Hand injury & reconstruction
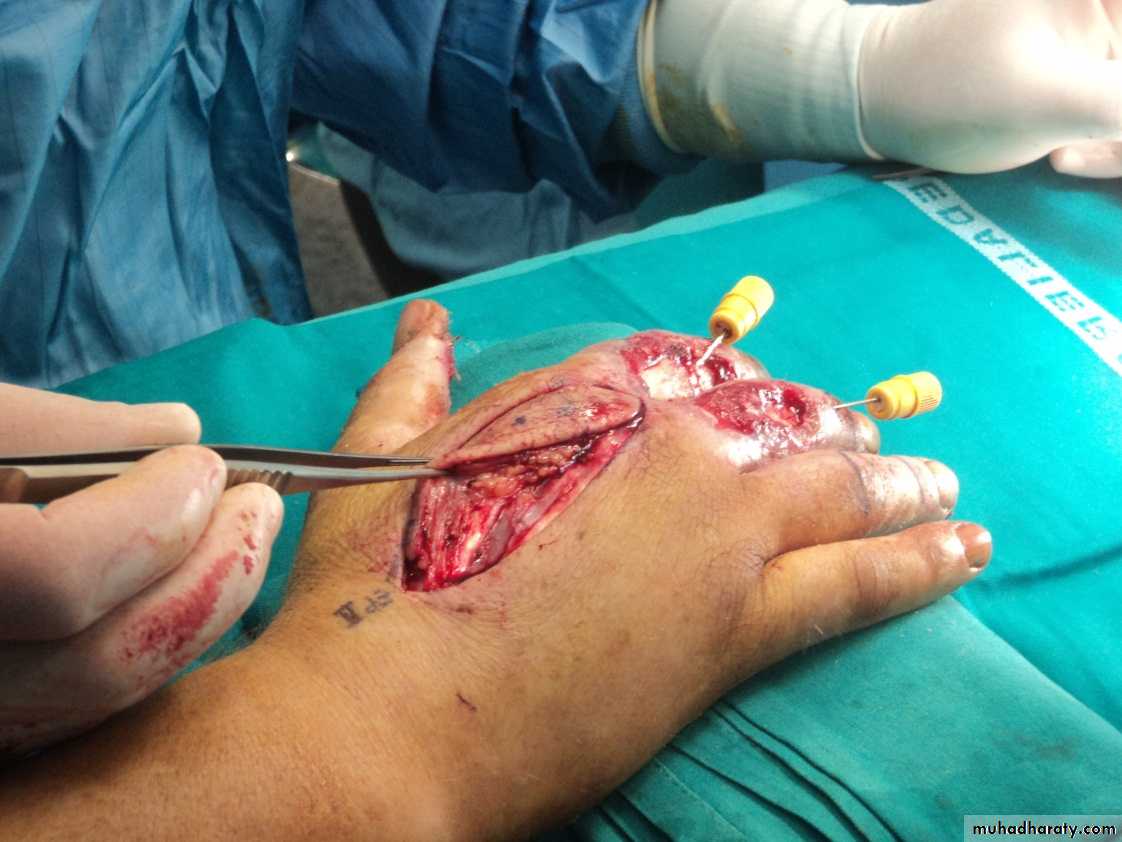
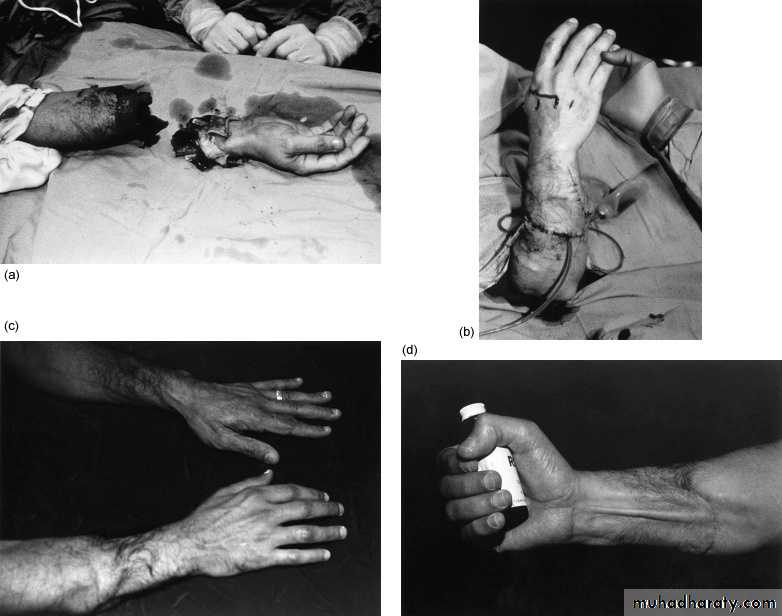
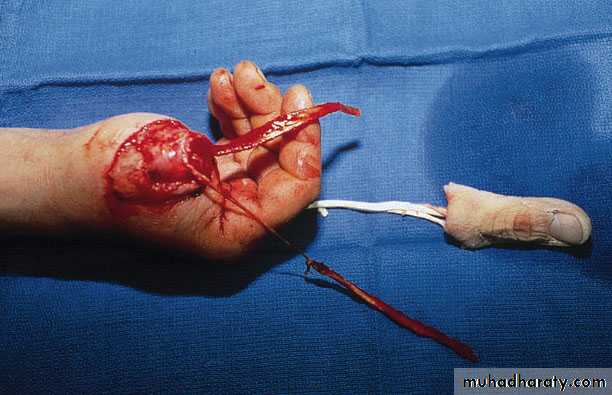
Treatment of Finger and thumb injuerieseither replantation or amputation or transimpantation
1--- replantation.
- levels amputation of many fingers at all levels except the most distal deserves an attempt at replantation.
From inspection of the parts it may be difficult to determine which will survive or which will be the most functional.
- multiple replanted fingers in the well-motivated patient usually function better than single
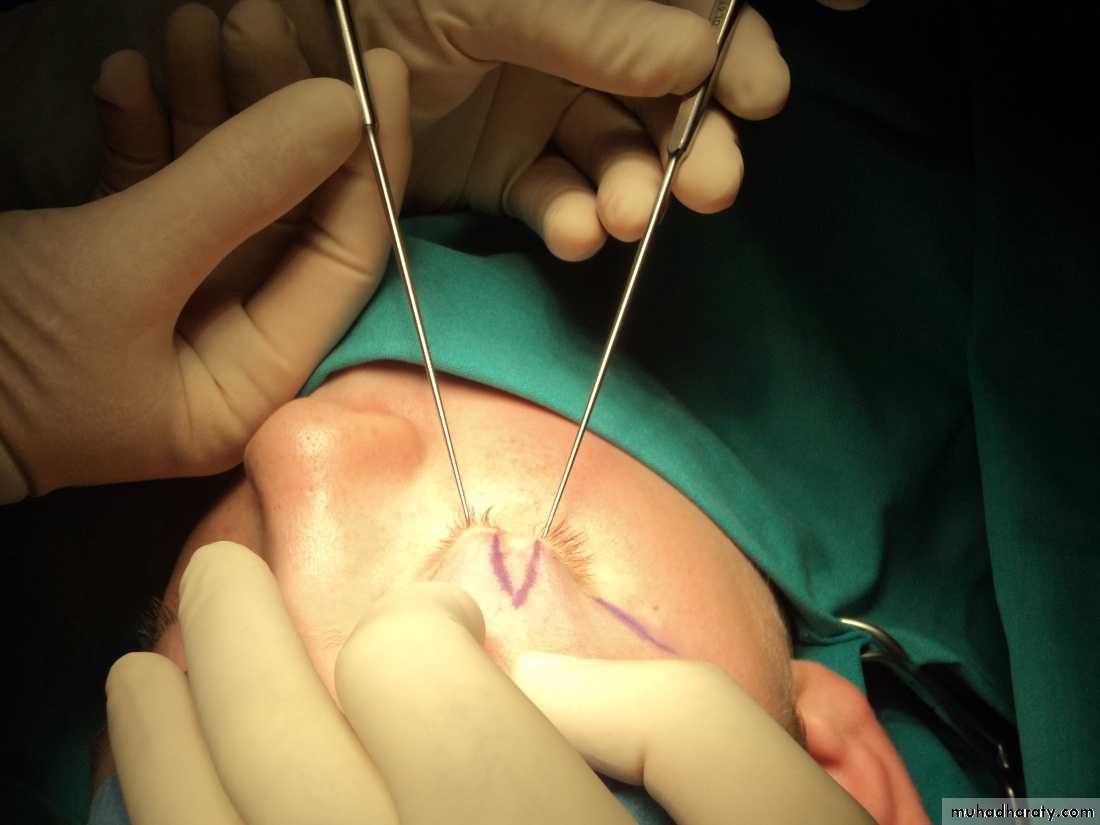
2--- amputation of single finger - V- shape, finger incision with resection of head of metatarsal bone, approximation of adjacent finger ( which is hindered by head of metatarsal ) give better shape & function
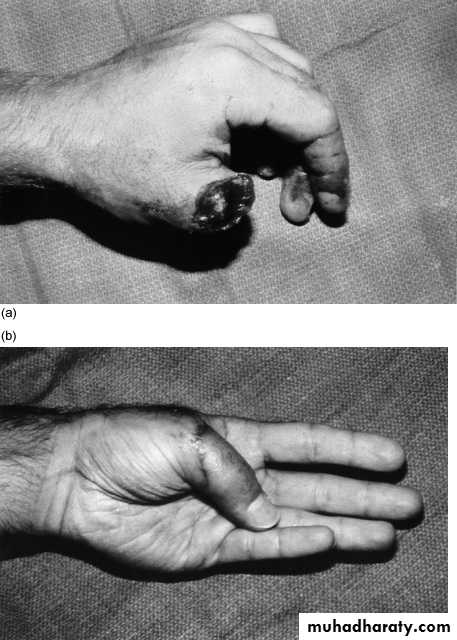
3-- transimpantation amputation of thumb , can use in some centers , big toe transimpantation
Success in revascularizing of the amputated part depends on the mechanism of injury
