Dermatology Dr. Ahmed Abdulhussein Alhuchami
2019
Autoimmune Bullous Diseases
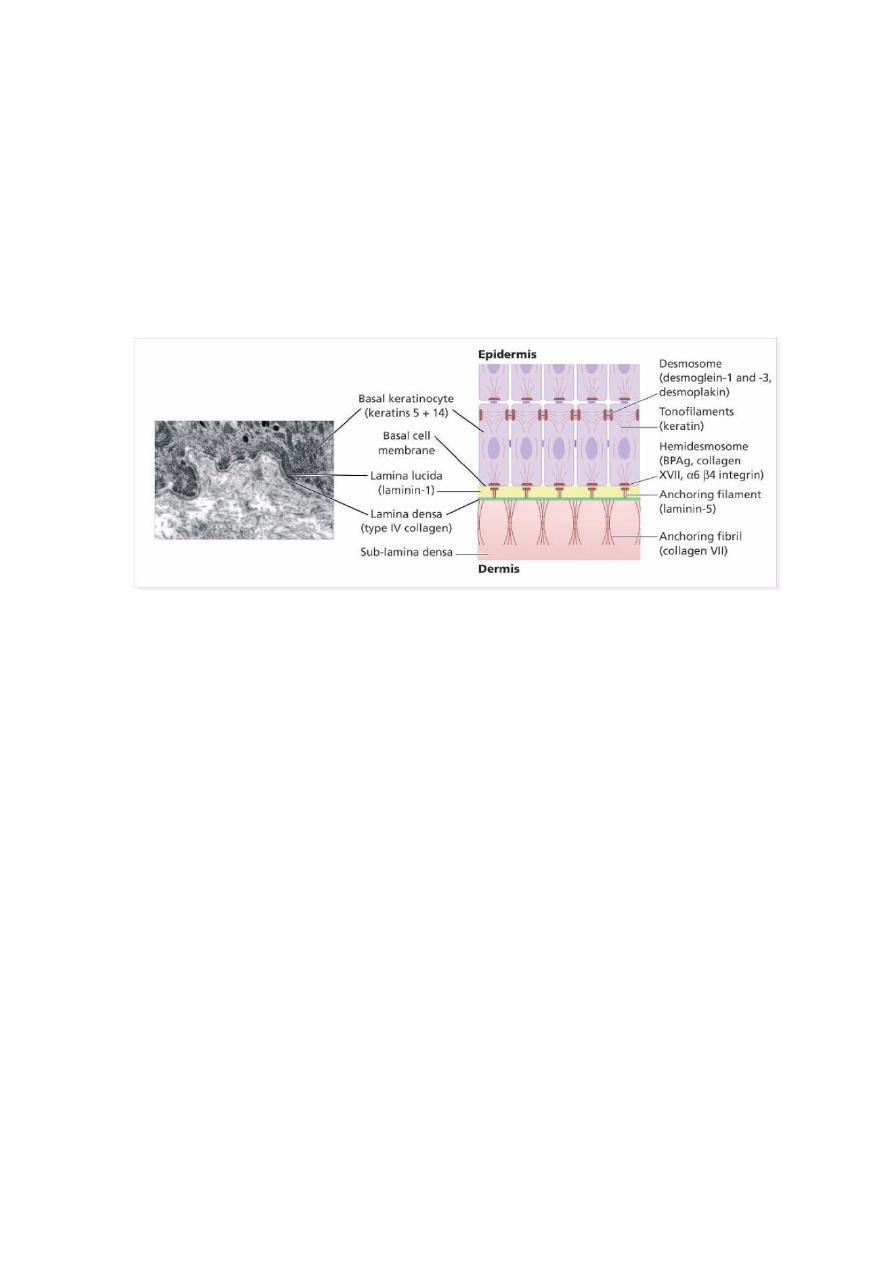
The dermo-epidermal junction
The basement membrane lies at the interface between the epidermis and dermis.
The plasma membrane of basal cells has hemidesmosomes (containing bullous pemphigoid
antigens) , While the attachment between
keratinocytes
cell is called desmosomes(
pemphigus
antigens).
Pemphigus Group
Group of disorders with loss of intraepidermal adhesion because of autoantibodies directed against
proteins of the desmosomal complex that hold keratinocytes together. Pemphigus can be divided into:
1. The deep form: pemphigus vulgaris, with its reactive state, pemphigus vegetans.
2. The superficial form: pemphigus foliaceus, with its lupus-like variant, pemphigus erythematosus
Pemphigus Vulgaris (PV)
Definition: Severe, potentially fatal disease with intraepidermal blister formation on skin and
mucosa caused by autoantibodies against desmogleins.
Epidemiology: not uncommon in our country affecting young adults with equal male:female ratio.
Pathogenesis:
Genetic predisposition: HLA associations exist.
Patients develop antibodies against desmoglein 3 (Dsg3) and later desmoglein 1 (Dsg1). The bound
antibodies activate proteases that damage the desmosome, leading to acantholysis.
Serum antibody titer usually correlates with disease activity.
Occasionally drugs cause pemphigus: penicillamine, captopril.
Clinical features: Sites of predilection include oral mucosa, scalp, face, mechanically stressed areas,
nail fold, intertriginous areas (can present as intertrigo). The blisters are not stable, as the epidermis
falls apart; therefore, erosions and crusts common.
Usually has three stages:

1-Oral involvement: In 70% of patients, PV starts in the mouth with painful erosions. Other mucosal
surfaces can also be involved.
2- Additional localized disease, often on scalp. (Always check the scalp in patients with unexplained
oral erosions.)
