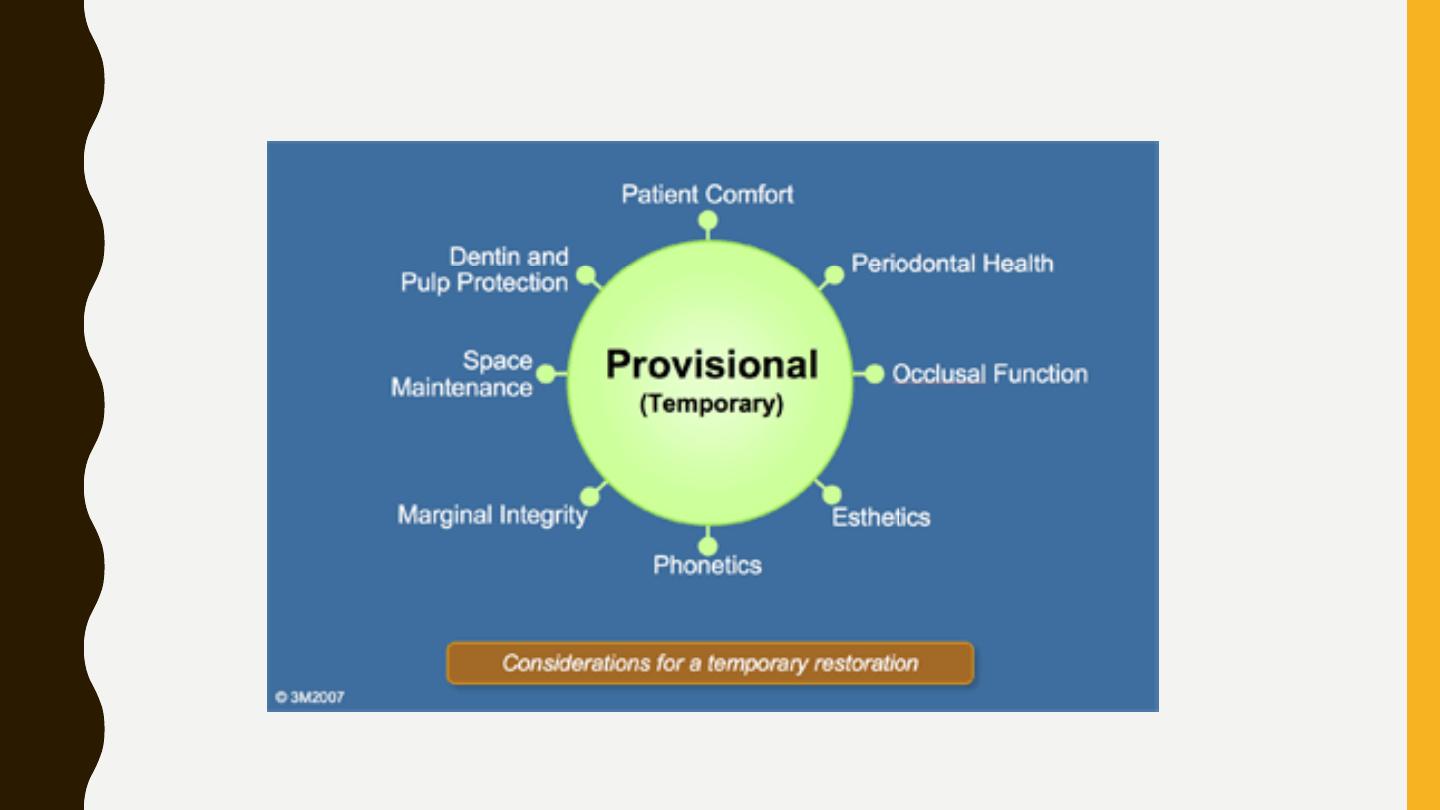
PROVISIONAL
RESTORATION
B A L S A M M . M I R D A N
PROVISIONAL (TEMPORARY) RESTORATIONS USED IN FIXED
PROSTHODONTICS ARE IMPORTANT TO THE OVERALL SUCCESS OF THE
TREATMENT.
•
First, they should adequately protect the pulp by completely covering prepared tooth structure
and providing thermal insulation.
