Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
1
Bone imaging
( Bone Lesions)
Primary Malignant Bony tumor
❖
Metastatic malignant tumors are by far the commonest bone neoplasm
❖
Radionuclide bone scans show substantially increased activity in the lesion.
❖
MRI is the most accurate technique for showing the extension into both the
medullary cavity and the soft tissues can be accurately defined, as can the
relationship to important nerves and blood vessels. MRI provides this information
better than CT
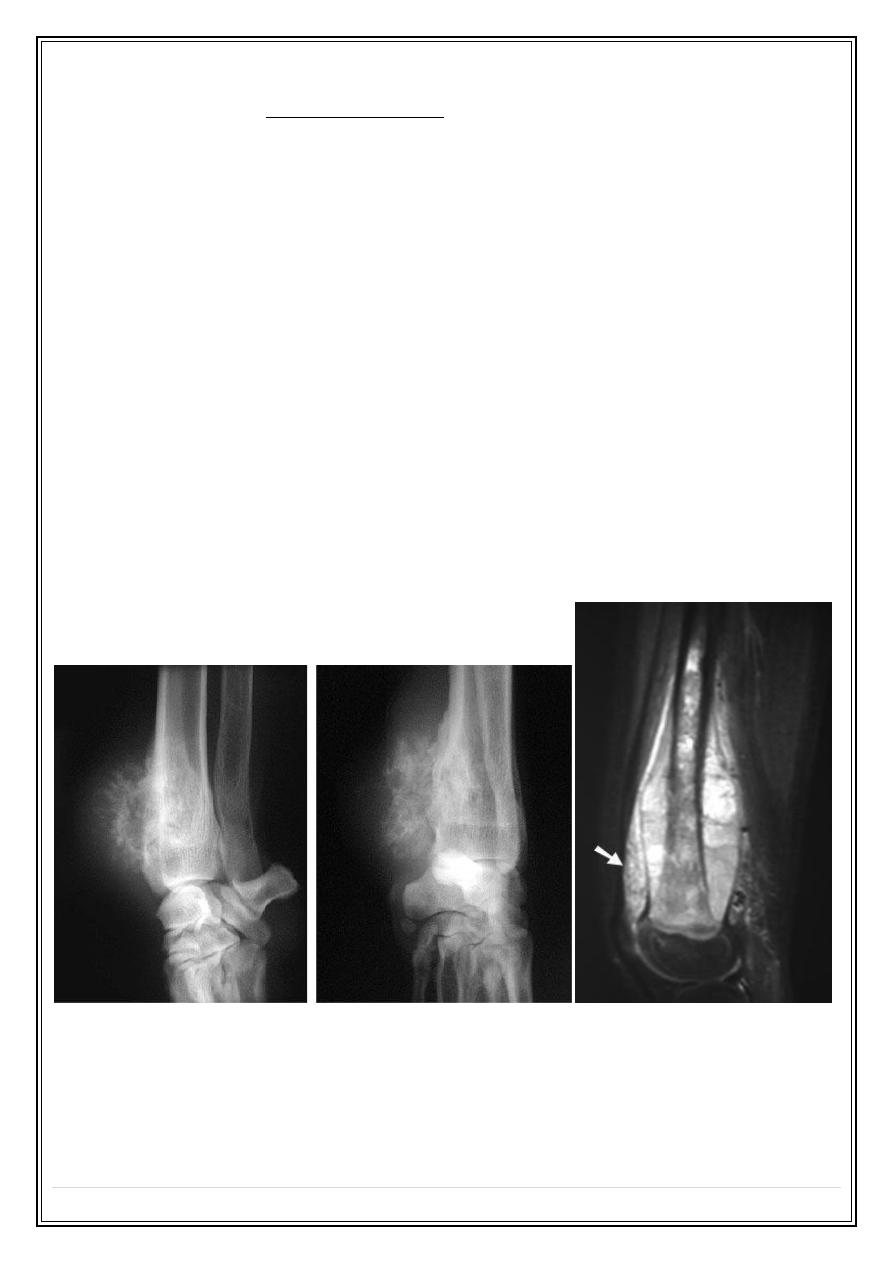
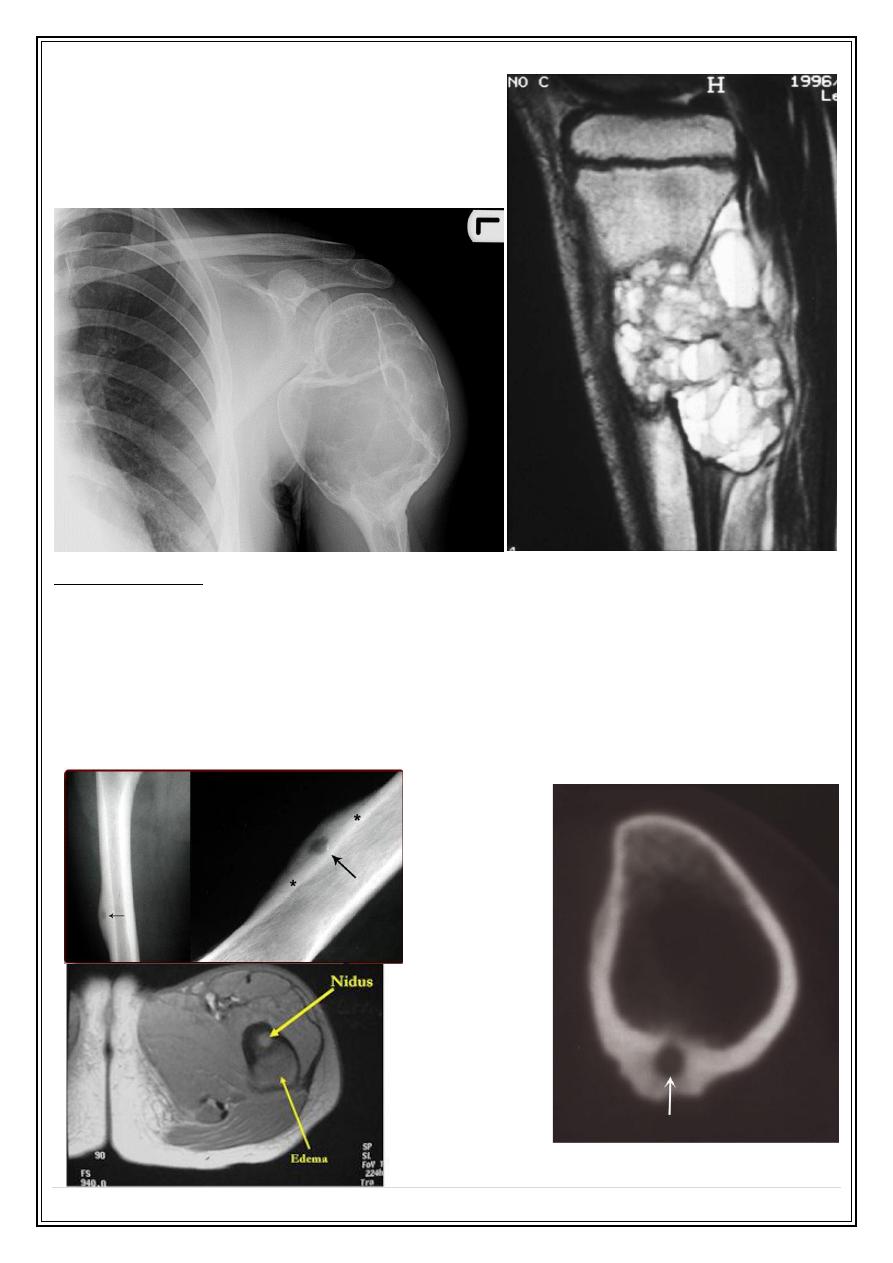
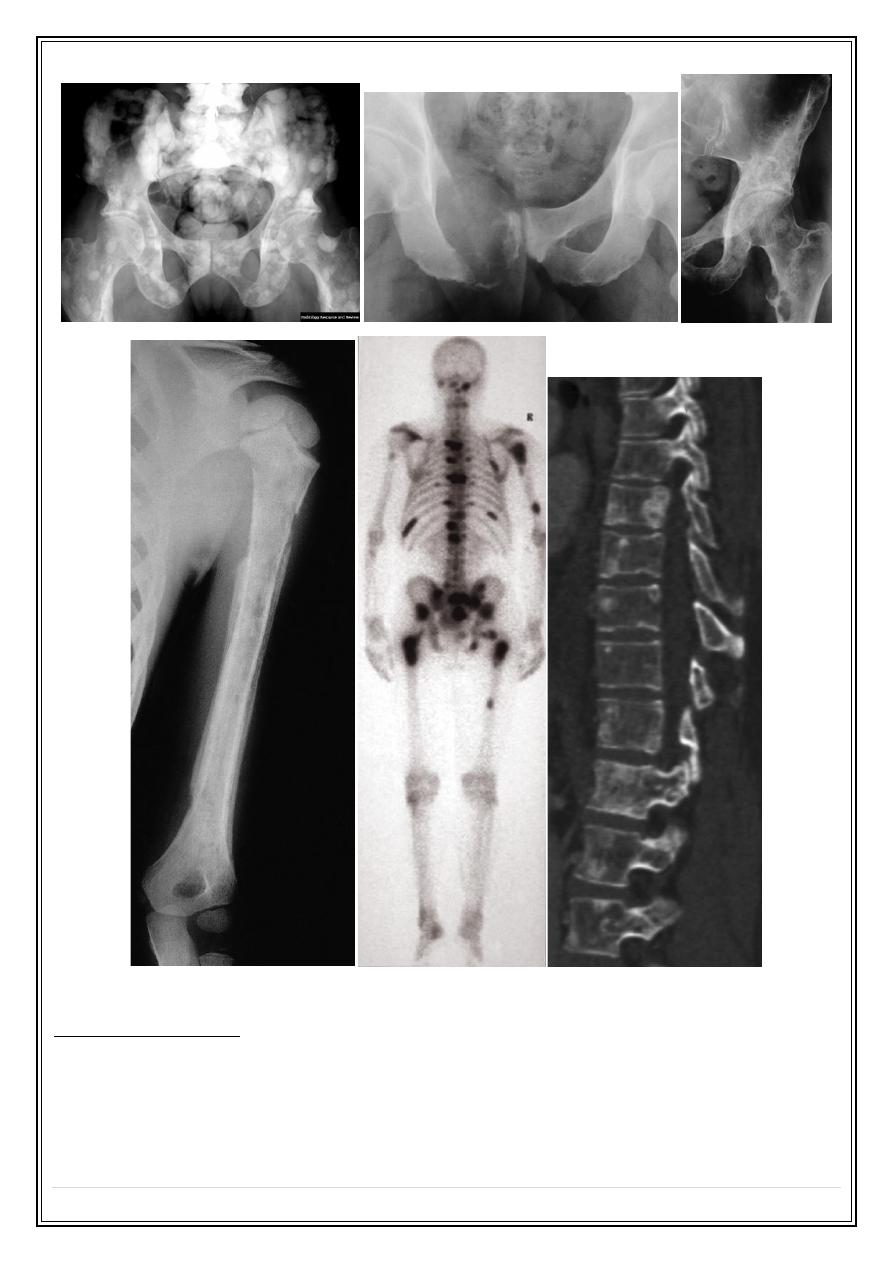
Osteosarcoma (osteogenic sarcoma)
❖
Occurs mainly in the 5–20-year-old age group, but is also seen in the elderly
following malignant change in Paget’s disease.
❖
