Dermatology Dr. Ahmed Abdulhussein Alhuchami
2019
Connective Tissue diseases:
Are groups of clinico pathological conditions involve connective tissue of most
systems of the body, include mainly LE, scleroderma, systemic sclerosis,
dermatomyositis, MCTD &others…
Lupus Erythematosus:
is an autoimmune disorder resulting from an interplay of genetic, environmental
&hormonal elements with a heterogeneous clinical expression extending from a
localized cutaneous form to a life threatening systemic form.
LE is a spectrum of diseases, in one end of spectrum: DLE is purely cutaneous LE, at
the other end :SLE. In the middle of spectrum: sub acute LE, neonatal LE, complement
deficiency LE& drug-induced LE .
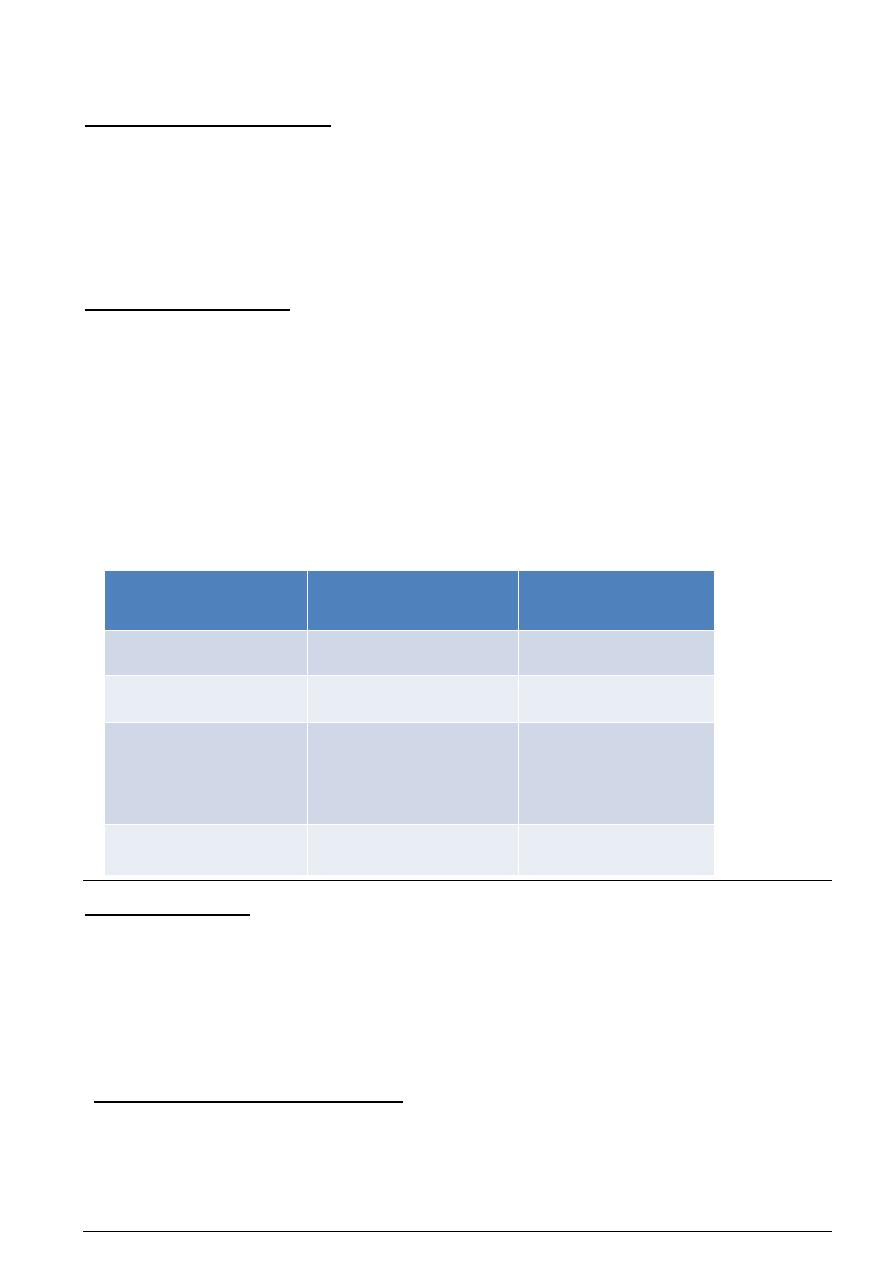
Types of lupus erythematosus
Chronic cutaneous
lupus
erythematosus(DLE)
Subacute cutaneous
lupus erythematous
(SCLE)
Acute cutaneous
lupus
erythematous(SLE)
Involve epidermis and
lower dermis
Involve epidermis and upper
dermis
Involve epidermis and upper
dermis
Don’t have systemic dis.(5-
10% develop SLE)
Majority don’t have systemic
disease
Systemic disease is present
Scarring , dyspigmentation,
atrophy and follicular
plugging is prominent
Skin lesions involve face,
scalp and ears but can be
widespread
Photosensitivity is
Prominent
Shawl distribution of skin
lesions(sun exposed areas)
Dx requires Require four
criteria out of eleven and
exclusion of drug-induced
SLE
F:M is 3:1
Anti-Ro(SSA)
Anti-La(SSB)
F:M is 6:1
ANA and anti-dsDNA and
anti-smith
:
Exacerbating factors
1. Ultraviolet light
2. Sex hormones
3. Stress
SLE criteria ( require 4 out of 11):
Creteria for classification of SLE:
1.Malar rash :fixed erythema over malar eminences, sparing nasolabial folds.