•
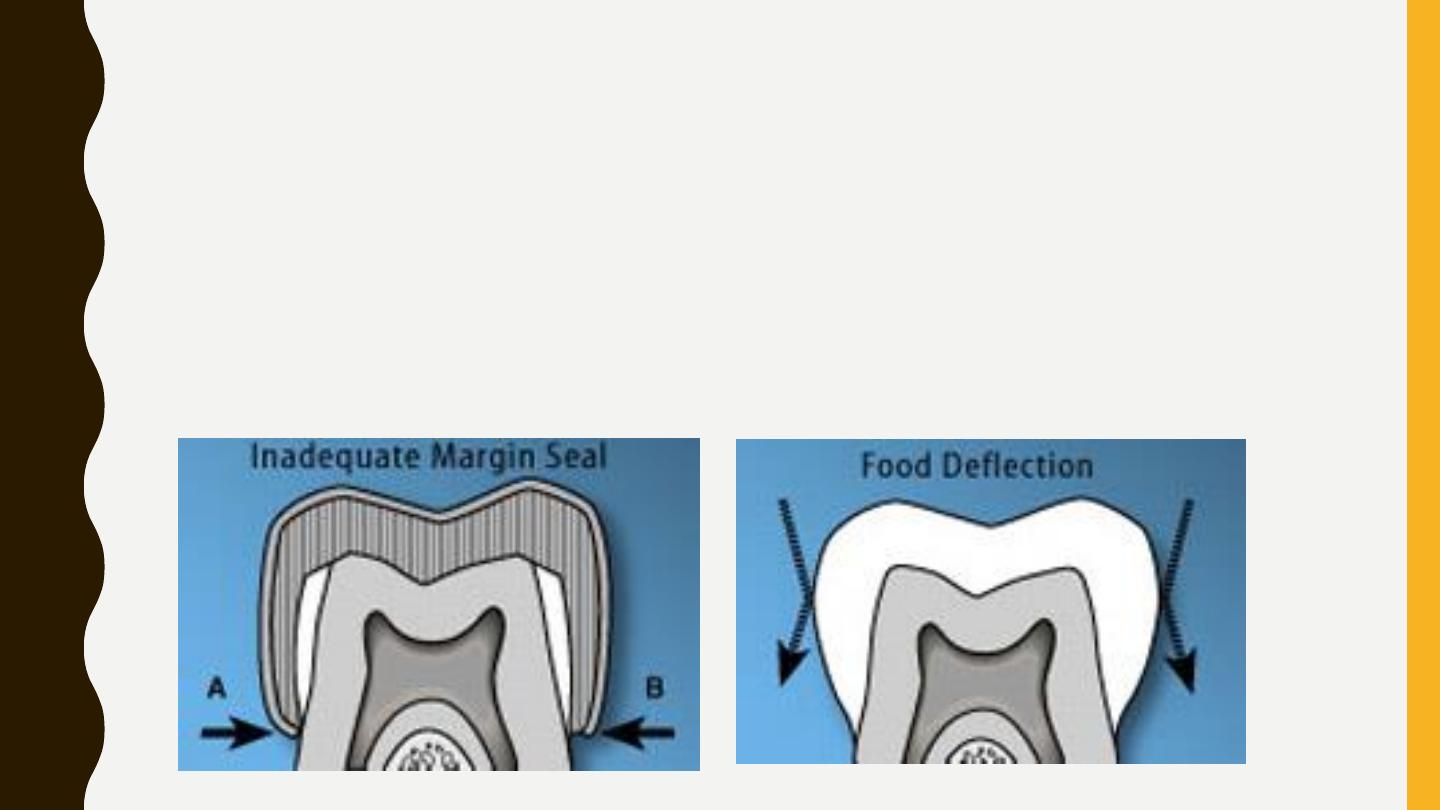
protect margins and prevent leakage by forming an intimate seal with the prepared tooth.
Provisional restorations have often been considered space maintainers, allowing the
patient to function until the final prosthetics were ready to be inserted.
