
1
2
Endocrine system
2019
…
prof. razzaq alrubaee…thiqar college of medicine
….L1
Hypothalamus &pituitary gland disorder & short stature
Thyroid ¶thyroid gland disorders
Adrenal gland disorder
Type 1 diabetes DKA .complication
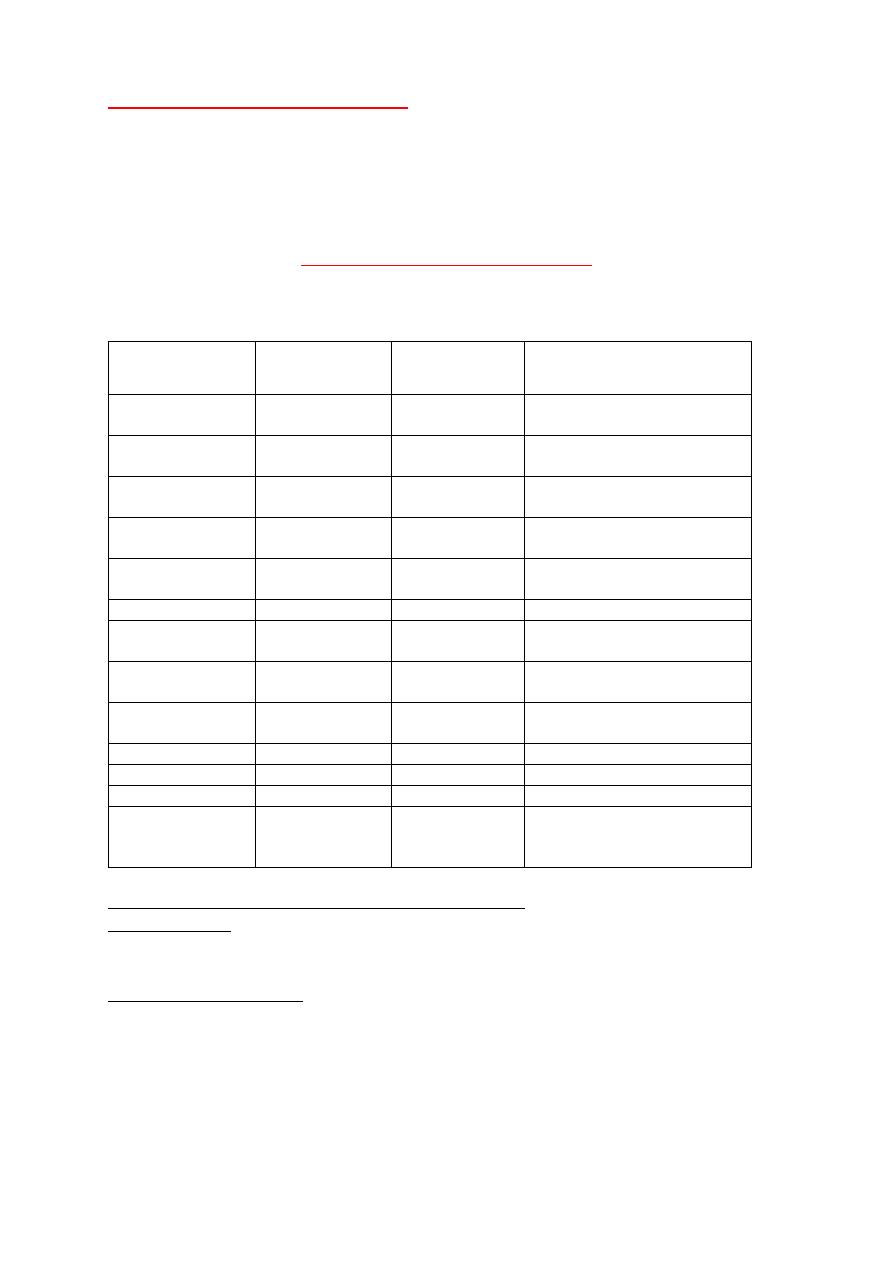
Hormones of hypothalamus and pituitary
The pituitary gland receive signals from hypothalamus & respond by sending pituitary hormones to
target glands which produce hormones that provide negative feedback at level of hypothalamus
and pituitary
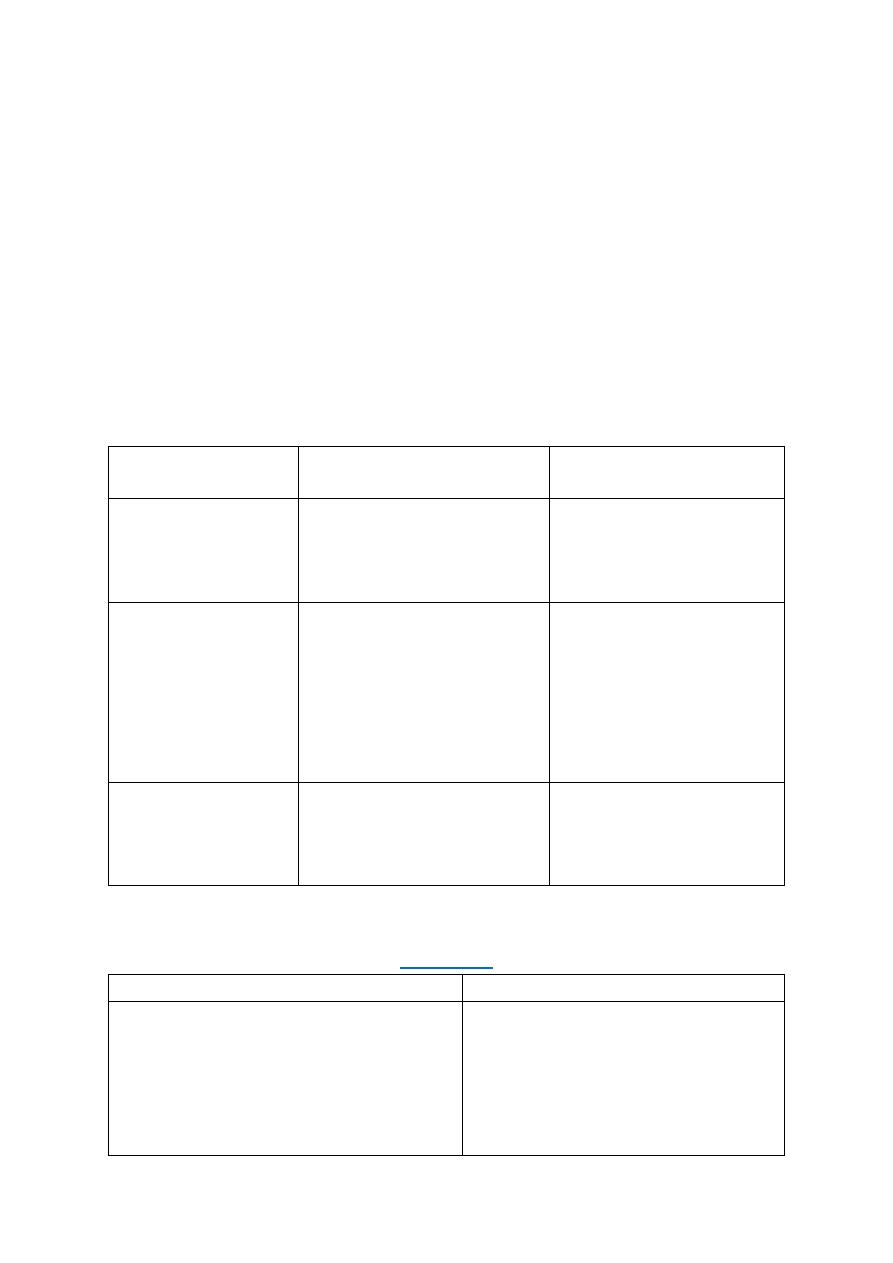
Hormones
Location
s\I(stimulate
.inhibit)
Function
ACTH
Ant. pituitary
S
Production of glucocorticoid
MC.miniralocorticoid.androgen
ADH
Post. Pituitary
S
Water reabsorption from renal
tubules
CRH. corticotropin
releasing hor.
Hypothalamus
S
Secretion of ACTH
FSH (female)
Ant. Pituitary
I
Secretion of estrogen from
ovary
FSH (male)
Ant. Pit
S
Production of sperm from
testes
GnRH
Hypothalamus
S
Secretion of LH &FSH
LH(female )
Ant. Pit
S
Ovulation and development of
corpus luteum
LH(male )
Ant. Pit
S
Production and secretion of
testosterone
Oxytocin
Post. Pit
S
Contraction of uterus at birth
&release of milk from breast
TSH
Ant. Pit
S
Secretion of T3.T4
PRL prolactin
Post. Pit
S
Promotion of milk synthesis
Somatostatin
Hypothalamus
I
Secretion of GH&TSH
TRH( thyrotropin
releasing
hormone)
Hypothalamus
S
Secretion of TSH & prolactin
Growth hormone deficiency &insensitivity (hypopituitarism )
Hypopituitarism : denotes underproduction of GH growth hormone alone or in combination with
deficiency of other pituitary hormones .
Congenital hypopituitarism :
Clinical features :
The child usually normal size and weight at birth .may have neonatal emergencies like apnea
.seizures .jaundice, cyanosis or Sever hypoglycemia with or without seizures prolonged neonatal
jaundice is common .nystagmus may suggest septooptic dysplasia . micropenis in boys can be clue
for GH def.
