Dental Implantology
Introduction
Generally the term implantation applies to the transplantation of non-viable tissue, it is the use of inert foreign body implants (alloplasts) in human body tissues.A dental implant is "a non-viable device of biocompatible material(s) placed within or against the mandibular or maxillary bone to provide additional or enhanced support for a prosthesis or tooth".
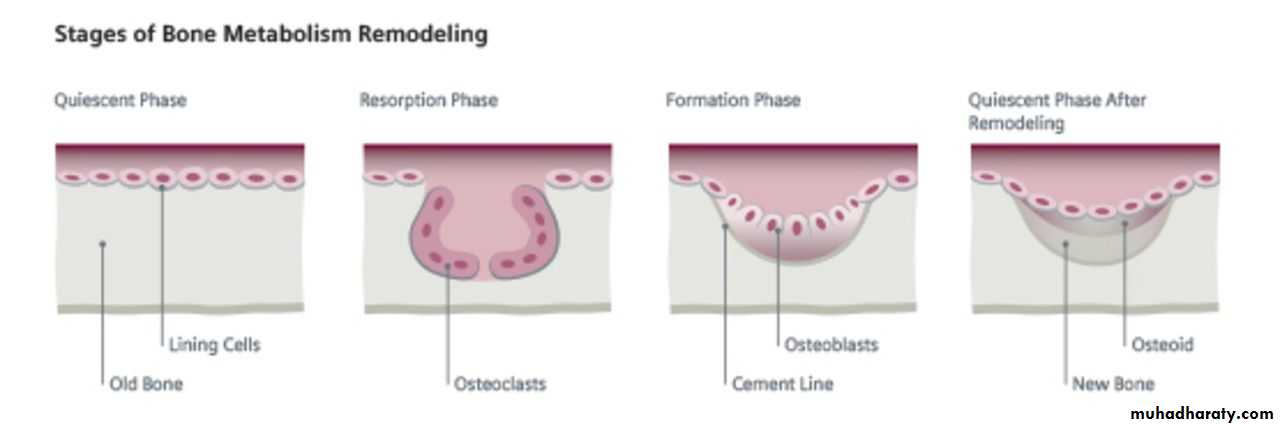
Bone remodeling
Modeling is the appropriate term to characterize changes in bone morphology occur during growth (turnover & replacement). Ridge resorption and atrophy are misnomer because resorption is a part of normal turnover process occurring in all bones, whereas atrophy implies a passive process.Remodeling of bone involves 3 steps:
* Activation: begins as a result of specific local (i.e. stress) and systemic (i.e. hormonal) stimuli.* Resorption: occur in all four of skeletal envelopes (periosteum, Haversian, cortical- endostea, trabecular). It is mediated strictly by osteoclasts which is the only cell in the body capable of resorbing bone. Often resorption occur parallel to the stress placed upon bone. Resorption also occurs in the absence of stress, but it does so in a less organized manner. Once resorption phase is complete, there is usually a delay period of 12-14 days after which formation begins.
* Formation:
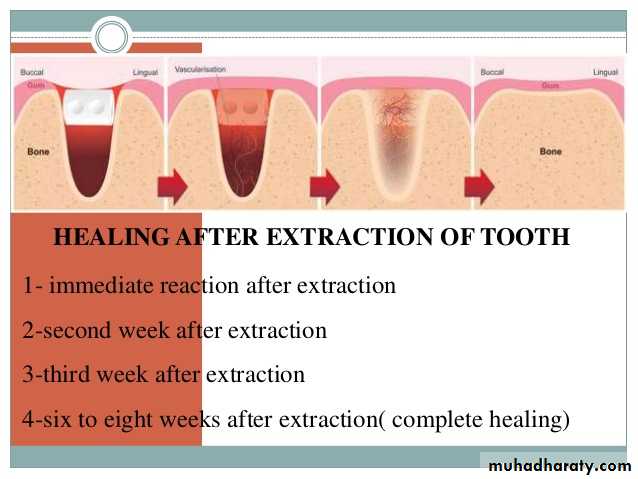
osteoblasts begin to lay down organic matrix, after 14 days osteoid begins mineralization. The site at which resorption ceases and formation begins is termed as cement line. The time involved is about 3 months in compact bone and 2 months in trabecular bone (trabecular bone turnover is of higher rate).The progression of healing after a tooth extraction goes through certain resorptive stages of:
1. Fibrin clot organization (first 4 weeks)
2. Immature (woven) bone formation (4-8 weeks)
3. Mature (lamellar) bone development (8-12 weeks)
4. Bone stabilization stage (12-16 weeks or about 4 months)
Factors Influencing Edentulous Bone Loss
• Metabolic factors:metabolic bone disease is any process that influences the normal modeling of bone. Osteopenia is a clinical term for any loss in bone density. The common metabolic bone diseases are:
1. Osteoporosis :
characterized by a reduction in the mass of bone per unit volume resulting in mechanical failure and pain, the ratio of mineral to organic matrix is usually normal.Clinical signs and symptoms of advanced osteoporosis: include
• pain in the spine.
