
1
SHIGELLAE 3
rd
Stage
• The genus Shigella contains fewer species than the genus
Salmonella and is antigenically less complex.
• Clinical dysentery may be caused by Shigella, Salmonella,
Entamoeba histolytica, Proteus morganii, and viruses.
• Shigella dysenteria was isolated by Shiga in Japan in 1898.
SPECIES:
• 1. Shigella dysenteriae
• 2. Shigella flexneri
• 3. Shigella sonnei
• 4. Shigella boydii
CLASSIFICATION:
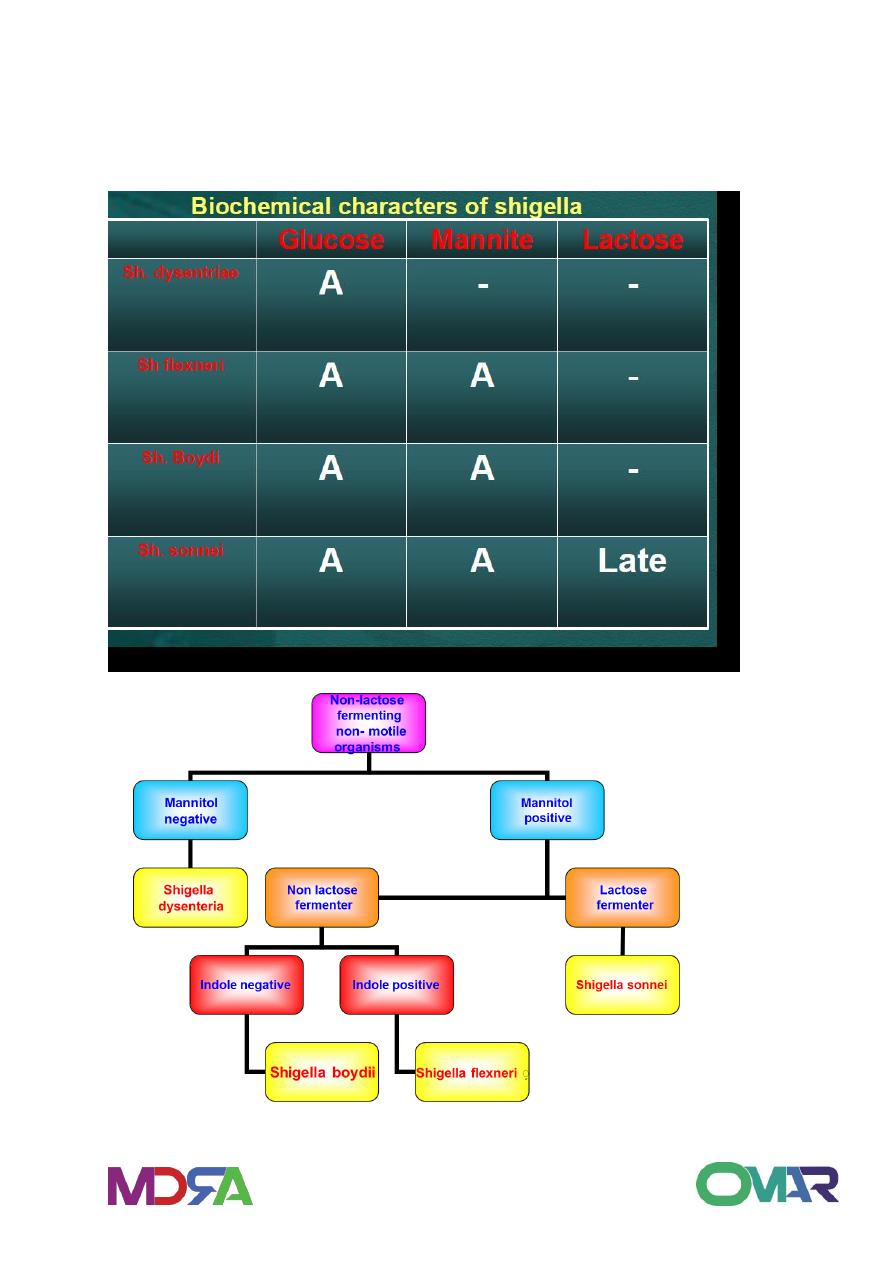
1. Non-mannitol-fermenters
Shigella dysenteria
2. Mannitol-fermenters
• Shigella flexneri
• Shigella boydii
• Shigella sonnei

