Histoplasmosis
Histoplasmosis is a pulmonary and hematogenous disease caused by Histoplasma
capsulatum; it is often chronic and usually follows an asymptomatic primary
infection. Symptoms are those of pneumonia or of nonspecific chronic illness.
Diagnosis is by identification of the organism in sputum or tissue or use of specific
serum and urine antigen. Treatment, when necessary, is with amphotericin B or an
azole.
(See also the Infectious Diseases Society of America’s
Management of Patients with Histoplasmosis
Histoplasmosis occurs worldwide.
In the US, the endemic area for histoplasmosis includes
The Ohio–Mississippi River valleys extending into parts of northern
Maryland, southern Pennsylvania, central New York, and Texas
Microfoci have been noted in other states, such as Florida, and along the St. Lawrence
and Rio Grande rivers.
H. capsulatum grows as a mold in nature or in culture at room temperature but
converts to a small (1 to 5 μm in diameter) yeast cell at 37° C and during invasion of
host cells. Infection follows inhalation of conidia (spores produced by the mycelial
form of the fungus) in soil or dust contaminated with bird or bat droppings. Severe
disease is more common after heavy, prolonged exposure and in men, infants, or
people with compromised T-cell–mediated immunity.
Initial infection occurs in the lungs and usually remains there but may spread
hematogenously to other organs if it is not controlled by normal cell-mediated host
defenses. Progressive disseminated histoplasmosis is one of the defining opportunistic
infections for AIDS.
Symptoms and Signs
Most histoplasmosis infections are asymptomatic or so mild that patients do not seek
medical attention. The disease has 3 main forms.
Acute primary histoplasmosis is a syndrome with fever, cough, myalgias, chest
pain, and malaise of varying severity. Acute pneumonia (evident on physical
examination and chest x-ray) sometimes develops.
Chronic cavitary histoplasmosis is characterized by pulmonary lesions that are often
apical and resemble cavitary TB. Manifestations are worsening cough and dyspnea,
progressing eventually to disabling respiratory dysfunction. Dissemination does not
occur.
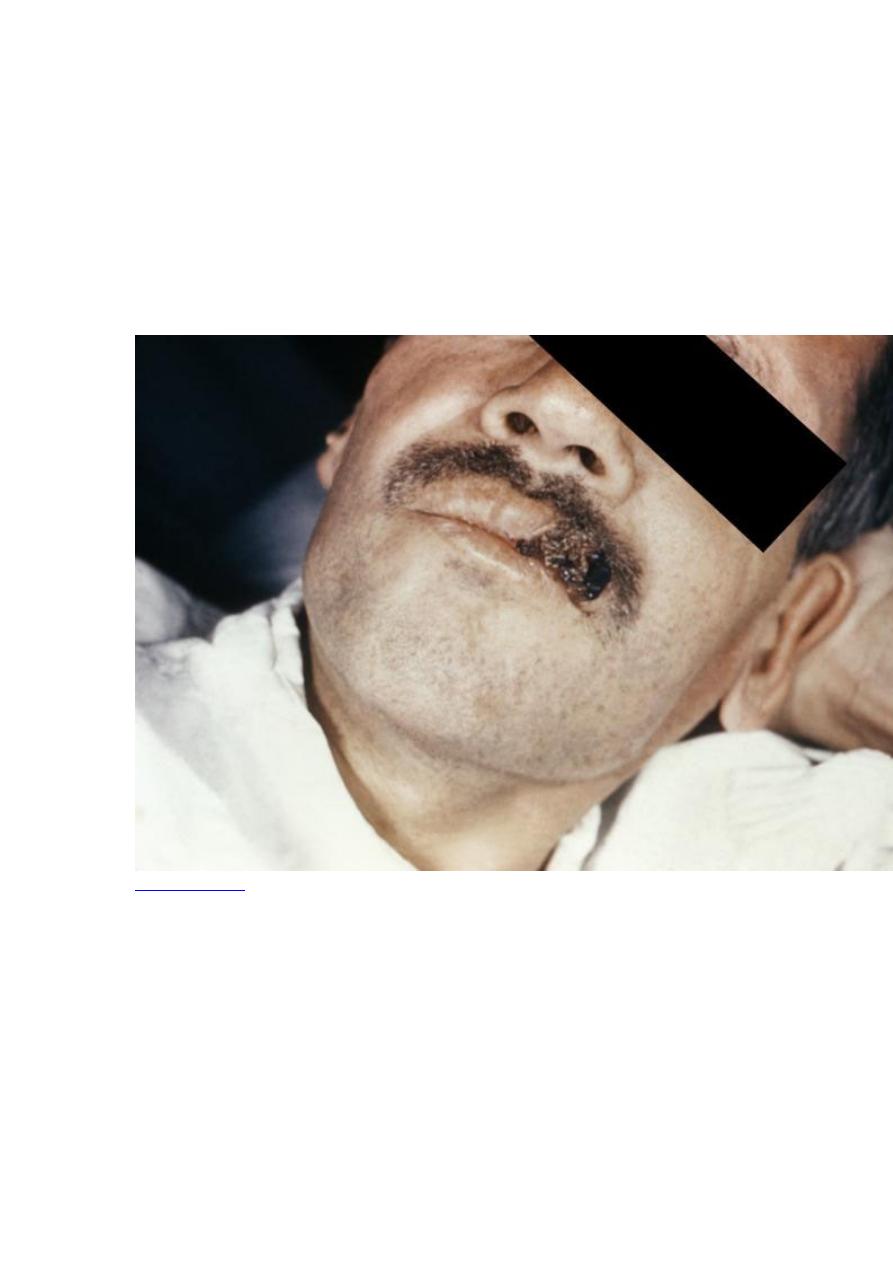
Progressive disseminated histoplasmosis characteristically includes generalized
involvement of the reticuloendothelial system, with hepatosplenomegaly,
lymphadenopathy, bone marrow involvement, and sometimes oral or GI ulcerations.
