Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
1
Urinary System Imaging
Aims of our lecture:
To know the different radiological techniques used in urinary tract
To know different renal pathologies.
Urinary bladder diseases
Prostate and urethra disease
Scrotal and testicular disorders
Female genital organs imaging
I) Radiological techniques used in urinary tract imaging:
Ultrasonography
Urography
CT scan
MRI
Radionuclide scanning
Special techniques:
o
Retrograde and antegrade pyelography
o
Voiding cystourethrogram (micturating cystogram) and videourodynamics
o
Urethrography
o
Renal arteriography.
Ultrasonography:
Investigate patients with symptoms thought to arise from the urinary tract.
Demonstrate the size of the kidneys and exclude hydronephrosis in patients with
renal failure.
Diagnose hydronephrosis, renal tumours, abscesses and cysts including polycystic
disease.
Assess and follow-up renal size and scarring in children with urinary tract
infections.
Assess the bladder and prostate.
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
2
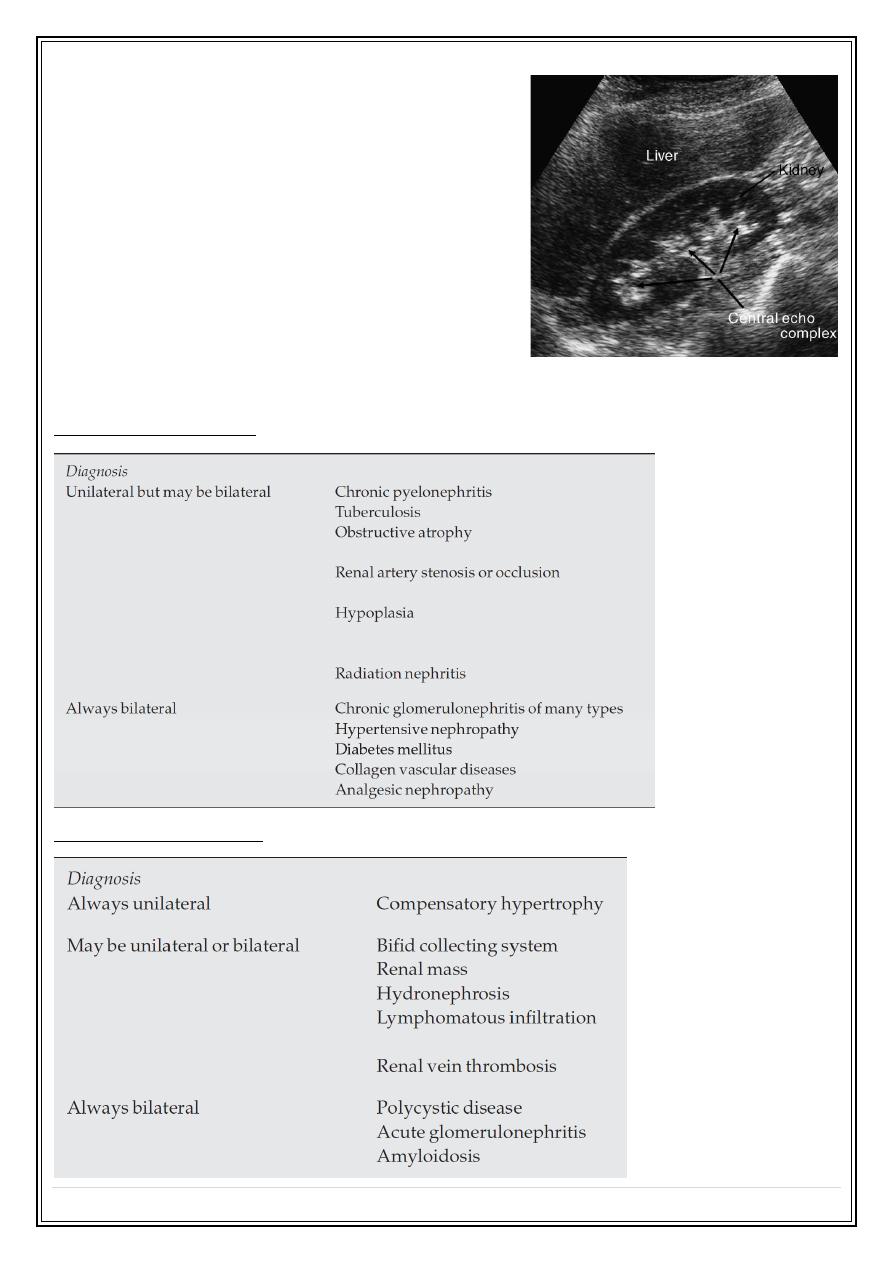
The normal adult renal length, measured by
ultrasound, is 9–12 cm.
