THE LIVERbyDr. Zahraa MarwanCollege of Medicine
• liver weighs 1500g, functions as station between splanchnic and systemic circulations to maintain body’s metabolic homeostasis through:
• -Processing dietary carbohydrates, amino acids, lipids, and vitamins
• -Removal of microbes and toxins in splanchnic to systemic circulation
• -Synthesis of plasma proteins
• - Detoxification and excretion into bile of endogenous waste products.
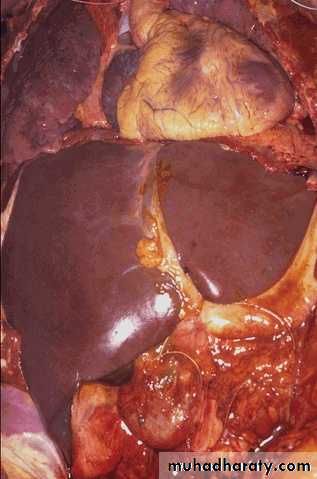
Macroarchitecture -By distribution of right and left portal circulation, liver is divided into right and left lobes -functionally liver is organizied into 8 segments numbered I to VIII, -liver receives 25% of total cardiac output -portal vein, hepatic artery and bile ducts branch in parallel within the liver in portal tracts
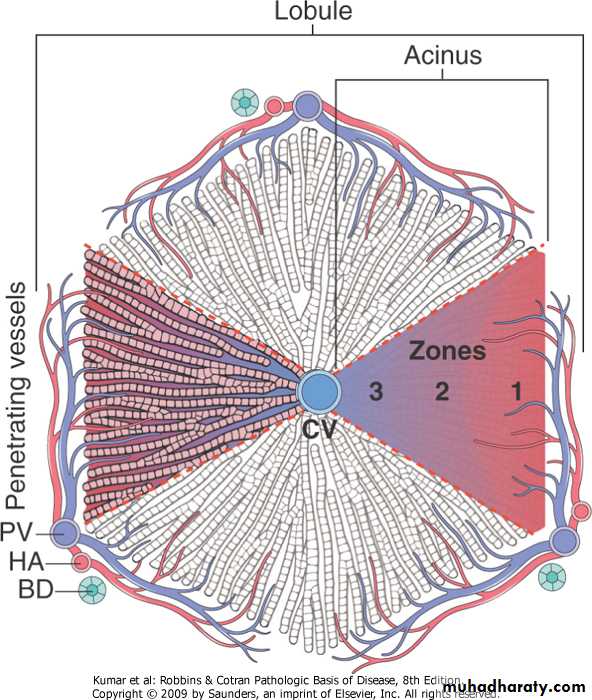
Liver, microarchitecture
Liver is divided histologically into lobules. The center of the lobule is the central vein. At the periphery of the lobule are portal triads. Functionally, the liver can be divided into three zones, based upon oxygen supply. Zone 1 encircles the portal tracts where the oxygenated blood from hepatic arteries enters. Zone 3 is located around central veins, where oxygenation is poor. Zone 2 is located in between.