The tumour often arises in a metaphysis, most commonly around the knee.
❖
Florid spiculated periosteal reaction is present, the so-called sunray appearance
❖
The tumour may elevate the periosteum to form a Codman’s triangle
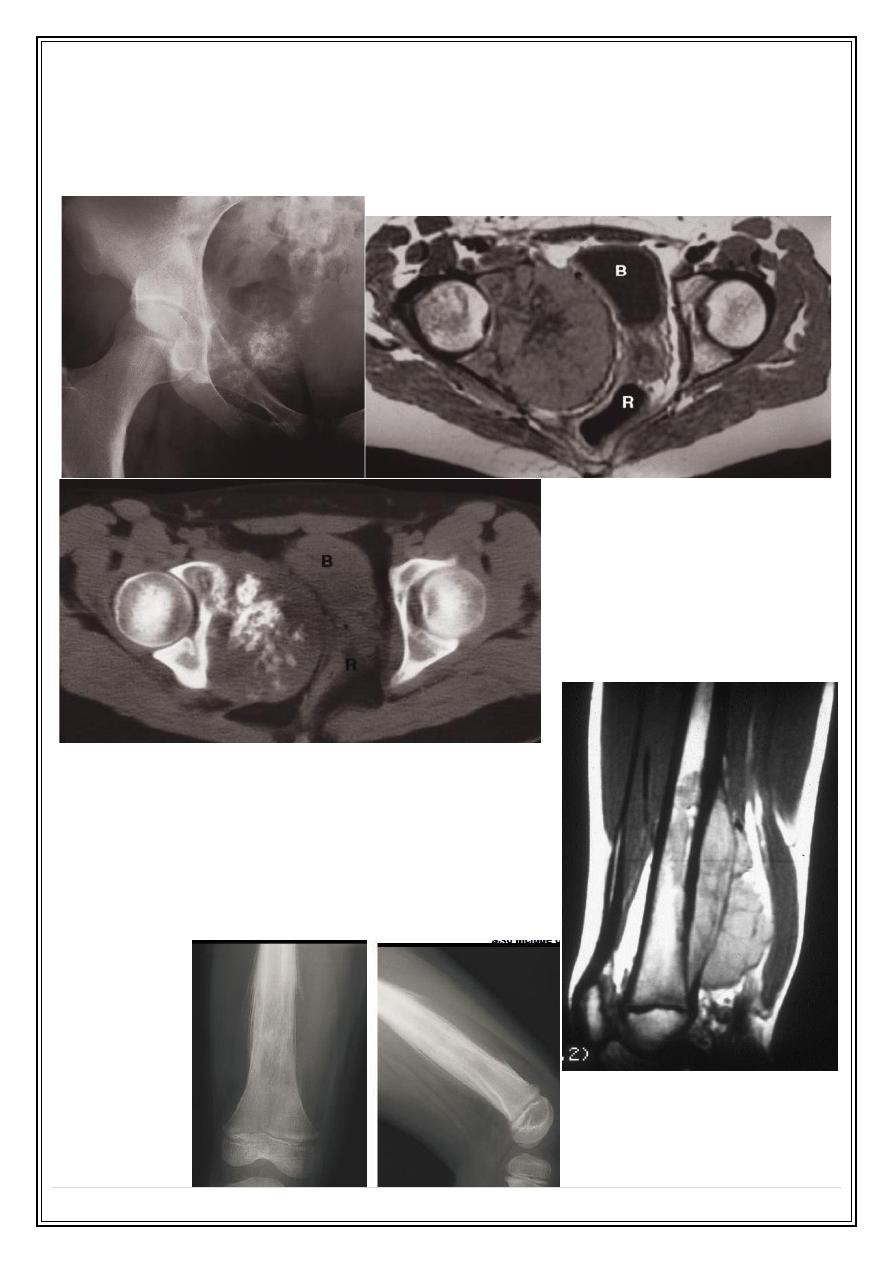
Chondrosarcoma
❖
30–50-year-old age group
❖
Most commonly in the pelvic bones, scapulae, humeri and femora.
❖
A chondrosarcoma produces a lytic expanding lesion containing flecks of calcium.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
2
❖
It can be difficult to distinguish from enchondroma, but it is usually less well
defined and may show a periosteal reaction.
❖
A chondrosarcoma may arise from malignant degeneration of a benign
cartilaginous tumour
Ewing’s sarcoma
A highly malignant tumour, commonest in
children
Arising in the shaft of long bones.
