Reconstructive Surgery
(bone Graft)Principles of Reconstructive Surgery of Defects of the Jaws
Defects of the facial bones, especially the jaws, have a variety of causes, such as eradication of pathologic conditions, trauma, infections, and congenital deformities. The size of the defects that are commonly reconstructed in the oral and maxillofacial region varies considerably from small alveolar clefts to mandibulectomy defects.In an “ideal reconstruction” the missing tissue is replaced with identical substitute. This ideal is difficult, and usually impossible, to achieve Without being able to perform an "ideal reconstruction in every case, the surgeon is left with options along the reconstructive ladder .This graduated range of reconstructive choices includes healing by secondary intention, primary closure, delayed closure, split thickness skin graft full thickness skin graft, tissue expansion, random pattern flap, pedicle flap and free tissue transfer. depend significantly on surgeon preference and expertise.
Goals of Reconstruction:
• Restoration of function• Restoration of cervico-facial symmetry and form
• Creation of barriers between cavities and spaces in the head and neck that should not communicate.
• Facial reanimation
• Dental rehabilitation
• Return of sensation
Biologic Basis of Bone Reconstruction
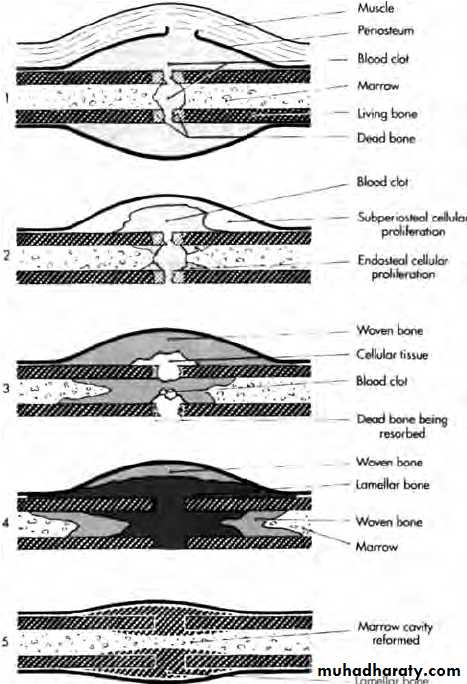
A tissue that is transplanted and expected to become a part of the host to which it is transplanted is known as a graft.The healing of bone and bone grafts is unique among connective tissues because new bone formation arises from tissue regeneration rather than from simple tissue repair, with scar formation.
This healing therefore requires the element of cellular proliferation (osteoblasts) and the element of collagen synthesis.
Two-Phase Theory of Osteogenesis:
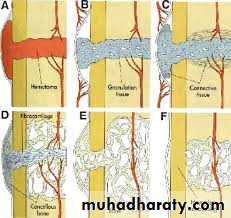
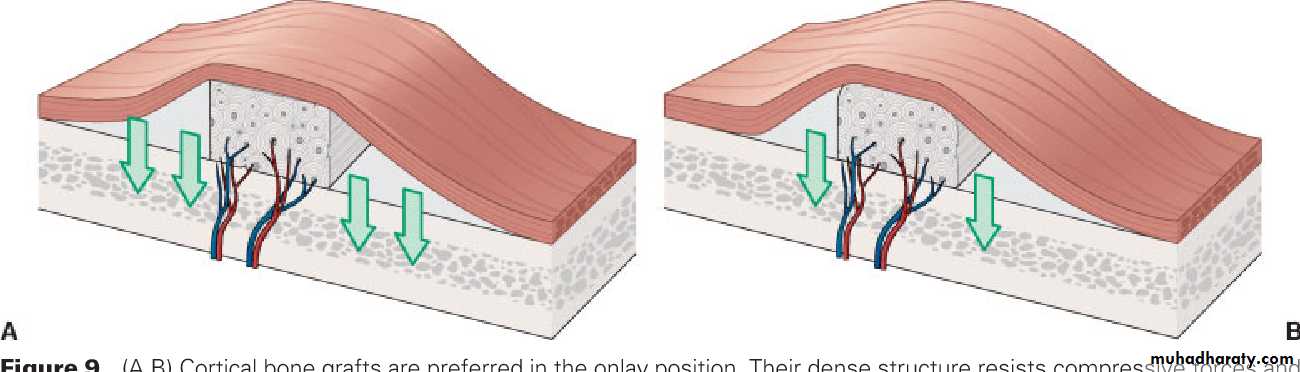
Two basic processes occur on transplanting bone from one area to another area in the same individual first process that leads to bone regeneration arises initially from transplanted cells in the graft that proliferate and form new osteoid. The amount of bone regeneration during this phase depends on the number of transplanted bone cells that survive during the grafting procedure. Obviously, when the graft is first removed from the body, the blood supply has been severed. Thus the cell in the bone graft depend on diffusion of nutrients from the surrounding graft bed (i.e., the area where the graft is placed) for survival.A considerable amount of cell death occurs during the grafting procedure, and this first phase of bone regeneration may not lead to an impressive amount of bone regeneration when considered alone. Still, this phase is responsible for the formation of most of the new bone. The more viable cells that can be successfully transplanted with the graft, the more bone that will form.