3
Physical exam: head is round & face is short & broad ,prominent frontal bones eyes somewhat are
bulging .mandible and chin are underdeveloped ,delayed teeth eruption and often crowded , short
neck and small larynx , high pitch voice which remain high after puberty
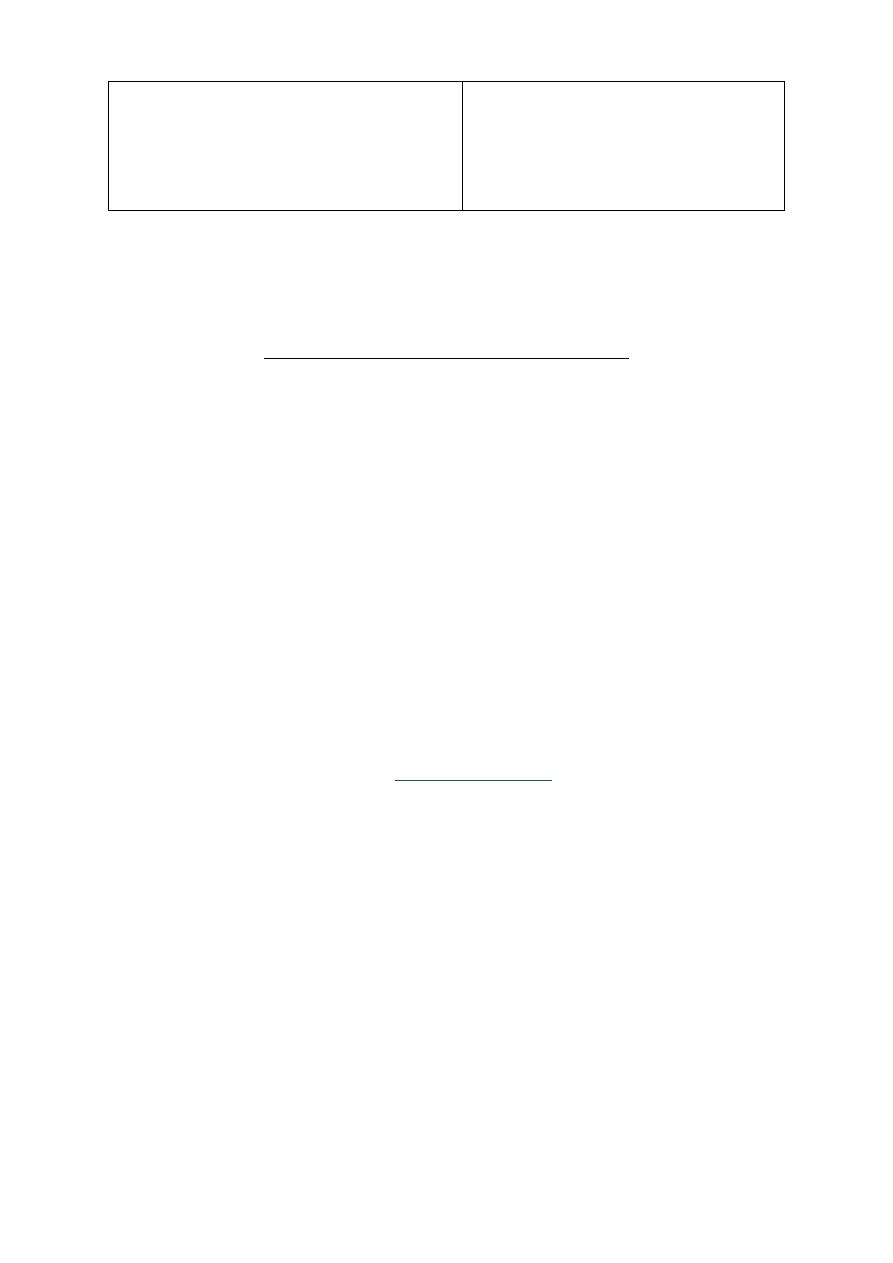
Evaluation of suspected growth hor. Def.
Growth related history &physical exam
Growth failure
Short stature
GHD affect 1in 3500 child
Image & other evaluation
Clinical diagnosis
Bone age ( delayed )
MRI,CT evaluate hypothamic
pituitary region
Lab . finding
Measures GH with stimulation ,
IGF-1 test
Rationale for treatment
Replacement with GHTshould be
started as soon as GHD is diagnosis
Diagnosis
: determined by low or absent level of GH in response to stimulation with insulin ,
arginine clonidine ,or glucagon to establish low level of GH <10 ng\ml and also necessary to
evaluate others pituitary hormones deficiency like ACTH, TSH cortisol ,gonadotropin .
Treatment
: recombinant hGH available since 1982 usually given in a dose 0.18-0.3 mg/kg/wk
during childhood and higher dose needed during puberty. Therapy should continued until near
final height is achieved and treatment discontinued if he or she tall enough or growth rate <I inch
/year and bone age >14 yr in girls &>16 years in boys
Indication of GH therapy :
1. GHD 6-Prader willi syndrome
2. Turner syndrome 7-SHOX gene abnormality (short stature homebox )
3. Chronic renal failure 8-noonan syndrome
4. Idiopathic short stature
5. Small for gestational age
Adverse effect of GH therapy .include pseudotumor cerbri ,gynecomastia ,slipped capital femoral
epiphysis & worsening scoliosis
Growth hormone insensitivity (LARON syndrome ): autosomal recessive disease.
Is a condition that occur when the body unable to utilize GH , and characterized by short stature
,hypoglycemia ,near normal at birth ,delayed puberty & short limbs (arms &legs) with obesity
.other signs include small genitals ,thin fragile hair those people have low risk of cancer and type II
diabetes .
Diagnosis :
S&S , GH usually high and reduced level of IGF1 & genetic study to show abnormality in GH gene
Treatment : no current cure for Laron syndrome & only available treatment is subcutaneously
injection of IGF1
Prognosis :generally good d not affect life span .
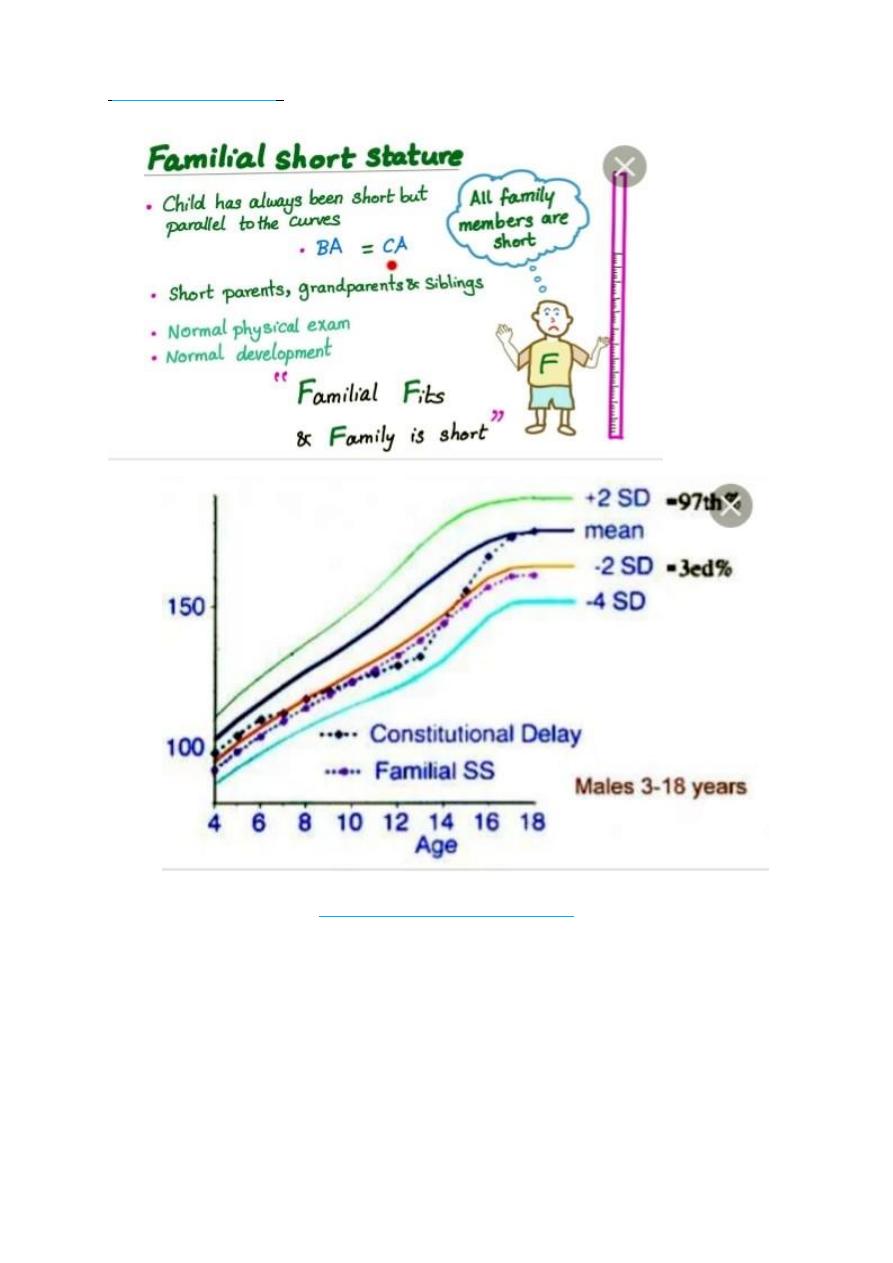
Constitutional Growth delay
: one of the variant of normal growth . length & weight normal at
birth , growth is normal for the first 4-12 months , height sustained at low percentile during
childhood ., the pubertal growth spurt delayed and eventual normal stature , normal bone age .
GH response to provocative test tend to be lower than in children with a more typical timing of
puberty . the prognosis of those children to achieve normal adult height is guarded
4
Familial short stature
: diagnosis made when child is growing at normal rate and one or both
parents are short all lab. Tests are normal
i.
HYPERPITUITARISM ( TALL STATURE )
Either primary or secondary
Table showed differential diagnosis of tall stature & overgrowth syndromes
FETAL OVERGROWTH :
Maternal DM
cerebral gigantisim (Sotos syndrome)
Beckwith Wiedemann
Postnatal overgrowth leading to childhood tall stature
i.
Nonendocrine causes
Familial (constitutional tall stature )
Exogenous obesity
5
Cerebral gigantism sotos syndrome
Marfan synd.
Bekwith wiedmann synd.
Klinfelter syndrome
Homocystinuria
ii.