Patterns Of Hepatic Injury:
• .Degeneration and intracellular accumulation• .Cell death
• .Inflammation
• .Regeneration
• .Fibrosis
Chronic Liver Failure and Cirrhosis
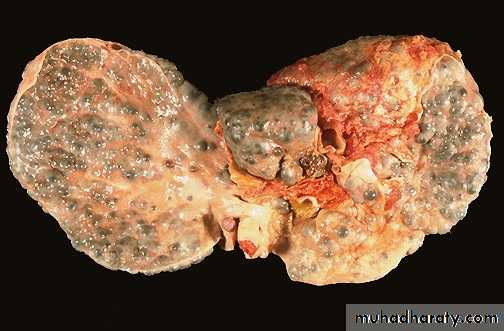
Cirrhosis is the morphologic change most often associated with chronic liver disease; it defined by 3 characteristics:-bridging fibrous septae
-parenchymal nodules
-diffuse disruption of liver architecture
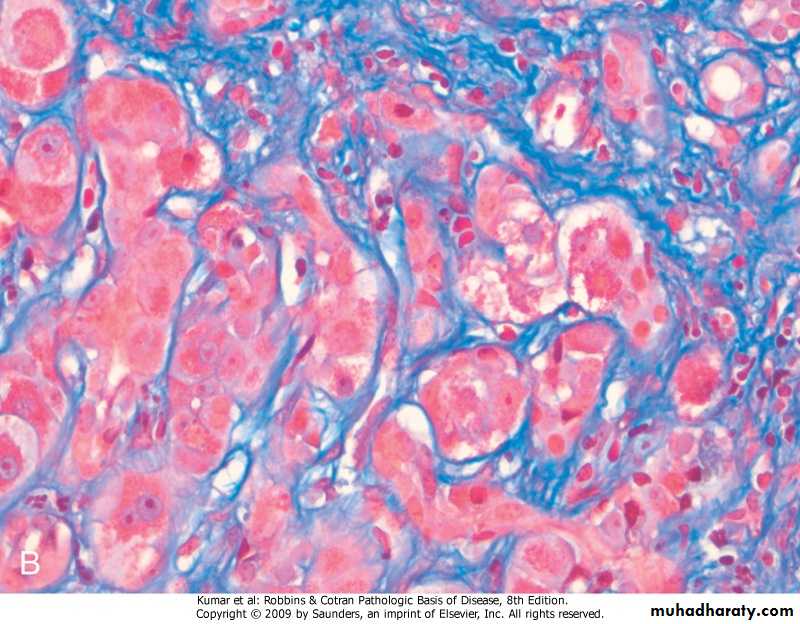
A. Normal liver. B. Cirrhosis resulting from chronic viral hepatitis. Note the broad scars separating bulging regenerative nodules over the liver surface.
A
B
Classification of cirrhosis: -the best is based on presumed etiology .excessive alcoholic consumption .viral hepatitis .biliary diseases .primary hemochromatosis .Wilson disease .α-1 antitrypsin deficiency .cryptogenic
.Clinical features of cirrhosis:
-asymptomatic (in 40% of cases)-non-specific (anorexia, weight loss, weakness)
-hepatic failure
-ultimate cause of death:
.progressive liver failure
.portal hypertension
.hepatocellular carcinoma
Pathogenesis of cirrhosis:
-progressive fibrosis and nodular regeneration of hepatocytes -reorganization of vascular micro- circulation>hypoxia>reduced secretion of substances into plasmaMorphology of cirrhosis:
Grossly:- Micronodular cirrhosis. The regenerative nodules are quite small, averaging less than 3 mm in size.
- The most common cause for this is chronic alcoholism. The process of cirrhosis develops over many years.
- Macronodular cirrhosis. Viral hepatitis (B or C) is the most common cause for macronodular cirrhosis. Wilson's disease and alpha-1-antitrypsin deficiency also can produce a macronodular cirrhosis.
Micronodular cirrhosis.
Macronodular cirrhosis.
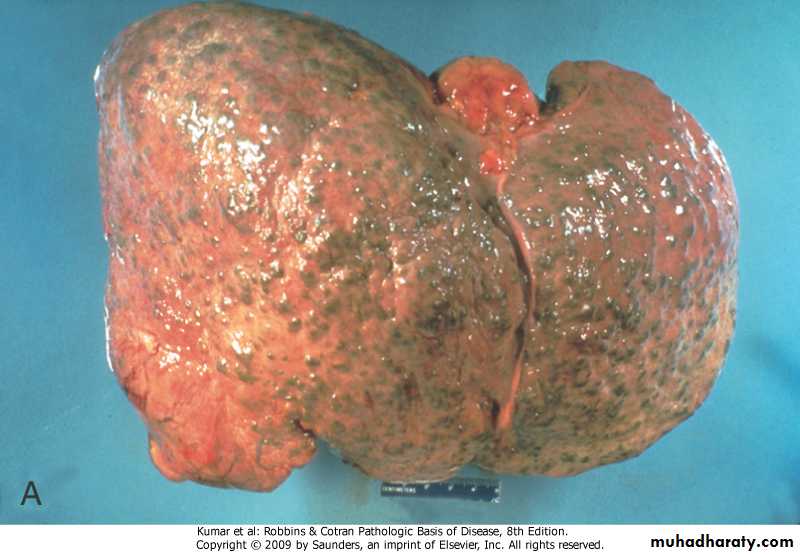
Microscopically:
- Cirrhosis is marked by the diffuse transformation of the entire liver tissue into regenerative parenchymal nodules surrounded by fibrous bands.Microscopically with cirrhosis, the regenerative nodules of hepatocytes are surrounded by fibrous connective tissue that bridges between portal tracts. Within this collagenous tissue are scattered lymphocytes as well as a proliferation of bile ducts.
