Dr.KHALID WISSAM
Lec 2Diseases of Respiratory System
Diffuse pulmonary disease:
Obstruction airway diseases (excluding tumor and foreign body): include (asthma, emphysema, bronchitis, bronchiectasis, cystic fibrosis and bronchiolitis).Emphysema and chronic bronchitis are often clinically grouped together and referred to as chronic obstructive pulmonary disease (COPD),
Restrictive lung disease:
Extra pulmonary disease: that affect the movement of the chest wall (obesity-scoliosis, kyphoscoliosis and neuromuscular disorder).
Pulmonary causes :
Acute : as acute respiratory distress disease .
Chronic: as pneumoconiosis, sarcoidosis, idiopathic pulmonary fibrosis.
Obstructive lung diseases
Asthma :reversible episode of bronchial spasm result from an exaggerated bronchial constriction in response to various stimuli.
Clinically manifest by episodic dyspnoea , cough and wheezing. It is of two types:
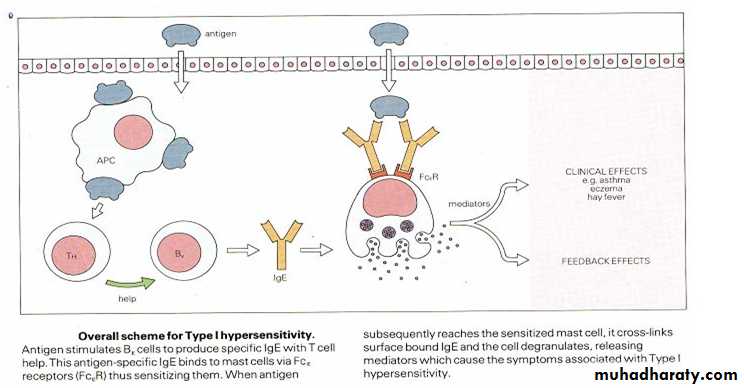
Atopic asthma : in which the attack is initiated by type І hypersensitivity reaction induced by exposure to extrinsic antigen. Serum IgE level is elevated as well as blood eosinophilic count.
Non Atopic asthma: in which the triggering mechanism are not immune.
• Several stimuli include: pulmonary viral infection, cold , exercise & psychological stress.
• There is no personal or family history of allergic manifestation and serum IgE is normal.
Asthma
Pathogenesis:
Asthma
Asthma
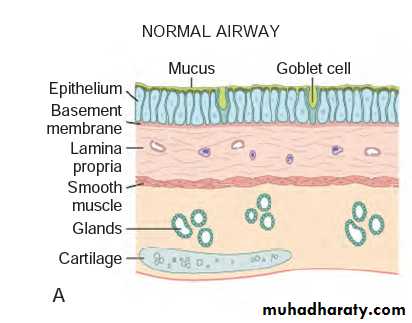
Gross: over inflation of the lung; occlusion of the bronchi by thick tenacious mucus plug.M: the mucus plug contain whorls of shed epithelium and numerous eosinophils.
The mucosa show marked edema, heavy inf. cell infiltrate (eosino. form 50% + lymphocyte &. Mast cell) increase in number of goblet cell; thicker basement. Submucosa show enlargement of mucus glands and hypertrophy of smooth muscle
Emphysema
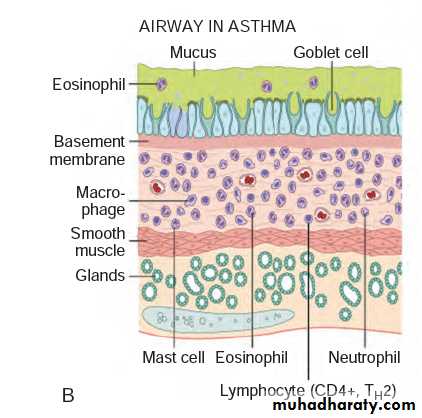