Endocrine cause
Excess GH secretion
Precocious puberty
Hyperthyroidism
Mc Cune –Albright syndrome
Postnatal overgrowth leading to adult tall stature
Familial
Marfan
Klinfelter
Excess GH
XXY
ACTH or cortisol deficiency
THYROID GLAND DISORDER : L2
Etiological classification of congenital hypothyroidism:
Primary hypothyroidism :
Defect of fetal thyroid development (dysgenesis )
Defect in thyroid hormones synthesis
Defect in thyroid hormones transport
Resistance tom thyroid hormones
Maternal antibodies
Iodine deficiency
Maternal medication (iodides .amiodarone . methimazole ,radioiodide )
Central hypo pituitary hypothyroidism
TSH deficiency
Isolated TRH deficiency
Multiple congenital pituitary hormones deficiencies
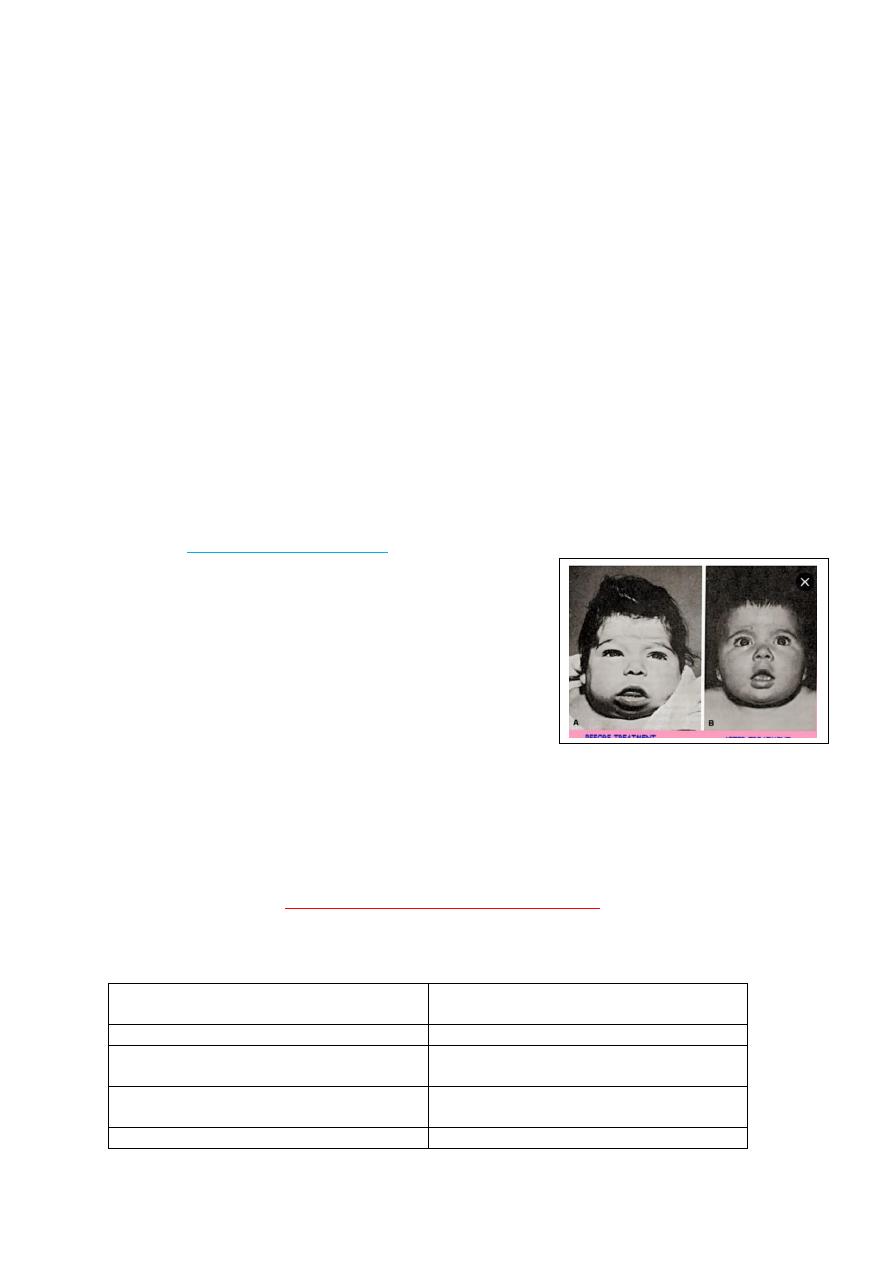
Clinical features of congenital hypothyroidism :
Most cases of congenital hypothyroidism are asymptomatic because partial trans placental
passage of maternal T4.
Normal weight & length at birth
Slight enlargement of head because
myxedema
Wide anterior &posterior fontanel
Prolonged physiological jaundice (early sign)
Feeding difficulties& choking &delayed
teeth eruption
Cry little &sleep much poor appetite
Constipation not respond to treatment with
umbilical hernia
Genital edema ,slow pulse ,cardiac murmur
with macrocytic anemia
Broad hands &short fingers
Dry scaly skin &little perspiration

6
Laboratory finding:
Heal prick between 2-5 days of age ( filter paper )
Serum level of T4 & free T4 usually low …..T3 may be normal & usually not helpful in diagnosis. ECG
show slow voltage ,echo may show pericardial effusion .
Radiological :
retarded osseous maturation at birth in 60 % of cases .
Distal femoral &proximal tibial epiphyses normally present at birth are often absent
Deformity( beaking )of the 12
th
thoracic or 1
st
or 2
nd
lumber vertebra is common , skull show wide
sutures ,enlarge and round sella turcica
Treatment :
Levothyroxine (L-T4)given orally at morning
Recommended initial starting dose is 10-20 µg/kg/day [ serum T4 &freeT4 ,TSH ]should be checked
every 1-2 mo.in 1
st
6 mo. Of life .then every 2-4 mo. From 6mo. -3 yrs. Of age .
Prognosis :
Early diagnosis and adequate treatment from 1
st
wk.of life result in normal linear growth
&development . variable degree of brain damage may contribute to [delay diagnosis, inadequate
treatment &poor compliance in first 2-3 years of life )
HYPERTHYROIDISM
:
Excessive secretion of thyroid hormones it is caused by Graves disease
Clinical features of hyperthyroidism :
Symptoms :
Hyperactivity .irritability ,altered mood, insomnia poor concentration
Heat intolerance
Fatigue ,weakness ,palpitation
Dyspnea weight loss ,thirst &polyuria with loose stool
Signs :
Sinus tachycardia
Fine tremor , hyperreflexia moist &worm skin
Palmer erythema ,
Hair loss or thinning
Chorea
Osteoporosis ,hypokalemic periodic paralysis
Psychosis
LAB. Finding :
High T3,T4 free T4 and low TSH and T3 usually elevated more than T4
Treatment :
Medical treatment is recommended rather than radioiodine or surgery
Propylthiouracil(PTU) &methimazole[Tapazole ]( potent 10 time than PTU)
Initial dose of Methimazole :0.25mg-1mg /kg /24hr once or twice daily
Developmental delay ,hoarse voice &they
don’t learn to talk
Physical &intellectual impairment increase
with age with delayed sexual maturation
7
Clinical response appear after 3-6 wks and adequate control evident in3-4 months
Beta blocker like propranolol in dose 0.5-2 mg/kg/day orally useful in toxic patients
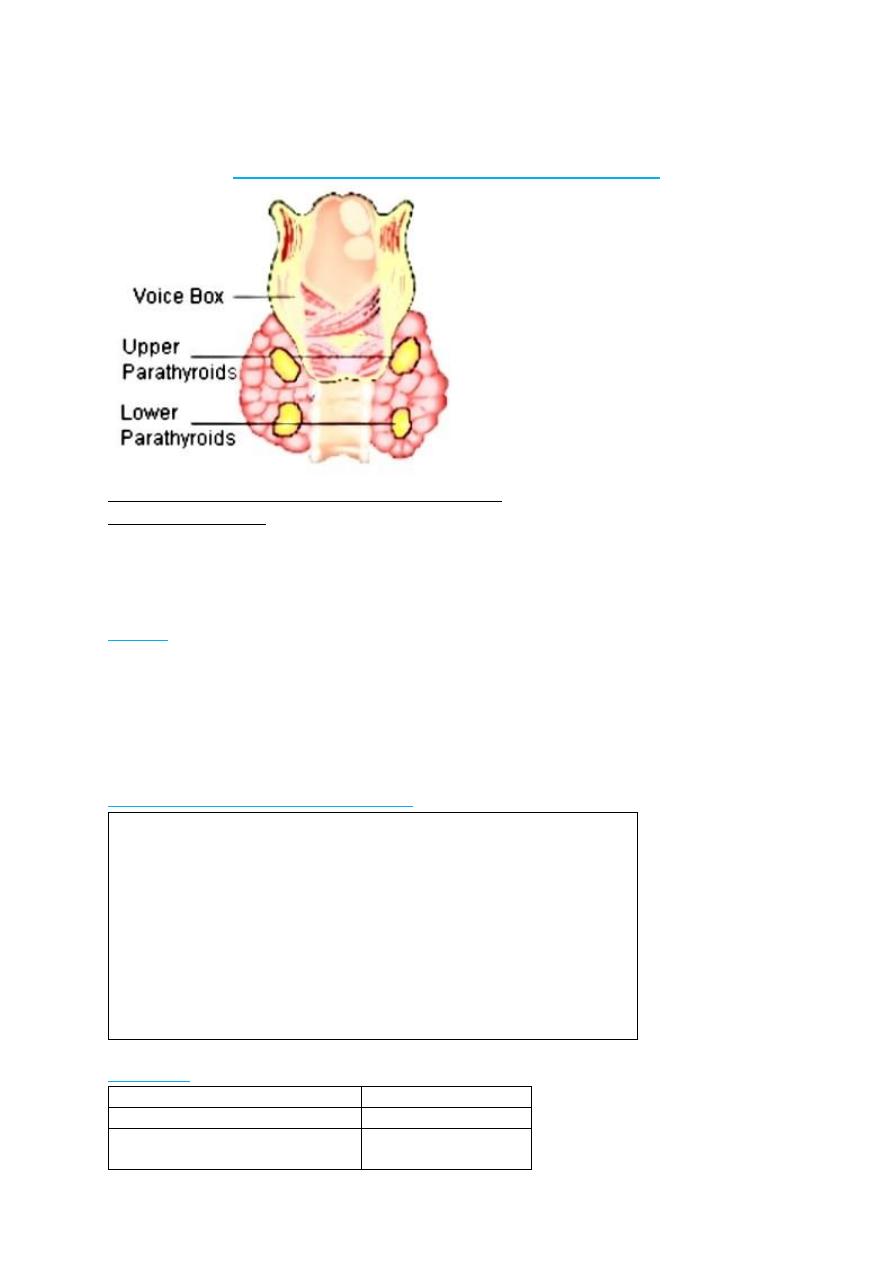
Disorder of parathyroid gland:
Parathyroid hormones : PTH also called parathemone secreted by parathyroid gland which is
important in bone remodeling .PTH secreted in response to low blood
serum calcium
level
.calcitonin : also called thyrocacitonin it is hormone produced primarily by Para follicular cell in
thyroid gland and act to reduce level of calcium and opposing the effect
of PTH
hormone .