It produces ill-defined bone destruction with
periosteal reaction that is typically ‘onion skin’ in
type
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
3
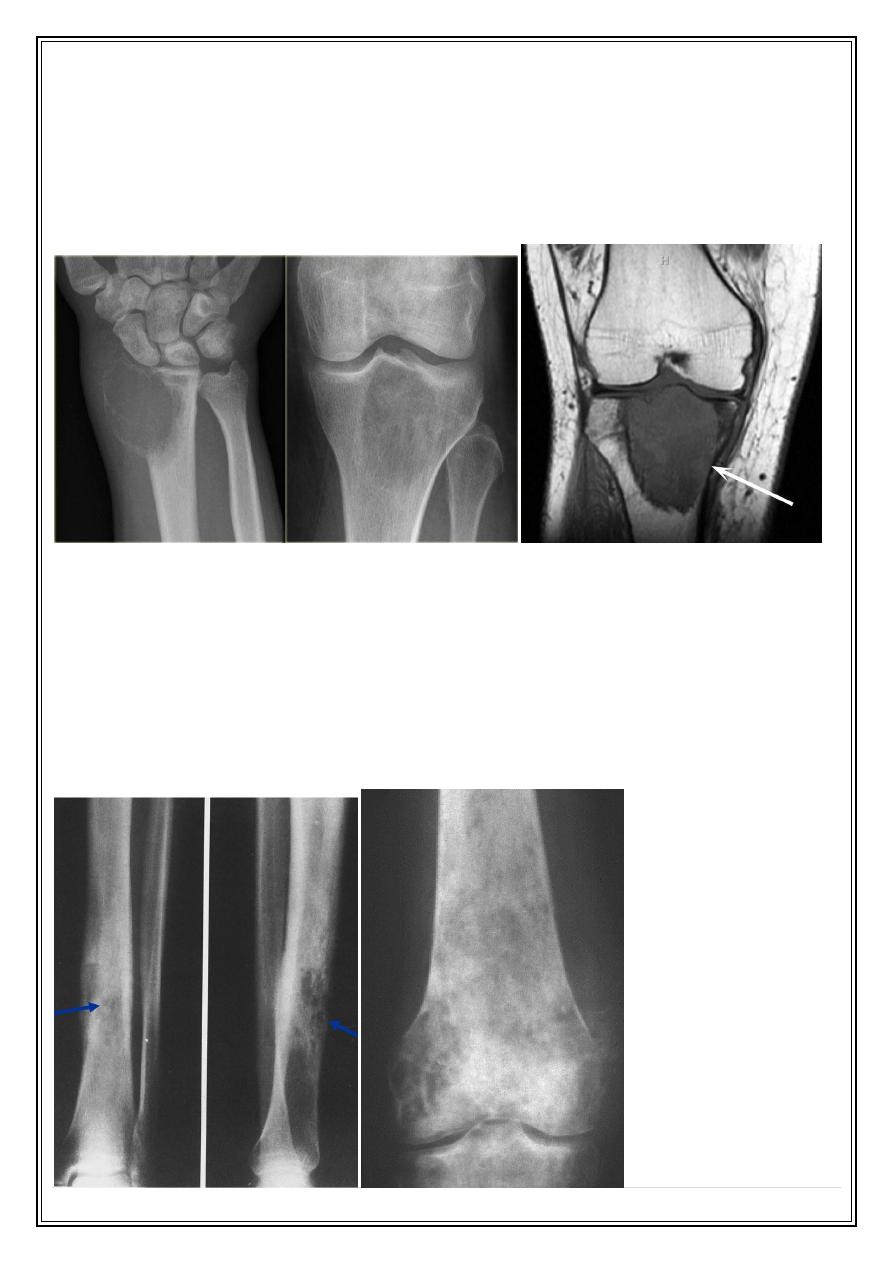
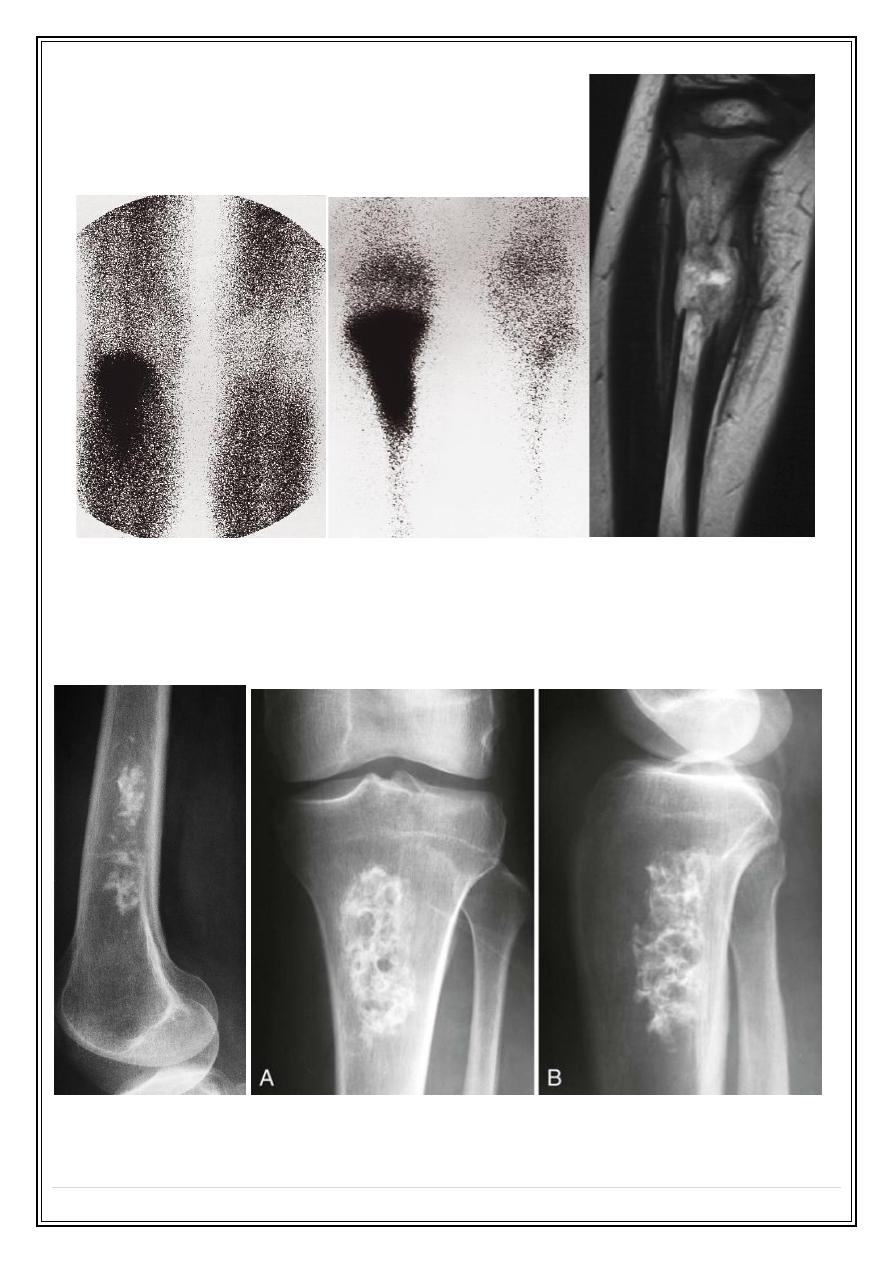
Giant cell tumour
❖
Has features of both malignant and benign tumours.
❖
It is locally invasive but rarely metastasizes.
❖
It occurs most commonly around the knee and at the wrist after the epiphyses
have fused. It is an expanding destructive lesion, which is subarticular in position
Primary lymphoma
❖
Bone involvement is rare
❖
Most osseous malignant lymphoma is associated with generalized lymph node
disease.
❖
When solitary primary lymphomas are encountered they may produce sclerotic or
lytic bone lesions
❖
Indistinguishable on imaging grounds from other malignant tumor

Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
4
Benign tumours and tumour-like conditions
❖
In general, benign lesions have an edge which is well demarcated from the normal
bone by a sclerotic rim.
❖
They cause expansion but rarely breach the cortex.
❖
There is no soft tissue mass and a periosteal reaction is unusual unless there has
been a fracture through the lesion.
❖
Radionuclide scans in benign tumours usually show little or no increase in activity,
provided no fracture has occurred.
Enchondromas:
❖
Are seen as lytic expanding lesions most commonly in the bones of the hand.
❖
They often contain a few flecks of calcium and frequently present as a
pathological fracture.
Fibrous cortical defects (non-ossifying fibromas):
❖
Are common chance findings in children and young adults.
❖
They produce well-defined lucent areas in the cortex of long Bones
Enchondroma
Fibrous cortical defects
Fibrous dysplasia
❖
May affect one or several bones.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
5
❖
Affects the long bones and ribs as a well defined lytic lesion and may expand the
bone.
❖
There may be a sclerotic rim around the lesion.