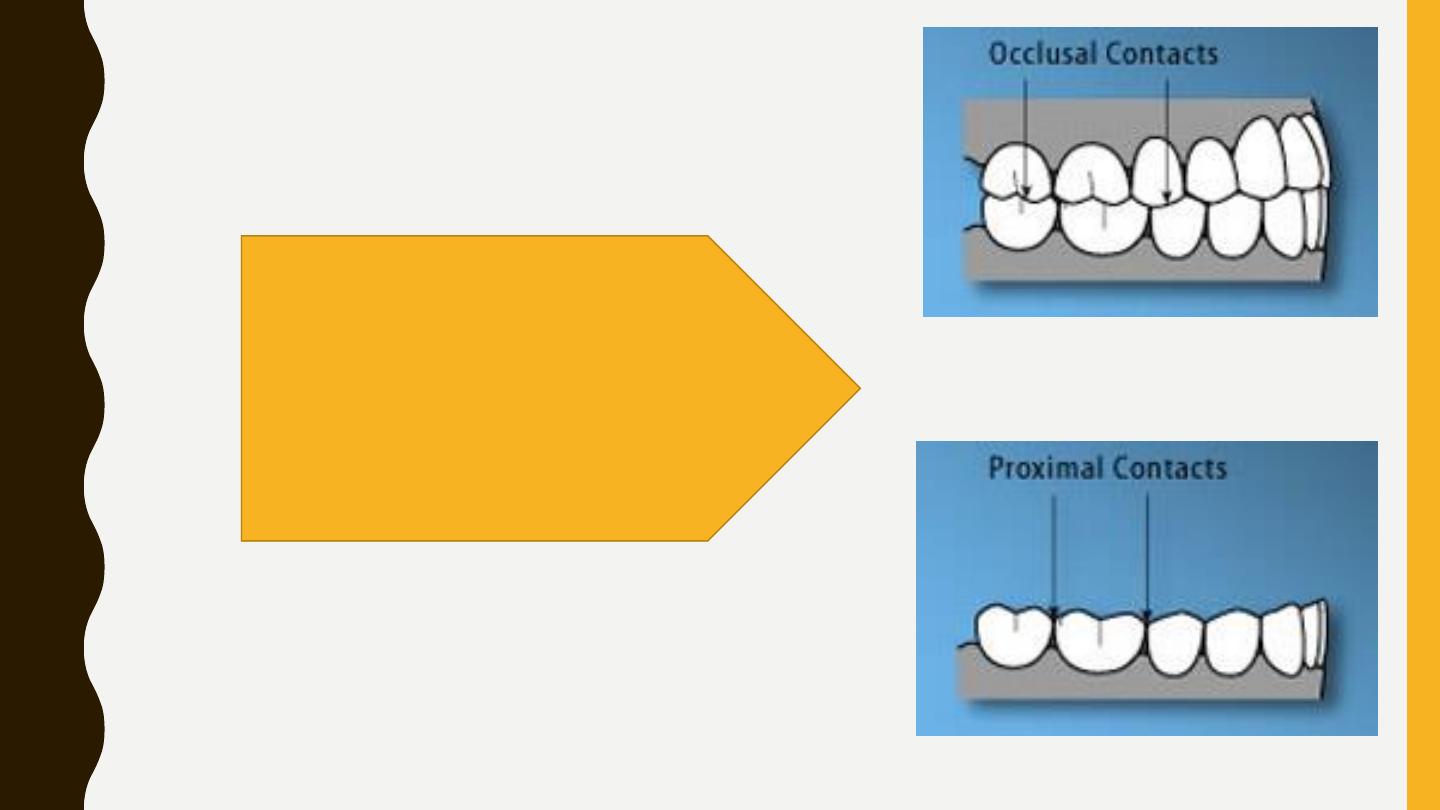
…..maintain space by
providing stable interproximal
and occlusal contacts.
•
Maintaining contacts helps patient function during treatment.
•
they should exhibit a good shade match and have a highly polished surface so they are
esthetically pleasing to the patient

BASIC REQUIREMENTS OF
PROVISIONAL RESTORATIONS
1. Provide pulpal
protection
2. Ensure marginal
seal
3. Maintain positional
stability
4. Provide for patient
comfort, esthetics,
and phonetics
5. Provide occlusal
function
6. Promote
periodontal health
7. Have minimal
shrinkage/distortion
8. Be adequately
strong
9. Be sufficiently
retentive
10. Have an adequate
level of radiopacity
11. Be easy to mix
and manipulate
12. Be easy to trim
13. Be color stable
TYPES OF TEMPORARY CROWNS:
