Rheumatology L-9
Behcet's syndrome : vasculitis of unknown cause affecting characteristically venules.There is a striking geographical distribution, it being most common in Turkey, Iran and Japan.
The prevalence per 100000 is 10-15 in Japan and 80-300 in Turkey. There is a link to the HLA-B51 allele (a split antigen of B5), with a relative risk of 5-10.
CLINICAL FEATURES
there is a wide range of clinical features. The disease is characterized by unpredictable exacerbations. There is no definite investigation & the diagnosis is made depending on clinical criteria:*recurrent oral ulcerations – minor aphthous , major aphthous or herpitiform ulceration at least 3 times in a 12 month period.
Plus 2 of the fallowing :
1-recurrent genital ulceration(60-80%)2- eye lesions : anterior uveitis , posterior uveitis , cells in vitreous on slit-lamp examination, retinal vasculitis. The involvement is usually bilateral.
3- skin lesions: erythema nodosum, pseudofolliculitis, papulopustular lesions, acne form nodules, migratory thrombophlebitis& vasculitis
4- positive pathergy test: involves intradermal skin pricking with a needle, a pustule develops within 48 hours.
Other manifestations include a self-limiting peripheral mono-or oligoarthritis affecting knee, ankle, wrist and elbows; gastrointestinal symptoms of diarrhea, abdominal pain and anorexia; pulmonary and renal lesions; brainstem syndrome; organic confusional state and meningo-encephalitis.
All the common manifestations are self-limiting except ocular attacks. Repeated attacks of uveitis can cause blindness.
The pathology is highly specific to Behcet's disease. Recurrent thrombosis can occur. Renal involvement is rare.
TREATMENT
Steroid(topical), immunosuppressants& cyclosporine are used for chronic uveitis& the rare neurological complications, colchicine for skin disease& arthralgia, thalidomide 100-300 mg/day for 28 days for oral & genital ulceration , but this drug is highly teratogenic(phocomelia)& neurotoxic.Systemic manifestations require systemic steroids& immunosuppressive drugs.
Inadequate and delayed mineralization of osteoid in mature compact and spongy bone
Major deficit is in Vitamin D , which is required for Ca++ uptake in intestinesDecreased Ca++ stimulates PTH, which does increase Ca++, but also increases phosphate excretion by kidney
When phosphate levels too low, mineralization cannot occur
• Osteomalacia (Adult Rickets)
4 categories of osteomalacia &rickets can be identified based on the underlying cause:
1- deficiency of v.D or defects in v.D metabolism.
2- hypophosphatemia.
3- drug induced inhibition of bone mineralization.
4- defects in pyrophosphate metabolism.
Etiology
More prevalent in extreme preemies, elderly, those following strict macrobiotic vegetarian diets and persons on anticonvulsant Rx
Pancreatic insufficiency
Hepatobiliary diseases
Lack of bile salts decreases absorption of Vit D
Malabsorption syndromes
Hyperthyroidism
Rare in US due to fortification of foods
Common in GB and Middle Eastern Countries
Clinical Presentation
Generalized body aches /LBP as well as hip painLower extremity pain & deformity
Physical examination
Scoliosis / kyphosis of spine
Deformities of weight bearing bones
Muscle weakness leading to classic waddling gait
Generalized Malaise
Patients with chronic renal failure cannot synthesize the active metabolite of v.D(1,25(OH)2D3) due to renal damage& this causes secondary hyperparathyroidism & in some cases osteomalacia.
Diagnosis
Serum Ca++ –↓ or Normal
Serum inorganic Phosphate ↑> 5.5
Vitamin D ↓
BUN & creatinine ↑
Alkaline Phosphatase & PTH ↑
Bone bx to determine aluminum levels
X-Rays
Demineralization
Pseudofractures
Bowing of long bones
Radiological examination is of limited value unless in advanced cases where focal radiolucent area ; pseudofracture or looser's zones are seen in ribs, pelvis& long bones. Radiological osteopenia &crush vertebral fracture may cause confusion with osteoporosis.
Diagnosis of osteomalacia is confirmed with bone biopsy which shows pathognomonic increased thickness of osteoid seams.
Clinical Management
Correcting serum Ca++ & phosphorousChelating bone aluminum if needed
Suppressing hyperthyroidism
Supplement with Vitamin D
Administer Ca++ carbonate to ↓ hyperphosphatemia
Renal dialysis/transplant for renal osteodystrophy
Correction of associated intestinal disorders
The response will be rapid clinically& radiologically. After 3-4 months, the treatment can be stopped or the dose of v.D is reduced to the maintenance . Patients with chronic renal failure require 1-alpha (OH)D or 1,25(OH)2D to bypass the metabolic defect in 1- alpha hydroxylation of 25(OH)D.
Screening of serum Ca& alkaline phosphatase is needed during treatment to avoid hyperCa. Alkaline phosphatase returns to normal after treatment.
Excess of bone destruction & unorganized bone formation and repair. The 2nd most common bone disorder in the U.S.