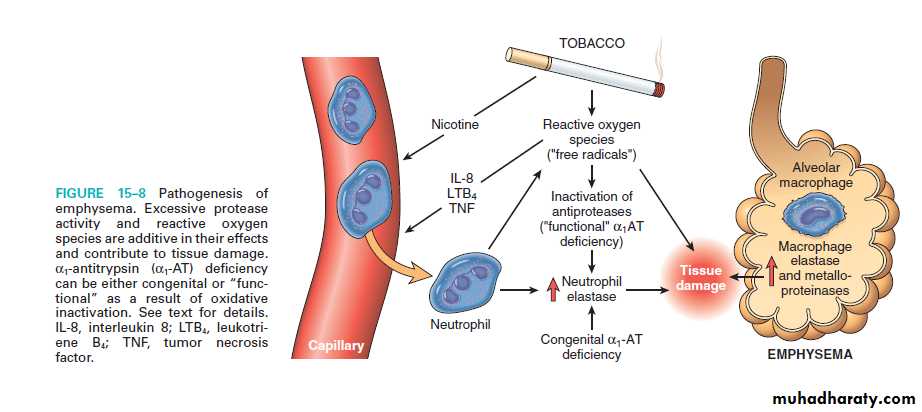
Emphysema: permanent enlargement of airspaces distal to the terminal bronchiole accompany by destruction of their walls.Pathogenesis of Emphysema
Types of emphysema:
Centriacinar emphysema : dilatation involve respiratory bronchioles only so normal and emphysematous airspaces are found within the lobule. The lesion more severe in the upper lobes. It is more common in heavy smoker.Panaciner emphysema: the whole acini is involved (from respiratory bronchiole to the alveoli) and more common in the lower lung zone and associated with alpha 1 antitrypsin deficiency.
Distal acinar emphysema.
Irregular emphysema.
Emphysema
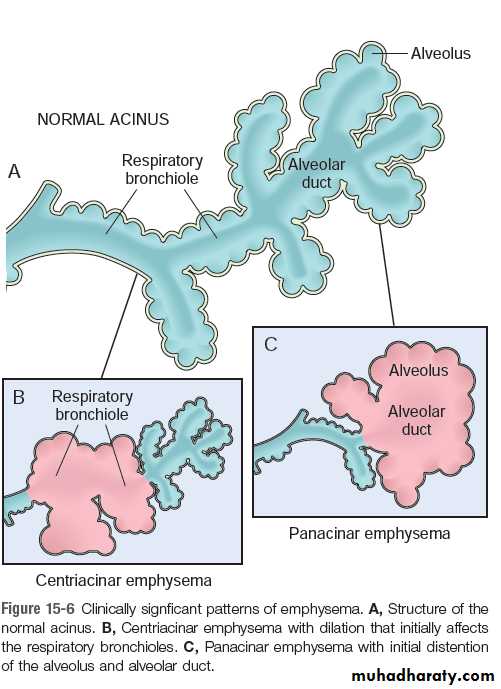
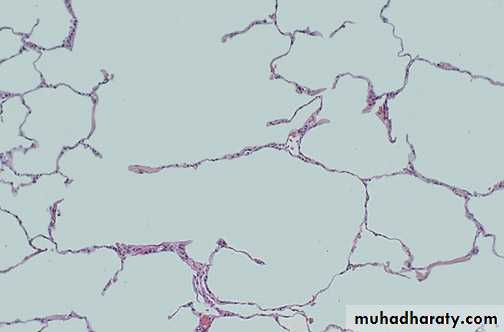
Gross : voluminous lungs, Large alveoli can easily be seen on the cut surface of fixed lungsMicroscopically, abnormally large alveoli are separated by thin destructed septa with only focal centriacinar fibrosis.
Emphysema
Clinical feature:
dyspnoea
weight loss
cough and wheezing.
Complication:
secondary pulmonary hypertension is usually develop and death occur either due to respiratory failure, or due to right sided heart failure.
Chronic bronchitis:
Chronic bronchitis is defined clinically as persistent cough with sputum production for at least 3 months in at least 2 consecutive years, in the absence of any other identifiable cause.Chronic bronchitis:
Pathogenesis:The commonest causative agent is cigarette smoking, in addition to other pollutant such as SO2, NO2.
these irritants cause bronchial hyper secretion , hyperplasia of mucous gland and formation of mucous secreting goblet cells.
Also they cause inflammation with infiltrate by T lymphocyte Macrophage and neutrophils.
The role of smoking; it interfere with ciliary movement , damage the bronchial epithelium & inhibit the ability of epithelium & leukcocyte to clear bacteria.