2
.
MORPHOLOGY AND STAINING:
Short rods
Non-encapsulated
Non-motile
Non-spore former
Gram-negative
HABITAT AND TRANSMISSION
• Shigella species are found only in the human intestinal tract.
• Carriers of pathogenic strains can excrete the organism up to
two weeks after infection and occasionally for longer periods.
• Shigella are killed by drying. Shigella are transmitted by the
fecal-oral route.
• The highest incidence of Shigellosis occur in areas of poor
sanitation and where water supplies are polluted.
CULTURAL CHARACTERISTICS
• All members of Shigella are aerobic and facultative anaerobes.
• Grow readily in culture media at pH 6.4 to 7.8 at 10 oC - 40 oC,
with optimum of 37 oC.
• After 24 hours incubation, Shigella colonies reaches a
diameter of about 2 mm.
• The colonies are circular, convex, colorless, but moderately
translucent with smooth surface, and entire edges.
3
• Small tangled hair-like projections can sometimes be seen at
one or more points on the periphery of the colony.
• In XLD they appear pinkish to reddish colonies while in
Heaktoen Enteric Agar (HEA), they give green to blue green
colonies.
• If a number of typical colonies present onto the original plate,
a tentative diagnosis can be made by direct slide agglutination
with polyvalent Shigella antiserum.
• In all instances, diagnosis should be confirmed by additional
biochemical tests and by specific type agglutination.
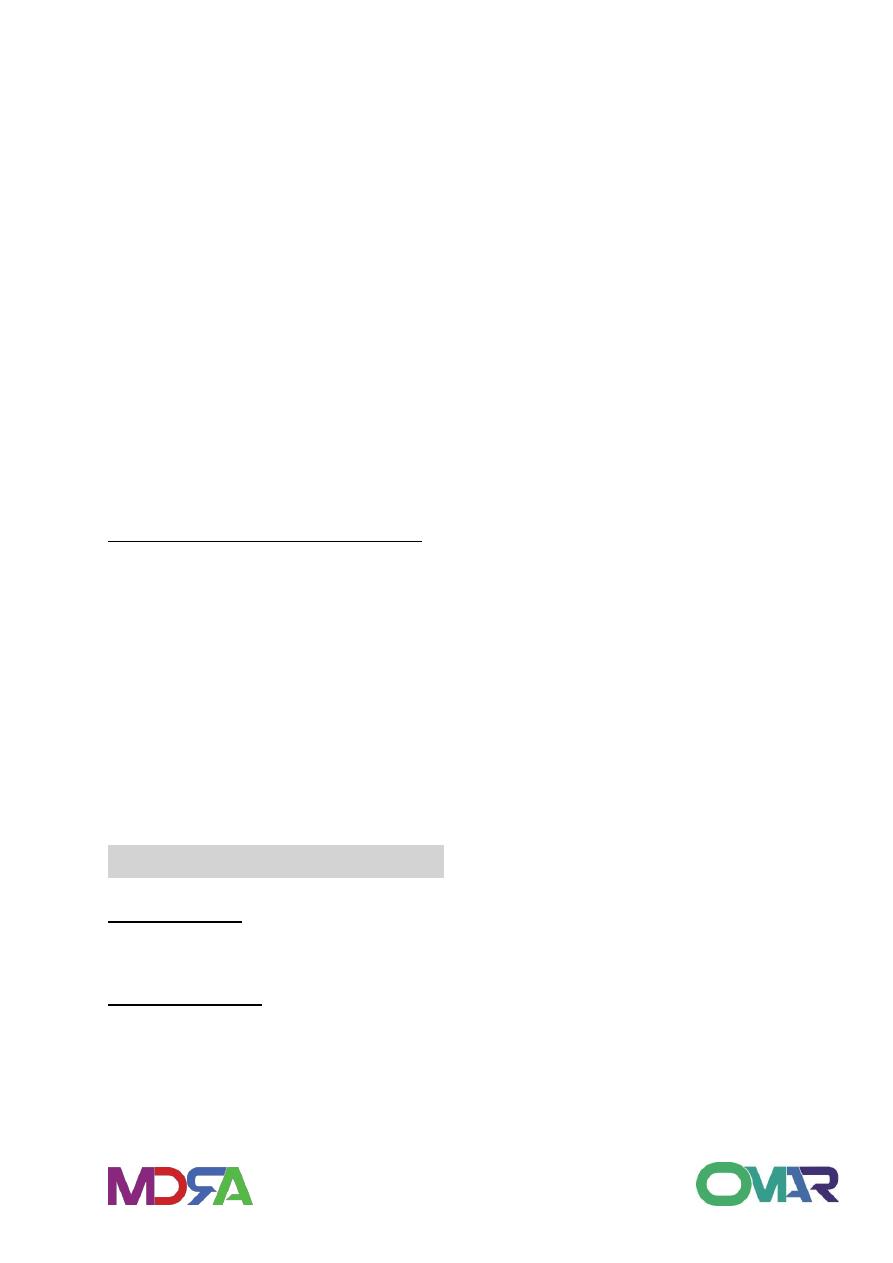
Biochemical Characteristics:
=All ferment glucose, some ferments mannitol
=They do not form acetyl-methylcarbinol,
=Does not hydrolyze urea or liquefy gelatin
=Citrate negative
=TSIA (Alkaline slant over acid butt)
=IMVIC V + - -
PATHOGENIC DETERMINANTS
O antigen: The ability to survive the passage through the host
defenses may be due to O antigen.
Invasiveness: Virulent shigella penetrate the mucosa and epithelial
cells of the colon in an uneven manner. Intracellular multiplication
leads to invasion of adjacent cells, inflammation and cell death. Cell
death is probably due to cytotoxic properties of shiga toxin that
interfere with protein synthesis. The cellular death and resulting

4
phagocytosis response by the host accounts for the bloody
discharge of mucus and pus and shallow ulcers characteristic of the
disease.
Other toxins: It has a protein toxin which may be neurotoxic,
cytotoxic, and enterotoxic. The enterotoxic property is responsible
for watery diarrhea.
LABORATORY DIAGNOSIS
The only satisfactory method
of laboratory diagnosis is to
cultivate the bacilli from the
patient.
In the early stages of acute
shigellosis, isolation of the
causative organism from the
feces is usually accomplished
without difficulties by using the
same special media and
methods
employed
for
salmonella
1. Cultivation of the bacilli from stool specimen during the first 4-5
days of the
disease.
2. Smears: Gram-negative bacilli appearing singly
TSIA = Alkaline/acid (No gas no H2S)
IMVIC reaction : V + - -
5
3. Serological examination with polyvalent and monovalent anti-
sera.

6
TREATMENT
1. Water an6d electrolytes replacement.
2. Antibiotic therapy is required to eliminate the organism. Due to
the emergence of resistant strains of shigella, antibiotic sensitivity,
must be performed on any shigella
isolate to determine suitable antibiotics:
Sulfonamides, tetracycline, Chloramphenicol, ampicillin and
streptomycin are known to be effective against shigella.