HYPORARATHYROIDISM :
Etiology:
A: congenital
Transient neonatal
Familial isolated hypopara .(AR,AD.Xlinked )
Di George syndrome & sanjad –sakati syndrome (short stature, retardation .dysmorphism )
Barakat syndrome (sensorineural hearing loss with renal dysplasia )
B :acquired (autoimmune ,infiltrative ,maternal hyperparathyroidism ,hypomagnesemia)
Clinical features:
Vary from asymptomatic to sever form of hypocalcemia
Muscular pain &cramps are early signs
Numbness stiffness &tingling of hands and feet
Chevostek or trousseau sign or carpopedal spasm may be only signs
Convulsion with or without loss of consciousness (mistaken as
epilepsy )
Headache & vomiting because raised ICP
Delayed teeth eruption &dry scaly skin
Mucocutaneous candidiasis
Cataract .addison diseasepernicius anemia ,alopecia .
Lab. Finding
:
serum calcium is low
5-7mg/dl
phosphorus level is elevated
(7-12mg/dl)
Ionized Ca which reflect 45% of
the total
Low
8
Alkaline phosphatase
normal or low
D3 level
Low
Magnesium
Normal
PTH
Low
Treatment :
Emergency treatment of neonatal tetany consist of injection of 5-10 ml or 1-3 mg/kg of 10%solution
calcium gluconate (elemental 9.3 mg/ml )
D3 also should be given (initial dose .25µg/24 hr .with maintenance dose 0.01-0.1 µg/kg/24hr
Supplemental calcium in form of calcium gluconate provide 800 mg elemental calcium daily
PSUODOHYPOPARATHYROIDSM( PHP) :{Albright hereditary osteodystrophy )
Parathyroid hormone here are normal and serum level of PTH are elevated even when patient is
hypocalcemic(peripheral resistance to PTH rather than deficiency ) .we have type 1A (common )
&type 1B less common & type 2.(tissue specific resistant to PTH)
Hypocalcemia ,high PTH, hyperphosphotemia
Type 1A : account for majority of cases
Tetany is often presenting sign
Short stocky build &round face
Brachydactyly with dimpling dorsum of the hand
2
nd
metacarpal bone involve result in index finger longer than
