Salivary glands diseases
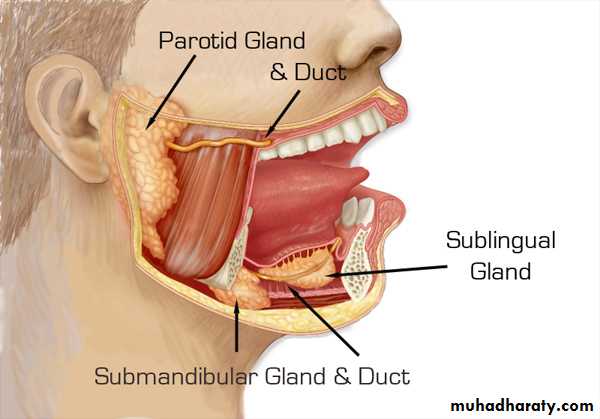
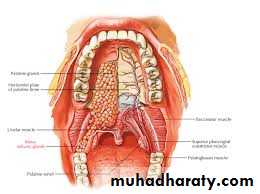
Diagnosis and management of salivary glands diseasesSalivary glands (S.Gs) may be classified as major and minor glands. Major glands are paired glands. They are parotid, submandibular and sublingual glands. There are numerous minor S.Gs, which are widely distributed in the oral cavity.
Other classification based on the type of secretion, the S.Gs may be grouped as serous (parotid gland), mucous (sublingual and minor glands), and mixed (submandibular gland).The S.Gs function to produce saliva, which serves as a lubricant, immunologic, digestive and cleansing properties. The saliva volume secreted by the glands is about 1500ml/day (submandibular glands provide saliva about 70%, parotid glands provide 25%, sublingual glands provide 3%-4%, and minor salivary glands provide about 1%).
Surgical anatomy:
I .Parotid gland1. Located in the retromandibular fossa in an area anterior and inferior to external auditory canal.
2. The parotid duct (Stensen's duct) emerges at the anterior part of the gland. It passes horizontally across the masseter muscle, piercing the buccinators muscle, then turn at right angles to reach the oral cavity. Stensen's duct opening is seen as a papilla in the buccal mucosa of the cheek opposite the maxillary second molar. Stensen's duct is about 1-3 mm in diameter and 6 cm in length.
3. Parotid gland has close association with external carotid artery and retromandibular vein.
4. The facial N. emerges through stylomastoid foramen, then enters the substance of parotid gland and divides the gland into superficial 80% and deep 20% parts.
5. The parotid gland receives sensory and autonomic innervations Sensory innervation supplied by the auriculotemporal nerve (branch of mandibular nerve V3). The parasympathetic innervation by preganglionic fibers of glossopharyngeal nerve synapse with the otic ganglia and the postganglionic parasympathetic fibers carried by the auriculotemporal nerve to the parotid gland.
Clinical considerations:
1. Because the fibrous fascia is covering the parotid, its inflammatory swelling is tense and hard.2. The parotid duct is wider at some distance before the opening, and the right angle turn of the parotid duct leads to stagnation of saliva, stone formation, and inflammation.
3. The close association of the facial N. with the gland is very important consideration, during the surgical procedures.
