Patent Ductus Arteriosus (PDA)
• approximately 5-10% of CHD (excluding premature infants).Etiology:
• Ductus arteriosus allow blood flow from the pulmonary artery to the aorta during fetal life.
• Failure of it closure result in PDA.
• With falling of PVR after birth, there is Lt-to-Rt shunt and increased pulmonary blood flow.
• It depend on the magnitude of Lt-to-Rt shunt, which determined by:
• the size of PDA• PVR (as in VSD).
• Small PDA is asymptomatic.
• Moderate-large PDA :
congestive heart failure (CHF) as the PVR decrease over the first 6-8 wks of life
Clinical Features:
• Wide pulse pressure.
• Continuous machinery murmur at Lt infra-clavicular area, with\without thrill.• Hyperdynamic precordium in large PDA.
• Split S2 occur with high pulmonary pressure.
Physical examination:
• It might be normal in small PDA.
Diagnosis:
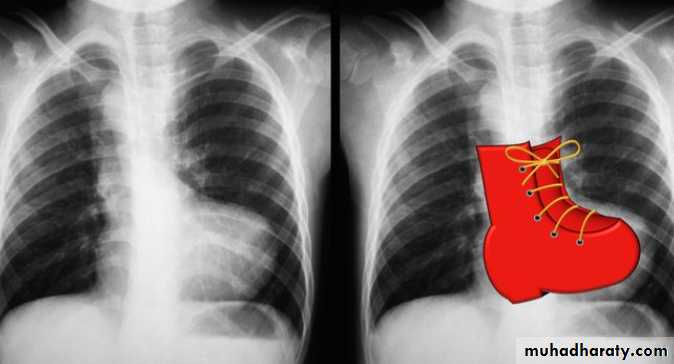
CXR:
Prominent
Pulm. AProminent
Pulm. marking
Cardiomegaly
ECG:
• Normal in small PDA• Evidence of LV or RV hypertrophy in presence of pulmonary HT.
Echocardiography: shows:
• Size of PDA• Magnitude of the Lt-to-Rt shunt
• Pulmonary pressure.
• Spontaneous closure is uncommon in full term infants.
• Treatment of CHF with diuretics and digoxin.
• Closure the PDA through the catheterization even in small PDA to prevent subacute bacterial endocarditis.
Treatment:
• Approximately 10% of all CHD.
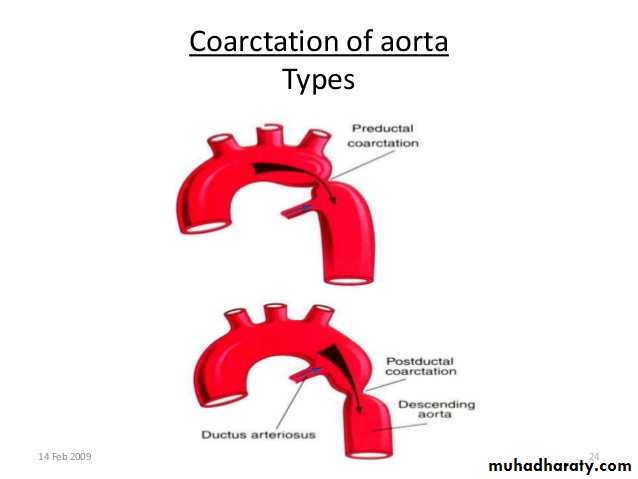
• It is almost always juxtaductal in position.• Occurs as a result of incorrect development of aortic arch near the ductus arteriosus insertion causing narrowing of aortic lumen.
COARCTATION OF THE AORTA:
• Infants:
Symptoms develop when the ductus close:• Poor feeding
• Respiratory distress
• Shock
• Femoral pulses classically weaker and delayed from the right radial pulse.
• B.pr. in the lower extremities is lower than that in the upper extremities.
Clinical Manifestations
• Older children
• are usually asymptomatic
• There may be a leg pain with exercise, headache, or epistaxis.