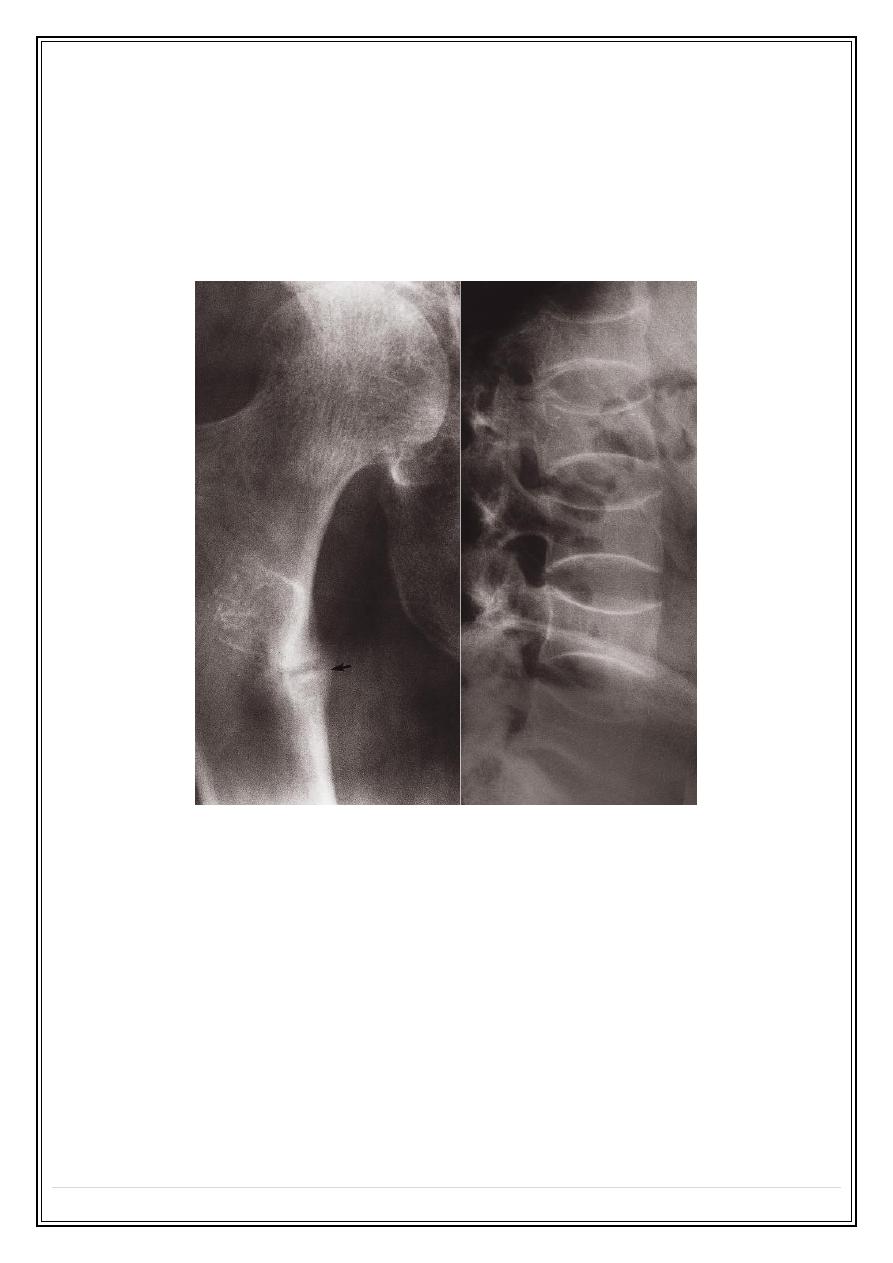
Simple bone cyst
❖
Has a wall of fibrous tissue and is filled with fluid.
❖
It occurs in children and young adults, most commonly in the humerus and femur.
❖
The cortex may be thin and the bone expanded.
❖
Pathological fracture.
Fibrous dysplasia
Simple bone cyst
Aneurysmal bone cysts
Mostly they are seen in children and young adults
❖
Affects the spine, long bones or pelvis.
❖
These lesions are purely lytic and cause massive expansion of the cortex, hence
the name ‘aneurysmal’. They may grow quickly and appear very aggressive but
are, nevertheless, benign lesions.
❖
Computed tomography and MRI may show the blood-fluid level within the cyst.
❖
The major differential diagnosis is from giant-cell tumour.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
6
Osteoid osteoma
❖
Is a painful condition found most commonly in the femur and tibia in young adults.
❖
Characteristic radiological appearance: a small lucency, sometimes with central
specks of calcification, known as a nidus, surrounded by dense sclerotic rim.
❖
A periosteal reaction may also be present.
❖
Radionuclide bone scanning: shows marked focal increased activity.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
7
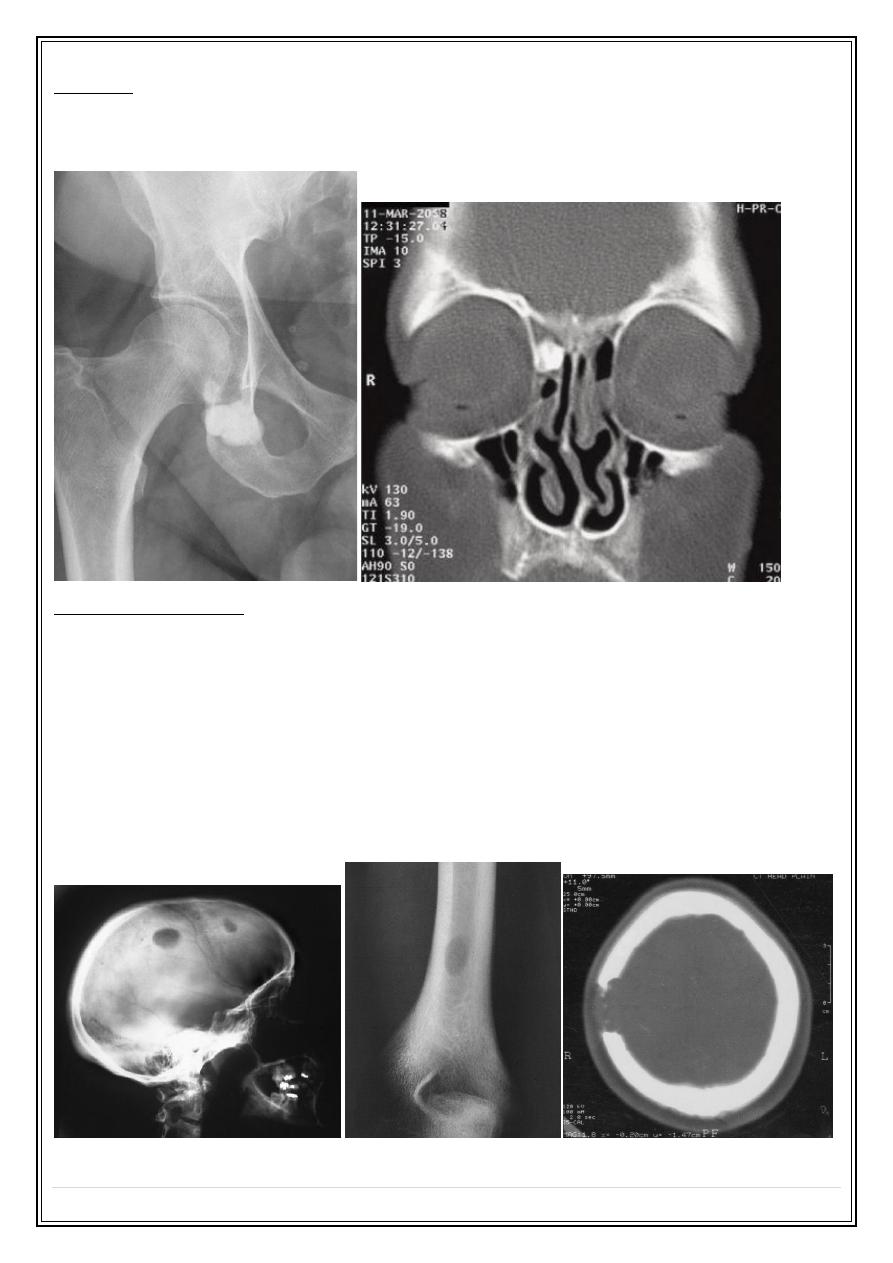
Osteoma
An is a benign tumour consisting of dense bone. They may occur in the paranasal
sinuses.
Eosinophil granuloma
Is the mildest and most frequent form of Langerhans histiocytosis.
It occurs in children and young adults
Lytic lesions which may be single or multiple, most frequently in the skull, pelvis,
femur and ribs.
May have the features of an aggressive lesion, or well defined and may have a
sclerotic rim.