middle
Short and wide phalanges .bowing ,exostoses &thickening of
calvaria
Moderate degree of cognitive impairment
Calcification of basal Anglia with lenticular cataract
Psudospodohypoparathyroidism(PPHP) :
Inherited disorder ,it is similar to pseudohypoparathyroidism (PHP) in presentation
serum level of calcium and phosphorus usually normal with PTH hormone slightly elevated & no
resistant to PTH
summary
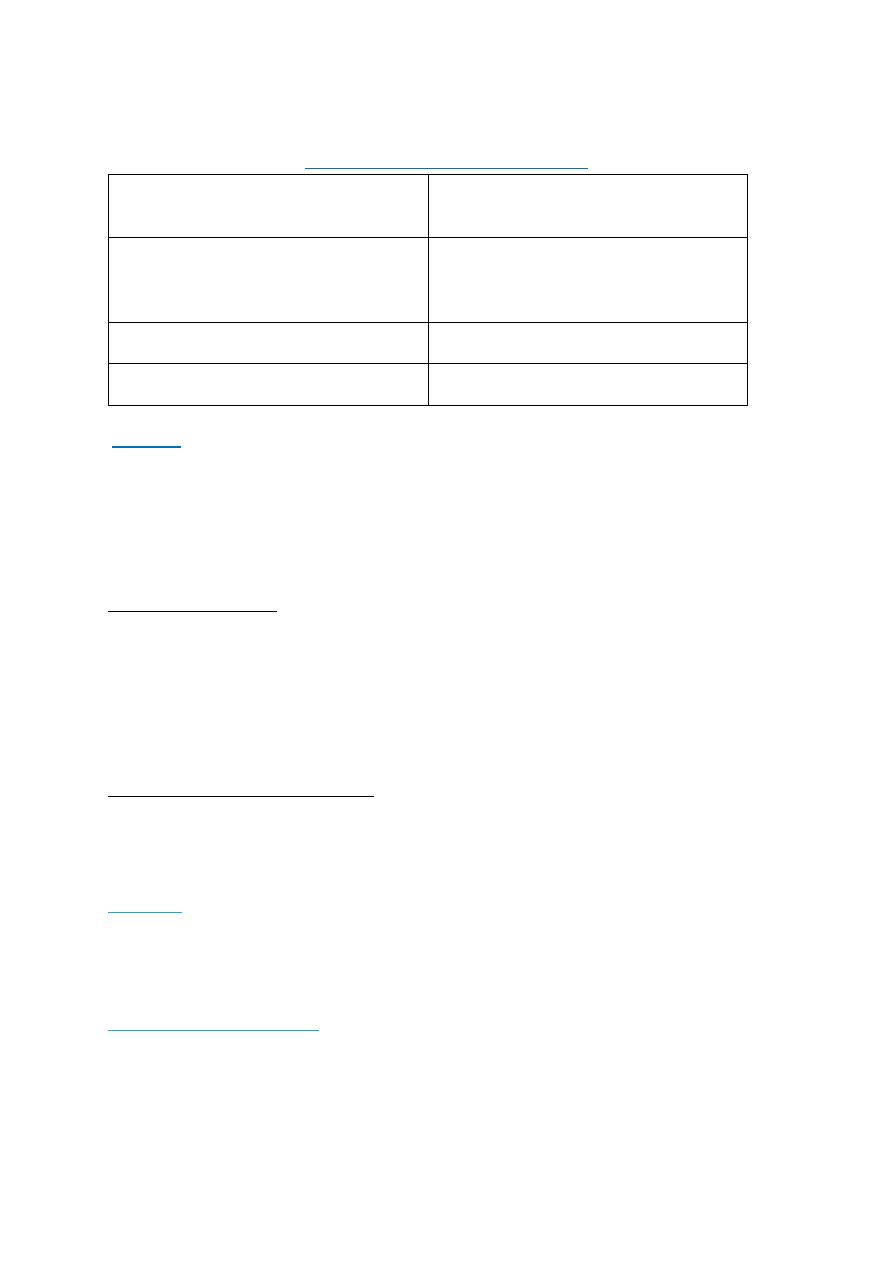
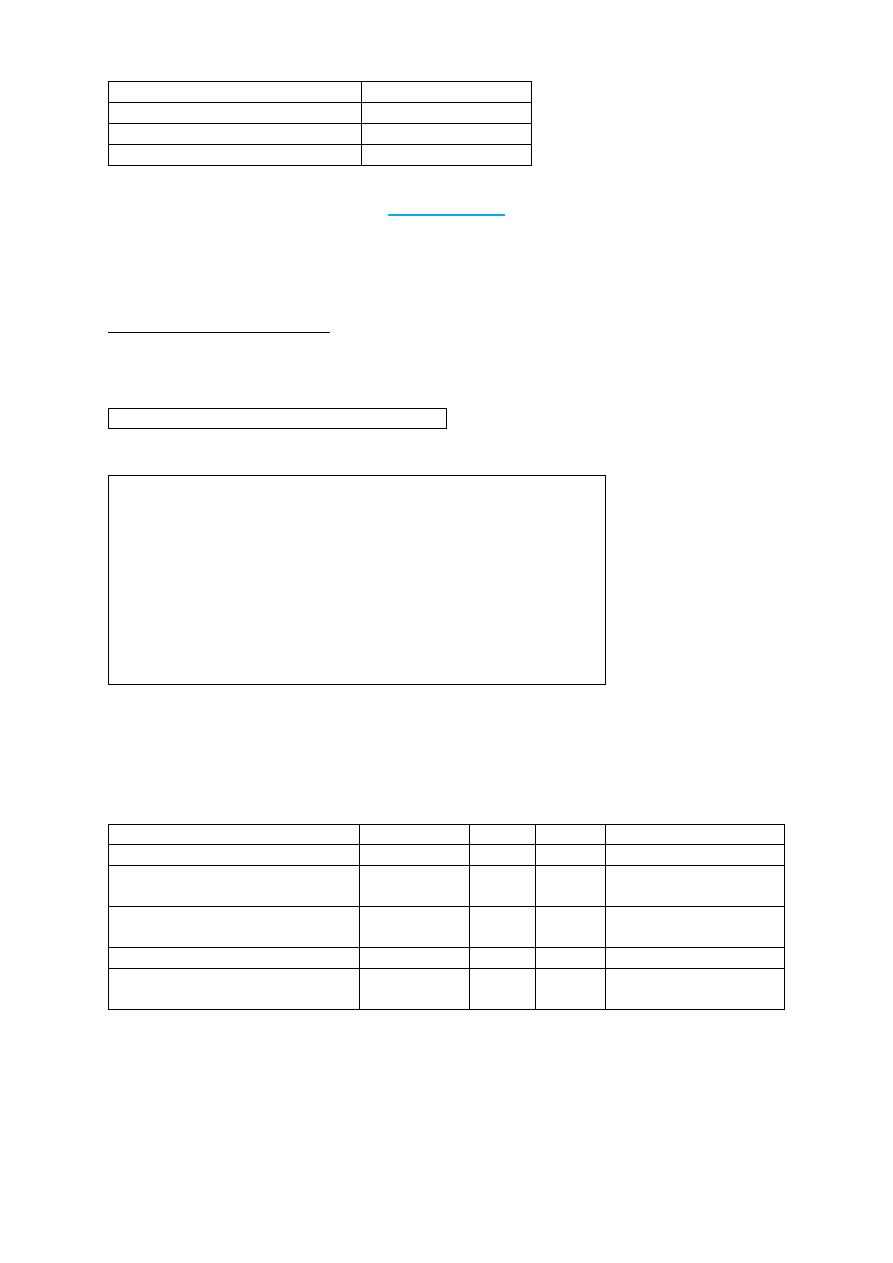
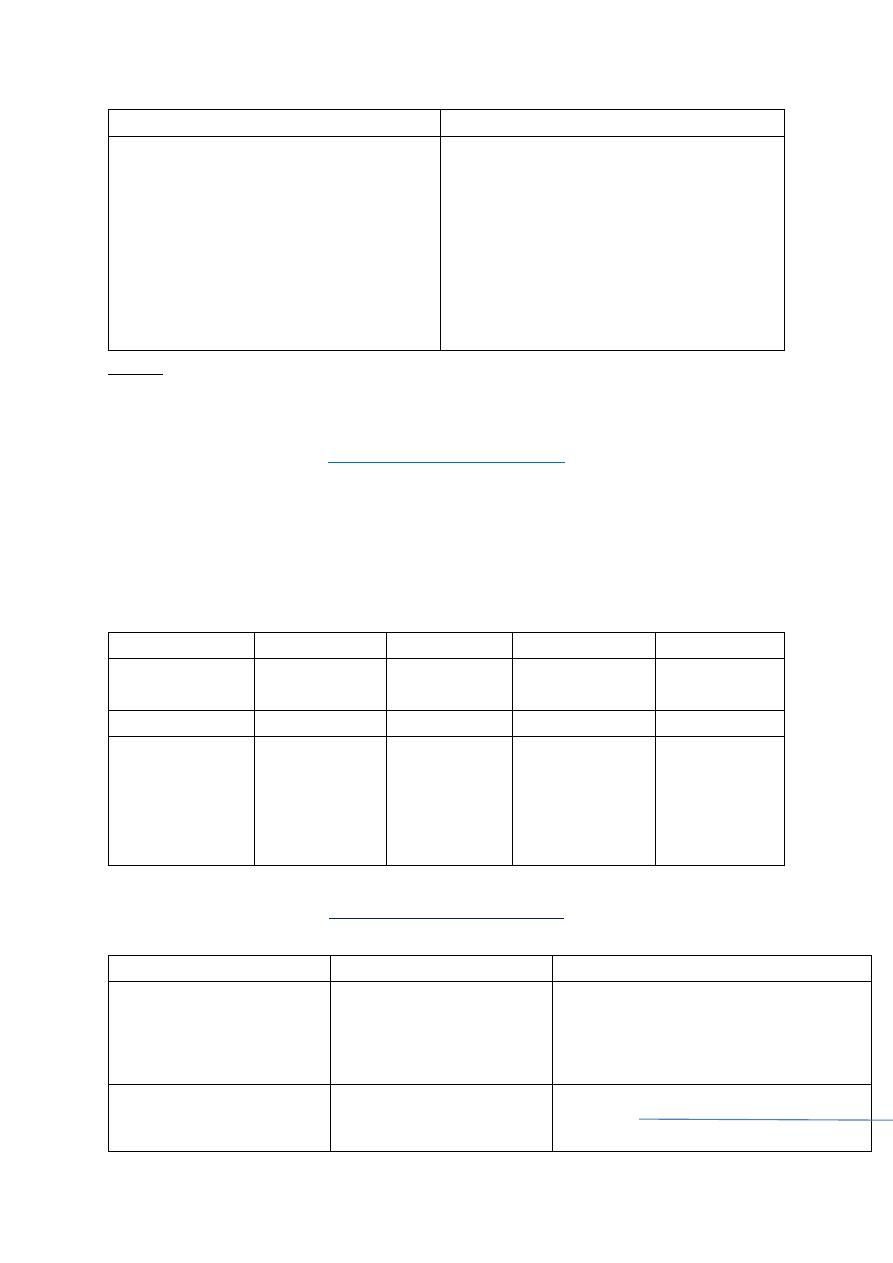
Condition
Appearance
PTH
Calcium Phosphates
Hypoparathyroidism
Normal
Low
Low
High
Pseudohypoparathyroidism type
1A
Skeletal
defect
High
Low
High
Pseudohypoparathyroidism type
1B
Normal
High
Low
High
Pseudohypoparathyroidism type 2 Normal
High
Low
High
Pseudopseudohypoparathyroidism Skeletal
defect
Normal Normal Normal
9
DISORDER OF ADRENAL LAND
,,,,,,,,,,,,,,,,,,,,,,
L3
Adrenal gland consist of cortex & medulla
1-Cortex {outer layer zona glomerularis(aldosterone secretion )
,middle layed :zona fasiculata (glucocorticoid &cortizole )
inner layer :zona reticularis (androgen secretion )
2- medulla (epinephrine &epinephrine )
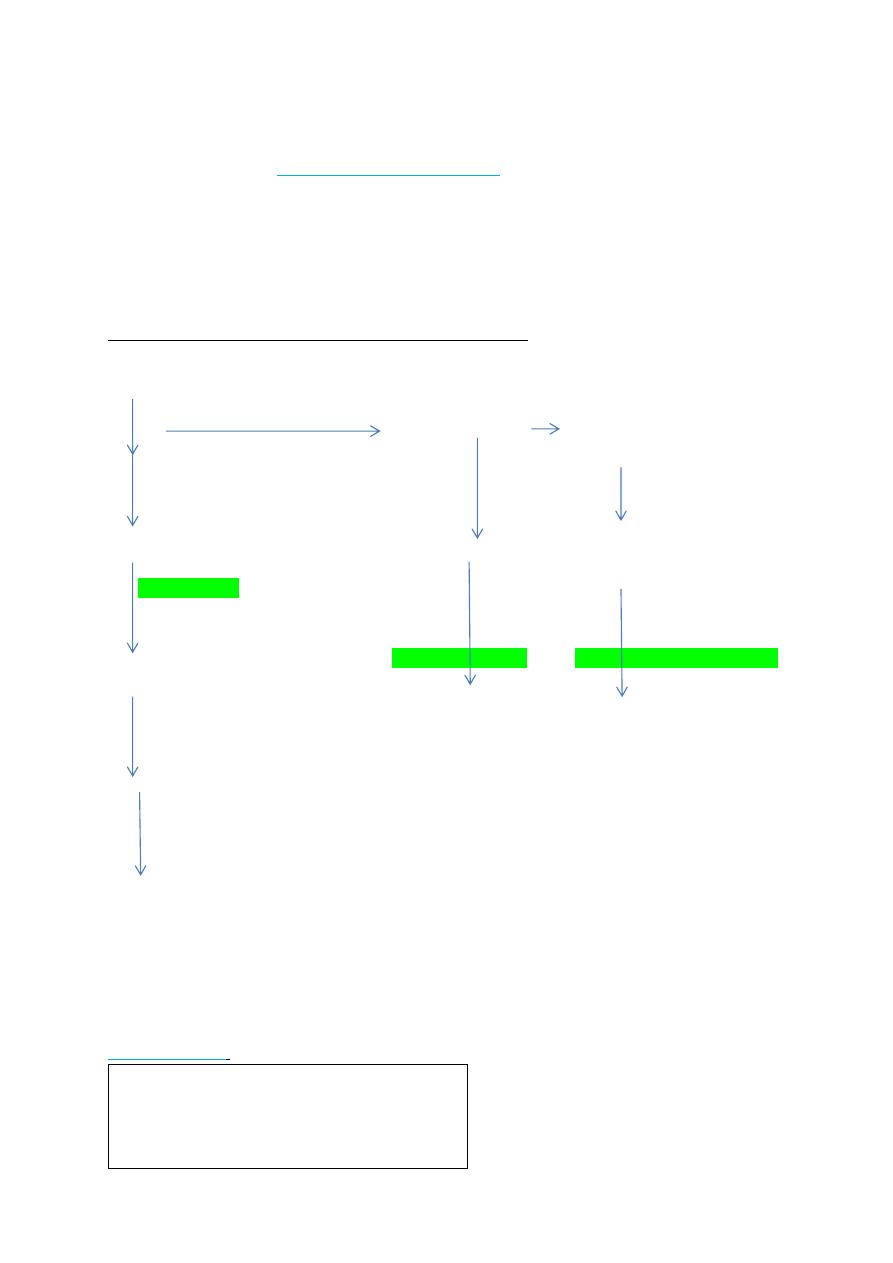
CONGENITAL ADRENAL HYPERPLASIA (adrenal insufficiency ):
Adrenal steroidogenesis
Cholesterol
Cholesterol desmolase
Pregninolone 17 OH pregninolone dehydroepiandrosterone
3 beta hydroxylsteroid dehydrogenasae DHEA
Progesterone
deoxycortisole Androsterone
21 hydroxylase
11 beta hydroxylase 17 OH steroid deh ydrogenase
Deoxycorticosterone
Cortisole testesterone
Corticosterone
18 oxydase
Aldosterone
A several of autosomal recessive disorder result from mutation of gene for enzymes mediating
biochemical steps of production of mineralocorticoids ,glucocorticoids & sex hormones from
cholesterol by adrenal gland
Most common types : 21 hydroxylase deficiency ,11β hydroxylase def..3βhydroxysteroid
dehydrogenase def.