• loss of height and/or thoracic kyphosis due to vertebral compression .
• fractures due to secondary trauma.
in most cases serum and urine biochemical examinations are normal. Osteoporosis seen in senile osteoporosis, postmenopausal osteoporosis, hyperparathyroidism and Cushing syndrome.
2. Osteomalacia:
is any disease in which excess osteoid is not mineralized and impaired bone healing is present. Osteomalacia seen in vitamin D deficiency, malnutrition, renal osteodystrophy, secondary hyperparathyroidism and drug therapy (chronic corticosteroid therapy, chronic heparin therapy, anticonvulsant therapy, alcohol).
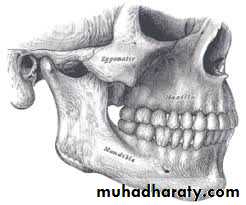
B. Anatomic factors:
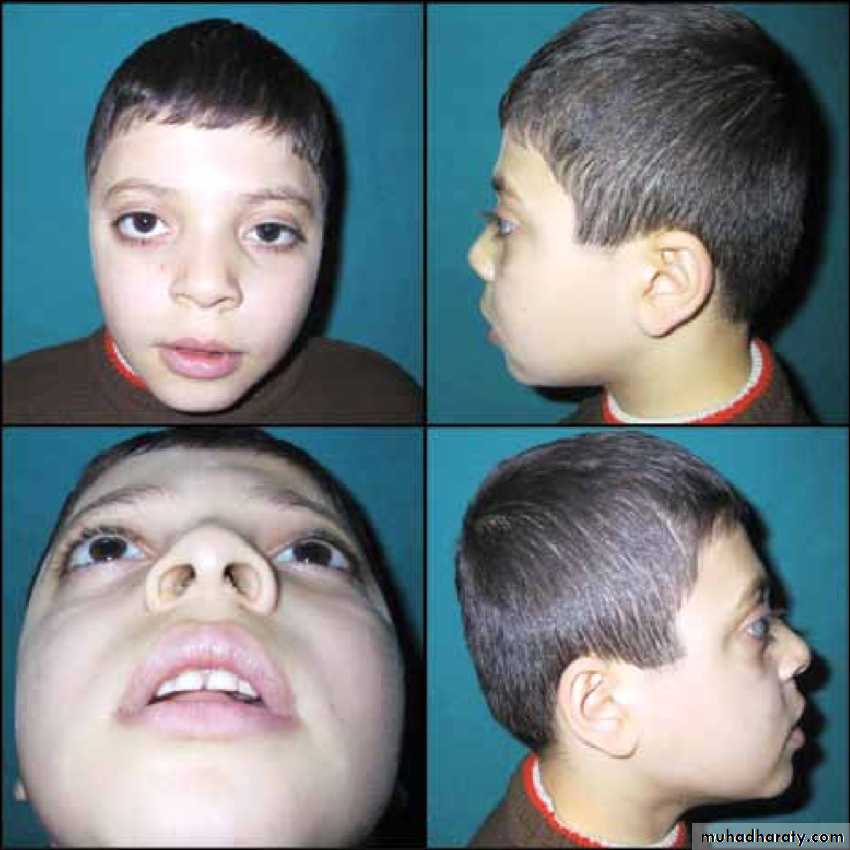
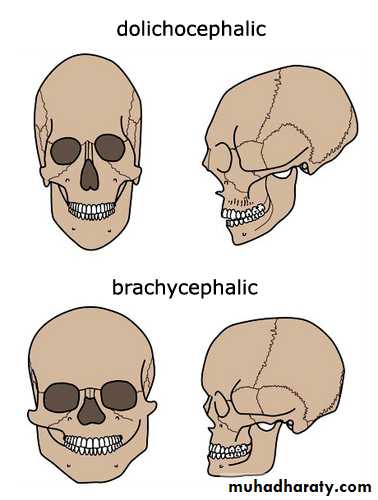
1. Facial morphology peoples with long faces (dolichocephalic) have more voluminous anterior alveolar ridge than those with short faces (brachycephalic) Brachycephalic faces (low mandibular plane angle and gonial angle) are capable of higher biting forces in both anterior and posterior regions, there is a direct correlation between short facial heights and edentulous bone loss.dolichocephalic
brachycephalic
2. Trauma and alveolectomy technique maximum conservation of bone should be practiced during extraction and management of the trauma patients.