• Decreased or absent lower extremity pulses and hypertension ( in upper extremity).
• Machinary murmur is typically best heard in the left interscapular area of the back.
• If significant collaterals have developed, continuous murmurs may be heard throughout the chest.
• An abnormal aortic valve is present approximately 50% of cases, causing systolic ejection click and systolic ejection murmur of aortic stenosis.
• ECG show evidence of RVH in infants and LVH and mildly enlarge heart in older children..
• CXR show marked cardiomegaly and pulmonary edema.
• Rib notching may seen in older children (>8 years of age) with large collaterals.
• Echocardiography shows the site of coarctation and associated lesions.
Diagnosis:
• IV infusion of prostaglandin E1 (chemically opens the ductus arteriosus), digoxin, diuretics, and other supportive care.
• Balloon angioplasty, especially in critically ill infants, but surgical repair of the coarctation is most commonly performed.
Treatment:
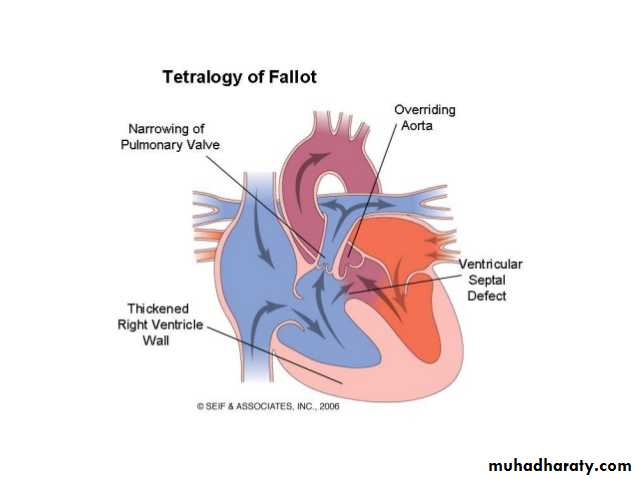
• Most common cyanotic CHD, represent 10% of all CHD.
• It consist of:
• Large, non-restrictive VSD.
• Rt ventricular out flow obstruction (pulmonary stenosis)
• Rt sided aortic arch which overriding the ventricular septum (overriding of aorta).
• Rt ventricular hypertrophy (HRV).
Tetralogy of Fallot (TOF):
• Systemic venous return to right atrium and right ventricle is normal.
• When the Rt ventricle contracts in the presence of marked pulmonary stenosis, blood is shunting across the VSD into the Lt ventricle then into aorta (Rt-to-Lt shunt) causing arterial desaturation and cyanosis.Pathophysiology:
• The severity of cyanosis depend on the degree of pulmonary stenosis.
• In the severe pulmonary stenosis the pulmonary blood flow is supplied by PDA.• Degree of Rt ventricular outflow obstruction determine the timing of onset of symptoms, the severity of cyanosis and the degree of RVH.
• In mild-moderate Rt ventricular outflow obstruction, there’s balanced shunt across the VSD and the patient is not visibly cyanosed (Acyanotic or “pink” TOF).
• When the obstruction is severe, the cyanosis present at birth and worsen with closure of ductus arteriosus.
1. Infants with mild pulmonary stenosis:
• Initially presents with heart failure due to severe Lt-to-Rt shunt across large VSD.
• Cyanosis is absent at birth, but it will appear latter in 1st year of life due to increased pulmonary stenosis secondary to hypertrophy of right ventricular infundibulum.
Clinical features:
2. Infants with severe pulmonary stenosis:
• Cyanosis in neonatal period and pulmonary blood flow is depend on the ductus arteriosus.• When the ductus begin to close over the 1st few hours or days of life it will cause severe cyanosis and circulatory collapse.
Clinical features:
• Older children with long-standing cyanosis have dusky blue skin, gray sclera with engorged blood vessels and marked clubbing of fingers and toes.
• Systolic ejection murmur due to pulmonary stenosis present in all patients which best heard at the 2nd Left intercostal space and radiate to the back.