The graft bed also undergoes changes that lead to a second phase of bone regeneration beginning in the second week. Intense angiogenesis and fibroblastic proliferation from the graft bed begin after grafting, and osteogenesis from host connective tissues so begins. Fibroblasts and other mesenchymal cells differentiate into osteoblasts and begin to lay down new bone. Evidence shows that a protein (or proteins) found in the bone induce these reactions in the surrounding soft tissues of the graft bed. This second phase is also responsible for the orderly incorporation of the graft into the host bed with continued resorption, replacement, and remodeling.
Immune Response
When a tissue is transplanted from one site to another area in the same individual. immunologic complications usually do not occur. The immune system is not triggered because the tissue is recognized as ‘‘self’’ However when a tissue is transplanted from one individual to another or from one species to another, the immune system may present an obstacle to the success of the grafting procedure.If the graft is recognized as a foreign substance by the host, it will mount an intense response in an attempt to destroy the graft. The type of response of the immune system mounts against foreign" grafts is primarily a cell-mediated response by T lymphocytes. The response may not occur immediately, however, and in the early period the incorporation of a bone graft into the host may appear to be progressing normally. The length of this latent period depends on the similarity between the host and the recipient. The more similar they are (antigenically) the longer an immunologic reaction may take to appear.
This type of immunologic reaction is the most common reason for rejection of hearts, kidneys, and other organs transplanted to another individual. Tissue typing procedures, in which a donor and recipient are e genetically compared for similarities before transplantation, are currently common place for organ transplantation but never for bone grafts.
Because of the immunologic rejection of transplants between individuals or between species, methods have been devised to improve the success of grafting procedures in these instances.
Two basic approaches are used clinically: The first is the suppression of the host individual's immune response. Immunosuppression with various medications is most commonly used in organ transplant patients. This approach is not used routinely in oral and maxillofacial surgical bone grafting procedures because of the potential complications from immunosuppression.
Another approach that has been used extensively in oral and maxillofacial surgical procedures is the alteration of the antigenicity of the graft so that the host's immune response will stimulated. Several methods of treating grafts have been used, including boiling, deproteinization, use of thimerosal (Merthiolate), freezing, freeze-drying, irradiation, and dry heating. All of these methods, potentially helpful for use in bone grafts, are obviously not helpful in organ transplants.
Types of Grafts
Autogenous Grafts:Also known as auto grafts or self-grafts, autogenous grafts are composed of tissues from the same individual. Fresh autogenous bone is the most ideal bone graft material. The autogenous graft is unique among bone grafts in that it is the only type of bone graft to supply living, immunocompatible bone cells essential to phase I osteogenesis. The larger number of living cells that are transplanted, the more osseous tissue that will be produced.
Autogenous bone graft can be taken from these area:
• Iliac crest.• Rib.
• Tibia.
• Symphysis.
• Retromolar area.
•
The advantages of autogenous bone are that it provides osteogenic cells for phase I bone formation, and no immunologic response occurs.
A disadvantage is that this procedure necessitates another site of operation for taking the graft.
Allogeneic Grafts:
Also known as allografts or homograft's, allogeneic grafts are grafts taken from another individual of the same species.Because the individuals are usually genetically dissimilar, treating the graft to reduce the antigenicity is routinely accomplished. Today, the most commonly used allogeneic bone is freeze-dried. All of these treatments destroy any remaining osteogenic cells in the graft, and therefore allogeneic bone grafts cannot participate in phase I osteogenesis. The assistance of these grafts to osteogenesis is purely passive, they offer a hard tissue matrix for phase II induction.