•
1. Preformed temporary crowns.
•
2. Customized temporary crowns and bridge(Chair side temporary crowns).
•
3. Laboratory made temporary crowns and bridge.
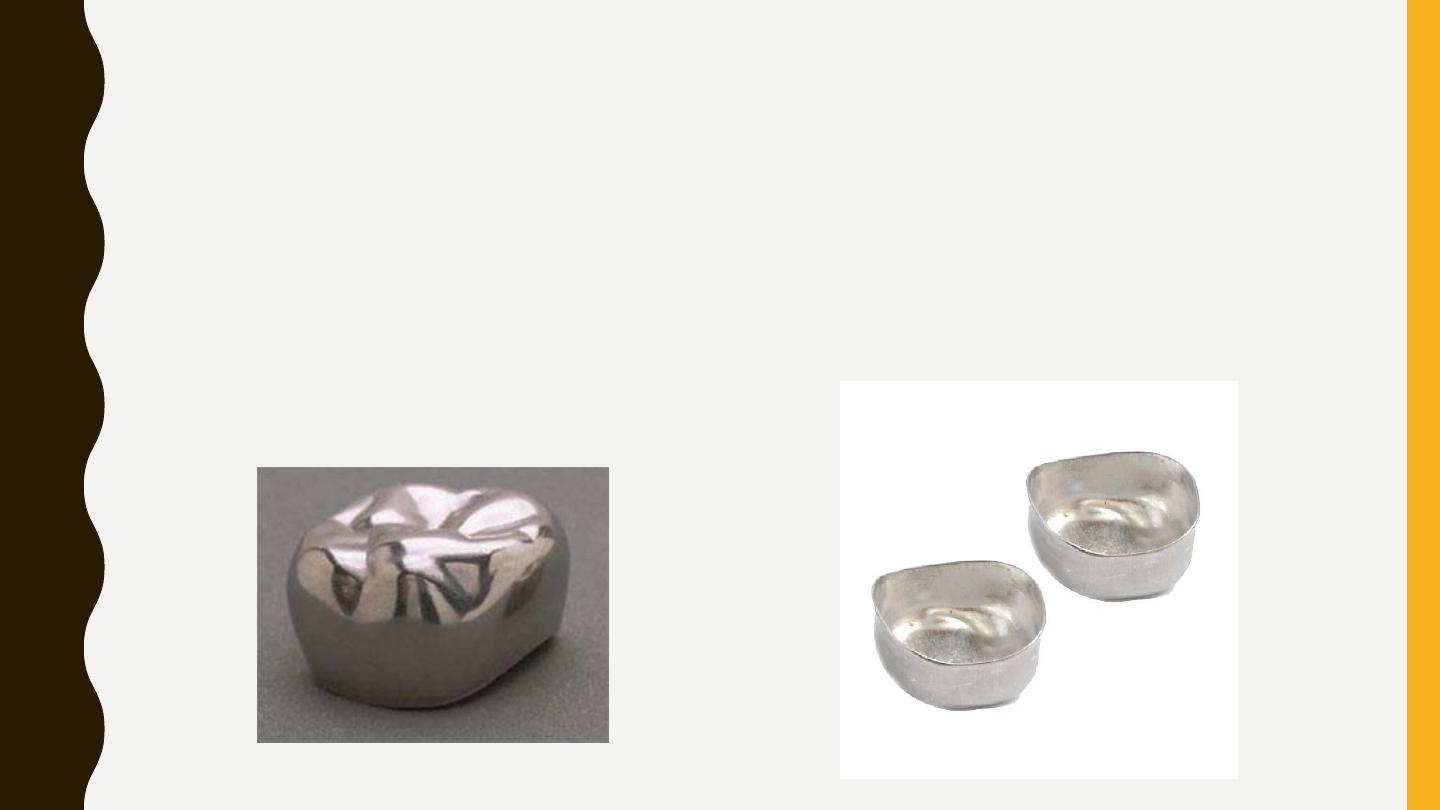
1. PREFORMED TEMPORARY CROWNS:
•
A. Metal crowns: Mainly used for posterior teeth, it comes in different shapes and
•
sizes made of stainless steel or aluminum. The Aluminum T.C. is either anatomical
•
(morphological) or non anatomical types (flat).
Technique for application of metal T.C.:
1. Select the proper size which fit the prepared tooth.
2. Trim (cut) the gingival margin with scissor to confirm it to the gingival
finishing line of the preparation & to accommodate the vertical height of the
occlusion.
3. Seat the T.C. on the prepared tooth inside the patient's mouth & check the
margin, occlusion & the proximal relation with opposing & adjacent teeth, if it
fit properly.
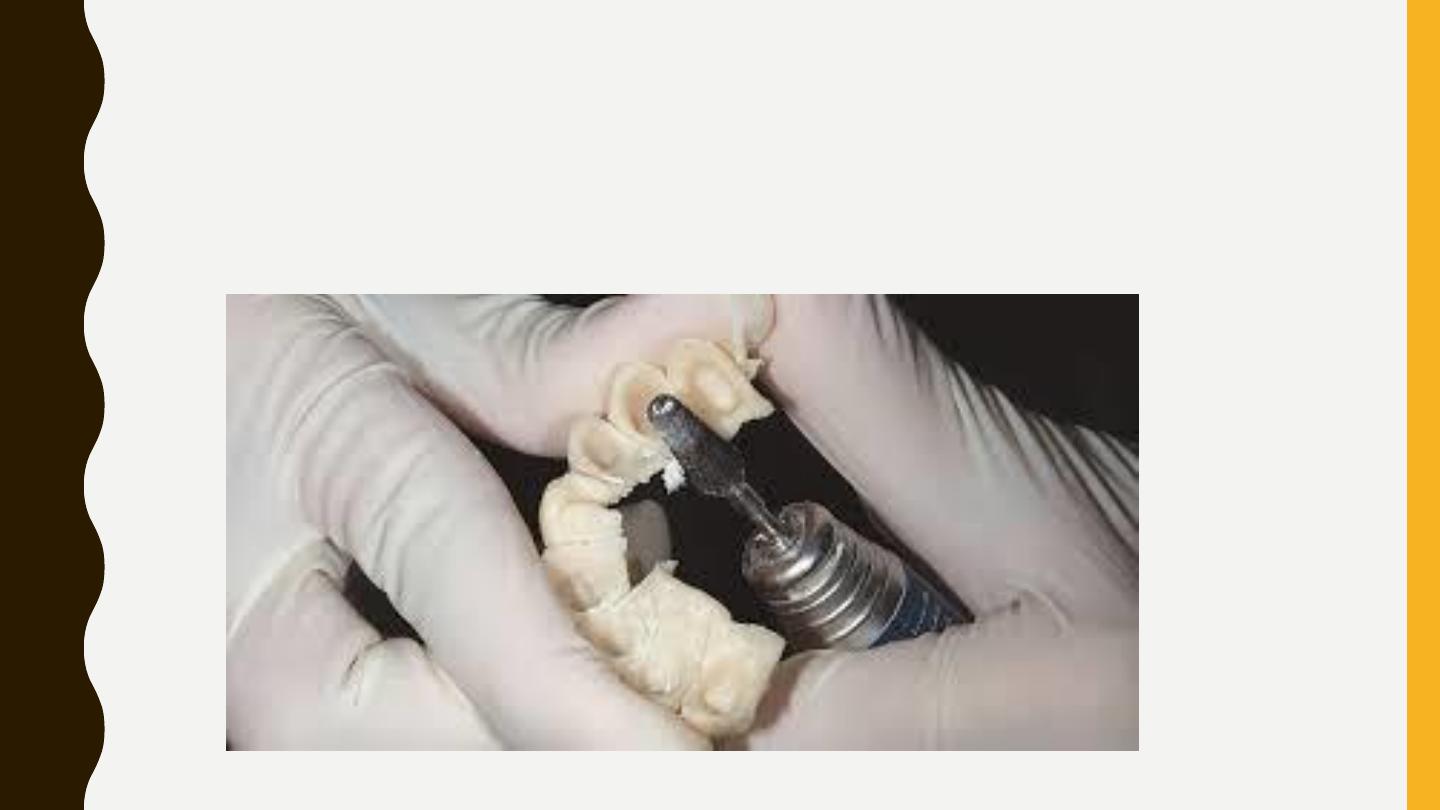
4. Remove the T.C. from the patient mouth; smooth the margin with stone bur.
5. Cement T.C. with ZOE cement on the prepared tooth.
B. Plastic crowns:
Polycarbonate temporary crown: made from poly carbonate plastic combined
with micro-glass fibers, available for anterior and posterior teeth.
Acrylic temporary crown
Celluloid crowns form: made from acrylic resin (tooth colored) and available in
different size and colors, they used for anterior teeth.
•
1. Select the proper size of T.C.
•
2. Try the crown on the prepared tooth if it is not fit on the prepared tooth , you should select
the most suitable size T.C. & follow the steps.
•
3. Cut the margin of the crown according to the finishing line.
•
4. Put a thin layer of separating medium on the preparation.
•
5. Mix cold cure acrylic.
•
6. Fill the crown with provisional crown material(acrylic or composite)& seat it on the prepared
tooth.
•
7. Remove the crown before it completely set; this is due to polymerization reaction of acrylic
which is exothermic reaction & this irritant the pulp
•
(On the polymerization reaction there is shrinkage in the acrylic).