C. Mechanical factors:
1. Disuse atrophy plays a role in the low-turnover type of remodeling.2. Excessive loading may contribute to high-turnover type of remodeling.
In bone loss secondary to the influence of dentures, the denture-bearing area of the maxilla is 1.8 times than that of the mandible. Therefore, compression (in pound/inch2) are greater on the mandible resulting in increased bone loss which is 4 times that of the maxilla, in this situation edentulous bone loss can be reduced through decreasing occlusal contact area and balancing the occlusion during occlusal arrangement of dentures.
3. Parafunctional activity (clenching & bruxism) contact during mastication occupies less than 15 minutes/day, whereas the teeth may be forcibly held together several hours/day in these activities, however the effects are not clearly understood.
Classification
Babbush 1985 classified implants according to the site into 4 types:1. Mucosal Inserts:
are composed of 2 parts the retentive base, which is placed into a prepared site in the prosthesis, and the vertical component (buttons), which enters the soft tissue receptor site in the oral mucosa. They were indicated in cases of severe atrophy of the alveolar ridge in maxilla that not permit the use of endosseous implant due to the presence of anatomical limitations which are the maxillary sinus and the nasal cavity.
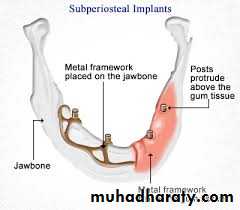
2. Subperiosteal Implant:
Was firstly introduced and performed in 1949. The design consist of 2 parts substructure which is a metallic framework that rests on bone under the periosteum, and superstructure which are abutment posts connected to the framework and penetrate the mucoperiosteum protruding in the oral cavity.3. Transmandibular Staple Bone Implant:
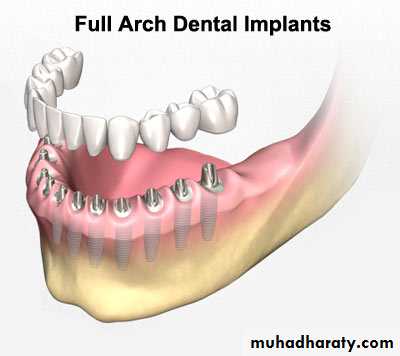
it is placed into the anterior portion of the edentulous mandible. The purpose of this implant is to act as a stabilizer and fastener for mandibular full denture. It is mainly indicated for edentulous mandible with minimal alveolar ridge height of 8-9 mm.Endosseous Implants
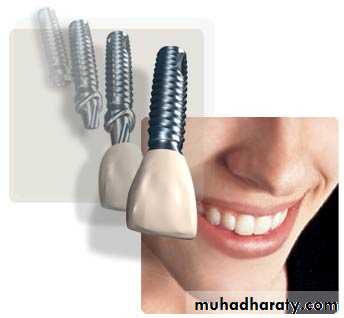
4. Endosseous Implants:History in 1950s and 1960s Linkow developed the blade implants, the mandibular staple implant developed by Small 1966- In 1951 Branemark began research leading to the development of an endosseous implant system that popularized the concept of osseointegration.