Alcoholic cirrhosis in an active drinker (A) and following long-term abstinence (B). A, Thick bands of collagen separate rounded cirrhotic nodules. B, After 1 year of abstinence, most scars are gone (Masson trichrome stain).
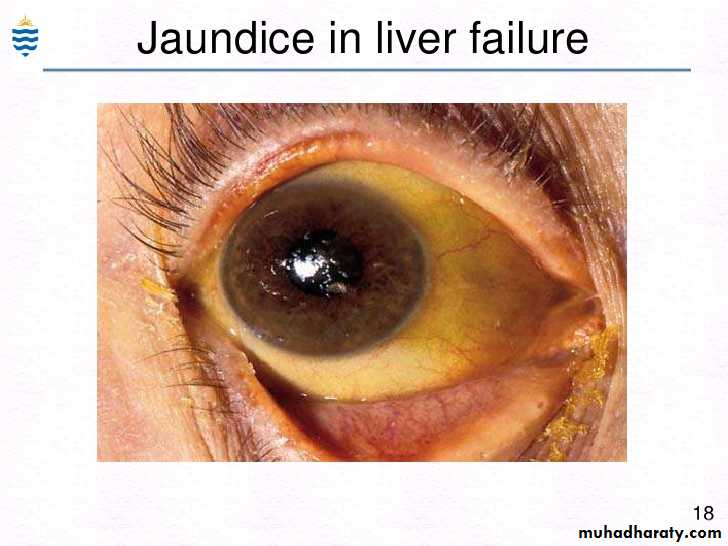
JAUNDICE:.Disequilibrium between bilirubin production and clearance due to one or more of the followings: -excessive production of bilirubin -reduced hepatocytes uptake -impaired conjugation -decreased hepatocellular excretion -impaired bile flow
CHOLESTASIS:.Presents clinically as jaundice and pruritus.results from -hepatocellular dysfunction -intrahepatic biliary obstruction -extrahepatic biliary obstruction.laboratory change is elevated serum alkaline phosphatase
Intracellular cholestasis
Cholestasis, showing the characteristic accumulation of bile pigments in the cytoplasm
VIRAL HEPATITIS.clinical syndromes: -acute self-limited hepatitis -acute fulminant hepatitis -chronic hepatitis -carrier state -cirrhosis -hepatocellular carcinoma.diagnosis -serological tests -liver biopsy
Hepatitis A Virus:
• HAV is a single stranded RNA picornavirus usually causing benign self-limited infection with an incubation period of 3-6 weeks.• It does not cause chronic hepatitis
• Rarely (in about 0.1% of cases) produces fulminant hepatitis.
• It is typically cleared by the host immune response, so it does not establish a carrier state.
• It occurs worldwide and is endemic in places with poor hygiene and sanitation.