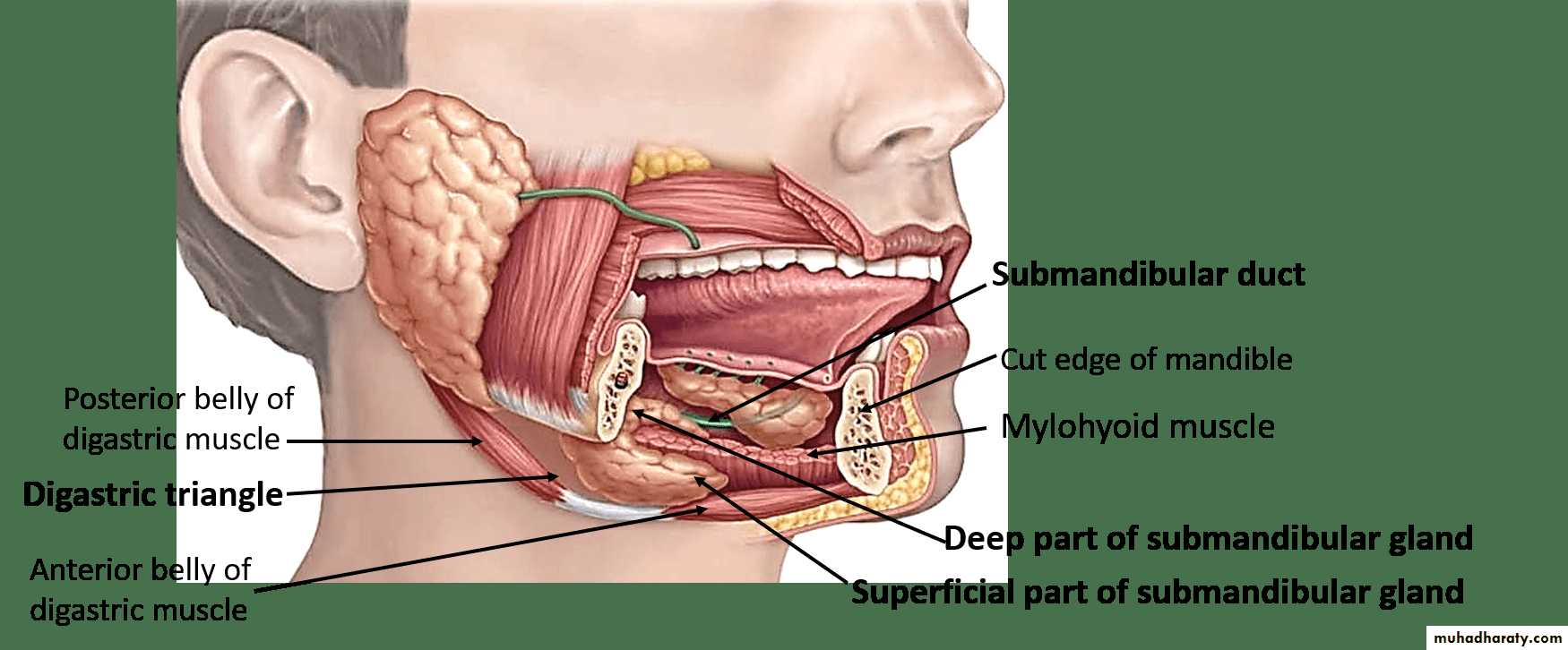
II. Submandibular gland
1. It is located in the submandibular space.2. The gland has superficial and deep parts. The superficial part is overlaying mylohyoid and hyoglossus muscles. The deep part is deep to mylohyoid muscle.
3. The submandibular duct (Warton's duct) emerges from the deep part of the gland and opens at the sublingual papilla in the floor of the mouth; lateral to the lingual frenum. Warton's duct is about 2-4 mm in diameter and 5cm in length
4. There are important nerves and blood vessels in relation to submandibular gland: mandibular branch of facial N., lingual N., hypoglossal N., facial artery and facial vein.
5. The submandibular and sublingual salivary glands are innervated by the facial N. via the chorda tympani nerve through the submandibular ganglion.
Clinical considerations:
1. The submandibular gland and duct located at a lower level to the oral cavity. It makes the gland prone to retrograde infection by oral flora.2. The Warton's duct is wider before reaching the papilla, and the sharp bend of the duct at the posterior border of the mylohyoid muscle allows stagnation of saliva and favoring the formation of salivary stones .
III. Sublingual gland
1. It is located in the sublingual space, just beneath the mucosa of floor of the mouth.2. It drains saliva by several short ducts (8-20 ducts) directly into the oral cavity or into the submandibular duct through the Bartholin's duct (main sublingual duct).