A periosteal reaction is sometimes seen.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
8
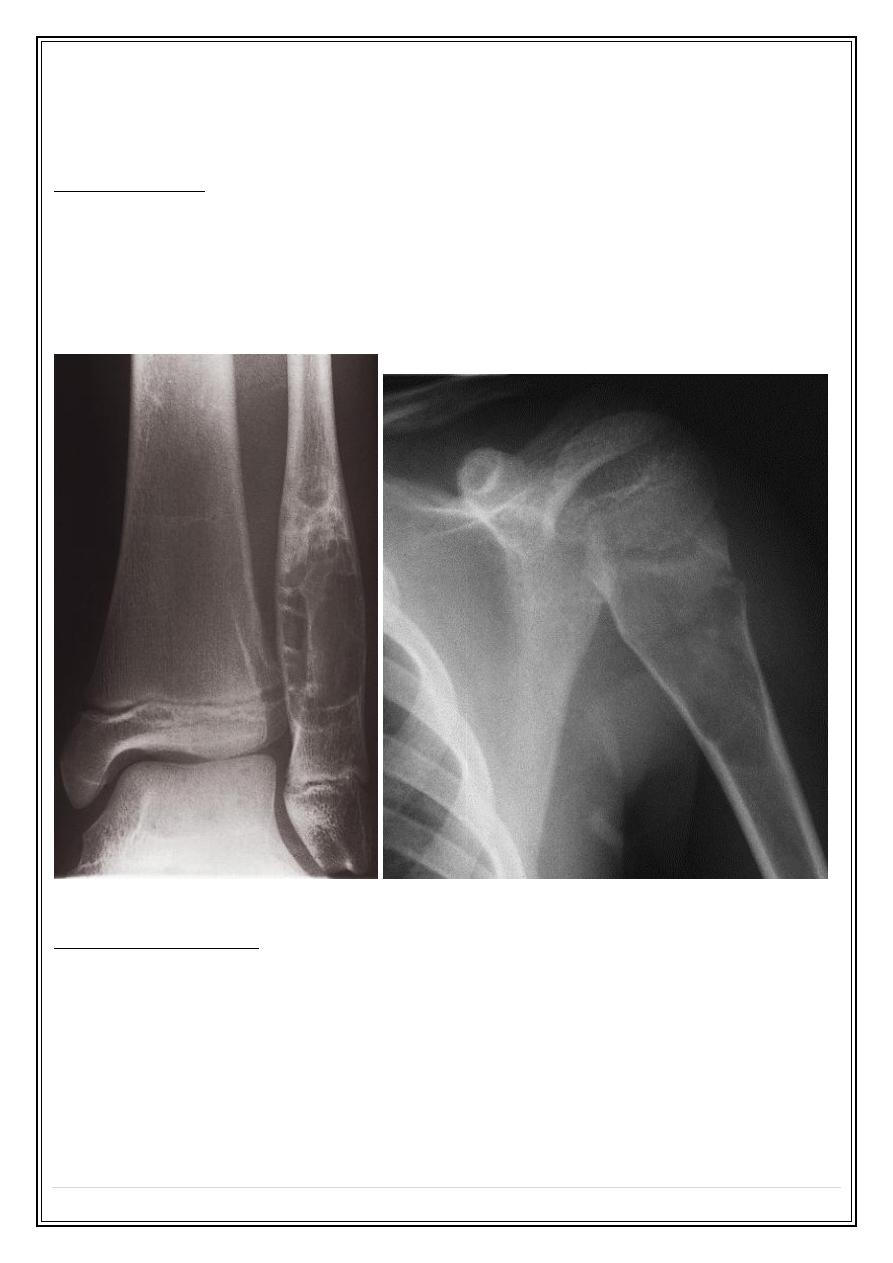
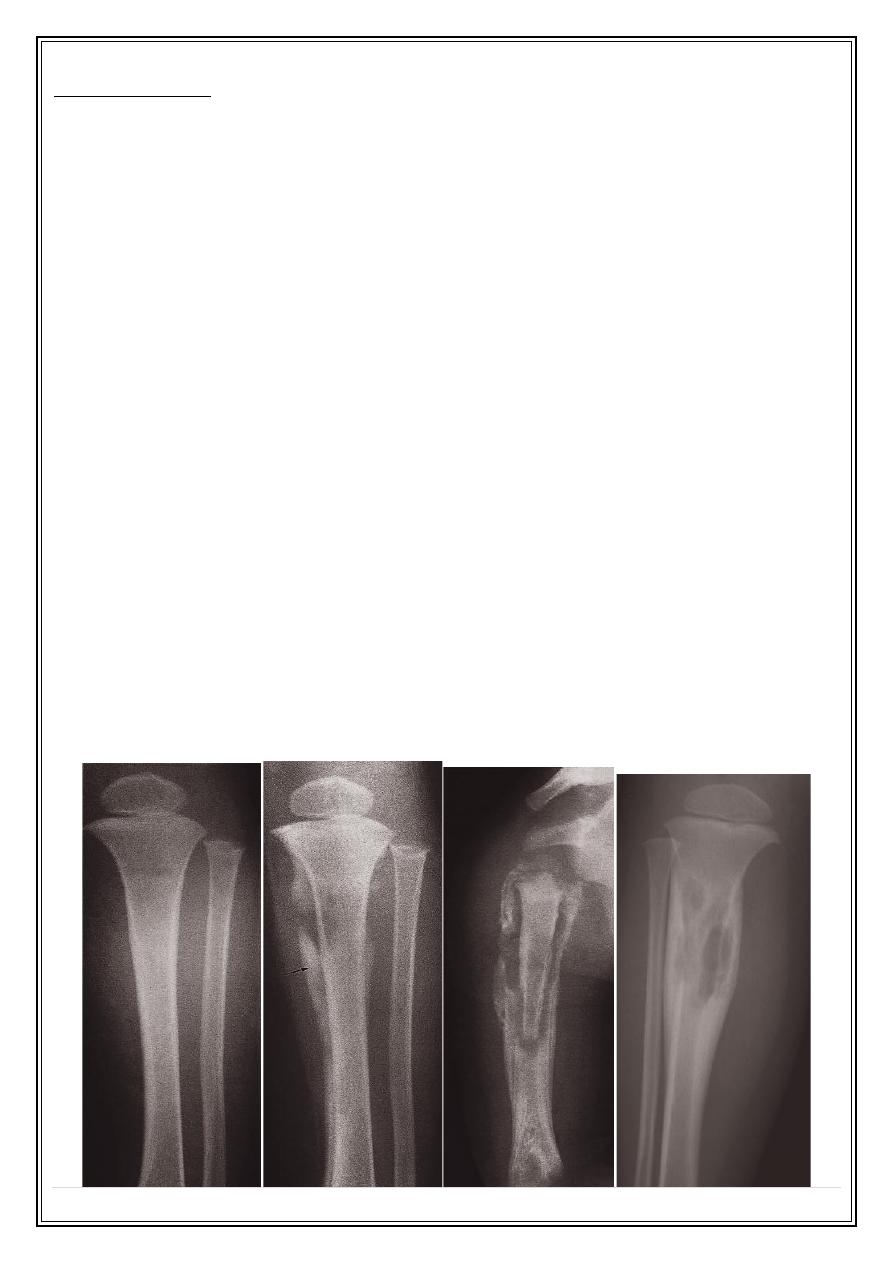
Osteomyelitis
Most often caused by Staphylococcus aureus and usually affects infants and
children.
The initial radiographs are normal as bone changes are not visible until 10–14
days after the onset of the infection, but the 99mTc radionuclide bone scan and
MRI show changes much earlier in the course of the disease within a day or two.
Typically, acute osteomyelitis affects the metaphysis of a long bone, usually the
femur or tibia.
The earliest signs on plain radiographs are soft tissue swelling and bone
destruction in the metaphysis, with a periosteal reaction that eventually may
become very extensive and surround the bone to form an involucrum.
A part of the original bone may die and form a separate dense fragment known as
a sequestrum.
In chronic osteomyelitis, the bone becomes thickened and sclerotic with loss of
differentiation between the cortex and the medulla. And may produce well defined
lytic lesion within the bone known as a Brodie’s abscess
Tuberculous osteomyelitis is a particular problem in African and Asian populations
and patients with AIDS.