Advantages are that allogeneic grafts do not require another site of operation in the host and that a similar bone or a bone of similar shape to that being replaced can be obtained (e.g , an allogeneic mandible can be used for reconstruction of a mandibulectomy defect)
The disadvantage is that an allogeneic graft does not provide viable cells for phase I
osteogenesis
Xenogeneic Grafts
Also known as xenografts or heterografts, xenogeneic grafts are taken from one species and grafted to another. The antigenic dissimilarity of these grafts is greater than with allogeneic bone. The organic matrix of xenogeneic bone is antigenically dissimilar to that of human bone, and therefore the graft must be treated more vigorously to prevent rapid rejection of the graft.Bone grafts of this variety are rarely used in major oral and maxillofacial surgical procedures.
Advantages are that xenografts do not require another site of operation in the host, and a large quantity of bone can be obtained.
Disadvantages are that xenografts do not provide viable cells for phase I Osteogenesis and must be vigorously treated to reduce antigenicity.
Osteoinduction, Osteoconduction and Osteogenesis
Osteoinduction: refers to new bone formation from the differentiation of osteo-progenitor cells, derived from primitive mesenchymal cells, into secretory osteoblasts This differentiation is under the influence of bone inductive proteins or bone morphogenic proteins BMP (agents from bone matrix).Osteoconduction: is the formation Of new bone from host-derived or transplanted osteo-progenitor cells along a biologic or alloplastic framework, such as along the fibrin clot in tooth extraction or along a hydroxyapatite block. Osteoconductive grafts provide only a passive framework or scaffolding. These grafts are biochemically inert in their effect upon the host. The grafted material therefore does not have the ability to actually produce bone. This type of graft simply conducts bone-forming cells from the host bed into and around the scaffolding.
Osteogenesis: is the formation of bone from osteo-progenitor cells. Spontaneous osteogenesis is the formation of new bone from osteo-progenitor cells in the wound. Transplanted osteogenesis is the formation of new bone from osteo-progenitor cells placed into the wound from a distant site.
Assessment of Patient in Need for Reconstruction
Hard tissue defect• Adequate radiographs are necessary to evaluate the full extent of the osseous defect. The site of the defect may be just as important as the size of the defect when dealing with mandibular Osseous problems. For example, if the mandibular condyle is missing treatment is relatively more difficult. A residual portion of the ramus with the condyle still attached makes osseous reconstruction easier because the temporomandibular articulation is difficult to restore.
Soft tissue defect:
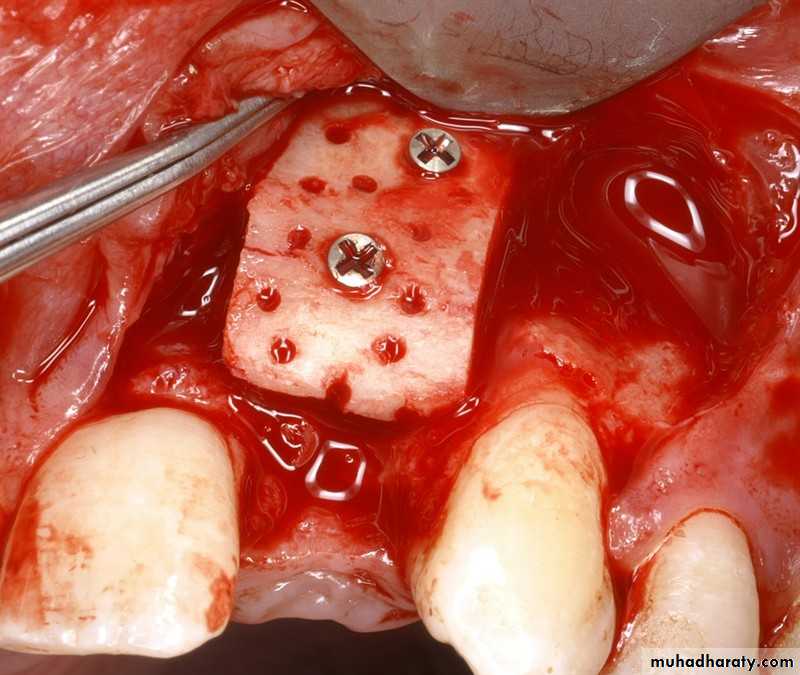
Proper preparation of the soft tissue bed that is to receive the bone graft is just as important to the success of bone grafting as the bone graft material itself. The transplanted bone cells must survive initially by diffusion of nutrients from the surrounding soft tissues. Revascularization of the bone graft through the development of new blood vessels from the soft issue bed must then occur.