IV. Minor salivary glands
More than 800 minor S.Gs may be present in the oral cavity. These are in groups scattered all over the mouth (palate, buccal mucosa and floor of the mouth). These glands have numerous short ducts.Clinical considerations:
1. The sublingual gland and the minor S.Gs have short ducts, where the chances of stasis are less. Thus, the salivary stones rarely occur in these glands.
2. Since the sublingual and minor salivary glands are located superficially beneath the mucosa, the traumatic lesions such as mucoceles commonly affect these glands.
Classification of salivary gland diseases
1. Developmentala. Aplasia -absence of the gland
b. Atresia- absence of the duct
c. Aberrancy-ectopic gland
2. Saliva gland infection (Sialadenitis)
3. Obstructive (Sialolithiasis)
4. Mucous retention or extravasation phenomena
5. Salivary gland dysfunction (Xerostomia & Sialorrhea)
6. Autoimmune disease (Sjögren's syndrome)
7. Necrotizing sialometaplasia8. Tumors:
a. Benign tumors:
(Pleomorphic adenoma, Warthin's tumor, Monomorphic adenoma , Basal cell adenoma, Myoepithelioma, Canalicular adenoma, ).
b. Malignant tumors:
(Mucoepideromoid carcinoma, Adenoid cystic carcinoma, Papillary cystadenocarcinoma, Acinic cell carcinoma, Malignant oncocytoma etc.).
Sialadenitis
Infection of the S.Gs is known as Sialadenitis. Viral and bacterial infections are the major causes for sialadenitis. It may be acute or chronic.
1. Acute sialadenitis
Acute infection of S.Gs may be due to viral or bacterial infection.
A. Viral infection
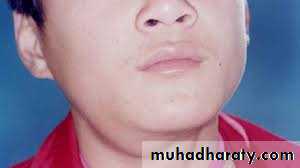
mumps is the most common viral infection affecting the parotid salivary glands, which is caused by a para-myxo virus. It is an acute, infectious disease.
Clinical features:
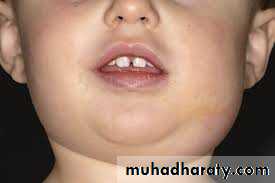
Few days fever, headache, chills, malaise and xerostomia followed by pain below the ear and sudden onset of firm, rubbery swelling of the S.Gs. usually affecting both sides of the parotid glands and mostly affect the children:Investigations
1.Increased level of serum amylase.
2. Demonstration of antibodies may confirm the disease.
Treatment:
it is self - limiting. Symptomatic relief can be given by oral fluids, analgesics and antipyretics. Antibiotic can be given to prevent the secondary infection. Mumps can be prevented in 95% of cases by having the routine MMR (measles, mumps and rubella) vaccination in childhood or later in life.B. Bacterial infection:
Mostly affecting parotid glands by bacterial infection (staph. Aureus , staph. Pyogenes or strept Virdans) it affects the neonate, children and adults with poor oral hygiene. Predisposing factors are drugs (tranquilizers, antidepressant, antihistamines, and diuretics) which decrease the salivary flow that increased chance of S.G infection.
Clinical features:
Sudden onset of pain at the angle of the mandible, usually unilateral. The affected gland is enlarged and tender. The overlying skin is worm and red. There is purulent discharge from Stensen 's duct, which can be seen on pressing the papilla.Investigations:
1. Leukocyte (WBC) count is high (leucocytosis).2. Swab taken from the purulent discharge from papilla, for culture and sensitivity test
Treatment:
1. Antibiotic (cephalosporin or oxacillin)2. Palliative treatment (hydration, stimulation of salivation by chewing sialogogues, and improve the oral hygiene), If there is no improvement then do:
3. Surgical drainage, by using fine needle aspiration guided by CT scan or Ultrasonography.
2. Chronic sialadenitis
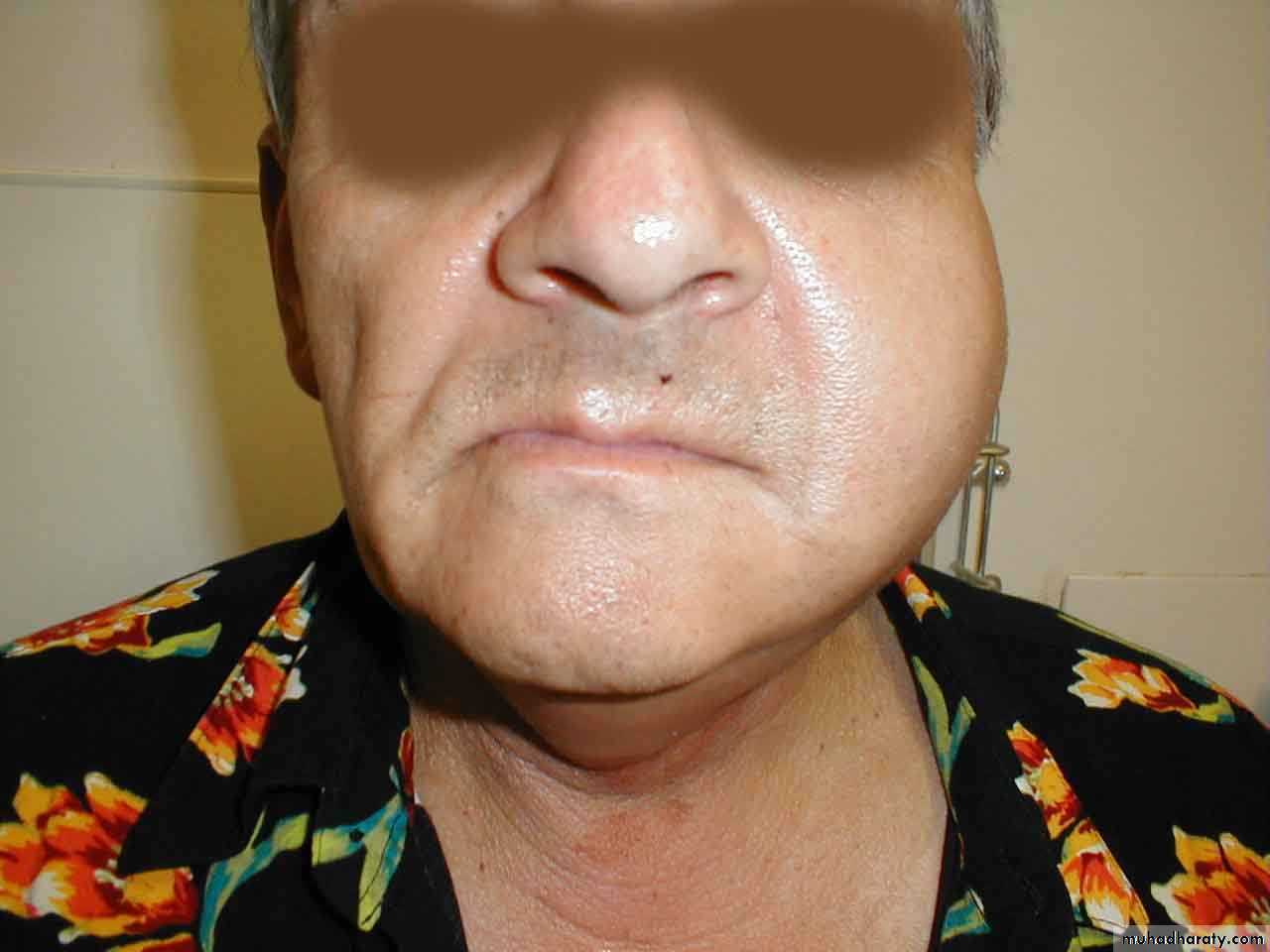
This may follow the acute infection of the S.G or may occur after pneumonia, diseases causing high febrile, papillary obstruction due to ill fitting denture or duct stone (Sialolithiasis); causing inflammation and blockage of S.G. duct. The resultant sialadenitis produce stricture of the duct, stasis, dilatation, stone formation and chronic recurrent infection.Clinical features:
current swelling of the S.G. which is firm, tender and palpable bimanually and mostly affecting the submandibular gland.