The spine is the most frequent site of infection, followed by the large joints, but
any bone may be affected. The disease is relatively indolent and produces large
areas of bone destruction which, unlike pyogenic osteomyelitis, may be relatively
asymptomatic in the early stages.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
9
Bone infarction
Causes: caisson disease, sickle cell disease or following radiation therapy or seen
in elderly people without known cause
Once healed, they appear as irregular calcification in the medulla of a long bone
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
10
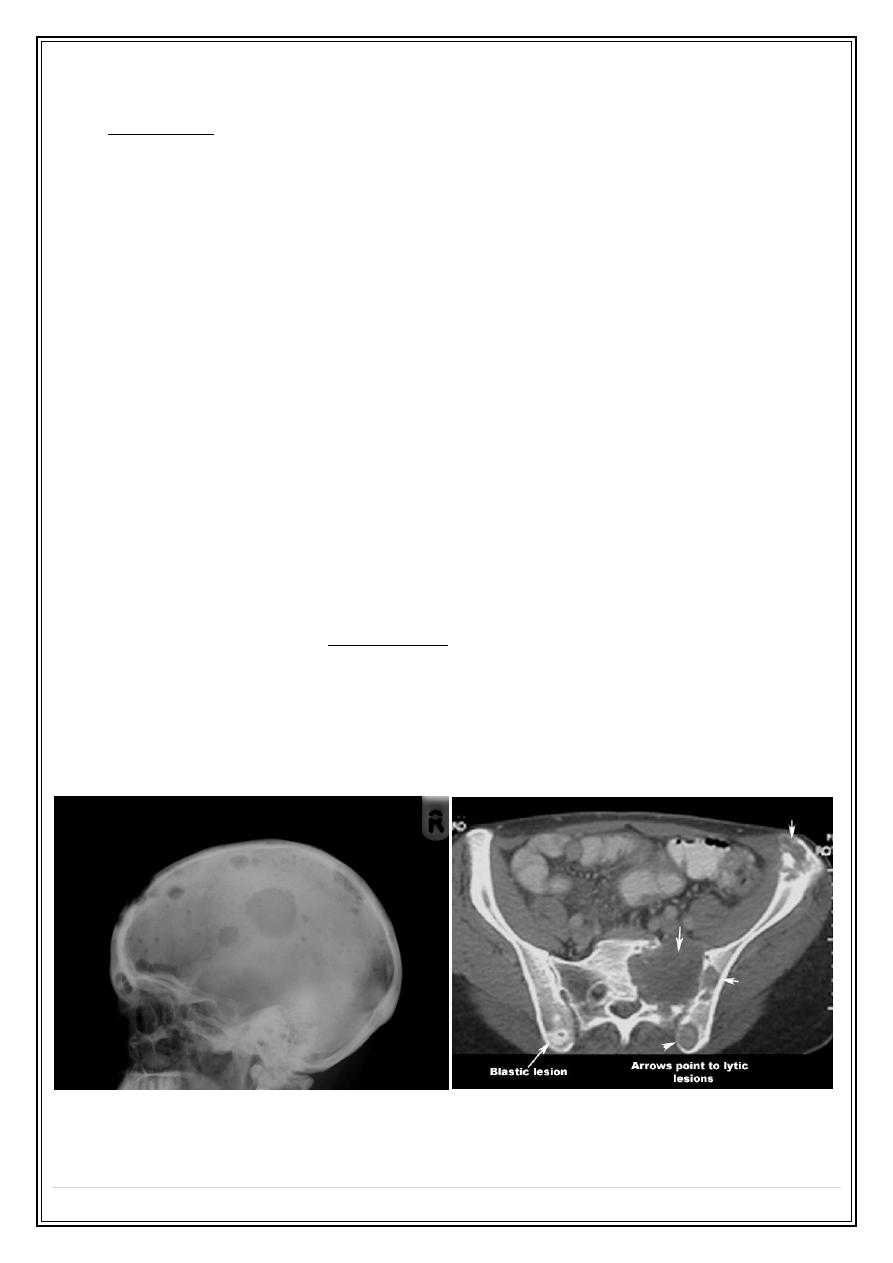
Multiple focal lesions
1. Metastases:
Commonest malignant bone tumour
Metastases may be sclerotic, lytic or a mixed.
Bones mostly affected are those containing red marrow: the spine, skull, ribs,
pelvis, humeri and femora.
Most of metastases are lytic
Metastases and myeloma are virtually the only causes of multiple obvious lytic
lesions in bone.
Sclerotic metastases: mainly from prostate CA in male and breast CA in female
Mixed lytic – sclerotic metastasis are mainly from breast CA.
Metastases with bone expansion occur in primary tumours of the kidney and
thyroid.
Neuroblastoma metastasis may cause periosteal reaction
Radionuclide bone scan: best modality, reveals 30% of lesions that are not
evident on X ray.
MRI: better sensitivity than radionuclide. Disadvantage?
CT scan: less sensitive than MRI, need bone window
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
11
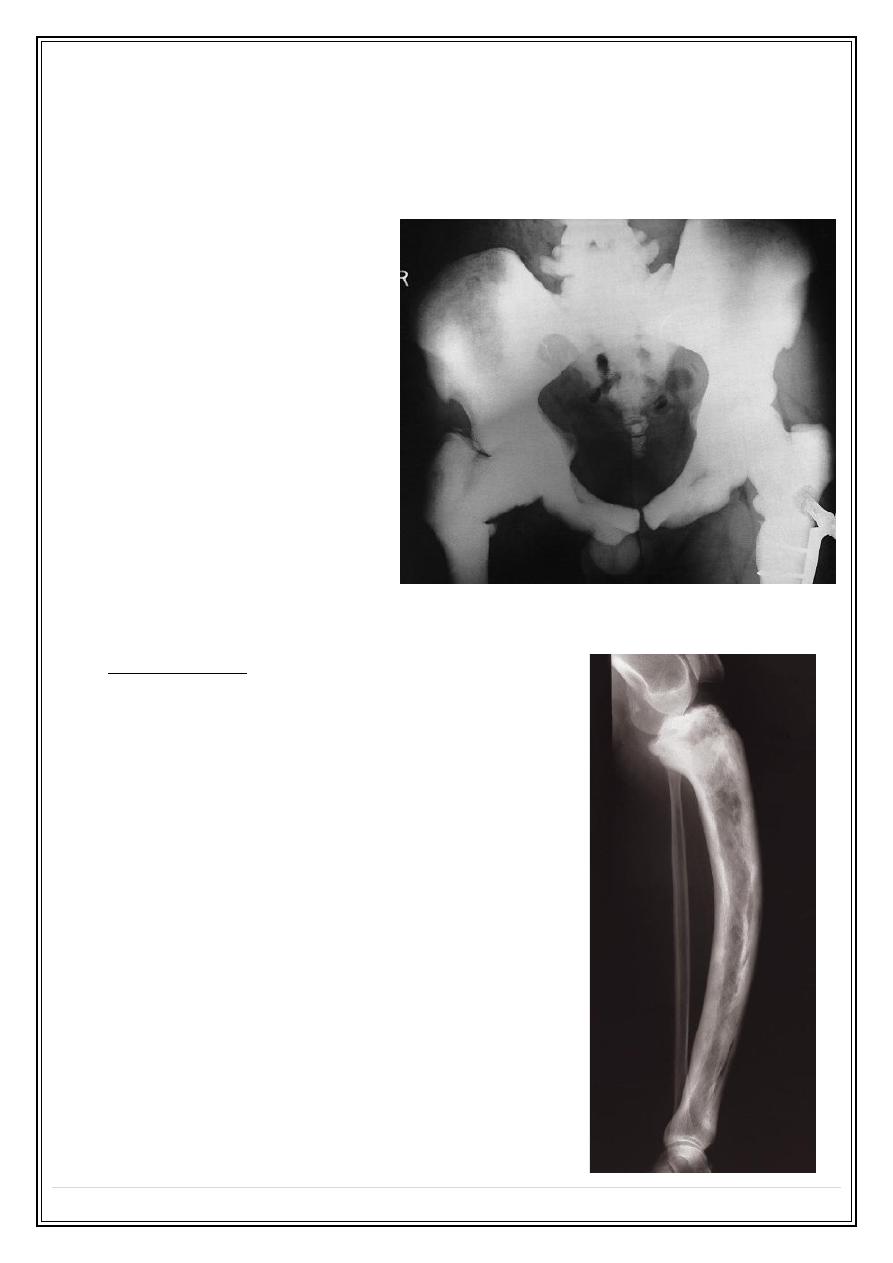
2- Multiple myeloma:
Most frequently seen in bones with active haemopoiesis.
The bone lesions may resemble lytic metastases in every way, but are often
better defined and may cause expansion of the bone

Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
12
Diffuse marrow involvement may give rise to generalized loss of bone density,
producing a picture similar to that of osteoporosis
Multiple periosteal reactions
1) Non-accidental injury
2) Widespread bone infection, e.g. congenital syphilis, neonates with infected
intravenous catheters
3) Venous stasis and ulceration of the legs
4) Hypertrophic pulmonary osteoarthropathy
5) Scurvy
chronic venous stasis
Hypertrophic pulmonary osteoarthropathy
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
13
Generalized decrease in bone density (osteopenia)
osteoporosis
osteomalacia
hyperparathyroidism
multiple myeloma
Osteoporosis
Osteoporosis is the consequence of a deficiency of protein
Osteoporosis predisposes to fractures
The changes of osteoporosis are best seen in the spine
Causes:
❖
idiopathic, often subdivided according to age of onset, e.g. juvenile,
postmenopausal, senile.
❖
Cushing’s disease and steroid therapy
❖
disuse.