-- in Clean, guillotine amputations success excess of 90 %-- in crushing amputations, the risk of vascular thrombosis .and failure
Success in Functional results are dependent on
--the mechanism of injury
-- rehaplitation ,
-- the age ,Young patients will regain more than old patients.
-- motivation of the patient.
Which injuries require replantation
: 1-all thumb amputations 2-multiple amputated digits 3-all children 4-all amputations proximal to the digits 5-single digits proximal to the FDS insertion
Strong contraindications : (life threatened)
1-significant associated injuries to the trank and head. 2-extensive injury to the affected limb or to amputated part (degloving, widespread crush) 3-severe chronic illness precluding transportation or prolonged surgeryRelative contraindications:
1-Single digit amputation, especially distal to insertion of FDP 2-avulsion injuries 3-severe degloving injuries(extensive section of skin is completely torn off the underlying tissue, severing its blood supply) 4-previous injury or surgery to that part 5-extreme contamination 6-lengthy warm ischemia >8hrs (at 4 degrees C >30 hrs)7- old age 8- poor rehabilitation potential
transplantation
Facial injuries
EyelidLower lid
Loss of up to 25 % primary closure
more cheek flap preauricular
Upper-lid
up to 25 % For primary closurelarger defects tissue is borrowed from the lower lid in the form of a cross-lid flap.
The lacrimal punctum of the lower lid should be preserved,
Nose
Partial--composite graft.
--A graft from the concha of the ear can be used to replace any missing cartilage.
--nasolabial flap..
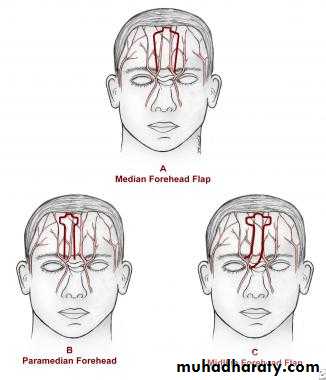
Total
forehead flap. This procedure is one of the oldest in plastic surgery. A flap based on the supratrochlear vessels may be turned 180° to cover the nasal structures
Composite graft
Nasolabial flap
Forehead flap
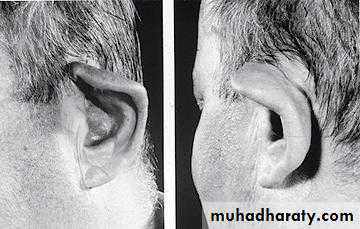
Ear
Reconstruction of all or part of the ear for either a congenital or a post-traumatic defect requires a cartilage framework and a thin-flap skin cover.