•
8. Seat the crown on the prepared tooth.
•
9. Check the occlusion, contact point, fitness and extension.
Clinical procedure:
2. CUSTOMIZED TEMPORARY
CROWNS AND BRIDGE:
The technique called direct chair side temporary crown or over impression, and its indication:
•
1. Coverage of multiple individual crown preparations.
•
2. Single tooth preparation which is usually large or of special design.
•
3. Abutment preparations for fixed partial denture to construct temporary bridge.
IMPRESSION METHOD
Indirect impression method (clinical procedure)
An alginate over impression is made from the patient mouth and carefully stored
until complete tooth preparation.
When the tooth preparation completed, another alginate impression is made
and poured in quick set plaster or stone, wait till stone is set, the cast were
then separate from the impression.
Coat the prepared tooth (on the cast) with separating medium, a colored
acrylic is mixed and loaded in the over impression at the area of prepared
tooth only.
seat the cast onto the over impression in upright position and maintain
pressure (rubber band can be used for this) until acrylic is set completely, be
sure that the cast correctly seat into the over impression.
After complete polymerization, separate the cast from the over impression,
removed the formed crown from the prepared tooth.
Trim any excess material from the formed crown, the crown were seat on the
prepared tooth, Check the occlusion ,the margins then smooth it.
Cement temporary crown on the prepared tooth with ZOE cement .
Direct Provisional Fixed Partial Denture
In the direct technique, patient's prepared teeth and the gingival tissues
directly provide the tissue surface form eliminating all the intermediate
laboratory procedures.
This is convenient when assistant training and the office laboratory
facilities are inadequate for efficiently producing an indirect restoration.
disadvantages
potential tissue trauma from the polymerizing resin and inherently
poorer marginal fit.