• Spreads by contaminated water and food
• HAV viremia is transient (blood-born transmission occurs only very rarely, donated blood is not tested for virus)- Specific anti-HAV IgM antibodies at onset of symptoms (diagnostic marker in acute infection), titer declines in months- IgG persists for years, providing protective immunity against re-infection by all strains of HAV
Hepatitis B Virus:
.DNA virus with incubation period of 2-26 weeks, it can withstand extremes of temperatures and humidity- The outcome of HBV infection varies widely, from:
• (1) acute hepatitis with recovery and clearance of the virus
• (2) nonprogressive chronic hepatitis
• (3) progressive chronic disease ending in cirrhosis
• (4) fulminant hepatitis with massive liver necrosis
• (5) an asymptomatic
• (6)enhances hepatitis D infection
• (7) hepatcoellular carcinoma
- IgM anti-HBc becomes detectable in serum shortly before the onset of symptoms, (diagnostic marker in acute infection). Over a period of months, the IgM anti-HBc antibody is replaced by IgG anti-HBc.- Carrier state is defined by presence of HBsAg in serum for 6 months or longer.modes of transmission -blood and its products -body fluids -vertical transmission from mother to neonate during birth -in 1/3 of cases mode is unknown
Hepatitis C Virus:
. HCV is a major cause of liver disease, It is single stranded RNA with incubation period of 4-26 weeks..Routes of transmission:
-inoculations
-blood transfusions
-sexual intercourse
-perinatal
• The most common risk factors for HCV infection are as follows:
Intravenous drug abuseMultiple sex partners
Having had surgery within the last 6 months
Needle stick injury
Multiple contacts with an HCV-infected individual
Employment in the medical or dental field
The outcome of HCV:
• Acute hepatitis• Chronic hepatitis
• Cirrhosis
-Persistent infection and chronic hepatitis are the hall- marks of HCV infection, despite the generally asymptomatic nature of the acute illness.
Hepatitis D Virus:.RNA virus with defective replication, causing infection when encapsulated by HBsAg .delta hepatitis arises in 2 settings: 1- Acute coinfection after exposure to serum containing both HDV and HBV . severe acute hepatitis and fulminant liver failure, and higher rates of progression to chronic infection. 2- super-infection of a chronic carrier of HBV .mild to severe hepatitis>fulminant chronic hepatitis>cirrhosis
Hepatitis E Virus:
.single stranded RNA with incubation period of 6 weeks.water-born infection affecting young to middle-aged adults
.in most cases the disease is self-limiting but has a high mortality rate among pregnant women (20%)
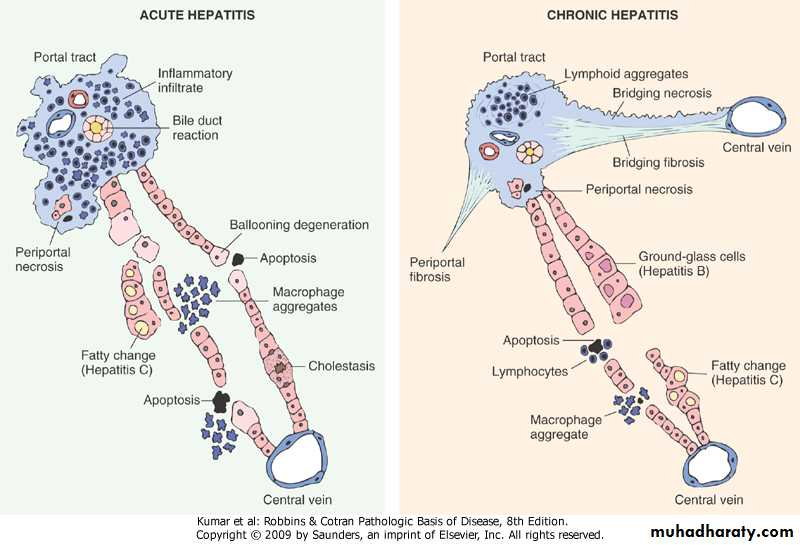
The Morphgology in viral hepatitis:
The morphological changes in acute and chronic viral hepatitis are shared among the hepatotropic viruses and can be mimicked by drug reactions or autoimmune hepatitis.Acute viral hepatitis.