Investigations:
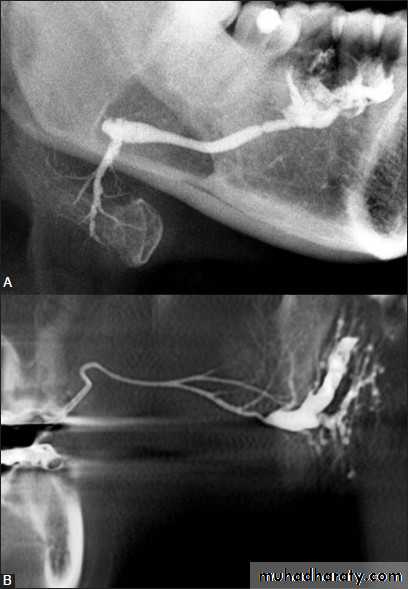
Sialography
Treatment:
l. Antibiotic (cephalosporin or oxacillin)2. Conservative treatment including removal of the obstruction, dilation of the duct, drainage of the abscess,. Diagnostic and therapeutic sialography may treat the condition.
3. If there is recurrent infection and not responded to treatment, surgical removal of the gland is necessary.
Sialolithiasis:
Sialolithiasis is the formation of sialolith (salivary calculi, salivary stone) in the salivary duct or gland resulting in the obstruction of the salivary flow. About 90% of the sialoliths form in the submandibular gland.The etiological factors for Sialolithiasis in the submandibular gland may be due to:
• long, curved Warton's duct which increases the chance of entrapment of organic debris.
• plus the secretion of this gland is higher in calcium content and thick in consistency.
• the position of the gland.
• Other factors like inflammation, local irritation or drugs, all these factors can cause stagnation of saliva leading to the buildup of an organic nidus , which will calcify . the sialolith occur in a wide variety of sizes and shapes lead to saliva stasis, infection, and finally atrophy of the S.G
Clinical features:
It may occur at any age, common in the middle aged, pain and swelling during eating and xerostomia. On examination the stone may palpated, especially if present at the peripheral aspect of the ductInvestigations:
1. Radiographs: OPG, Posteroanterior, True lateral, oblique lateral of mandible or intraoral occlusal views shows the calcified stone.2. Sialography: reveals dilation of the duct and site of the stone even if it is un calcified (radiolucent).