• It’s sudden sever cyanotic attack.
• Particularly during the first 2 years of life• Due to reduction of an already compromised pulmonary blood flow
• Precipitated by:
• Excessive crying
• Vigorous exercise
• Systemic infection.
5. Paroxysmal hypercyanotic attacks “cyanotic” or “blue” or “tet” spells:
• These spells are characterized by:
• Spontaneous and unpredictable onset.
• Frequently occurs in the morning on awaking or after vigorous crying.
• Infants developed hyperpnea, increasing cyanosis, gasping breathing and might end with syncope or death.
• Temporary disappearance or reduction of ejection systolic murmur due to decrease blood flow across the aortic valve.
• The spells may last from a few minutes to a few hours.
• Short spells followed by generalized weakness and sleep• Prolong severe spells may progress to unconsciousness or convulsion or hemiparesis.
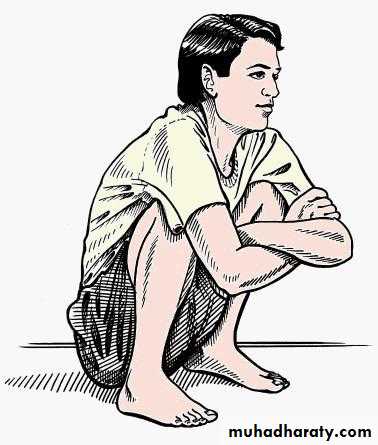
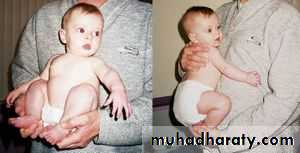
• Toddler patient adapt squatting position during the spell in attempt to increase systemic venous return and then increase pulmonary blood flow.
Infants who are only mildly cyanosed at rest are more liable to develop cyanotic attacks because they lack the homeostatic mechanisms to tolerate rapid decrease of arterial oxygen saturation such as polycythemia.
Note:
• ECG: shows Rt axis deviation and RV hypertrophy.
• CXR: shows boot-shaped heart (created by small main pulmonary artery and upturned apex secondary to RVH) and oligemic lung fields.
Diagnosis:
• Echocardiography: shows the anatomical features of TOF.
• Depending on the frequency and severity 1 or more of the following procedures should be done in sequence:• Knee-chest position of the infant may prevent progression of an early spell.
• Oxygen administration (although it will not reverse cyanosis because it’s due to intracardiac shunting).
Treatment of TOF:
1. Treatment of hypercyanotic attacks:
Knee-chest position
• S.C morphine in a dose not in excess of 0.2 mg/kg.
• IV infusion of sodium bicarbonate if the spell is severe and not responding to above measures.
• Intubation and sedation are often sufficient to break the spell which is severe and not responding to other treatments.
1. Treatment of hypercyanotic attacks:
• Drugs that increase SVR, such as I.V phenylephrine, can improve right ventricular outflow, decrease the right-to-left shunt, and improve the symptoms.
• IV propranolol (0.1 mg/kg given slowly to a maximum of 0.2 mg/kg).
1. Treatment of hypercyanotic attacks:
Treatment of TOF:
• Complete surgical repair can be performed during infancy.• Blalock-Tausing shunt a palliative shunt created between subclavian artery (systemic circulation) and pulmonary artery. It done for a complex TOF with complete repair later in life.
• Prophylactic antibiotic to prevent subacute bacterial endocarditis.
• Cerebral thrombosis: In patient < 2 years, as a complication of severe polycythemia and dehydration.
• Brain abscess: It less common than cerebral thrombosis,occurs in children older than 2 years.
• Subacute bacterial endocarditis.
Complications of TOF:
• Heart failure: Is unusual, except in young infants with “pink” or “Acyanotic” TOF and as the degree of pulmonary stenosis increase with age the symptoms of heart failure resolved and the patient develop cyanosis often at 6-12 months of age.
Thank you for your attention