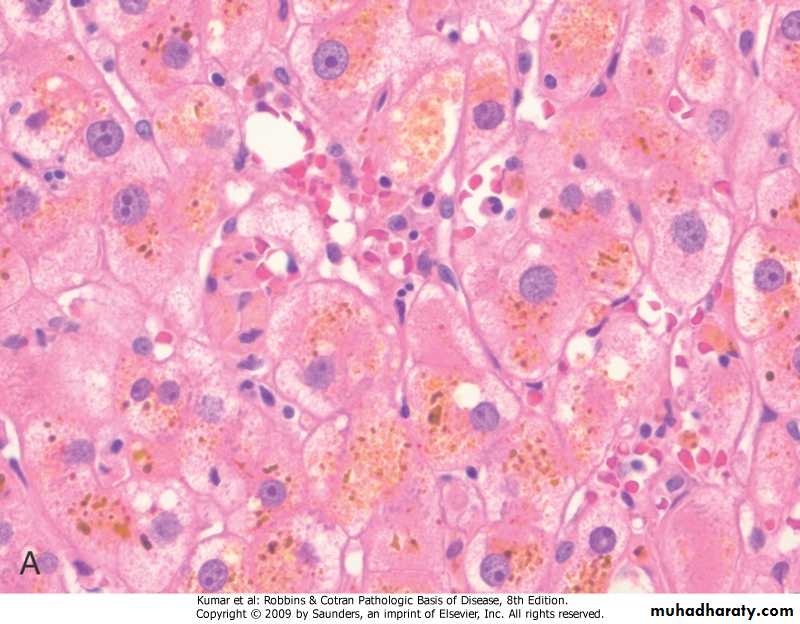
Grossly, livers involved by mild acute hepatitis appear normal or slightly mottled. Rarely, massive hepatic necrosis may produce a greatly shrunken liver.Microscopically, as is typical of many viral infections, mononuclear cells predominate in all phases of viral hepatitis. Most parenchymal injury is scattered throughout the hepatic lobule as “spotty necrosis” or lobular hepatitis.
Portal inflammation in acute hepatitis is minimal or absent.
Chronic viral hepatitis.
The defining histologic feature of chronic viral hepatitis is mononuclear portal infiltration..The hallmark of progressive chronic liver damage is scarring.
At first, only portal tracts exhibit fibrosis, but in some patients, with time, fibrous septa-bands of dense scar will extend between portal tracts.
In the most severe cases, continued scarring and nodule formation leads to the development of cirrhosis.
Certain histologic features point to specific viral etiologies in chronic hepatitis. In chronic hepatitis B,“ground-glass” hepatocytes (cells with endoplasmic reticulum swollen by HBsAg) are a diagnostic hallmark.
Liver biopsies involved by chronic hepatitis C commonly show large lymphoid aggregates. Often, hepatitis C, is associated with fatty change in scattered hepatocytes.
A diagram illustrating the difference between acute & chronic viral hepatitis
Autoimmune Hepatitis:
.chronic hepatitis with histology similar to those of chronic viral hepatitis.may run an indolent or severe course.
-Characteristics features include:
• female predominance
• absence of viral serologic markers
• high serum IgG level
• high serum titers of auto-antibodies