types of endosseous implants:
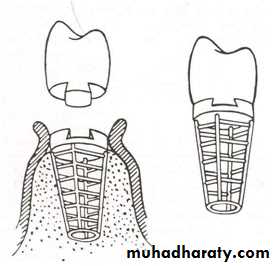
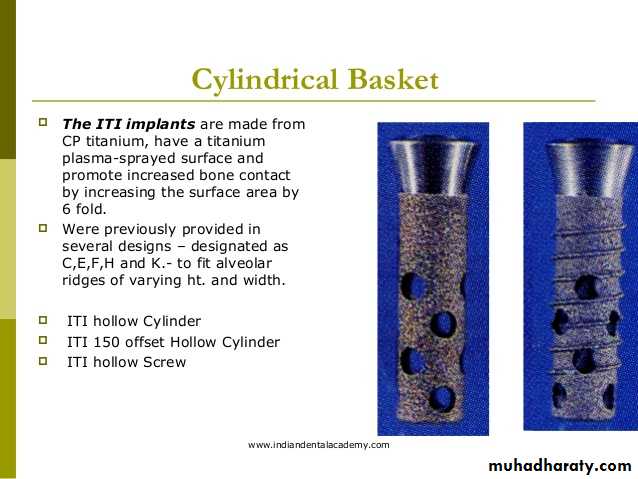
1. blade-vent implants: firstly introduced by Linkow 1967.2. hollow-basket implant system (C.E, H, K or F)
3. Screws and other implant systems: such as TPS-Screw (Titanium plasma-sprayed screw system). Vitreous Carbon Implant, Tubingen Aluminum Ceramic, TPC Implant (Tetracalcium Phosphate), IMZ Implant Branemark Osseointegrated Titanium Implant etc.
Advantages of the screws over Subperiosteal and Stanle implants:
1. Screws can be inserted under local anesthesia through a relatively small mucoperiosteal incision.2. Can be placed against opposing natural teeth with less risk than other implants.
3. Permits final restoration of the case immediately or after few days.
4.In case of failure the screw can be easily removed and replaced without endangering the adjacent screws or without loss of the prosthesis.
5. Relative simplicity of the superstructure.
6. Can be used as support for Cranio-Facial prosthesis that applied in cases of craniofacial deformities (auricle, nose, orbit, maxilla and mandible).
7. Can be applied for treatment of some orthodontic problems such as correction of simple cross-bite.
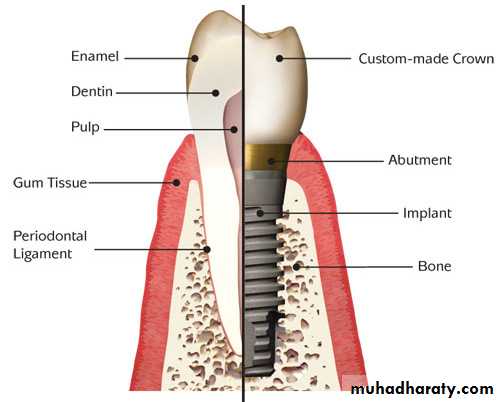
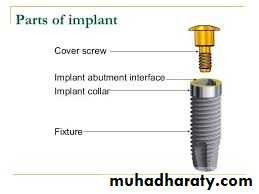
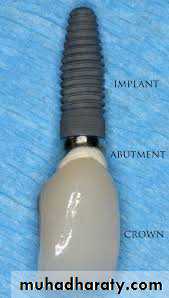
Parts of Dental lmplant:
Fixture (DI): consist of 3 parts - crest module, body and apexCover screw: which is placed into the top of the implant, in first stage surgery.
Permucosal extension (healing abutment, gingival former): is the transepithelial portion which extends above the soft tissue and results in the development of a permucosal seal around the implant.