3-Generalized disease, flaccid blisters that rupture to painful, poorly healing crusted erosions and
ulcers; blisters hard to find. Pruritus is uncommon.
Diagnostic approach
: Clinical evaluation; check sites of predilection.
Nikolsky sign: Gentle rubbing allows one to separate upper layer of epidermis from lower, producing
blister or erosion. Fairly specific for pemphigus.
Histology: Can be helpful, but often just erosions or nonspecific changes. When a fresh lesion is
biopsied, acantholysis is seen (free-floating, rounded keratinocytes) with retention of basal layer
keratinocytes (tombstone effect) and mild dermal perivascular infiltrates.
Direct immunofluorescence: Perilesional skin shows deposition of IgG, C3. Antibodies surround the
individual keratinocytes.
Indirect immunofluorescence: 90% of sera show positive reaction; titer can be used to monitor
disease course.
ELISA: Can be used.
Treatment
: Because of the dangers of pemphigus vulgaris, and the difficulty in controlling it,
patients should be treated in a specialized unit.
A-supportive and Topical measures:
good nutrition, fluid replacement, daily bathing, potassium
permanganate compresses, local anesthetic gels in the mouth before meals, antiseptics and anticandidal
measures may also be useful
.
B-Specific therapy : Treatment needs regular follow-up and is usually prolonged. Includes the
following:-
1-Systemic corticosteroids are necessary for long periods of time. Resistant and severe cases need
very high doses of systemic steroids, such as prednisolone 80–320 mg/day, and the dose is dropped
only when new blisters stop appearing.
Patients should be screened for osteoporosis and latent tuberculosis before starting long-term
corticosteroid therapy.
The main cause of morbidity and mortality today in patients with pemphigus vulgaris is corticosteroid
side-effects. For this reason, corticosteroids are always combined with steroid-sparing agents.
Immunosuppressive mycophenylate mofetil, are often used as steroid-sparing agents.
2- New and promising approaches include plasmapheresis and intravenous immunoglobulin as used
in other autoimmune diseases.
3- other agents, such as azathioprine or cyclophosphamide,
4-High-dose intravenous immunoglobulin (HIVIg) ;(2 g/kg every 3–4 weeks) may help gain
quick control whilst waiting for other drugs to work.
5-Rituximab ( Anti-CD20 monoclonal antibody) has been reported to help multidrug resistance,
IV , once a week for 4 weeks.
In superficial types of pemphigus, smaller doses of above treatments are usually needed, and the use
of topical corticosteroids may help too.
C
C
o
o
m
m
p
p
l
l
i
i
c
c
a
a
t
t
i
i
o
o
n
n
s
s
o
o
f
f
P
P
.
.
v
v
u
u
l
l
g
g
a
a
r
r
i
i
s
s
1-Infections such as septicemia, chest infection… etc.
2-Fluid and electrolyte loss due to widespread denudation of the skin and mucous
membranes leading to what called
skin failure
that will result in end organ failure
(causing renal ,heart ,respiratory or /and liver failure).
3-Side effects of treatment with corticosteroids and other immunosuppressive agents.
These side effects are inevitable and now considered as the leading cause of
death in patients with P. vulgaris.
Pemphigoid Group
Bullous Pemphigoid
(BP)
Definition: hemidesmosomes in the basement membrane zone (BMZ).
Epidemiology: Favors elderly, with male:female ratio of 2:1.
Pathogenesis: Autoantibodies are directed against two hemidesmosomal proteins: called bollous
pemphigoid antigens (BPAGs )1and 2.
The binding of autoantibodies leads to complement activation, attraction of eosinophils, release of
proteases, and separation between the epidermis and dermis.
Less common causes include drugs (benzodiazepine, furosemide, penicillin, sulfasalazine), sunlight,
and ionizing radiation.
Clinical features:
Before blisters develop, pruritus, dermatitic, and urticarial lesions may be present. The blisters tend
to develop in these areas.
Blisters are tense and stable. They often have a fluid level and some are hemorragic. In contrast to
pemphigus, the Nikolsky sign is negative.
The course is chronic and benign. The lesions involve the trunk, extremities, and intertriginous areas,
with the oral mucosa involved in about one third of the cases.
Diagnostic approach: Laboratory: elevated ESR, eosinophilia, increased IgE.
Histology: subepidermal blister with cellular infiltrate containing many eosinophils and neutrophils.
Direct immunofluorescence: band of IgG and C3 along BMZ.
Indirect immunofluorescence: circulating antibodies are positive but not correlate with the disease
activity.
ELISA: identifies antibodies against both BPAGs.

Treatment of Bullous Pemphigoid (BP)
: in addition to general supportive measures the
specific therapy includes ;-
1-Mainstay is systemic corticosteroids: In the acute phase, prednisolone at a dosage of 40–60
mg/day is usually needed to control the eruption. The dosage is reduced as soon as possible, and
patients end up on a low maintenance regimen of systemic steroids, taken on alternate days until
treatment is stopped.
2-Immunosuppressive agents (azathioprine) may also be required as steroid-sparing agent.
Some patients do well on high-potency topical corticosteroids; worth a try with localized disease
or systemic problems (especially diabetes mellitus). Large open blisters and erosions may require
topical antiseptics
.
3
3
-
-
D
D
a
a
p
p
s
s
o
o
n
n
e
e
:
:
2 mg per kg per day may be useful in some cases.
Course of BP
is often self-limiting and treatment can often be stopped after one or
few years of treatment.
Remission of BP may be spontaneous or treatment-induced.
Complications
of BP are similar but milder and to lesser extent than those of PV
(less mortality rate).
" Best Regards "