Renal length varies with age, being maximal
in the young adult.
There may be a difference between the two
kidneys, normally less than 1.5 cm.
A kidney with a bifid collecting system is
usually 1–2 cm larger than a kidney with a
single pelvicaliceal system.
Causes of small kidney
Causes of large kidneys
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
3
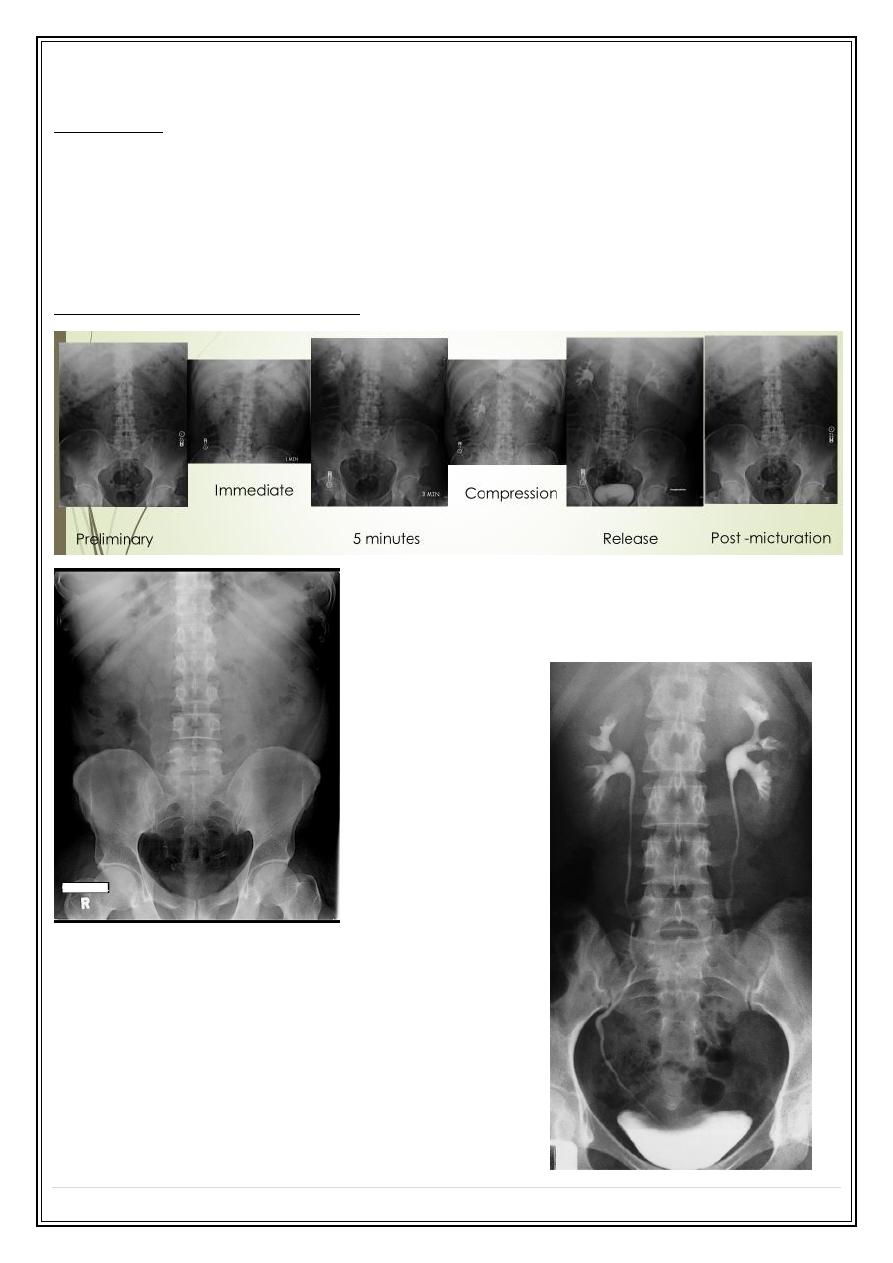
Urography:
Indications:
When detailed demonstration of the pelvicaliceal system and ureters are required
Suspected ureteric injury, e.g. following pelvic surgery or trauma
Assessment of acute ureteric colic
Intravenous (Excretory) Urography
1. Check the Kidneys: outline, size,
site
2. Check the calyces: cupped
3. Check renal pelvis and ureter
4. Check the bladder
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
4
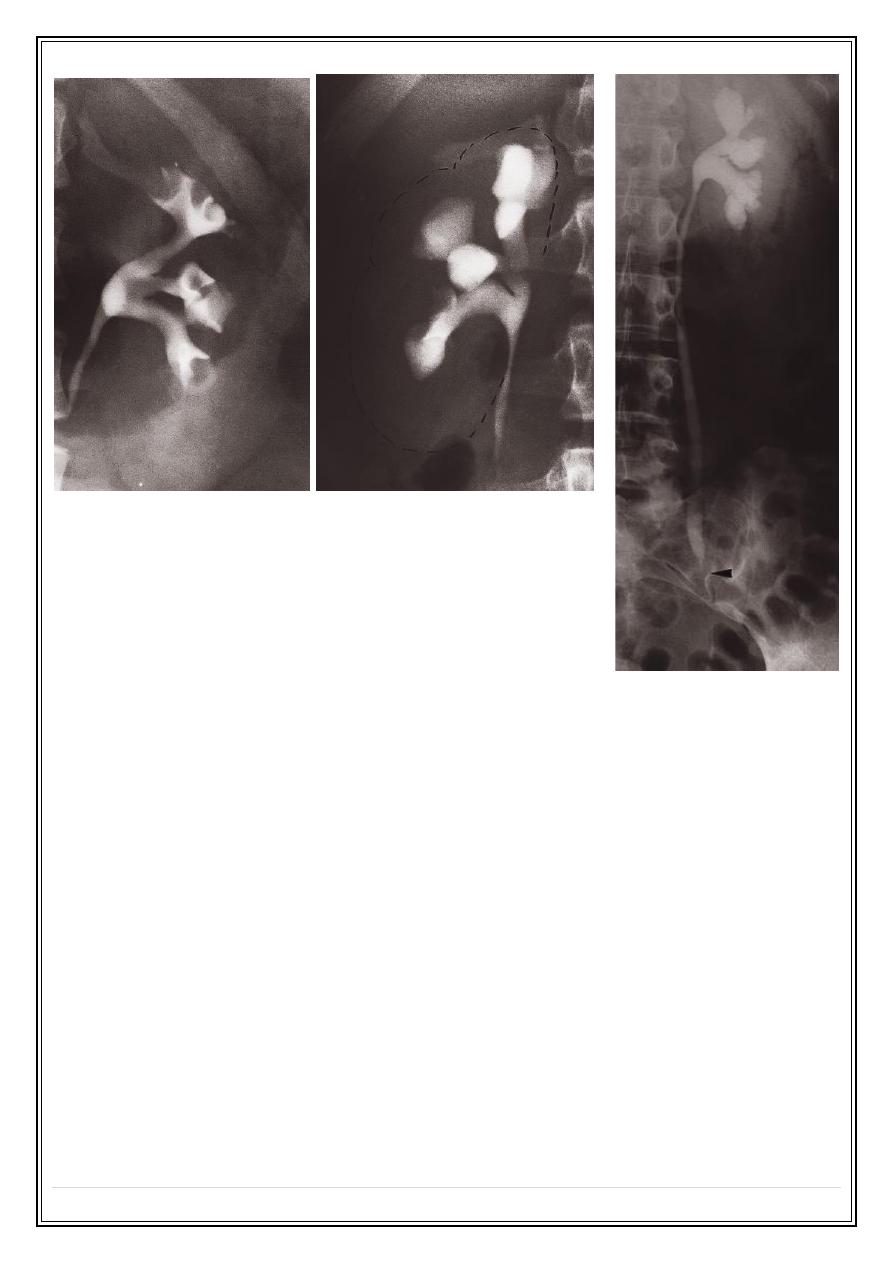