Therefore, the routine use of directly formed interim restoration is not
recommended when indirect techniques are feasible
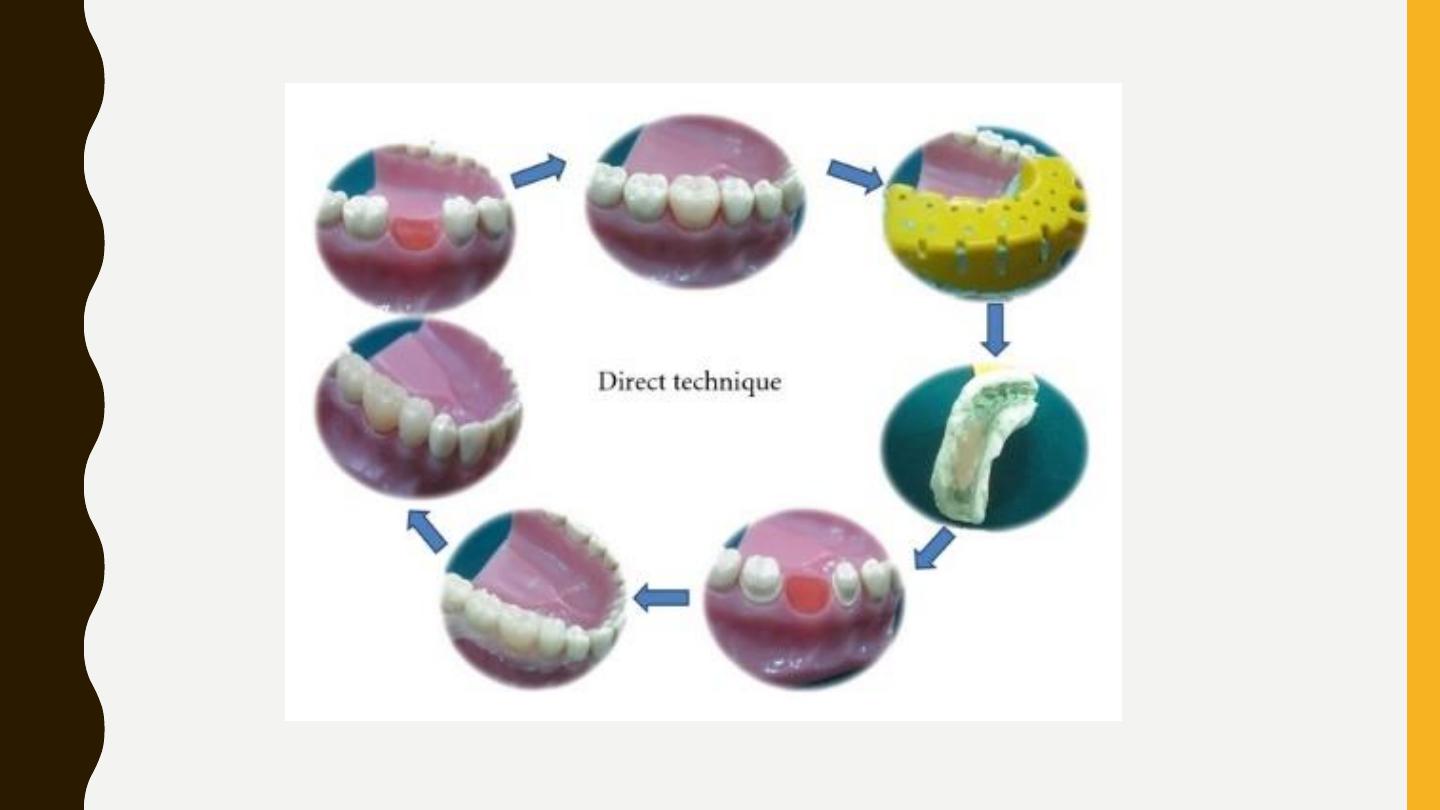
Procedure:
Before the tooth preparation, place an acrylic tooth in place of the missing tooth
and make an alginate impression or a putty index.
1.Prepare the patient's teeth in the usual manner.
2.Lubricate the prepared teeth and the adjacent gingival margins with petroleum
jelly, and reseat the index or the alginate impression with provisional restorative
material in the dough stage on the tissue surface of the impression.
3.Remove and reseat the restoration until it sets.