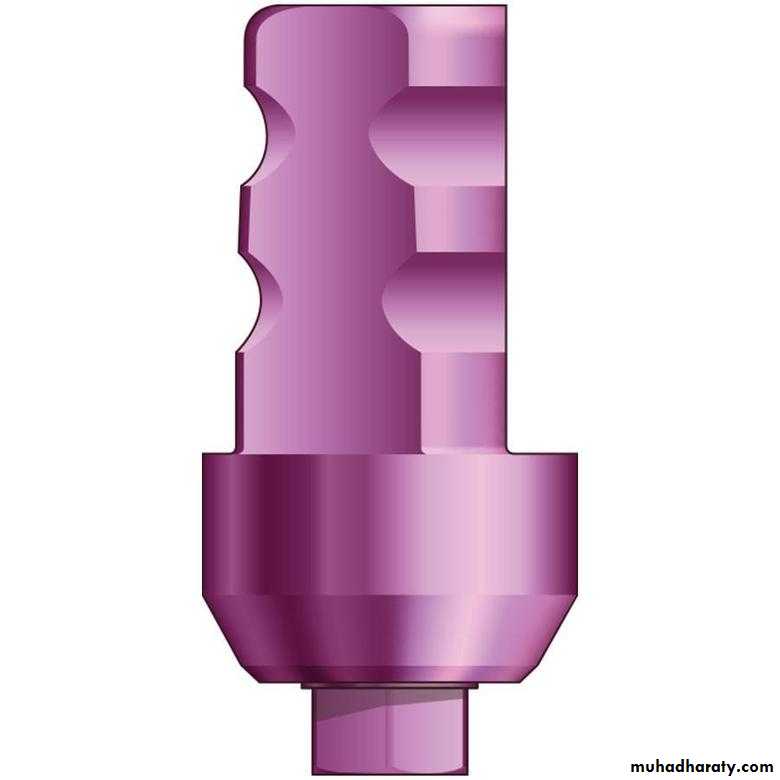
Abutment: is the portion of the implant that supports or retains a prosthesis or implant superstructure.
fixture
Gingival former
Cover screw
AbutmentTransfer coping: the component used to transfer the position and the design of the implant or the abutment to the master cast for prosthesis fabrication. It is either indirect transfer coping used in closed tray impression or direct used in open tray impression.
Analog: used in the fabrication of the master cast to replicate the retentive portion of the implant body or abutment (implant body analog, implant abutment analog).
Transfer coping
AnalogTissue Reactions to Implants
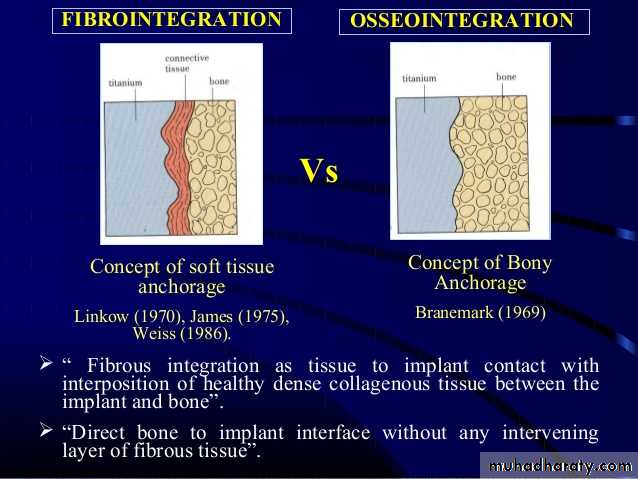
1. Ankylosis: or direct apposition of bone to the implant which is accepted as the most desirable alternative to true periodontal attachment and can provide effective load transmission.2. Fibrous encapsulation: fibrous capsule around implants are associated with numerous factors including implant mobility, shape and toxicity.
3. Epithelial down growth: has been observed around both endosseous and subperiosteal implants which cause brealk down of the bond between the implant and the surrounding bone.
1
2
3
Factors Influencing Tissue Behavior:
1. Site preparation: it is important to avoid overheating when placing the implant which may lead to osteonecrosis or delayed bone regeneration and replacement by fibrous connective tissue.
2. Implant material: the material from which an implant is made has a profound effect on the type of tissue which forms around it and the stability of the implant- tissue interface.
There are 3 basic types of interaction between host and implant:
A. Bio-tolerance where there is a mild reaction to the implant, as seen around stainless steel.B. Bio-inertness where the implant is ignored, as seen around vitreous carbon.
C. Bio-activity where the implant interacts chemically with the body in a controlled fashion so as to become incorporated into the tissues.