Chronic bronchitis:
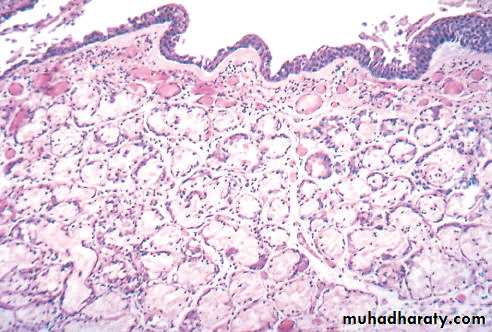
Gross: The lining of the bronchi become swollen and hyperemic and covered by mucinous or mucopurulent secretion.M: enlargement of mucous secreting gland, increase in the number of goblet cell with loss of ciliated columnar epithelial & stratified squamous metaplasia is seen mononuclear inflammatory cell together with neutrophils.
Chronic bronchitis:
Clinical features :Cough & sputum.
COPD with outflow obstruction, this is accompanied hypercapnia, hypoxia and cyanosis .
complication it may be complicated by pulmonary hypertension and cardiac failure. Recurrent infection and respiratory failure are constant features
Bronchiectasis :
Permanent dilatation of bronchi and bronchioles proximal to the terminal bronchiole , due to destruction of muscle & elastic supporting tissue resulting from or associated with chronic necrotizing infection.Pathogenesis:
Two processes play in the pathogenesis of Bronchiectasis:
• 1- Obstruction.
• 2- chronic persistent infection.
Bronchiectasis
Pathological appearances:Grossly : It affect the lower lobes , usually bilateral . the dilated bronchi form cavities of variable size lined by thick fibrous wall . the surrounding lung tissue show consolidation .
Microscopic features :
Suppurative exudates in the lumen . the mucosa show ulceration with squamous metaplasia . the wall of bronchi is heavily infiltrated by chronic inflammatory cells . the surrounding alveoli show evidence of consolidation i.e.( accumulation of inflammatory exudates & cells in the alveolar spaces ) .
Bronchiectasis
Clinical feature:
Severe, persistant cough with mucopurulent bad odor sputum which may contain stretch of blood sometime frank haemoptysis occur. Clubbing of the finger may develop .
Complication:
Sever bronchiectasis causes hypercapnia, hypoxia and pulmonary hypertension and rarely causes corpulmonale , brain abscess , amyliodosis is a rare complication.The Pleura
Pleural effusion: collection of fluid in the pleural cavity. It may lead to collapse of the lung and interfere with respirationPleural effusion may be:
Transudate pleural effusion (hydrothorax) :is due to :
1.Heart failure: due to increase hydrostatic pressure in pulmonary veins
2. Hypoproteinaemia due to renal or liver diseases leading to decreased oncotic pressure
3. Meigs' syndrome : ovarian fibroma associated with right sided pleural effusion
Pleural effusion(cont)
Exudative pleural effusion:1) microbial invasion through either direct extension of a pulmonary infection or blood-borne seeding (suppurative pleuritis or empyema);
(2) cancer (lung carcinoma, metastatic neoplasms to the lung or pleural surface, mesothelioma);
(3) pulmonary infarction; and
(4) Viral pleuritis.
(5) Systemic diseases e.g. Uraemia, SLE.
Empyema
Collection of pus in the pleural cavity
Causes: spread of infection from lung, subdiaphramatic infection, blood born, trauma, from rupture esophagus
Effect:
- pressure collapse of lung.- Organization preventing lung from expansion
Haemothorax
Collection of blood in pleural cavityCauses:
1. Trauma , surgery
2. Ruptured aortic aneurysm
Effect: pressure collapse of lung
PneumothoraxPresence of air in pleural cavity
Causes:
Spontaneous pneumothorax as a result of ruptured emphysematous bulle
Traumatic: perforating wound, or during aspiration of pleural fluid, Mechanical ventilator.
Effect: Pressure collapse of lung.
Tension Pneumothorax
A ball valve like connection between pleural cavity and the lung lesion which allow air to enter the pleura during inspiration and prevents its escape during expiration
It is serious condition cause severe respiratory distress
Treatment is by chest tube
Tumors of pleura
1. Primary tumors:Malignant Mesothelioma arises from mesothelial cells.
Macroscopically: Form whitish mass compressing the lung. Asbestosis is a predisposing factor
Microscopically: it may have carcinomatous or sarcomatous appearace.
2. Secondary tumours:
More common, commonly from breast , bronchus. Usually present as haemorrhagic pleural effusion