Causes of calyceal dilatation:
A: Due to obstruction
1. Within the lumen:
I. calculus
II. blood clot
III. sloughed papilla
2. Within the wall of the collecting system
I. intrinsic pelviureteric junction obstruction
II. transitional cell tumour
III. infective stricture (e.g. tuberculosis or schistosomiasis)
3. Extrinsic compression
I. retroperitoneal fibrosis
II. pelvic tumour, e.g. cervical, ovarian or rectal carcinoma
III. aberrant renal artery or retrocaval ureter
B) Due to papillary atrophy or destruction:
1. Reflux nephropathy
2. Papillary necrosis
3. Tuberculosis
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
5
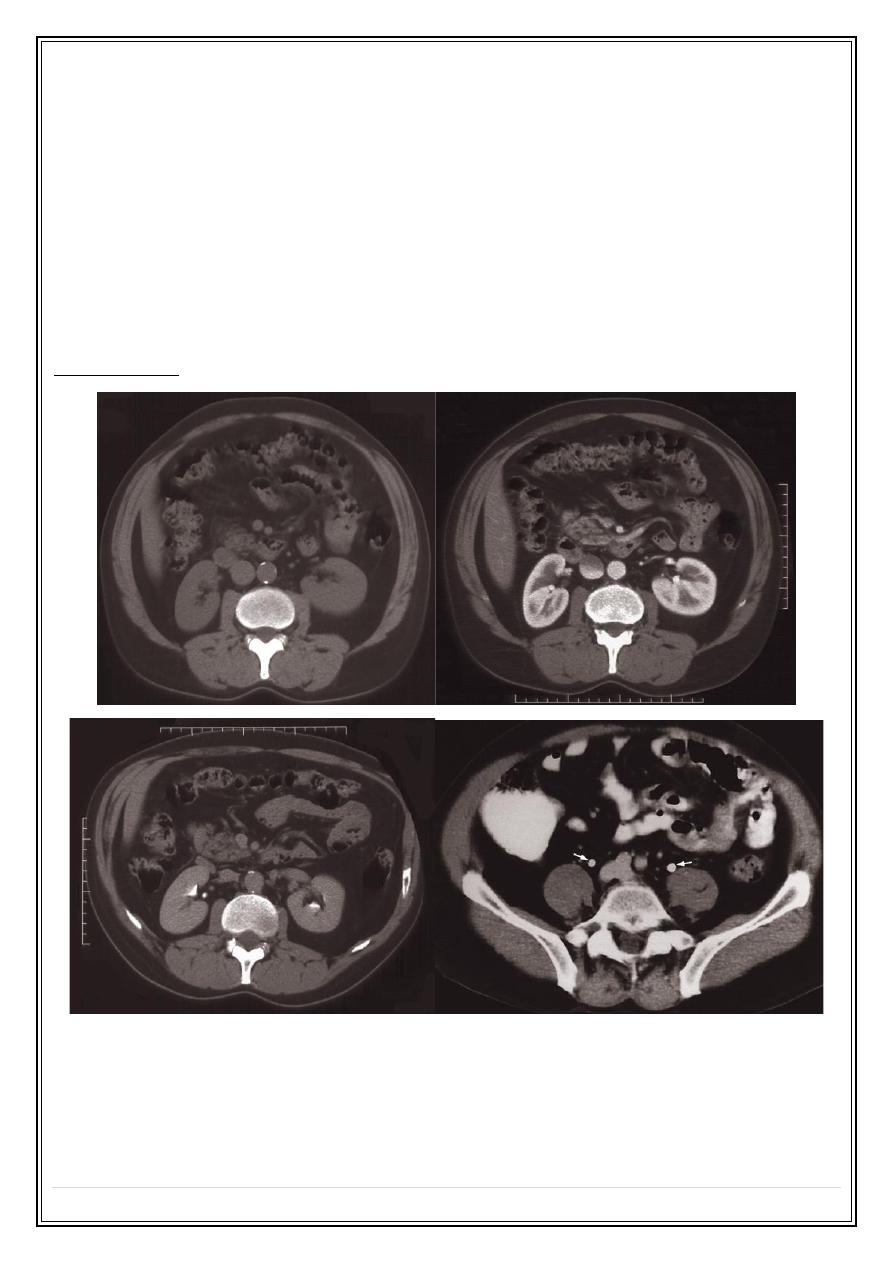
Indication of CT urography
Investigation of renal calculi
Investigation of haematuria
Characterization of a renal mass
Staging and follow-up of renal carcinoma