3. Implant design: there is a little evidence that variations in implant surface texture at a microscopic level influence the subsequent tissue response implants with sharp corners elicit a fibrous reaction, and there is evidence that implant shape in the cervical region can also influence pattern of bone behavior
Osseo integration
Osseointegration
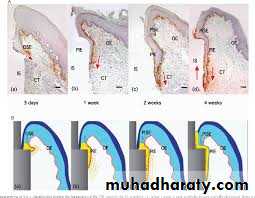
According to Branemark 1982 it was defined as: a "direct structural and functional connection between living bone and a load carrying endosseous implant at the light microscopic level"Initial stability and successive remodeling of bone tissue depend on:
1. Gentle surgical technique2. Controlled application of functional load
In spite of the widespread use of titanium implants, little is known about the events taking place in the tissue at different times after insertion (hypothesis)
1. A general concept appears to be that the implant surface serves to support osteogenic cells, thus providing favorable conditions for bone formation leading to osseointegration.
2. Titanium oxide forming the surface of the implant has certain properties favorable for mineralization (bind with calcium which might be beneficial for bone formation).
Types of Stability:
1. Primary stability is largely a mechanical parameter, a function of bone quantity & quality.2. Secondary stability viewed as increased stability (biological) after placement.
Factors Control (affecting) Osseointegration:
A- Surgical factor: primary stability and surgical techniqueB- Tissue factor : bone quality & quantity, healing, remodeling
C-Implant factor: macrostructure (implant design and surface treatment), microstructure and dimensions
D- Occlusal/Mechanical factor: forces (loading) & prosthetic design
Measurement of Osseointegration:
1. Tensional test (lateral load)2. Push-out/Pull-out test (only for non-threaded cylinder Dl)
3. Percussion test (subjective)
4. Insertion torque
5. Removal torque (reverse)
6. Thread cutting force
7. Perio test (1986)
8. Resonance Frequency Analysis 1998 (0sstell )
9. Radiographic evaluation (difficult to perceive changes in bone structure & morphology of bone-implant interface unless over 30% bone loss occur)
10. Histology & Histomorphometry (non-clinical studies & experiments)
Surface Characteristics of Titanium Implants:
For most metal surfaces (except those of the noble metals) exposed to air or other oxidizing media, this results in the formation of a thin surface oxide (10 nm in thickness). The composition of surface oxide is in most cases Titanium oxide. The surface of Titanium implants prior to implantation consist of a thin surface oxide which is covered by a hydrocarbon-dominated contamination layer.Roughness at implant surface can be modified by
1. Sandblasting the surface is bombarded by fast hard particles in order to remove gross surface defects and contamination.2. Plasma spraying in which the surface is coated by spraying molten drops of metal onto the surface at a high velocity.
Clinical and Radiological Assessment for Dental Implants
Clinical :A. History
1. Patient's complaints and expectations:
a. Elicit the patient chief complaints
b. Major concerns
c. Treatment requests
2. Medical:
a. The general health status
b. Contraindications: Absolute V/S Relative
- Implants are not recommended for elderly infirm persons
- Drug or alcohol dependence, uncontrolled depression and those with some psychiatric disorders
- Heart failure, uncontrolled diabetes and blood dyscrasias,
immunocompromised
- Heavy smokers, irradiation of the face and jaws, osteoporosis in the oral
region, parafunctional habits
- Unfinished cranial growth and teeth eruption
3. Dental History:
a. Cause of teeth lossb. Compliance
4. Social History
B. Examination:
1. Extraoral
a. Facial proportions
b. Mouth opening
C. Jaw relationship
d. Morphology and function of the lips
e. Facial muscles hypertrophy
2. Intraoral
a. Oral hygiene assessment
b. Condition of the remaining dentition
c. Palpation of the alveolar ridge at the prospective implant sites
d. Space analysis of edentulous areas:
- Height, Width, and Length (Inter-coronal distance) -, Osteometer (bone caliper), alveolar ridge mapping
- Inter-arch distance
- Thickness of the soft tissue
RADIOLOGICAL:
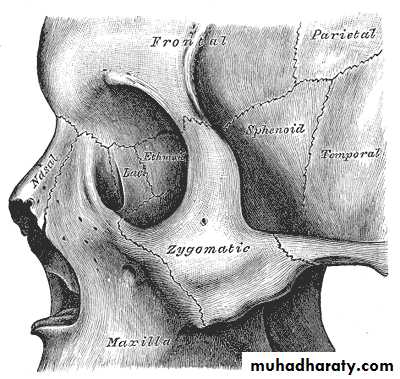
Radiographic Presurgical Assessment of Endosseous Implants; the specific imaging objectives for implant surgery are:1. Jaw Size (height & width) the horizontal and vertical dimensions of the alveolar and basal bone are important for treatment planning and implant retention. The larger and denser alveolar ridge the better the long-term success for implant integration.