4.Finish, polish, and cement the restoration
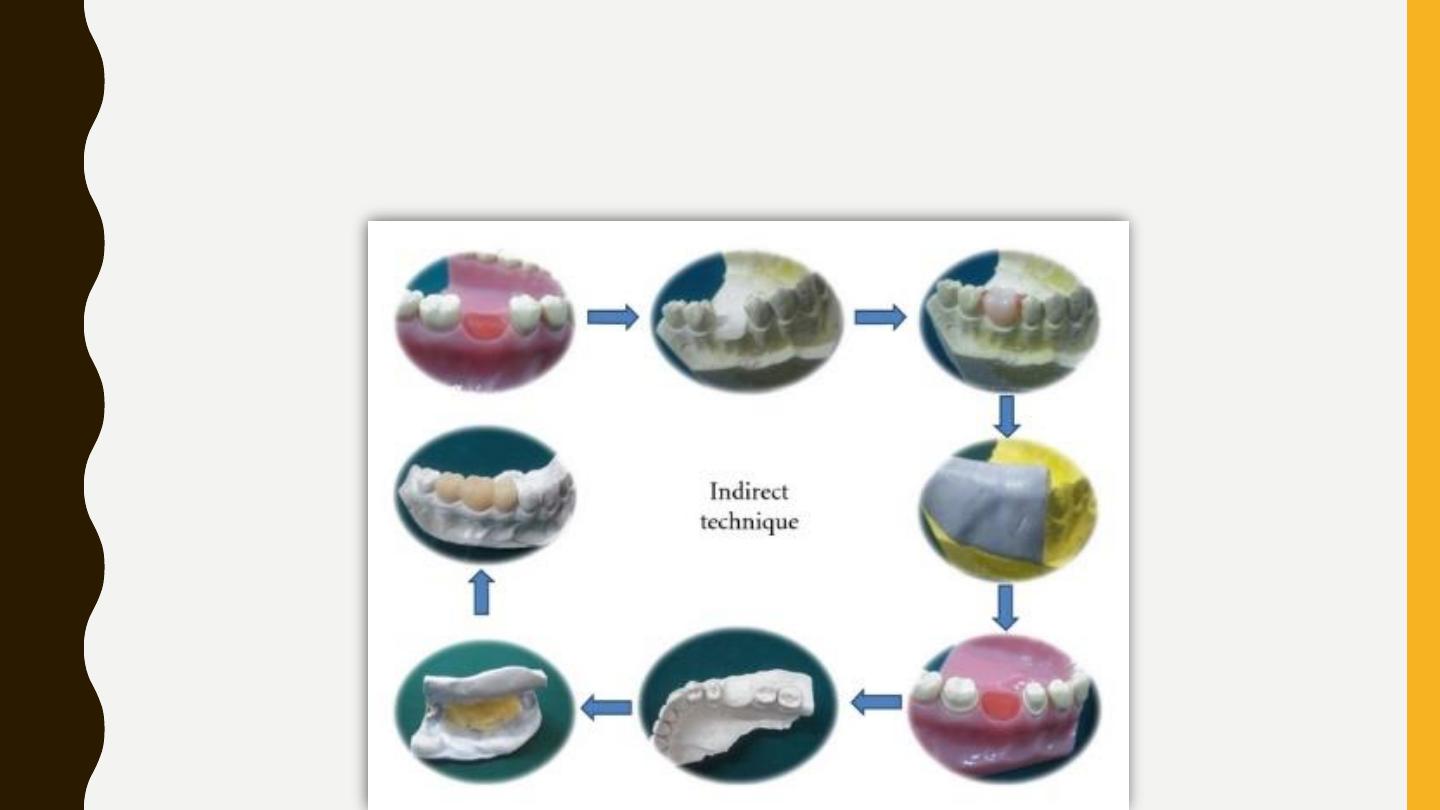
Indirect-Direct Provisional Fixed Partial Denture (clinical procedure)
Procedure:
(1)Pour an accurate pretreatment diagnostic cast from an impression of the unprepared teeth. For FPDs, wax a
pontic into the edentulous area of the study cast, and modify with wax to obtain ideal contours, contacts, and
occlusion.
(2)Lightly lubricate the modified diagnostic cast, and make an impression using a high-viscosity elastomeric
impression material. To provide an adequate bulk of material at the margins of the provisional, trim the sharp edge
on the elastomeric over impression that represents the gingival crevice with a round bur to allow for extra bulk of
resin material in this area. The silicone putty index is made involving at least on tooth each beyond the abutment
teeth.
(3)Remove the acrylic tooth and prepare the abutments on mounted diagnostic casts. (The diagnostic cast
preparations should be more conservative than the eventual tooth preparation and should follow precisely the
gingival margins.)
(4)Lubricate the prepared diagnostic cast with a petroleum jelly or any suitable separating media, mix the
provisional restorative material, and place it in the tissue surface of the index and reseat it on the prepared
diagnostic casts.
(5)After the acrylic resin has polymerized, finish the restoration. The provisional restoration should be paper thin
and correctly contoured, and it should precisely follow the gingival margins on the cast.
(
6)Prepare the patient’s teeth in the usual manner (to the gingival margins).
