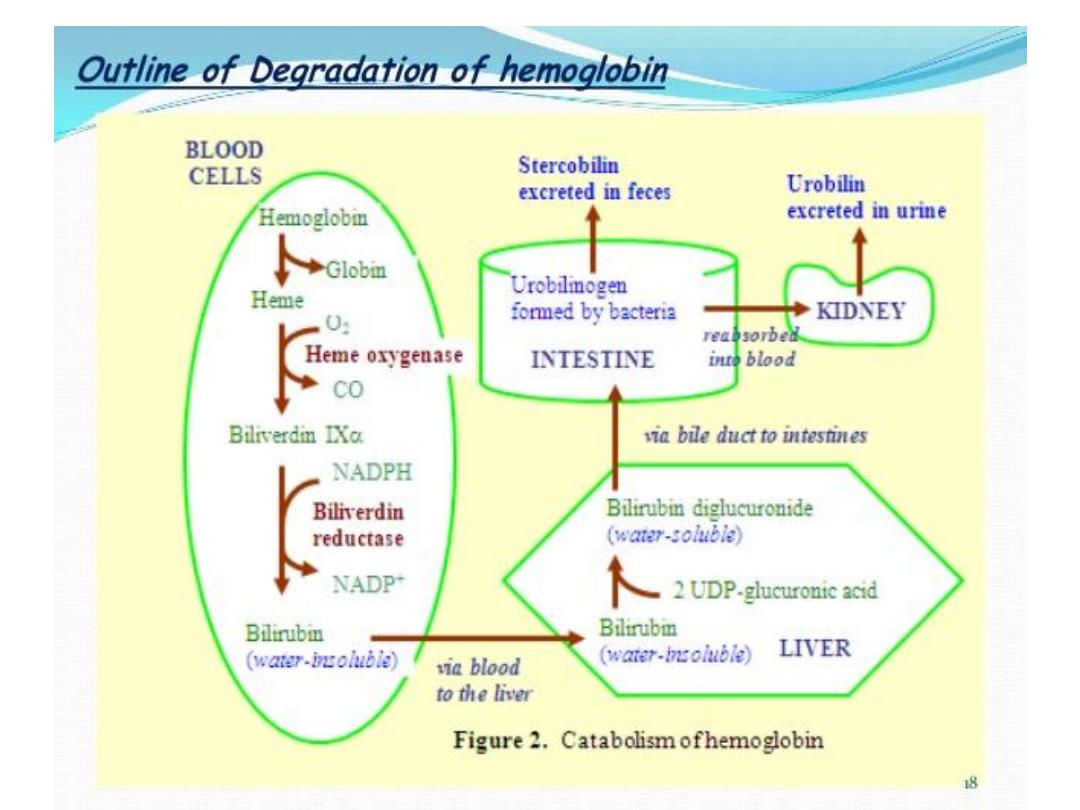
5-billrubin and bile metabolism:
Bile contains bile acids ,phospholipids
,bilirubin and cholesterol
Investigations
1- Bilirubin and albumin
The degree of elevation of bilirubin can reflect the degree
of liver damage. A raised bilirubin often occurs earlier in
the natural history of biliary disease (e.g. primary biliary
cirrhosis) than in disease of the liver parenchyma (e.g.
cirrhosis) where the hepatocytes are primarily
involved.
Serum albumin levels are often low in patients with liver
disease.. Since the plasma half-life of albumin is about 2
weeks, albumin levels may be normal in acute liver failure
but are almost always reduced in chronic liver failure.
2-Alanine aminotransferase (ALT) and aspartate
aminotransferase (AST) :
are located in the cytoplasm of the hepatocyte; Although
both transaminase enzymes are widely distributed,
expression of ALT outside the liver is relatively low and
this enzyme is therefore considered more specific for
hepatocellular damage.
Large increases of aminotransferase activity favour
hepatocellular damage, and this pattern of LFT
abnormality is known as ‘hepatitic’
3-Alkaline phosphatase and gamma-glutamyl transferase :
(ALP) is widely distributed in the body, but the main sites of
production are the liver, gastrointestinal tract, bone, placenta and
kidney, levels rise with intrahepatic and extrahepatic biliary
obstruction and in infiltrative liver disease.
(GGT) is a microsomal enzyme found in many cells and tissues of
the body. The highest concentrations are located in the liver
-The pattern of a modest increase in aminotransferase activity
and large increases in ALP and GGT activity favours biliary
obstruction and is commonly described as ‘cholestatic’ or
‘obstructive’ .
Isolated elevation of the serum GGT is relatively common, and may
occur during ingestion of microsomal enzyme-inducing drugs,
including alcohol ,but also in NAFLD.

4-Other biochemical tests
• Hyponatraemia occurs in severe liver disease due
to increased production of ADH
• Serum urea may be reduced in hepatic failure,
whereas levels of urea may be increased following
GI haemorrhage.
• Significantly elevated ferritin suggests
haemochromatosis. Modest elevations can be seen
in inflammatory disease and alcohol excess.
5-Haematological tests
•
A normochromic normocytic anaemia
-gastrointestinal
haemorrhage,
chronic blood loss is characterised by a hypochromic microcytic
anaemia secondary to iron deficiency.
-(macrocytosis) is associated with alcohol misuse,
•
Leucopenia
may complicate portal hypertension and
hypersplenism, whereas leucocytosis may occur with cholangitis,
alcoholic hepatitis and hepatic abscesses.
. •
Thrombocytopenia
--due to reduced platelet production,
hypersplenism. Thrombopoietin, required for platelet production,
is produced in the liver and levels fall with worsening liver function.
A low platelet count is often an indicator of chronic liver disease,
Thrombocytosis is unusual in patients with liver disease but may
occur in those with active GI haemorrhage and, rarely, in
hepatocellular carcinoma
.
6-Coagulation tests
vitamin K-dependent coagulation factors (1972)in
the blood are short (5–72 hours) and so
changes in the prothrombin time occur relatively
quickly following liver damage. An increased PT is
evidence of severe liver damage in chronic liver
disease.
Vitamin K does not reverse this deficiency if it is
due to liver disease, but will correct the PT if the
cause is vitamin K deficiency, as may occur with
biliary obstruction due to non-absorption of fat-
soluble vitamins.