Goals of Mandibular Reconstruction1. Restoration of continuity
2. Restoration of alveolar bone height3. Restoration of osseous bulk
Diagnostics
Radiographic imaging :CT scan
Digital volume tomography (DVT) (also known as CBCT)
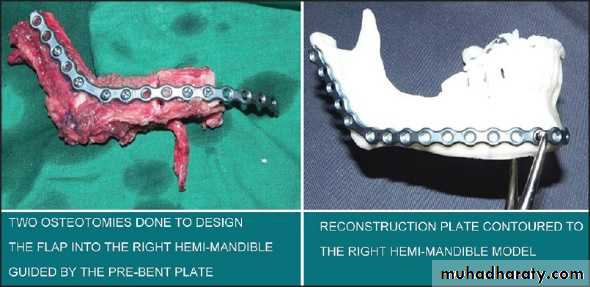
Mandibular Reconstruction
Autologous non vascularized bone.Iliac crest
Rib
Tibia
Local pediculated osseomyocutaneous flaps.
major pectoralis muscle flap 1n combination with a rib,
sternocleidomastoid flap with part of the clavicle,
trapezius muscle flap with a portion of the scapula has been introduced for mandibular reconstruction. Despite the better prognosis of the transferred bone,
these techniques were limited to only a few indications due to their high donor site morbidity and the poor outcome in terms of function and esthetics
vascularized free bone grafts
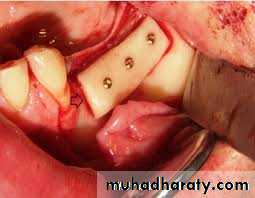
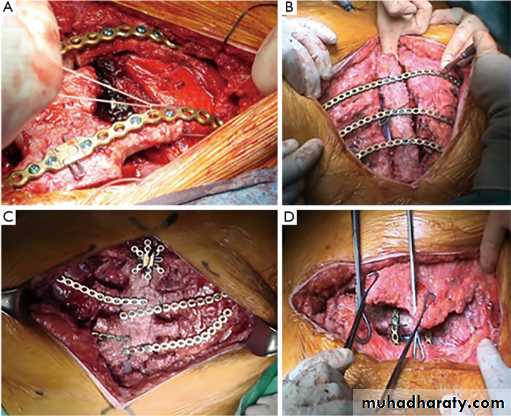
Iliac crest, scapula, fibula, and other bones emerged as the most common and promising donor sites. Today, they are the gold standard for mandibular reconstruction. The reconstruction with vascularized osseous free flaps has become a safe and consistent procedure with a success rate of more than 90%.Surgical Principles of Maxillofacial Bone Grafting Procedures:Several important principles should be followed during any grafting procedure. They must be strictly adhered to if a successful outcome is desired. The following are a few that pertain to reconstructing mandibular defects:
1- Control of residual mandibular segments:
2- A good soft tissue bed for the bone graft:3- Immobilization of the graft:
4- Aseptic environment:
5- Systemic antibiosis:
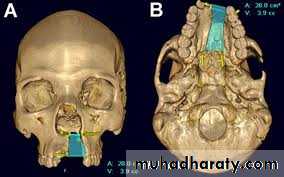
Maxillary Reconstruction
Maxillary and midface reconstruction is more challenging than most oro-mandibular defects for several reasons:
• Complex geometry
• Distance of target vessels for revascularization
• Impaired access and visibility without trans-facial incisions
• Exposure to the sinus, nasal, and oral cavities
Defect Classification
Two classifications have been selected because of their simplicity and their comprehensive applicability Both systems describe the vertical and horizontal components of the defects to provide a three-dimensional description of the defect.Okay classification of Maxillary Defects
• Defect Class• Criteria
• la
• Limited defect in the central portion of the palate that does not involve the alveolus
• Ib
• Defect in the palate that involves the alveolus but is located posterior to the canine or is limited to the premaxilla with preservation of the canine teeth bilaterally
• II
• Hemi-palatal defect that does not cross the midline in a conventional longitudinal resection and does not extend posterior to the midpoint of the palate for a defect that is created in the horizontal orientation, thus preserving at least half of the palatal surface
• III
• A subtotal or total palatectomy that involves morethan one half of the palatal surface
• F
• Indicates a defect in the floor of the orbit
• Z
• Indicates a defect in the body of the zygoma
Brown classification
This classification system was introduced by Brown and Shaw in 2010.Their system subdivides the vertical, described numerically, and horizontal components, described alphabetically, of maxillectomy defects.