The course is usually subacute or chronic, with only nonspecific, often subtle
symptoms (eg, fever, fatigue, weight loss, weakness, malaise); the condition of HIV-
positive patients may inexplicably worsen. The CNS may become involved, causing
meningitis or focal brain lesions. Adrenal infection is rare but may result in Addison
disease. Severe pneumonia is rare, but patients with AIDS may develop severe acute
pneumonia with hypoxia suggesting Pneumocystis jirovecii infection, as well as
hypotension, mental status changes, coagulopathy, or rhabdomyolysis.
Fibrosing mediastinitis, a chronic but rare form, ultimately causes circulatory
compromise.
Patients with histoplasmosis may lose vision, but organisms are not present in ocular
lesions, antifungal chemotherapy is not helpful, and the link to H. capsulatum
infection is unclear.
Diagnosis
Histopathology and cultures
Antigen testing

The index of suspicion must be high because symptoms are nonspecific. Chest x-rays
should be done and may show the following:
In acute infection: Normal or a diffuse nodular or miliary pattern
In chronic pulmonary histoplasmosis: Cavitary lesions in most patients
In progressive disease: Hilar adenopathy with diffuse nodular infiltrates in
about 50% of patients
Bronchoalveolar lavage or tissue biopsy may be necessary to obtain histology
specimens; serologic testing and culture of urine, blood, and sputum specimens are
also done. Because culturing Histoplasma can pose a severe biohazard to laboratory
personnel, the laboratory should be notified of the suspected diagnosis.
Microscopic histopathology can strongly suggest the diagnosis, particularly in patients
with AIDS and extensive infections; in such patients, intracellular yeasts may be seen
in Wright- or Giemsa-stained peripheral blood or buffy coat specimens. Fungal
culture confirms the diagnosis. Lysis-centrifugation or culture of buffy coat improves
the yield from blood specimens.
A test for H. capsulatum antigen is sensitive and specific, particularly when
simultaneous serum and urine specimens are tested; however, cross-reactivity with
other fungi ( Coccidioides immitis, Blastomyces dermatitidis, Paracoccidioides
brasiliensis, Penicillium marneffei) has been noted.
Prognosis
The acute primary form is almost always self-limited, although very rarely, death
occurs after massive infection. Chronic cavitary histoplasmosis can cause death due to
severe respiratory insufficiency. Untreated progressive disseminated histoplasmosis
has a mortality rate of > 90%.
Treatment
Sometimes no treatment
For mild to moderate infection, itraconazole
For severe infection, amphotericin B
Acute primary histoplasmosis requires no antifungal therapy unless there is no
spontaneous improvement after 1 mo; itraconazole 200 mg po is given tid for 3 days,
then once/day for 6 to 12 wk. Fluconazole is less effective, and other azoles are not
well-studied but have been used successfully. Severe pneumonia requires more
aggressive therapy with amphotericin B.
For chronic cavitary histoplasmosis , itraconazole 200 mg po is given tid for 3 days,
then once/day or bid for 12 to 24 mo. Other azoles or amphotericin B is used if
patients are seriously ill or do not respond to or tolerate itraconazole.
For severe disseminated histoplasmosis , liposomal amphotericin B 3 mg/kg IV
once/day (preferred) or amphotericin B 0.5 to 1.0 mg/kg IV once/day for 2 wk or until

the patient is clinically stable is the treatment of choice. Patients can then be switched
to itraconazole 200 mg po tid for 3 days, then twice/day continued for 12 mo after
they become afebrile and require no ventilatory or BP support. For mild disseminated
disease, itraconazole 200 mg po tid for 3 days, then twice/day for 12 mo can be used.
In patients with AIDS, itraconazole is given indefinitely to prevent relapse or until
CD4 cell counts are > 150. Blood levels of itraconazole and Histoplasma antigen
levels should be monitored during therapy. Fluconazole may be less effective, but
voriconazole and posaconazole are very active against H. capsulatum and may be
effective in the treatment of patients with histoplasmosis. Further data and experience
are required to determine which drug is the best in each clinical situation.