• absence of mitochondrial antibodies
• response to immunosuppression
DRUG And TOXIN-INDUCED LIVER DISEASE:
Mechanisms:-direct toxicity
-conversion of xenobiotic to active toxin
-through immune mechanisms
Types of morphologic injury: -hepatocyte necrosis -cholestasis -chronic hepatitis -micro and macrovesicular steatosis
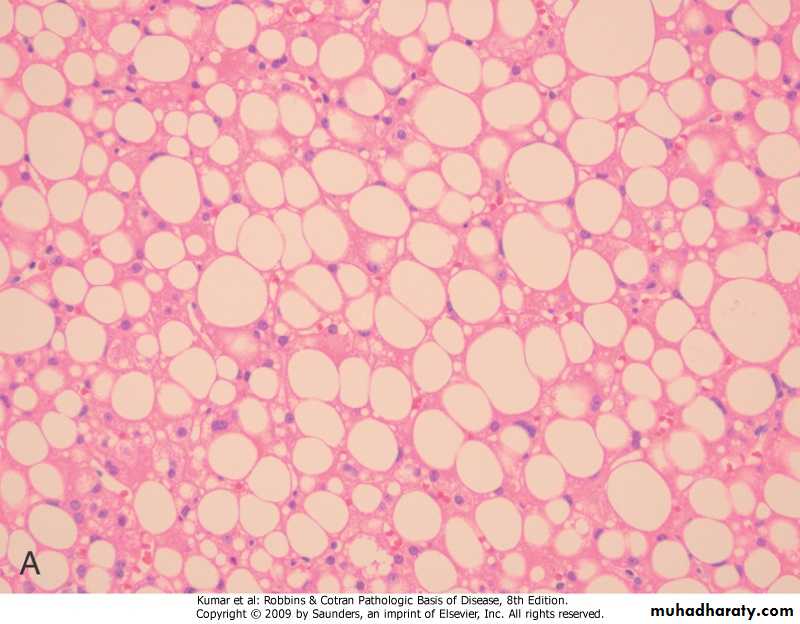
ALCOHOLIC LIVER DISEASE.pathogenesis -short-term ingestions of up to 80 mg of alcohol over one to several days cause mild reversible fatty change -daily intakes of 80 mg or more produce severe hepatic injury .only 15% develop cirrhosis -women are more prone to injury than men (? genetic susceptibility)
.clinical features:
• Steatosis.asymptomatic
.hepatomegaly and mild elevation of
serum bilirubin and alkaline phosphatase
• Acute hepatitis, (minimal to fulminant)
• Cirrhosis
Liver, steatosis
Steatosis (Fatty change)
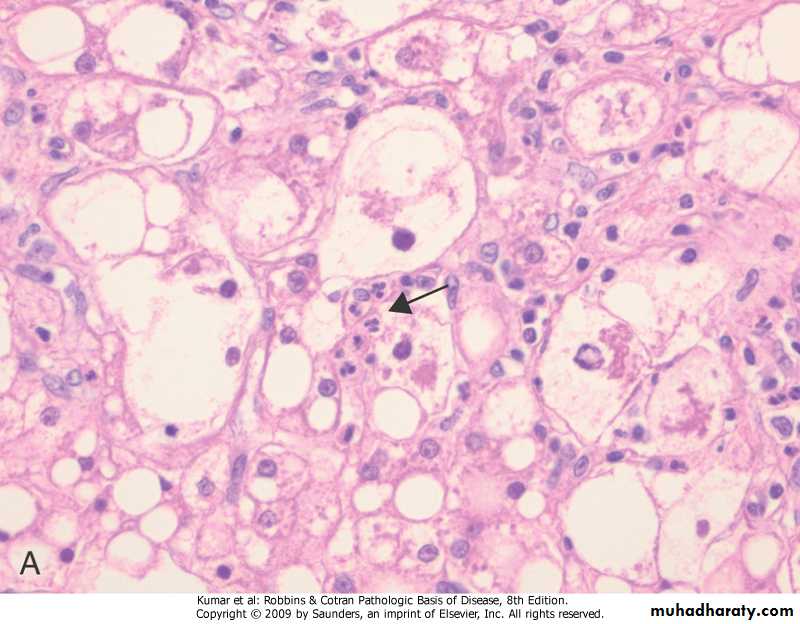
Alcoholic hepatitisAlcoholic hepatitis
Alcoholic hepatitis, Mallory bodies, Masson stainAlcoholic hepatitis: Mallory bodies are visible as eosinophilic cytoplasmic inclusions in degenerating hepatocytes
Alcoholic cirrhosis
Alcoholic Cirrhosis
TUMORS AND TUMOR-LIKE LESIONS.hepatic masses may present as
-epigastric fullness and discomfort
-detected incidentally by
.routine physical examination
.radiographic studies
Benign Neoplasms: 1- Cavernous Hemangiomas 2- Liver Cell Adenomas
Malignant Neoplasms:1- Hepatocellular Carcinoma
2- Cholangiocarcinoma
3- Hepatoblastoma
4- Angiosarcoma
Metastatic Tumors .far more common than primary ones .the most common primaries -breast -lung -colon.typically, multiple nodules are produced