Defects are graded vertically from I to IV based on their extension from the maxillary alveolus toward the cranial base. Class I defects are limited to alveolus and palatal bone only. By definition, these defects do not involve the maxillary antrum. Also known as low maxillectomies, class II defects include alveolus and antral walls, but do not involve the orbital floor.
Class I
Class IIClass III defects, or high maxillectomies, extend further superiorly to include the orbital floor; however, by definition the globe is not involved in the resection. Also known as radical maxillectomies.
Class IV defects are essentially the same as class III defects in terms of bony involvement, but orbital exenteration is included in the resection.
Class V and VI were later added in the modified system to address isolated orbito-maxillary and naso-maxillary defects respectively. Unlike the traditional class I to IV defects, these special categories do not involve the lower maxilla and alveolus.
Class III
Class IVWithin the modified Brown classification, horizontal extent is graded separately as either a, b, c, or d. Isolated defects of the palate not including the alveolus are termed a. Defects involving 50% or less of the transverse width of the maxilla are termed b. Horizontal anterior defects of the maxilla are termed c. Large horizontal defects involving greater than 50% of the transverse width are termed d.
Maxillary defect reconstruction
Brown class 1 defects can be treated with local flaps, or with an obturator if there is an oro-antral or oro-nasal communication. Similarly, class II a defects can be obturated or reconstructed with local and pedicle flaps, or a combination of both. As the horizontal extent increases, such as in classes II b and II c, prosthetic rehabilitation with an obturator becomes more difficult and implant support may become necessary to improve stability. Consequently, a composite flap may be used to assist with soft tissue closure and provide bone for implant placement.Class III defects, involving midline and cross-midline structures, are usually not treated with obturators, because the weight and size of a device presents challenges in achieving a functional and stable prosthesis. For Classes 3b and 3c defects, a composite vascularized flap capable of addressing both maxillary and orbital defects is the recommended treatment. Class 4 defects are almost never amenable to obturator rehabilitation without free flap reconstruction, as they involve the entire orbit and sometimes the cranial base. A composite free tissue transfer that provides not only bone, but also a generous amount of soft tissue for closure of fistulas, obturation of the orbit, and sealing of cranial communications is needed.
Pediatric patients
Wherever possible, pediatric patients should be obturated while they are growing. If a bone flap is placed, there is a risk that the flap will not grow. Lack of growth of the flap will then have a reciprocal effect on the remaining maxilla and result in a secondary ,deformity that can be prevented with a temporary prosthetic option. Second, if the flap is not restored with teeth, there will be no antagonist for the opposing teeth. These will then super-erupt, leading to a secondary deformity in the opposite jaw that can only be corrected with an osteotomy.A prosthetic solution allows a child to have a functional reconstruction that provides a dentition to prevent a deformity in the opposite jaw and permits normal growth and development in the remaining maxilla. It is also the most efficient process to allow a child to resume their normal academic. athletic, and social activities that are so important in the younger years of life. Most children adapt very quickly to a prosthetic option.
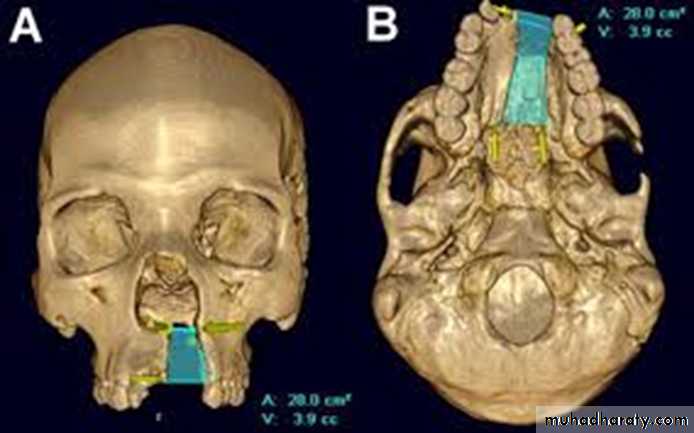
COMPUTER-ASSISTED SURGICAIL PLANNING
If a bony reconstruction of the maxilla is to be accomplished, it should be correct in both position and form. The complex three-dimensional nature of the maxilla and associated parts makes virtual planning particularly valuable. Virtual planning may take many forms in maxillary reconstruction according to the needs and preferences of the surgeon. At a minimum, it can help ensure appropriate positioning of the bone flap over the opposite arch with adequate inter-arch space for a dental rehabilitation.
T
H
A
N
K
S