Treatment:
Surgical removal of the stone, however, if the removal of the stone leads to extreme damage to the gland, may indicate surgical excision of the gland.Mucous retention or extravasation phenomena Mucocele:
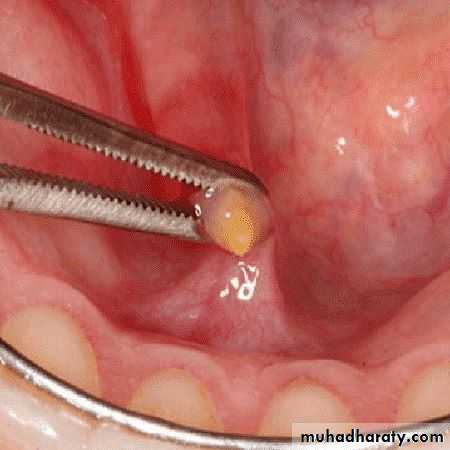
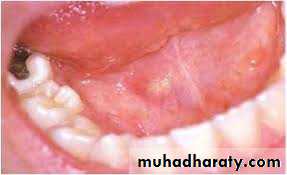
This is a swelling due to accumulation of saliva, as a result of obstruction or trauma to the minor S.G ducts. Secretions accumulate within the tissues and produce a pseudocyst (without a true epithelial lining) that contains thick, viscous saliva. There are two types of mucoceles: Extravasation type and Retention typeMucous extravasation
it is caused by trauma (mainly biting of lip or cheek) leading to the laceration of the duct, resulting in extravasation of the mucin into the connective tissue.Mucous retention
It is caused by obstruction of the duct by sialolith, scar or by tumor leads to the accumulation of the saliva within the gland and ducts, it is mainly affects minor S.G of palate.Clinical features:
Painless recurrent swelling; Mucocele may occur superficially and appear as bluish translucent and fluctuant, or may occur deep and covered by normal appearing mucosa and it is firm.Investigations: Biopsy
Treatment: Surgical excision
Ranula
It is a special type of mucocele, and considered as a mucocele of the sublingual salivary gland, result from mucous retention or extravasation. It starts as painless swelling on one side of the floor of the mouth. The swelling is fluctuant. It may be superficial or deep, superficial ranula have bluish translucency, the deep ones have the color of the mucosa. Rarely herniate the mylohyoid muscle resulting as swelling in the neck called “plunging ranule”Investigations: Aspiration biopsy
Treatment : Marsupialization
Salivary gland dysfunction
Xerostomia:
it is a condition of dry mouth due to decreased glandular secretion. It affects women more than men. This condition occurs due to aging, duct obstruction, medications (antihistam antidepressant, antihypertensive, anticholinergic drugs), excessive smoking, local radiation therapy, Sjogren's syndrome, diabetes, etc..
Treatment:
Conservative treatment; including maintenance of oral hygiene, use of sialogogues as pilocarpine but not more than 30 mg per day.Sialorrhea (ptyalism):
It is excessive salivation i may be mild, intermittent or continuous profuse drooling. This condition occurs due to irritation from ill fitting denture teething rabies , heavy metal poisoning mentally retarded children, medicine (cholinergic agonist)Treatment:
Anticholinergic medication (atropine) and physical therapy.
Sjögren's syndrome
It is an inflammatory disease that can affect many different parts of the body, but mostly affect the tear and salivary glands. Sicca syndrome, which is characterized by xerostomia and dry eyes only; and the Sjögren's syndrome which is composed of Sicca syndrome and associated connective tissue disorder, most commonly rheumatoid arthritis. This is a condition consisting of dry eye, dry mouth and rheumatoid arthritis. The etiology is unknown, mainly autoimmune disorder.Clinical features:
Painless swelling of the salivary glands and the patient complains from xerostomia, dental caries, gingivitis, acute pseudomembranous candidiasis (thrush), burning sensation and ulceration on the oral/ conjunctival mucosa, also the patient has rheumatoid arthritis. Women more affected than men.Investigations:
1. Laboratory investigation: Rheumatoid factor, antinuclear antibodies and increased ESR.
2. Sialogram: demonstrates the cavity defects which are filled with radiopaque contrast media, producing the “snow storm" appearance.