To delineate renal vascular anatomy (e.g. suspected renal artery stenosis or prior
to live related kidney donation)
To diagnose or exclude renal trauma
CT urography:
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
6
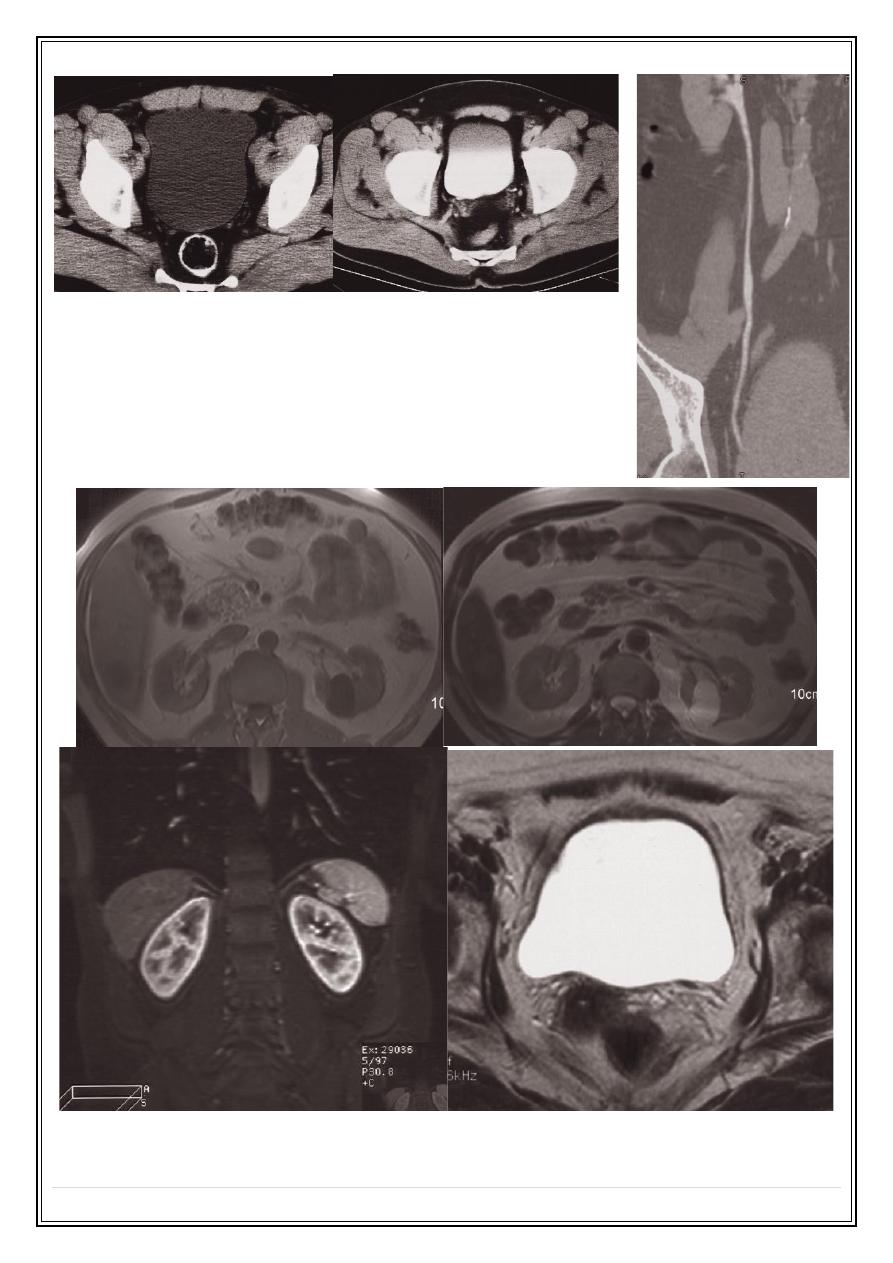
MRI
Fifth Stage
Diagnostic Imaging
Dr. Firas A. – Lecture 8
P a g e
7
MRA
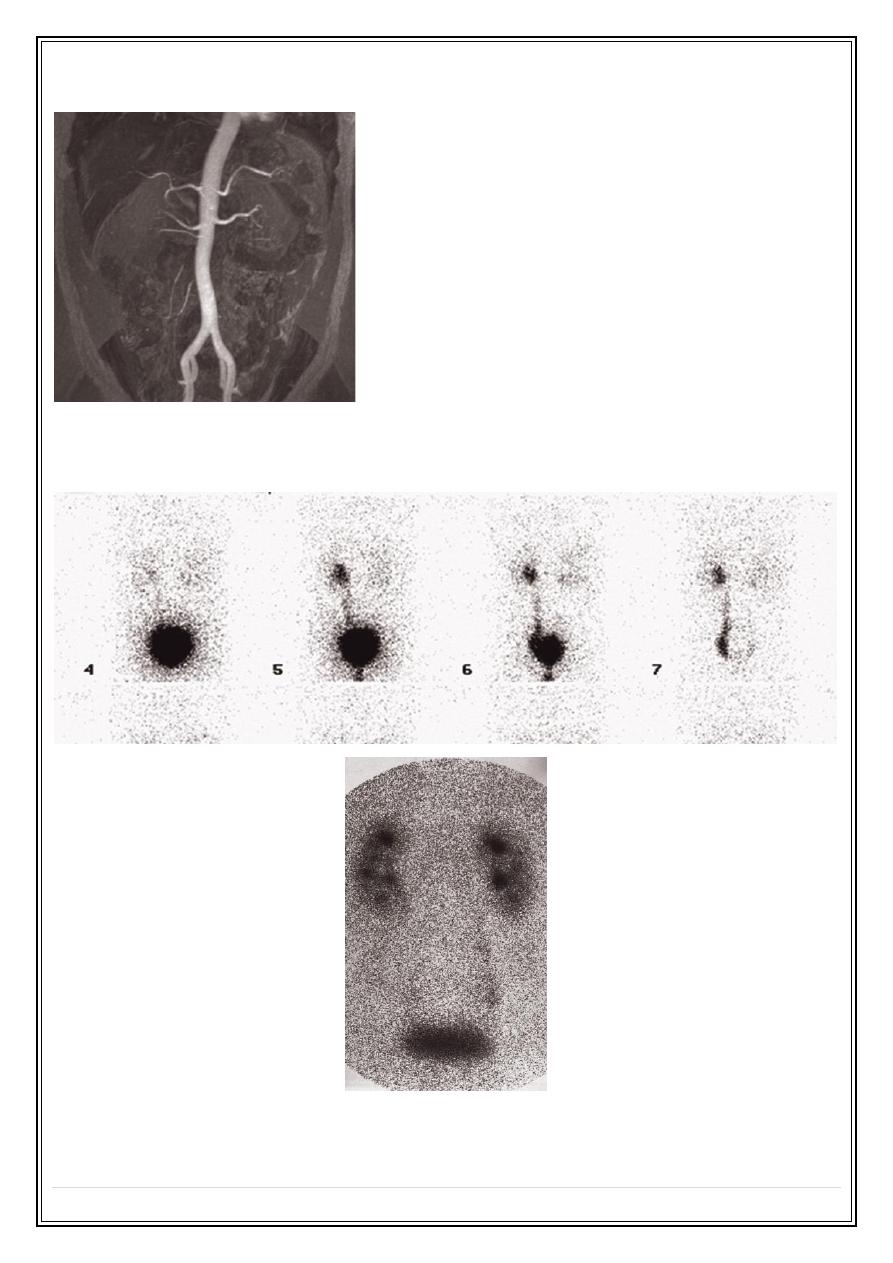
Radionuclide examination
Tha nk
y ou, , ,