It is ideal to have at least 1 mm of bone on all sides of the implant and therefore the cross- sectional dimension of the alveolar ridge should be at least 6 mm. Implants that have bicortical anchorage are more successful than those that are suspended in trabecular bone. Therefore, determination of the implant length is necessary to allow for engagement of the terminal end in cortical bone.
2. Orientation of the Vertical Long Axis of the Jaw The axis orientation can be determined only with cross-sectional imaging techniques.
3. Jaw Boundaries the buccal and lingual walls of the maxilla and mandible are not always parallel, the canine fosse on the buccal surface of the anterior maxilla and the submandibular fossa on the lingual surface of the mandible arc common normal anatomic depressions.
4. Internal Anatomy to reveal the location of neurovascular structures, cortices, sinuses, nasal fossae and nasopalatine duct.
5. Soft-tissue Morphology it is important to determine the thickness of the soft tissues overlying the alveolar ridge for accurate determination of the location and alignment of the prosthetic element that attached to the implant.
6. Three -dimensional Spatial Localization 2 planes perpendicular to each other (longitudinal and cross-sectional images), this allow localization of relevant anatomic structures.
7. Pathology Detection any disease process or abnormal condition may diminish the probability of successful implant placement and retention (root tips, inflammatory processes, cysts and tumors).
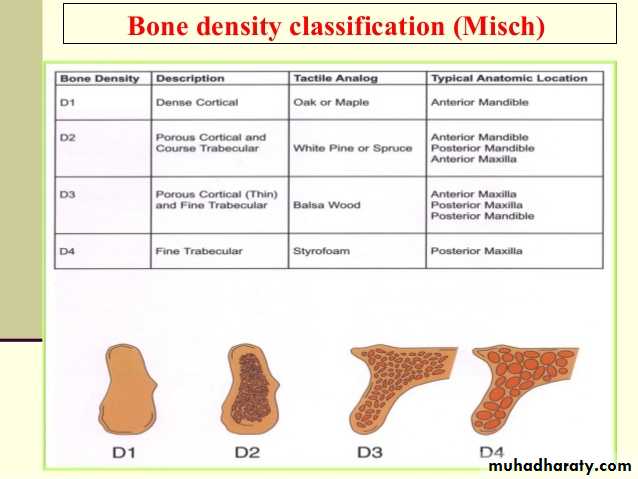
8. Bone Quality the amount of mineralized bone/ unit area at implant site affect the success of implant integration ,maxillary tuberosity is a poor implant site because of the porosity of trabeculated bone).
Imaging Modalities
A. Conventional Imaging:1.Panoramic Projections provide information about the vertical height of the mandible and location of the mental foramina.
2.Cephalometric Projections lateral Cephalometric provide information about the cross-sectional dimensions of the mandible The main disadvantage is the significant Superimposition.
3. Periapical projections produce excellent anatomic detail and information related to bone quality, but it 1) does not provide information about cross-sectional anatomy of the jaws, 2) nor does it demonstrate all regions of the law, 3) relatively high radiation dose per image
4. occlusal projections the same to periapical but demonstrates larger areas. This image can evaluate 1) curve of the jaws 2) bone quality 3) largest buccolingual dimensions of the mandible,
5. Tomographic projections It I is an imaging technique that provides an image of a tissue plane or layer. The main disadvantage due to this single image plane is blurred image.
B. Digital Imaging:
I. Computed Tomography CT produce image with contrast sensitivity much greater than that of images produced by conventional methods, the images are superior because there is no superimposition. The main disadvantage is the high radiation dose and cost.2. Cone Beam Computed Tomography CBCT less dose than CT. CBCT give 3:dimensional images, and applied when cross-sectional images required.