Senile osteoporosis, penciled cortex
Disuse osteoporosis
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
14
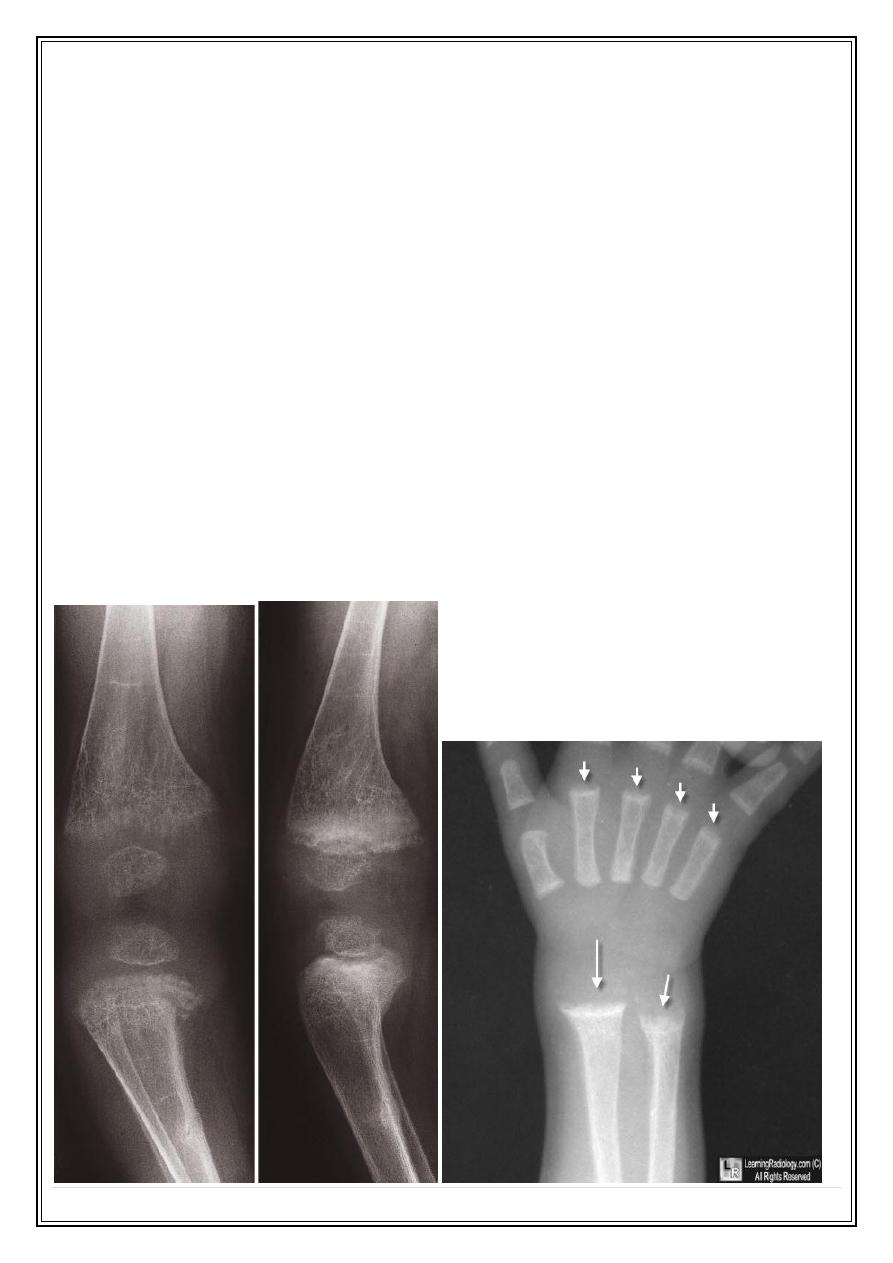
Rickets and osteomalacia
Poor mineralization of osteoid
The main causes:
Dietary deficiency of vitamin D, or lack of exposure to sunlight.
Malabsorption.
Renal disease.
Rickets
The changes are maximal where bone growth is occurring, so they are best seen
at the knees, wrists and ankles.
The zone of provisional calcification is deficient and the metaphyses are
irregularly mineralized, widened and cupped
Widened growth plate
Generalized decrease in bone density
Deformities of the bones
Greenstick fractures are common.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
15
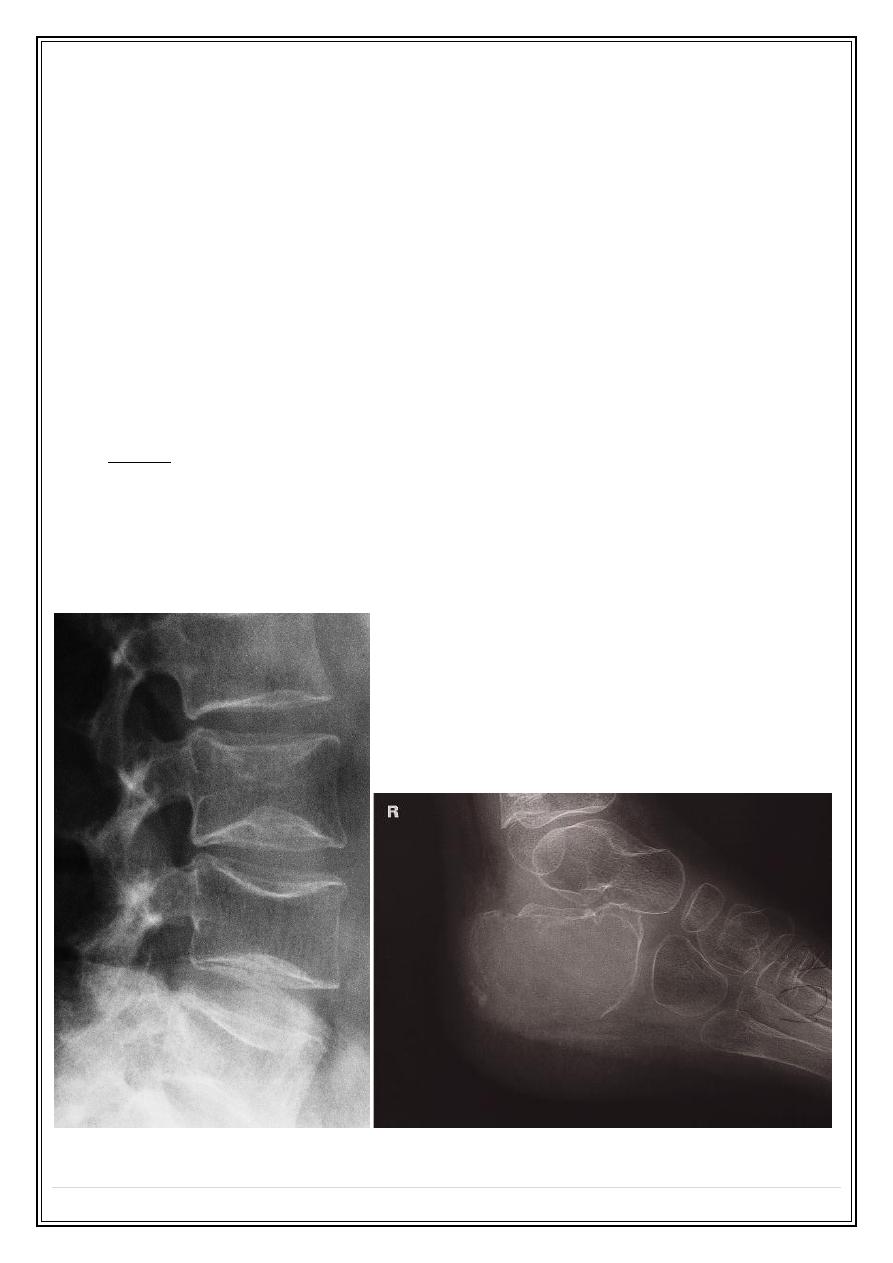
Osteomalacia
Loss of bone density
Thinning of trabeculae and cortex
Looser`s zones (pseudofractures): commonest in the scapulae, medial aspects of
the femoral necks and in the pubic rami.