The best source of cartilage graft is the confluence of the lower costal cartilages
Cauliflower ear
Full thickness skin graft for scalp lesion
TUMORS
• Skin lesions• Breast
Skin lesions
Benign skin lesionsI-Non-aggressive benign tumors
Papilloma, Fibroma, Lipoma, Neuroma
II-Aggressive benign tumors
Desmoid's tumors or aggressive fibromatosis
Atypical lipomas and atypical fibrous histiocytomas
Malignant tumours
1-Carcinomas , 2-Sarcomas, 3-Germ cell tumours
Skin lesions
Benign skin lesionsI-Non-aggressive benign tumors
Papilloma
consists of a central axis of connective tissue, blood vessels and lymphatics; the surface is covered by epithelium,
Fibroma
--A true fibroma rare (containing only fibrous connective tissue).
-- combined fibromas with other mesoderm tissues such as
muscle (fibromyoma), fat (fibrolipoma) ,nerve sheaths (neurofibroma).
--Multiple tumours are not uncommon as, for example, in neurofibrormatosis (von Recklinghausen ’ s disease,
von Recklinghausen ’ s disease
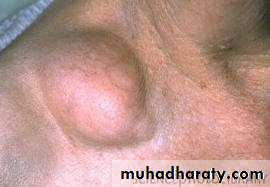
Lipoma
--Lipomas may be encapsulated or diffuse.--Most lipomas are painless , But sometimes painful and multiple eg. neurolipomatosis. Dercum ‘ s disease ,characterised by tender deposits of fat
Neuroma
True neuromas are rare. They usually mixed types:
• Ganglioneuroma
• Neuroblastoina
• Neurilemmoma (syn. Schwannoma)
dermoid
arise from totipotent cells containing cells from 3 embryonic layers (contain hair , teeth , muscles , gland ….)Types of dermoid:
--Teratomatous D - overy ,testicular , retroperitonial
-- sequestrated angular D(root of nose ),lat. Side of eyeborow ,
-- implantation D - wound , finger
-- congenital reminent :- thyroglosal Cyst tubodermoid ,postanal
-- other - lingual , sub lingual
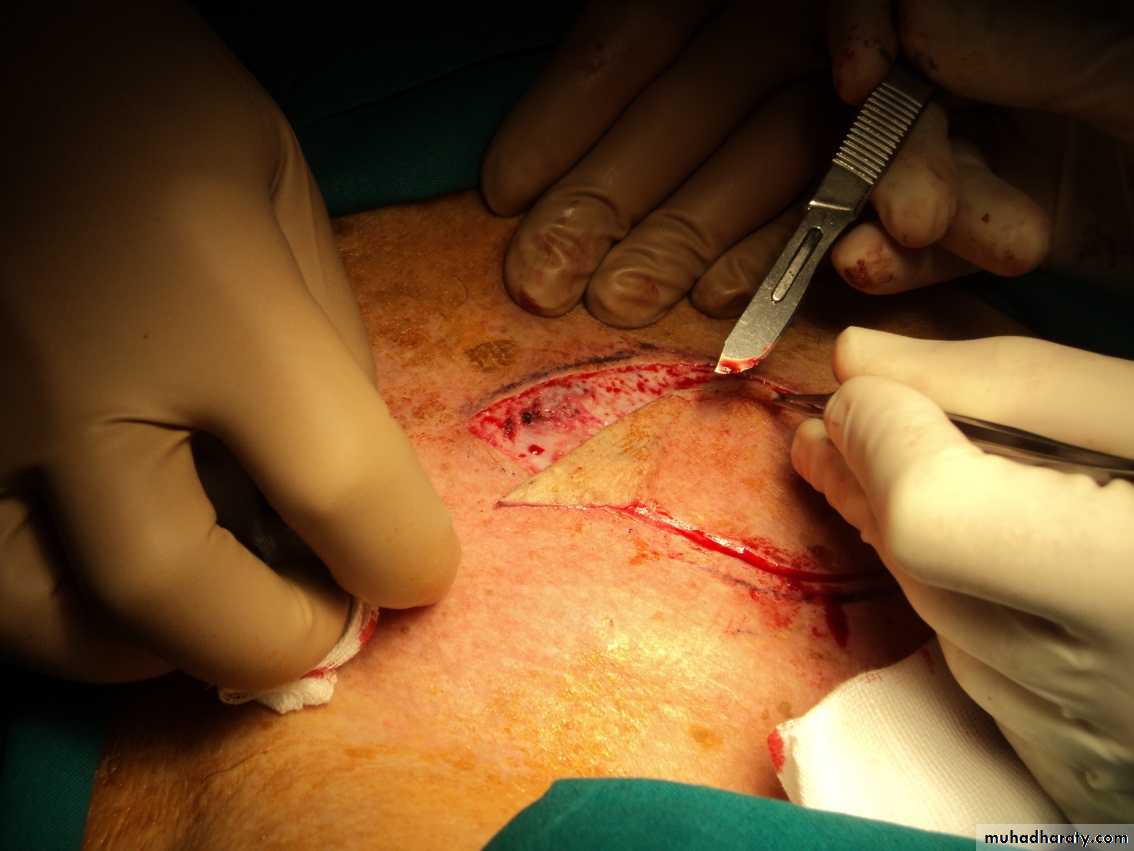
Treatment of benign tumors
All These benign lesions are usually excised as an elliptical incision, with out save margin which allows a straight-line closure* before treatment of angular dermoid should take skull X ray to exclude any connection with intracreanial structures
II-Aggressive benign tumors
Desmoid's tumors or aggressive fibromatosis can arise from any fascial tissue.