Symptoms:
depend on the form of CAH and sex of patient
Mineralocorticoid deficiency :
Vomiting due to salt loss(dehydration
&death
Excess androgen :
Average size penis
10
Ambiguous genitalia in females
Early pubic hair & rapid growth in
childhood
Precocious puberty
Excessive facial hair virilization
Infertility due to anovulation
Clitoromegaly
Undervirilization in XY male which can
result in apparently female external
genitals
Investigation : treatment
Hypoglycemia ,hyperkalemia.
hyponatremia (due to
hypoaldosteronism )
Low cortisole level
High ACTH
High 17 α hydroxyprogesterone in
blood
High 17 ketosteroid in urine
Most definite (measure serum cortisol
pre & after ACTH administration
Immediate & vigorous fluid
&electrolytes replacement
supply enough glucocorticoid to
reduce hyperplasia &
overproduction of androgen or
mineralocorticoid
Replace enough mineralocorticoid
Provide testesterone or estrogen
at puberty if deficient
Optimize growth &bone
maturation
Hydrocortisone
Na succinate
10-15
m \m²\24hr TID
fludrocortisone
(synthetic
mineralocorticoid
) orally in dose
0.05-0.2
mg/day
Addison dsiaese :
(acquired adrenal insufficiency ):
Occur as a part of autoimmune polyendocrinopathy syndrome type-2(APS-2): which consist of
Addison dis.autoimmune thyroiditis , or type 1 DM .
Type 1 polyendocrinopathy : consist of : mucocutaneous candidiasis & various autoimmune
endocrinopathies like hypoparathyroidism ,Adrenal insufficiency .
Clinical features:
Symptoms :
fatigue ,anorexia ,weight
loss,myalgia &joint pain
nausea ,vomiting
Glucocorticoid deficiency
Both glucocorticoid
&mineralocorticoid
Signs :
Low blood pressure
Skin or mucosal hyperpigmentation
Both mineralo&glucocorticoid lack
Excess of proopiomelanocortin –
derived peptide
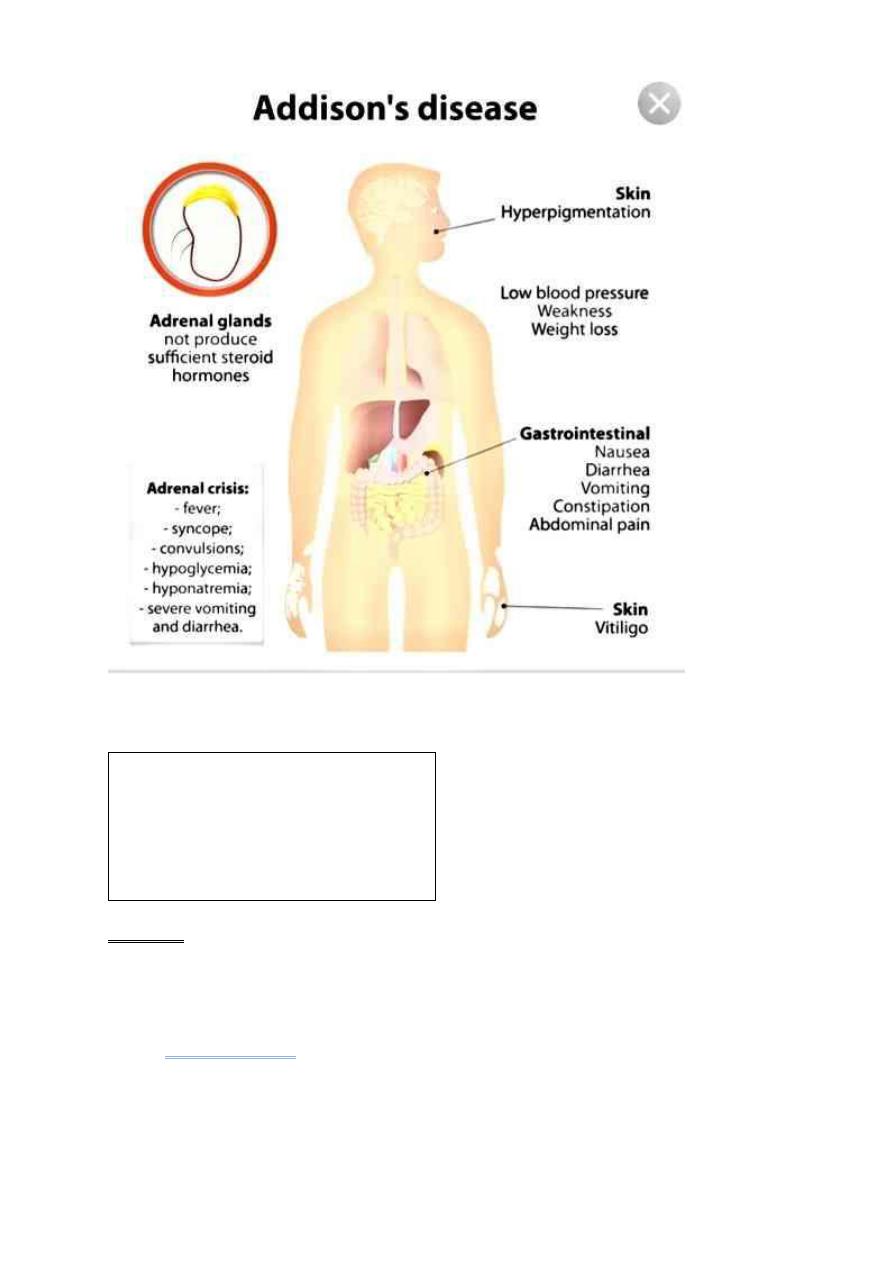
11
Lab .finding :
Hyponatremia
Hypoglycemia &ketosis
Hyperkalemia
Low cortisol level
Eosinophilia &lymphocytosis
High ACTH level
High plasma renin activity
Treatment :
Correction of electrolyte abnormality with hypoglycemia
Steroid replacement. Hydrocortisone orally in daily dividing dose of 10-15 m/m²/day
Cushing syndrome:
excess of cortisol or other glucocorticoid due to either adrenal tumors or central pituitary
involvement and or exogenous steroid usage (details in internal medicine lectures ).

12
L4
Physiology of puberty
Between early childhood and 8-9 yr of age (prepubertal stage )the
hypothalamic –pituitary –gonadal axis is dormant as reflected by undetected
level of LH & sex hormones testosterone in boys and Estradiol in girls .1-3 yr
before onset of puberty low serum level of LH demonstrate during sleep in
pulsatile fashion . the pulsatile secretion of gonadotropins is responsible for
enlargement and maturation of the gonads and the secretion of the sex
hormones . in mid puberty the level of LH become evident even during day
time and occur at about 90-120 minutes intervals
It is clear that GnRH is the primary if not the only , hormone responsible for
the onset and progression of puberty
The effect of gonadal steroid (testosterone and estradiol )on bone growth and
osseous maturation are critical , both aromatase deficiency and estrogen
receptor defect result in delayed epiphyseal closure and tall stature in affected
boys, that is mean
estrogen
rather than androgen are responsible for process
of bone maturation and epiphyseal fusion and cessation of growth
Estrogen also mediate the increased production of growth hormone which
also responsible with sex hormone for pubertal growth spurt.
The onset of puberty vary and more correlated with osseous than with
chronological maturation age
In female, breast bud(thelarche ) is first sign of puberty (10-11yrs) followed
by pubic hair (6-12 months later ), the interval to menarche usually 2-2.5 yrs.
peak height velocity usually start early 12 yr of age in girls &always precedes
menarche (12.75yr)
In male growth of testes(>2.5 cm) and thinning of scrotum is the first sign of
puberty followed by pigmentation of scrotum and enlargement of penis .pubic
hair then appeared . axillary hair appear in mid puberty in male unlike female
growth acceleration appears after puberty . in male growth spurt usually 2
yrs later than in females .and growth may continue beyond 18 yrs .of age
Precocious puberty :
Definition :
onset of breast development before age of 8 yrs. In girls & onset of
testicular development before age of 9 years in boys .
13
Etiology :
Central (gonadotropin dependent true precocity )
Idiopathic
Brain lesions
Hypothalamic hamertoma
Brain tumors
Prolonged untreated hypothyroidism
Combined peripheral ¢ral
Treated CAH congenital adrenal hyperplasia
Familial male precocity
Peripheral (gonadotropin independent precocious
puberty)
Girls
o Isosexual (feminizing )
o Ovarian tumors
o Teratoma
o Exogenous androgens
o Mc Cune –Albright syndrome
o Heterosexual (masculinizing)
o CAH
o Exogenous androgen
o Adrenal &ovarian tumors
Boys
o Isosexual ( Masculinizing)
o CAH
o Leydig cell tumor
o hCG secreting tumors
o teratoma
o exogenous androgen
o heterosexual (feminizing )
o exogenous androgen
Clinical features :
hair underarm &genitalia
&
for boys on face
acne
adult body odor
sexual development ( breast & testes )
emotional changes
mood swings
14
Diagnosis:
o Hormonal levels(sex hormones
Low
estradiol level or undetected in girls
High testosterone (detectable in boys
Detectable level of LH in girls & boys
o bone age (advance) osseous maturation
o ultrasound for adrenal &uterus size
MRI or CT scan role out tumors
Treatment :
GnRH .analogs are effective in arresting pubertal progression in patient with
central precocity like decapeptyle (zoladex ) monthly IM injection .
Meroxyproesterone acetate some time used to :suppress puberty and arrest
menses
Peripheral precocity :
Testolactone which inhibit conversion of testosterone to estrogen
Ketoconazole inhibit steroid biosynthesis 200mg tds
Cyproterone acetate Potent progestin & antiandrogen, inhibit
androgens at the receptor level / supress gonadal & adrenal
steroidogenesis : antigonadotrophic 100 mg/m2 2 divided doses
Diabetes mellitus in children (type 1 DM ):
L5
Definition :Common chronic metabolic disease characterized by
hyperglycemia as a cardinal biochemical features .