2.Discoid rash :erythematous raised patches with adherent keratotic scaling &follicular
plugging .
3.Photosensitivity :skin rash as a result of unusual reaction to sunlight .
4.Oral ulcer: usually painless.
5.Arthritis:non erosive arthritis involving 2 or more peripheral joints ,characterized by
tenderness, swelling or effusion .
6.Serositis:pleurisy or pricarditis.
7.Renal disorder: persistent proteinuria >0.5g/day or cellular casts.
8.Neurological disorder: seizure or psychosis .
9.Hematological disorder: Hemolytic anemia ,leucopenia<4000/mm3, lymphopenia
<1500/mm3, or thrombocytopenia less than 100.000/mm3.
10.Immunological disorder:
anti-DNA, anti-Sm, antiphospholipid antibodies
11.Abnormal antinuclear Ab titer
Drug-induced SLE:
It is different from idiopathic SLE by presence of anti-histone antibodies instead of ANA
Most commonly implicated drugs:
Procainamide, hydralazine, minocycline, INH, penicillamine and TNF-alpha inhibitors
Diagnosis:
Hx e.g joint pain and swelling, worsening or appearance of skin lesions with sun exposure,
weight loss, fever( which indicates systemic involvement), Hx of drugs
Physical exam: scar, follicular plug, dyspigmentation , oral ulcer, pleural or pericardial rub,
Investigations: CBC ( decreased WBC, RBC or platelets), ESR(high in SLE), urinalysis ( cast or
protein), ANA (sensitive but not specific)
If ANA is positive go to specific autoantibodies e.g. anti-dsDNA for SLE
Treatment:
Topical: Sun protection, topical and intralesional steroids
Systemic: Antimalarial e.g. hydroxychloroquine, chloroquine

Morphea
Affect female more than male
Does not affect survival but can cause a disability especially the linear type
Fibroblast isolated from morphea lesion produce increased amount of collagen and this is
thought to be due to production of IL-4 and TGF-β by T-cells
Some believes that Borrelia plays a role
Clinical types:
1. Plaque-type : present as shiny indurated plaque surrounded by lilac border
2. Deep morphea: invlove deep dermis, subcutis +/- fascia
3. Generalized morphea: plaques coaleasce affecting the entire trunk except nipple, can involves
the extremities, it is disabiling and causing difficulty in breathing. Distinguished from systemic
sclerosis by :
(a) Absence of Raynaud's phenomenon,
(b) Absence of internal organ involvement and
(c) Asymmetry of involvement
4. Linear morphea: different from plaque morphea by:
(a) Childhood onset,
(b) High ANA titer and
(c) Disabling especially when involve joint or cause atrophy of the whole limb
Variants of linear morphea:
En coup de sabre type (sword hit): linear morphea of head, can involve muscle, bone and rarely
brain causing seizures
Parry-Romberg syndrome: hemi facial atrophy including eyes and tongue (the most severe form
of linear morphea)
Diagnosis:
Hx and physical examination e.g. hardenening of skin lesion
Investigations e.g. autoantibodies: ANA and anti-ssDNA are commonly seen in linear and
generalized types
Biopsy: hyalinized and thick collagen bundles
Treatment:
Topical :
ineffective
Corticosteroid is
Vit D analogues e.g. calcipotriol may be of benefit
Systemic :
Glucocorticoids, methotrexate , PUVA (psoralen plus UVA)
Cutaneous manifestations of scleroderma:
1. Hardening of skin (hard to pinch)
2. Microstomia (hard to open mouth) with furrowing around mouth
3. Beaking of nose
4. Loss of facial expression
5. Telangiectasia of skin, lip and tongue
6. Ulcers and necrosis of finger tips
7. Calcinosis cutis (deposition of calcium in skin, subcutaneous tissue and muscle)
8. Nail fold telangiectasia
Dermatomyositis
Classification (1):
Polymyositis (muscle only)
Amyopathic dermatomyositis ( skin only)
Dermatomysitis (skin and muscle)
Classification (2):
Juveile type: not associated with malignancy but associated with more calcinosis than adult type
Adult type: associated with malignancy especially ovarian, lung and breast
Clinical features:
Cutaneous:
Heliotrop rash
: violaceous patch and edema around eyes
Gottron papules
: flat-topped violaceous papules on knuckles
Gottron sign
: violaceous discoloration of knuckles, elbows and knee
Photodistribution
of skin manifestations (shawl distribution)
Nail fold telengictasia
Calcinosis cutis
: deposition of calcium in skin, subcutis and muscle
Systemic(extracutaneous) :
Proximal myopathy (most important): inability to comb, to walk upstairs or to stand from sitting
position
Lung: interstitial lung disease, restrictive lung disease
Heart: conduction defects, arrhythmia
:
Diagnosis
History :. appearance or worsening of skin lesions with sun exposure
Physical examination: e.g. nail fold telengictasia, heliotrop rash, etc…
inability to walk upstairs, physical exam of muscle strength
Investigations :
Increased muscle enzymes in the serum ex. creatine phosphokinase (CPK) and adolase.
- Increased 24 - hour urinary creatine.
- Electromyography (EMG).
- Magnetic resonance imaging (MRI) or spectroscopy.
- Serum antibodies: autoantibodies such as ANA, anti-Jo1, anti-Mi2 antibodies
- Muscle biopsy.
- Searching for internal malignancy in adult dermatomyositis.
LE)
: the same as cutaneous LE (but less responsive to treatment than cutaneous
Treatment
Oral steroids.
- Cytotoxic drugs.
- Antimalarials.
- Intravenous immunoglobulin.
- Physical therapy.