* Surgical resection wide resection
. Positive margins is generally followed by recurrence.
*Irradiation is effective in controlling desmoid tumors if 60 Gy can be delivered.
*The hormonal with progesterone, tamoxifen, indomethacin, and ascorbic acid have all been reported to induce remissions.
Atypical lipomas and atypical fibrous histiocytomas are generally located deep in the soft tissue or muscle;
- they tend to recur locally after resection
Malignant tumours
1-Carcinomas arise from cells which are ectodermal or endodermal in origin, and they are classified- squamous -celled
- basal-celled
- glandular (adenocarcinomas).
2-Sarcomas occur in connective tissues with structures of mesoblastic origin,
-- fibrosarcoma,
-- osteosarcoma.
3-Germ cell tumours arise from germ cells (teratoma, seminoma,).
( Ovarian cancer is an adenocarcinoma: it does not (arise from oocytes
Management of malignant tumors
Basal-cell carcinomaThe lesions are best excised with save margen and intraoperative control of margins. by frozen section
repeat excision is usually recommended.
Squamous-cell carcinoma
a wider margin than is required than basal-cell cancers. Intraoperative examination of the resection margins by frozen section is advised.
Because of the increased risk of metastasis, the draining lymph nodes
Melanoma
wider margin than squamous-cell carcinoma. A margin of 1.5 cm is recommended on the face near vital features; a margin of 3 cm is recommended elsewhere.
-- adjunctive treatments irradiation, chemotherapy, and immunotherapy, none has been successful.
BCC
Sentinel LN
Breast surgery
1- Augmentation2-Reduction (mastopexy)
3- Reconstruction mammoplasty
4-Subcutaneous mastectomy1- Augmentation
increase the size, change the shape, and alter the texture of the breasts of a woman. by placement of an implant behind the mammary tissue or behind the subjacent pectoral muscle.The indications : --
--cosmetic interests of the patient
-- marked asymmetry due to dystrophy of one breast
The operation.
--The route of access is through an incision either in the areola ,or just above the inframammary crease, or within the axilla.