Etiologic classification of Diabetes :
1-Type 1 DM (beta cell destruction )
Immune mediate
Idiopathic
2-type 2DM (insulin resistance &deficiency )
Typical
Atypical )
3-enetic defect of beta cell
Mody (maturity onset diabetes of young )
Wolfram syndrome (DDMOD diabetes mellitus
,diabetes insipidusoptic atrophy &deafness)
Mitochondrial DNA mutation
15
Thiamine responsiveness megaloplastic anemia
with diabetes
4-drug or chemical induced
L-asparginase
Anti rejection .cyclosporine …..
Phenytoin
Diazoxide
Beta blockers
α interferone
5- disease of exocrine pancreas
Cystic fibrosis
Trauma to pancreas
Pancreatitis
6-infection (CMV ,Rubella .HUS)
7-genetic syndromes
Prader willi syndrome
Downs syndrome
Turner syndrome
Klinefelter syndrome
8-Gestational diabetes
9-Neonatal diabetes
Transient
Permanent
Type 1 diabetes mellitus :
Insulin dependent or juvenile diabetes characterized by low or absent level of
endogenously produced insulin & by dependence on exogenous insulin ;
insulin act on movement of glucose into cells to subdue hepatic glucose
production & halt movement of fatty acid from periphery to liver
the natural history include 4 stages :
1. Preclinical Beta cell autoimmunity with progressive defect of insulin
production
2. Clinical diabetes
3. Transient remission ,homeymoon period
4. Established diabetes
Its account about 10 % of cases of diabetes affecting >10 million people in
the world ,over all incidence of type 1 DM varies from 0.7/100 000 /year
[2hin Pakistan to 40/100 000/year In Finland. Girls and boys are equally
effected ,no apparent correlation with socioeconomic status .
16
Age incidence ,2 peak group 5-7 yrs and time of puberty .there familial
clustering inT1DM with prevalence in sibling approaching 6% but in general
population is 0.4%in US .
HLA system mostly associated with DR3/4-DQ2/8
Natural history of diabetes involve some or all of the following stages :
1. Initiation of autoimmunity
2. Preclinical of autoimmunity with progressive loss of beta cell function
3. Onset of clinical disease
4. Transient remission
5. Established disease
6. Development of complications
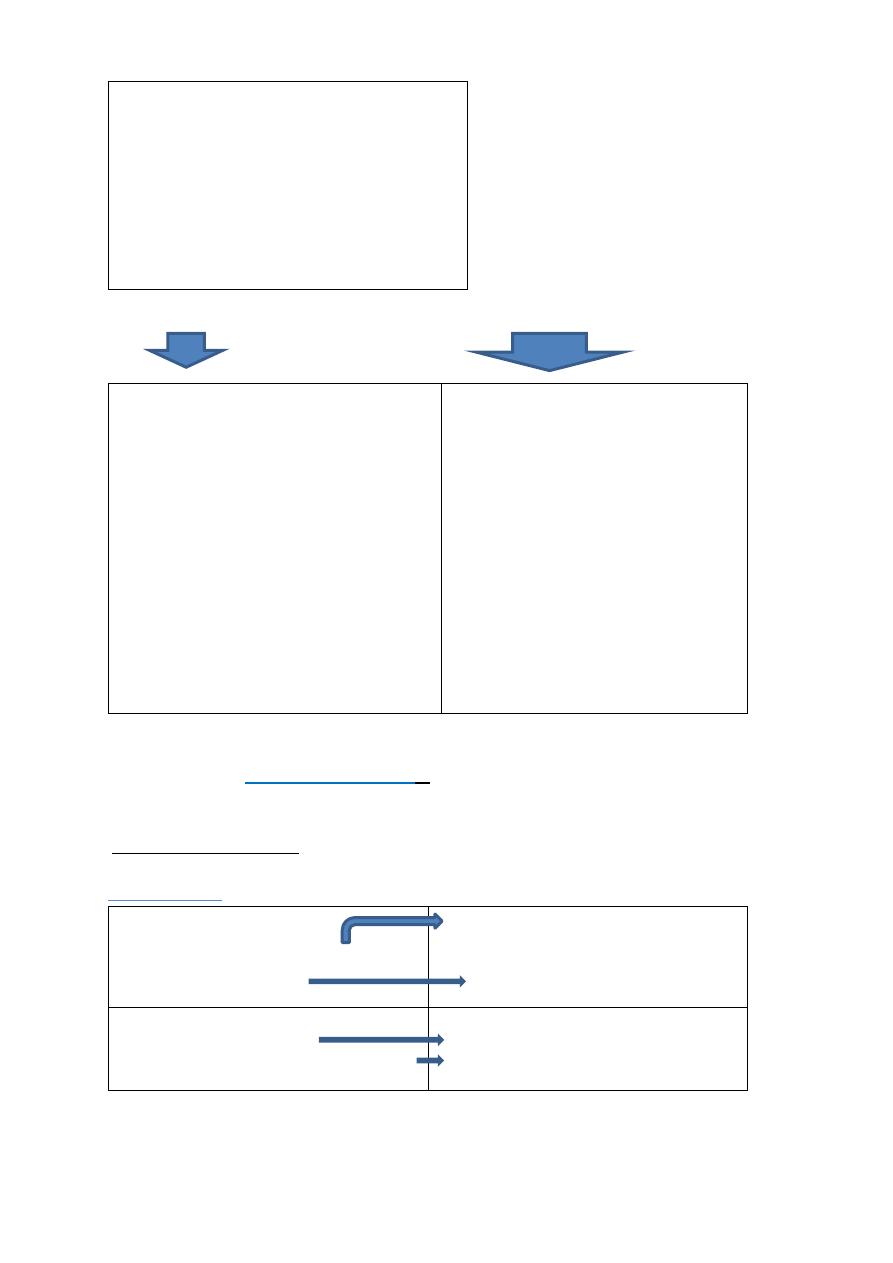
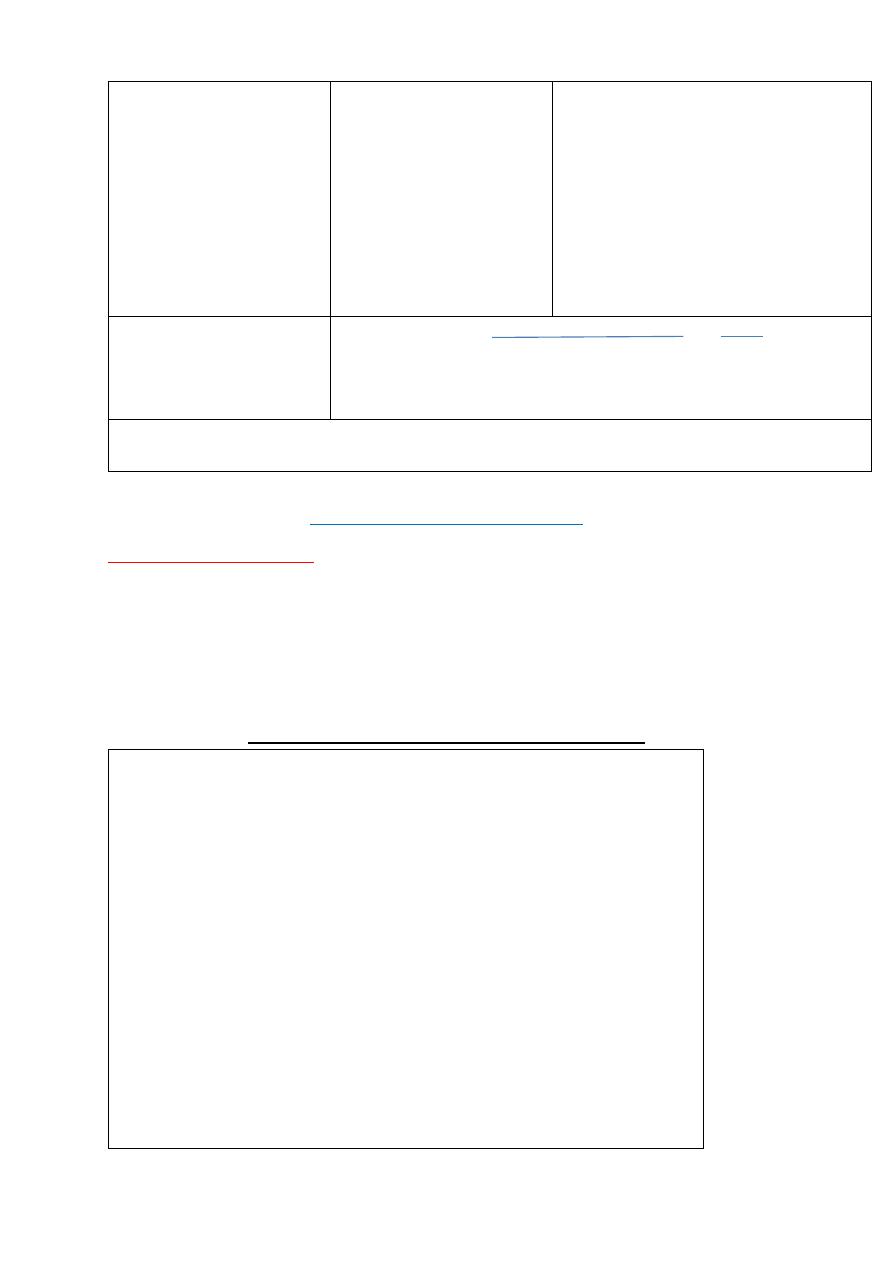
Influence of high insulin vs low insulin on some metabolic processes in liver, muscle &adipose tissues :
High plasma
insulin(postprandial state )
Low plasma insulin (fast
state )
Liver
Glucose uptake
Glycogen synthesis
.lipogenesis
Absence of ketognesis
Glucose production
Glycogenolysis
Gluconeogenesis
Muscles
Glucose uptake
Glucose oxidation
Glycogen synthesis
Protein synthesis
Absence of glucose
uptake
Fatty acid &ketone
oxidation
Glycogenlysis
Proteolysis
Adipose tissues
Glucose uptake
Lipid synthesis
Absence of glucose
uptake
Lipolysis & fatty acid
release
Diagnosis :
Impaired glucose tolerance
Diabetes mellitus
Fasting glucose 100-125mg/dl
Or
2hrs plasma glucose during OGTT more
or equal 140mg/dl but <200mg/dl
Symptoms of diabetes +random
plasma glucose more or equal to
200mg/dl
Or
Fasting (at least 8 hr )plasma
glucose more or equal to 126mg/dl
17
or
2hrs plasma glucose during OGTT
more or equal to 200mg/dl
Or HA1c >or equal to 6.5%
DM should suspected in any child with polyuria & dehydration ,poor weight
gain ,hyperglycemia ,glucosuria & ketonuria
Random serum sugar >200mg/dl with typical symptoms with or without
ketonuria is diagnostic .