Bone deformity: biconcave vertbebra. Bowing of long bones. Triradiate pelvis
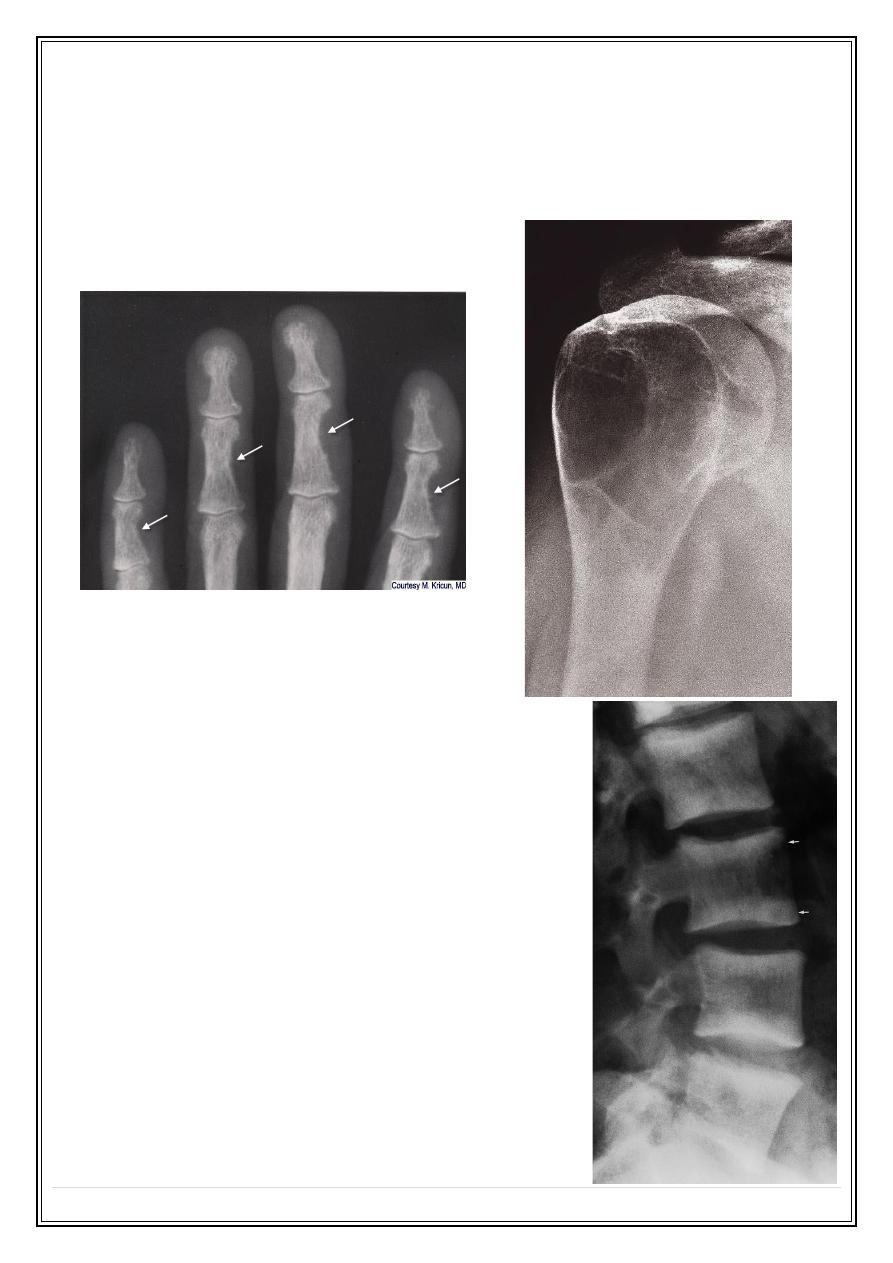
Hyperparathyroidism:
Excess parathyroid hormone secretion mobilizes calcium from the bones, resulting
in a decrease in bone
Primary: hyperplasia or a tumour of the parathyroid glands
Secondary: chronic renal failure
A generalized loss of bone density, with loss of the differentiation between cortex
and medulla. The trabecular pattern may have a fine lacework appearance. With
advanced disease there may be marked deformity of the skeleton.
The hallmark of hyperparathyroidism is subperiosteal bone resorption, particularly
at the radial side of the middle phalanges and at the tips of the terminal
phalanges.
There may also be resorption of the outer ends of the clavicles.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
16
Soft tissue calcification, vascular calcification and chondrocalcinosis: more in the
secondary type
Brown tumours: seen more in primary type. Lytic lesions, single or multiple, of
varying size and may be expensile. They occur most commonly in the mandible
and pelvis.
Renal osteodystrophy
Three distinct pattern of bony involvement:
Osteomalacia in adults; rickets in children
Hyperparathyroidism
Sclerosis, Rugger jersey spine or sclerosis of
the metaphyses of the long bones.
Rugger jersey spine (Renal osteodystrophy):
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
17
Generalized increase in bone density
Sclerotic metastases
Osteopetrosis (marble bone disease): congenital disease.
Myelosclerosis: is a form of myelofibrosis, replacement of bone marrow by fibrous
tissue. Splenomegally.
Osteopetrosis :
Alteration of trabecular pattern and change in shape
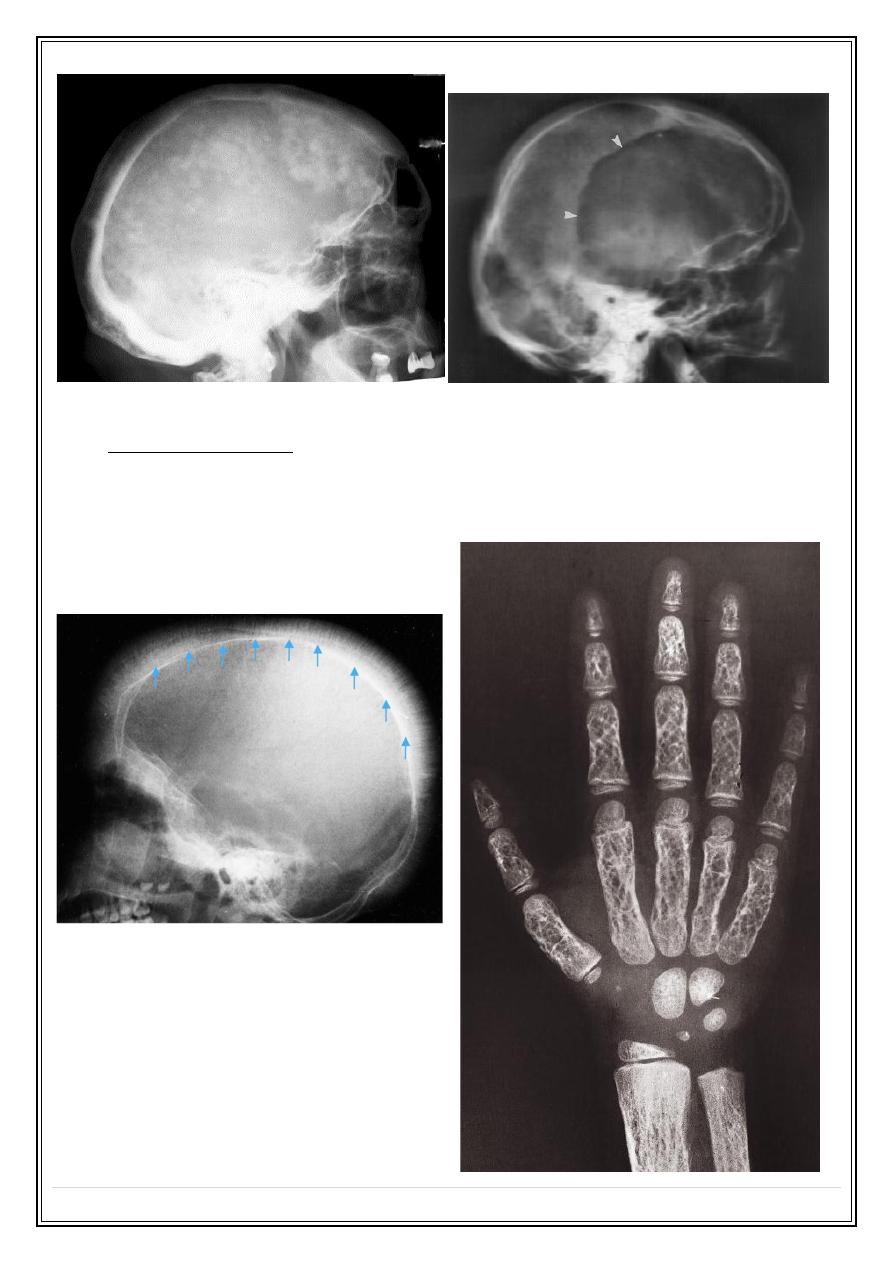
Paget disease:
Elderly
Thickening of trabecula. Enlargement of
affected bone, loss of CM differentiation.
Thickened calvarium with cotton wool
appearance.
One form is lytic: osteoporosis circumscripta of
skull.
Risk of malignant changes
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 2
P a g e
18
Hemolytic anemia:
Marrow hyperplasia: phalanges, skull: hair on end
Infarction and infection
Thank you,,,