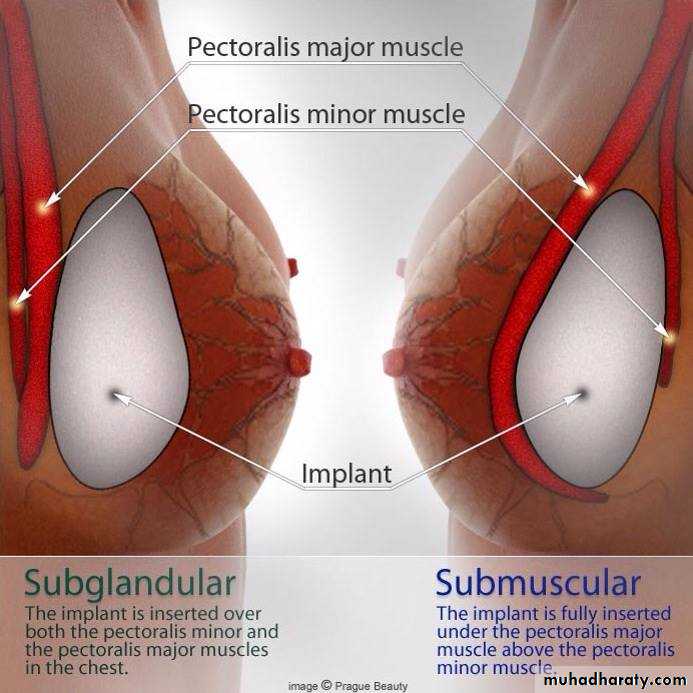
-- The a pocket carried down to a plane either over pectoralis major under breast glands (subglandular ) or between the pectoralis and pectoralis minor muscles( submascular),
--Implants used usually Silastic outer envelopes filled with either a gel of the same material or with saline.
complications
1- the breast become rounder and firmer than desired because capsule contraction around the implant,2- decreased nipple sensation
,
3- hematoma formation within the pocket,
4- a hypertrophied scar at the incision,
5- necrosis2-Reduction mammoplasty and mastopexy
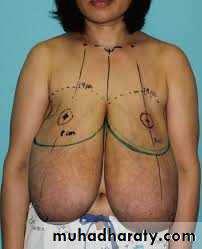
• reduction mammoplasty :- is procedure for reducing the size of large breasts• mastopexy is procedure to correct breast ptosis is not indicated by medical cause or physical reason, but by the self-image of the woman;
• Large breasts may cause:-
• 1--neck and back pain,
• 2--grooving of the shoulders from the brassiere straps,
• 3-- intertrigo.
• A breast reduction is performed either to alleviate these symptoms or to improve the appearance.
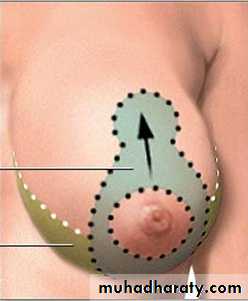
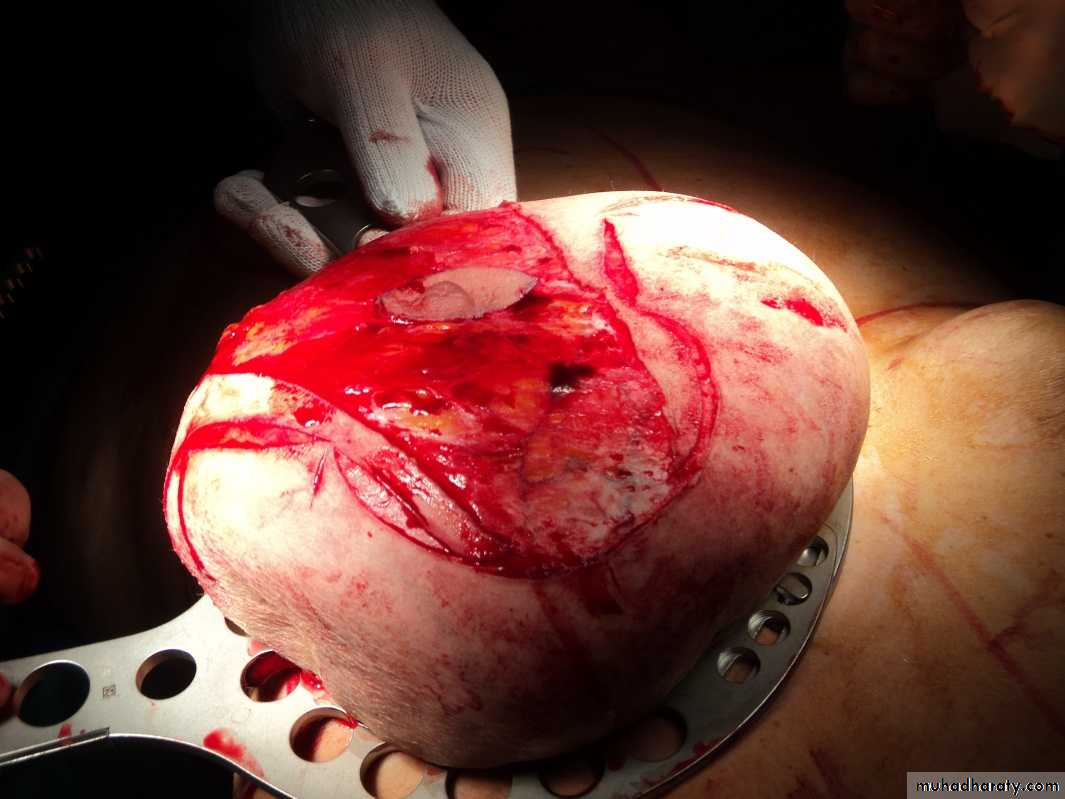
1-Mammoplasty
is remove excess of 300 g per breast.
The pattern for breast reduction is best in a standing position before surgery.