Initial management of type1 DM
Most newly cases of DM are alert and able to eat and drink and can manage
with subcutaneous insulin alone . iv fluid required if the child vomiting or
dehydrated . intensive educational programme is needed for the parents and
child to cover
Basic understanding of pathophysiology ofDM
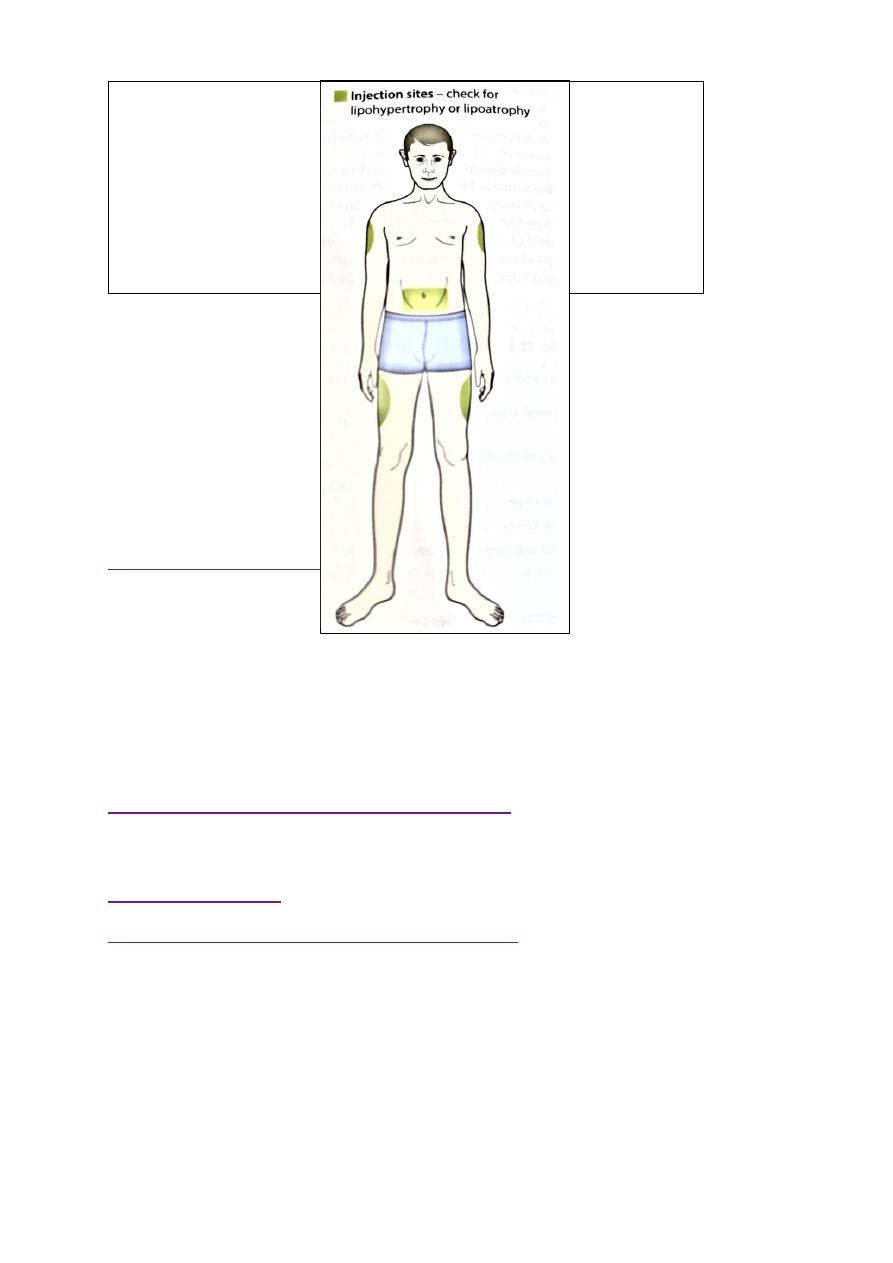
Insulin injection technique &sites
Diet , regular meal & snacks ,reduced refined CHO .healthy diet no >than
30% fat intake
match food intake with insulin &exercise
blood glucose monitoring
recognition and treatment of hypoglycemia
the psychological impact of lifelong condition with serious short & long
term complications
INSULIN THERAPY
Most insulin used in Iraq for children is humen with concentration
100U/ml with different types includes
human insulin analogues . rapid acting like lispro &aspart within few
minutes
short acting soluble insulin onset 30-60 min. peak 2-4 hrs. duration up
to 8 hrs. given 15-30 min.before meal
intermediate acting insulin onset 1-2 hrs . peak 4-12 hrs( insulin with
protamine )
mixed short & intermediate 30/70 mixtard
very long acting insulin analogues e.g glargine (lantus)
teenager preferable to use bolus & basal (basal .lantus at night and short
acting before each meal )
18
factors affecting blood glucose :
Increase blood glucose
Decrease blood glucose
omission of insulin
refined food
illness
menstruation
growth hormone
corticosteroids
sex hormones at puberty
stress of an operation
insulin
exercise
anxiety (marked )
some drugs
DIET : healthy diet recommended with high complex CHO &relatively low fat
content ,diet should be high in fiber
Diabetic ketoacidosis DKA :
End result of metabolic abnormalities result from sever deficiency of insulin or
insulin ineffectiveness. It is occur in 20-40 % of children with newly diagnosed
diabetes & DKA consider when serum sugar >300 mg .acidosis .+S/S of DM
with ketosis .
classification of DKA
Normal
Mild
Moderate
Sever
Co2)meq/l
venus
20-30
16-20
10-15
<10
pH venous
7.35-7.45
7.25-7.35
7.15-7.25
<7.15
Clinical
No changes
Only fatigue Kussmaul
,oriented but
sleepy
Kussmaul or
depress
respiration
,sleepy to
coma
Treatment protocol of DKA
Time
Therapy
Comment
1
st
hr.
10-20ml/kg IV bolus
0.9%NaClor LR
Insulin drip at 0.05-
0.1unit/lg/hr
Volume expansion ,NPO monitor
I/O,use flow sheet prepare manitol
1g/kg at bed side if cerebral edema
developed
2
nd
hr. until DKA
resolution
0.45% Nacl plus
continue insulin drip
85ml/kg +maintenance -bolus
IV rate =
23 hr
19
20meq/l KPhos &20
meq/l K Ac….5%glucose
if blood >250mg/dl
If K <3meq give 0.5-1 meq as oral
solution or increase iv K to
80meq/l
Maintenance =100ml/kg for 1
st
10
kg+50ml/kg for 2
nd
10 kg +25 ml/kg for
remaining kg
Initial bolus fluid consider part of total
fluid allowed & subtracted before
calculating iv rate
Sample calculating for
30 kg child
1
st
hr 300 ml iv bolus
0.9% NaCl or LR
2
nd
& subsequent hrs= (85ml × 30)+1750ml -300ml = 175 ml
23 hr hr
I/O input output, NPO nothing by mouth ,KAc potasium acetate ,kphos=potasium
phosphate ….LR lactated Ringer..NaCl sodium chlodide
Long term management of DM
Aim of long term management :
1. normal growth & development
2. normal home & school life as possible
3. good diabetic control through knowledge & technique
4. encourage children to be self- reliant
5. avoidance of hypoglycemia
assessment of child with diabetes (summary )
Assessment of diabetic control :
any episode of hypoglycemia
school absence
interference with normal life
HbA1C result
Insulin regimen ---appropriate
Diet –healthy diet
General overview :
Normal growth and pubertal development , ovoid obesity
Blood pressure checking
Renal for microalbuminuria
Eye ---cataract
Feet –care
Screening for celiac and thyroid disease
Knowledge &psychological aspects
20
Breakfast
a bowl of cereal with semi-skimmed milk
wholegrain toast with spread and/or jam
yogurt and fruit
a cereal bar and a glass of milk.
Find out more healthy breakfast swaps
Lunch
a chicken or ham salad sandwich...
a small pasta salad...
soup and a roll...
...with a piece of fruit and a yogurt.
Read more about healthy lunchtime swaps
Dinner
roast chicken with potatoes and vegetables
beef stir fry, vegetables and rice
chicken tortillas and salad
salmon and noodles
curry and rice
What sort of snacks do I need to eat?
Good understanding of diabetes
Becoming self-reliant but appropriate supervision at home
Taking exercise ,sport?
Smoking ???
Is hypo treatment readily available ?

21
Sometimes, you might need to eat a small snack between meals, to
help keep blood glucose levels up. Regular snacks can make it difficult
to maintain a healthy weight so check with the diabetes team for
specific advice that is tailored for your diabetes management.
The healthiest snack choice is definitely a piece of fruit, but rice cakes,
crackers, a couple of biscuits, a small bag of crisps, a cereal bar, or a
yogurt are good snack choices too.

22
23