The etiology is unknown
Usually affects the axial skeleton, vertebrae and skull, although the pelvis, tibia, femur are the other common sites of disease.
Most persons are asymptomatic & diagnosis is incidental.
Paget’s Disease (Osteitis Deformans)
Vascularity is increased in affected portions of the skeleton. Lesions may occur in one or more bones, does not spread from bone to bone.
Deformities & bony enlargement often occur. Bowing of the limbs & spinal curvature in persons with advanced disease.
Bone pain- is the most common symptom. Is usually worse with ambulation or activity but may also occur at rest. Involved bones may feel spongy & warm because of increased vascularity.
Skull pain is usually accompanied with headache, warmth, tenderness & enlargement of the head.
Pathologic fractures- because of the increased vascularity of the involved bone-bleeding is a potential danger.
Alkaline phosphatase levels- markedly elevated as the result of osteoblast activity.
Serum calcium are normal except with generalized disease or immobilization.
Gout and hyperuricemia may develop as a result of increased bone activity, which causes an increase in nucleic acid catabolism.
Radiograph reveals radiolucent areas in the bone, typical of increased bone resorption. Deformities & fractures may also be present.
Goals of the treatment- to relieve pain & prevent fracture & deformities.
Pharmacologic agents are used to suppress osteoclastic activity. Bisphosphonates & calcitonin are effective agents to decrease bone pain & bone warmth & also relieve neural decompression, joint pain & lytic lesions.
Use of analgesics & NSAIDs. Assistive devices, including cane, walker.
Deformities may be corrected by surgical intervention (osteotomy). ORIF may be necessary for fractures.
Osteoporosis
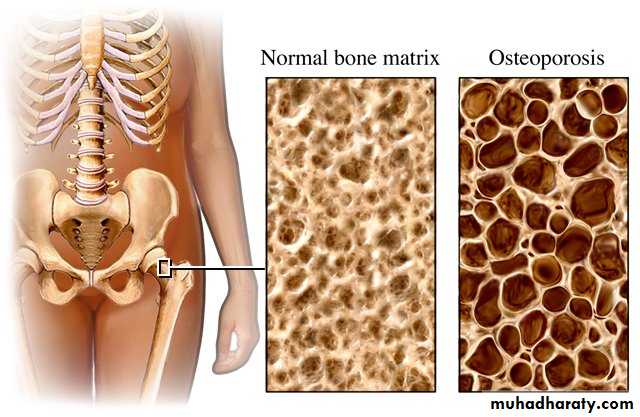
• Characterized by low bone mass and structural deterioration
•Normal homeostatic bone remodeling is altered – the rate of bone
resorption is greater than the rate of bone formation.
• Eight times more common in women than men for several reasons
• Lower calcium intake than men• Less bone mass because of smaller frame
• Bone resorption begins earlier and accelerates after menopause
• Pregnancy and breastfeeding deplete woman’s skeletal reserve of calcium
• Longevity increases likelihood of osteoporosis; women live longer than men
Risk factors (cont’d)
Excess alcohol intake
Cigarette smoking
Anorexia
Oophorectomy
Sedentary lifestyle
Insufficient calcium intake
Low testosterone levels (hypogonadism in men)
Etiology and Pathophysiology
Peak bone mass is achieved before age 20
Bone loss after midlife is inevitable but rate of loss is variable
Bone resorption exceeds bone deposition
Bones become weakened and prone to fracture, loss of height, and kyphosis.
Etiology and Pathophysiology
Diseases associated with osteoporosis
Intestinal malabsorption
Kidney disease
Rheumatoid arthritis
Hyperthyroidism
Chronic alcoholism
Cirrhosis of the liver
Hypergonadism
Diabetes mellitus
OsteoporosisDiagnostic Studies
Clinical Manifestations
Known as silent disease
Diagnosis
Bone Mineral Density (BMD)
Dual-energy x-ray absorptiometry (DEXA)
History and physical examination
Quantitative ultrasound
Treatment and Nursing Care
Diet Therapy
Weight bearing Exercises
Decrease Risk Factors
Quit smoking and decrease consumption of alcohol
Drug Treatment of Osteoporosis
Estrogen Replacement Therapy
Calcium & Vitamin D supplements
Calcitonin
Biphosphonates (Fosamax, Didronel, Actonel, Boniva, Aredia, Bonefos, Skelid)
Selective Estrogen receptor modulator – Evista
Teriparatide (Forteo)
Portion of parathyroid hormone
First drug to stimulate new bone formation
Hormone Replacement Therapy – Estrogen
Controversy over use. Should discuss with health care provider
Calcium
There are a variety of calcium supplements available
Calcium carbonate should be taken with ___food____ _ to aid in absorption since it needs high gastric acidity to be absorbed properly.
*parathyroid hormone: the main action is bone formation. The hormone should be given in an intermittent dosing to alleviate the risk of bone resorption in cases of sustained hyperparathyroidism. The available drug is teriparatide which is given as single S.C. daily dose.