The nipple, is left as an island
on the pedicle.Medial and lateral segments
of breast tissue and fat are
removed.
.
ptosis
complications
1- hematoma2- decreased nipple sensation
3- hypertrophied scars
4- asymmetry
5- nipple loss due to ischemia.
Patient satisfaction with the change in breast shape and weight is usually high
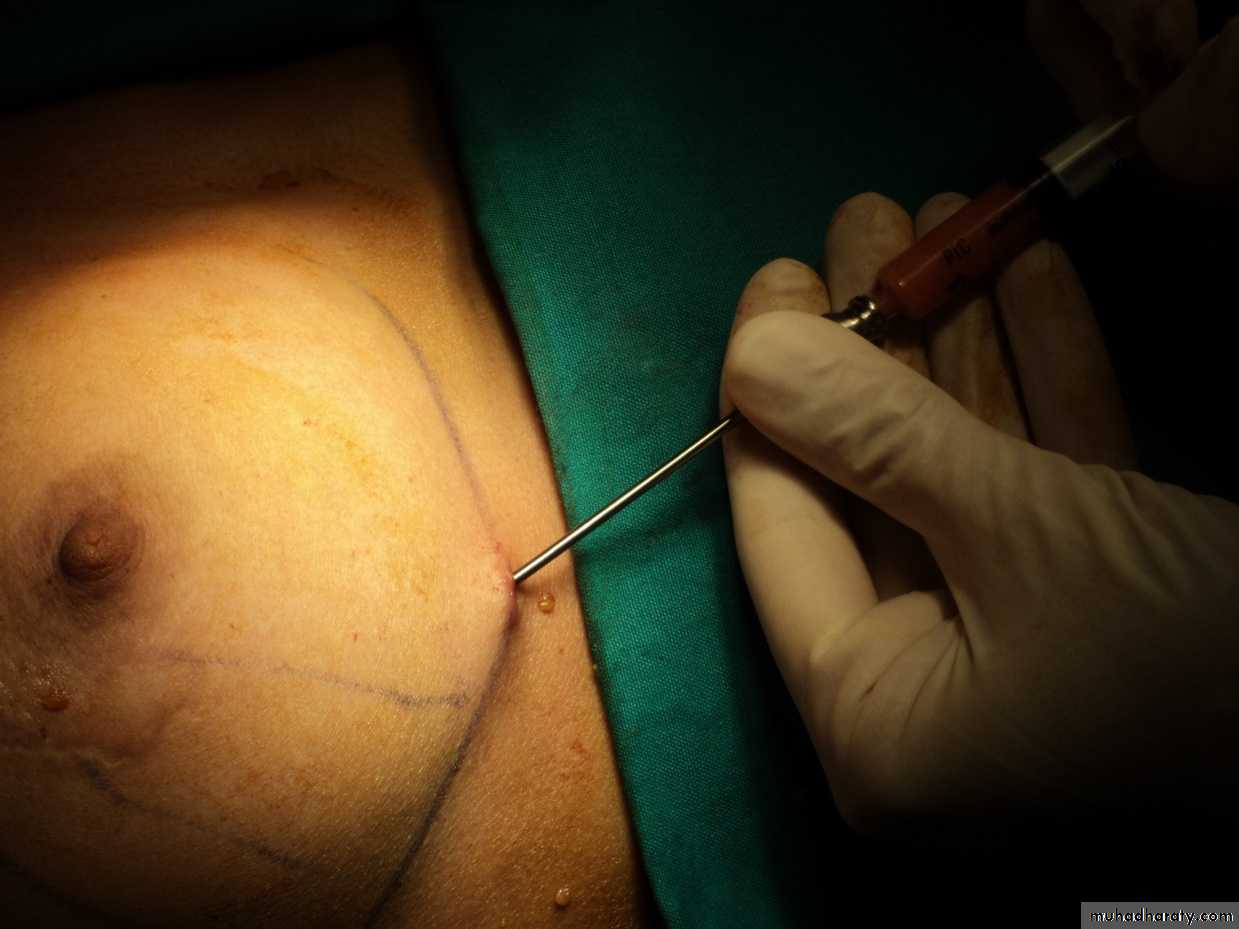
2- Suction lipectomy
Its better than mammoplasty by minimize the resultant scars , may be performed to reduce axillary fat.Suction mammaplasty--and indeed all short-scar procedures that are performed on the breast, face, and body
3- Reconstruction mammoplasty
• after mastectomy or traumatic or genetic deformity• The early immediate
• --No other operation
• --Psychological
• Should be preserves more of the native breast skin ,
• The delayed
• --operation may give more time to decide which type of reconstruction, prevention of complications
• -- may required postoperative radiation or chemotherapy.
Types of operations
implant placed in a submuscular pocket, similar to augmentation. but in 2 steps1st use implant expander (to produce appropriat pocket for implant
2nd removal of expander and insert implant
Usually completely beneath muscles
--to protect the implant from overlying flap necrosis and
--to minimize scar capsule contraction.