7-Immunological tests
- Elevation in overall serum
immunoglobulin levels can also be
suggestive of autoimmunity
(immunoglobulin (Ig)G and IgM).
-Elevated serum IgA can be seen, often
in more advanced
alcoholic liver disease and NAFLD

8- Ultrasound
a ‘first-line’ test to identify gallstones, biliary
obstruction or thrombosis in the hepatic
vasculature.
Focal lesions, such as tumours, may not be
detected if they are below 2 cm in diameter and
have echogenic characteristics similar to normal
liver tissue.
. Doppler ultrasound allows blood flow in the
hepatic artery, portal vein and hepatic veins to be
investigated.
Endoscopic ultrasound provides high-resolution
images of the pancreas, biliarytree and liver

9-
(CT) detects smaller focal lesions in the
liver, especially when combined with
contrast injection .
(MRI) can also be used to localise and
confirm the aetiology of focal liver
lesions, particularly primary and
secondary tumours
10-Cholangiography
(MRCP)& ERCP, or the percutaneous
approach (percutaneous
transhepatic cholangiography, PTC).
The latter does not allow the
ampulla of Vater or pancreatic duct
to be visualised
.
11-liver biopsy can confirm the severity of liver damage and
provide aetiological information.
It is performed percutaneously with a Trucut or Menghini
needle, usually through an intercostal space under local
anaesthesia, Percutaneous liver biopsy is a relatively safe
procedure.
mortality of about 0.01%. The main complications are
abdominal and/or shoulder pain, bleeding and biliary
peritonitis.
liver disorders can be broadly classified histologically
into fatty liver (steatosis), hepatitis (inflammation,
‘grade’) and cirrhosis (fibrosis, ‘stage’).

12-Non-invasive markers of hepatic fibrosis
***Serological markers of hepatic fibrosis, such as α2-
macroglobulin, haptoglobin.
The ELF®(Enhanced Liver Fibrosis) serological assay uses a
combination of hyaluronic acid, procollagen peptide III
(PIIINP) and tissue inhibitor of metalloproteinase 1
(TIMP1). These tests are good at differentiating severe
fibrosis from mild scarring, but are limited in their ability
to detect subtle changes.
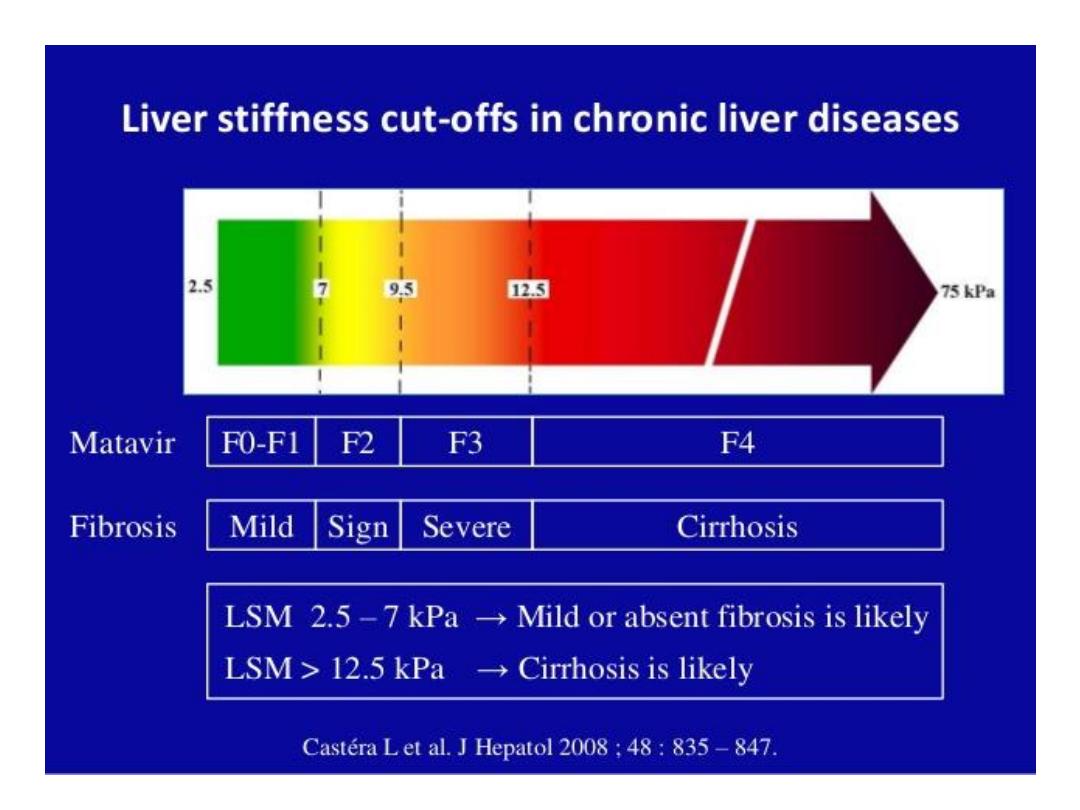
-***fibroscan.:
elastography in which ultrasound-based shock waves are
sent through the liver to measure liver stiffness as a
surrogate for hepatic fibrosis.