(7)Try in the preformed restoration. (If the amount of tooth reduction is adequate, the provisional restoration will
show optimal marginal fit with no need for adjustment.)
(8)Reline the temporary restoration to perfect the internal fit.(9)Finish, polish, and cement the restoration
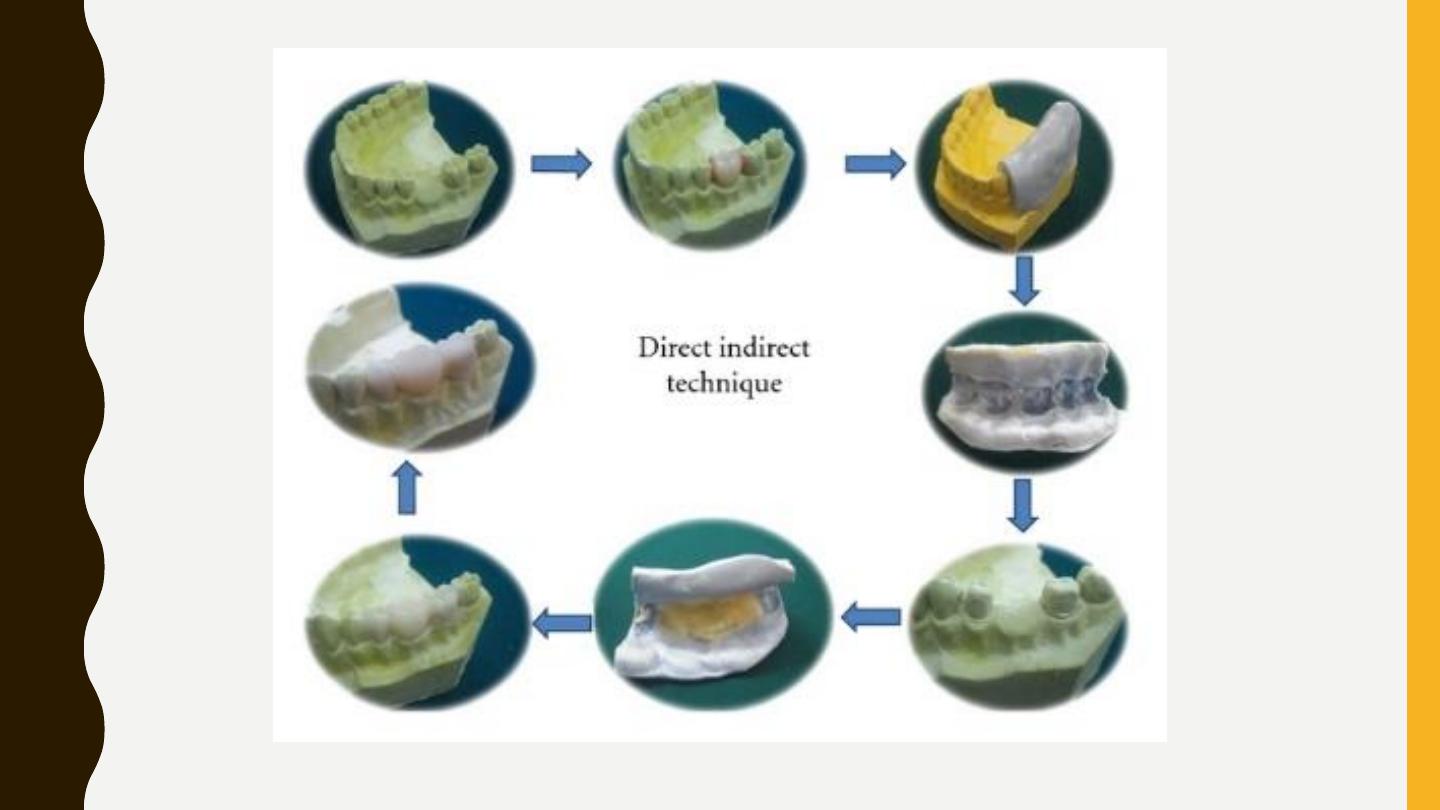
The technique produces a custom made preformed external surface form of the
restoration but the internal tissue surface form if formed by the underprepared
diagnostic casts.
Advantages
.
1/ chair time can be reduced, since the provisional shell is fabricated before the
patient
’s appointment.
2/Enhanced control over restoration contours minimizes the time required for chair
side adjustments.
3/ smaller amount of acrylic resin will polymerize in contact with the prepared
abutment, resulting in decreased heat generation, chemical exposure, and
polymerization shrinkage compared to the direct technique.
4/ the contact between resin monomer and soft tissues is reduced and less chances
of allergic reactions.
The
disadvantage
of this procedure is the potential need of a laboratory phase before
tooth preparation and the adjustments that are frequently needed to seat the shell
completely on the prepared tooth