--early recognize any recurrence of tumor
myocutaneous flap from latissimus dorsi with an implant placed under the pectoralis major.
expander
implant
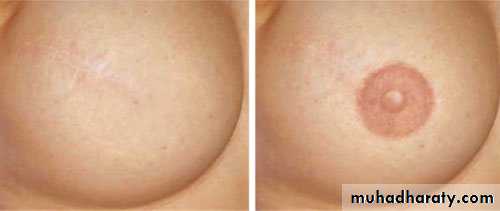
Reconstruction of nipple and areola
:
Latissimus Dorsi Flap
Complications
1- bilateral dispreportion A larger and more ptotic breast when compared with opposite breast
2- There is little functional deficit from the transposition of the muscle.
3- The blood loss from the rectus abdominis is an extensive
4-necrosis of skin over implant
necrosis of skin over implant
4-Subcutaneous mastectomy
The breast tissue may be removed with preservation of the entire breast skin and nipple in .The indications
- premalignant disease.- benign breast disease
- gynecomastia
Subcutaneous mastectomy
Gynecomastia
common disorder of the endocrine system in which there is a non-cancerous increase in the size of male breast tissueCauses :-
1- Idiopathic In adolescence usually resolves spontaneously in several years.
2-hormonal ;- either increase of esterogen due to gonadal problems or tumours or non gonadal diseases ( liver , lung , adrenal)
3- drug :- hormonal , cimitidin , digitalis
4- Klinfelter syndrome
5- breast tumour :- Unilateral breast enlargement in older men should be biopsied because of the rare occurrence of male breast cancer.