Treatment:
Symptomatic treatment with artificial tears and salivary substitutes. Medical management include Hydroxy chloroquine (Antimalarial) or prednisolone , immuno-suppressants ( methotrexate, Azathioprine, Cyclophosphamide).Necrotizing sialometaplasia
This condition is an inflammatory lesion of unknown etiology, which affects the minor S.Gs of lip, palate or retro-molar pad. Trauma leads to ischemia, acinar necrosis and squamous metaplasia of the duct. Since the lesion mimics a malignant lesion, both clinically and histologically, the diagnosis should be carefully done. The lesion occurs as a large ulcer or ulcerated nodule, which is well demarcated from the normal tissue.Investigations: Biopsy
Treatment:
Irrigation by hydrogen peroxide or saline and application of gentian violet. The lesion is self-limiting and heals in 6-8 weeks by secondary intention.Tumors of S.Gs
The tumors of the S.G can affect the major and the minor gland. These tumors may be benign or malignant lesions. S.G tumors occur much more commonly in the major glands which is about 80%, while about 20% in the minor glands. Additionally 80% of major gland tumors are benign, whereas 50% of minor gland tumors are benign.Benign tumors:
Pleomorphic adenoma, Warthin's tumor, monomorphic adenoma, Basal cell adenoma, Canalicular adenoma, Oxyphilic adenoma, MyoepitheliomaPleomorphic adenoma
Pleomorphic adenoma derives its origin from epithelial and myo-epithelial elements, and constitutes about 90% of all the benign tumors involving the S.Gs. it can affect both major and minor S.Gs commonly affects the parotid gland, followed by minor S.G of the palate and lip, and less frequently affect the submandibular glandClinical features:
The tumor starts as a small painless nodule, at the angle of the mandible or beneath the ear lobe, deep lobe tumors present with fullness in retromandibular area along with soft palate swelling. The nodule slowly increases in size to a very large size, firm in consistency, movable (without fixity to deeper tissues or to overlying skin). Palatal lesion may show fixity to the underlying bone, but doesn't invade the bone.Investigations:
1. Sialogram: As the neoplasm enlarges it displaces the glandular tissue and its duct system to the periphery producing "grasping fingers" appearance in sialogram.2. CT scan, MRI & USG
3. Biopsy (FNA, incisional & excisional biopsy)
Treatment:
Surgical excision of the tum or. Radiotherapy is contraindicated because the tumor is radioresistant.Prognosis:
1. The incomplete excision of the tumor may lead to recurrence.
2. The long-standing untreated benign pleomorphic adenoma may undergo malignant transformation.
Warthin's tumor (papillary cystadenoma lymphomatosum)
It is the second most common benign tumor of the parotid gland. It is more comm in older white men and likely to be bilateral in 10% of the cases.
Clinical features:
Painless, slowly growing benign tumor affects the parotid gland. The tum0 is firm, movable, non- tender beneath the ear lobe.
Investigations:
1. Sialography: Sialogram shows displacement of glandular tissue by tumor.
2. CT scan, MRI & USG
3. Biopsy (FNA, incisional, excisional)
Treatment: Surgical excision
Malignant tumors:Mucocpideromoid carcinoma, Adenoid cystic carcinoma, Malignant mixed tumor, Acinic cell carcinoma are the com malignant tumors involving the S.Gs.
Mucoepideromoid carcinoma
This malignant tumor exhibits a very varible degree of agresiveness. Some tumors grow rapidly,while others grow slowly .the tumor is painless unless infection or invasion of vital structures
occurs Mostly g affect the parotid gland, but may affect minor S.G of palate. It is firm indurated and not movable
Investigations:
1. Sialography: cavitations may appear where necrosis has occurred and hyperplastic glandulartissue.
2. CT scan & MRI
3. Biopsy (FNA, incisional, excisional)
Treatment: Surgical excision of the tumor, radical neck dissection not indicatcd unless there is regional node metastasis. Iradiation may be benefit in controlling metastasis and for palliative therapy.
Adenoid cystic carcinoma (Cylindroma)
It arises as a slow or rapid growing swelling, but has a greater potential for local destruction and invasiveness particularly along the perineural, lymphatics and bone. It is hard, fix mass anesthesia of the overlying skin and muscle paralysis.
Investigations:
1-Sialography: cavitations resulting from necrosis and hyperplastic glandular tissue.
2- CT scan & MRI
3- Biopsy (FNA, incisional, excisional)
Treatment:
Surgical excision of the tumor associated with radical neck dissection when indicated. Irradiation isbenefit in controlling metastasis and for palliative therapy.