3. Intraoral Detectors allow direct digital capture and display of intraoral images on a video monitor
Bone Density (bone volume, bone quantity)
There are various conditions of residual ridge depending on history and duration of edentulous. A tooth loss due to advanced periodontal disease lead to rapid resorption to the apex 13-15 mm, while a tooth loss due to apical ostietis or trauma may preserve the alveolar process for longer period of time.In infra-foraminal region there is a visible angle between the axial inclination of the teeth/alveolar process and the basal bone, this angle must be taken into account in order to prevent perforation of the lingual cortical bone and possible trauma to lingual artery.
A ridge width of at least 6 mm is necessary for placing implant of a 3.5 mm diameter. A good evaluation of bone density allows the surgeon to do the following:
1. Select the proper implant diameter.
2. Decide about the optimal drilling sequence, in soft bone use of final drill half depth only with minimal use of countersink and use of smaller drill diameter than standard, while in hard (dense) bone use of oversized drill diameters.
3. Determine the length of healing period.
4. Evaluate occlusal loading capacity of different implants.
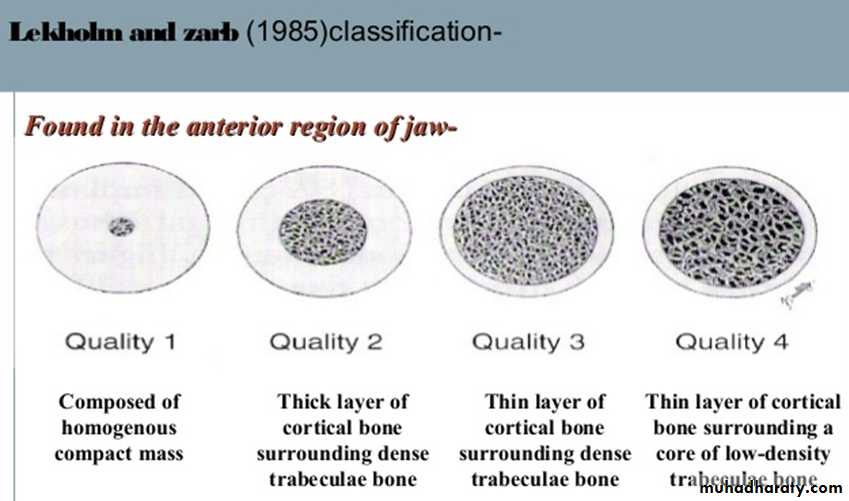
Classification of bone density (Lekholms & Zarb)
1. Type I essentially cortical bone2. Type II dense cortico-cancellous bone
3. Type III sparse cortico-cancellous bone
4. Type IV thin cortical bone and very sparse medullary bone
Bone Quality (Structure)
Classification of bone quality from biological point of view (BHP bone healing potential):1. BHP1 bone with normal bone healing
2. BHP 2 bone with moderately reduced healing potential (as in moderate smoking 10 Cigarette / day, controlled diabetes mellitus, long-term corticosteroid treatment, regenerated bone, long-term non-steroidal anti-inflammatory agents I like indomethacin).
3. BHP3 bone with substantially reduced healing potential (heavy smoing 20 cigarettes or more/ day, diabetes mellitus, severe anemia, Gauchers disease, severe osteoporosis, Paget's disease, fibrous dysplasia, hyperparathyroidism, thalassemia, irradiated bone, rheumatoid arthritis and antimitotic drugs).
SURGICAL TECHNIQUE:
Preparation of surgical feildApproach:
Flapped ApproachFlapless Approach (minimally invasive approach)
Flapped Approach:
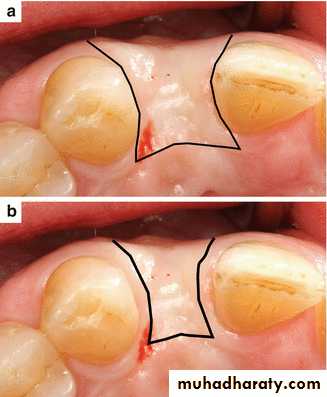
1. Extensive flap design (conventional three or two-sided)
2. Envelope flap
3. Conserved flap (limited flap design, papilla-saving incision)
1
2
3
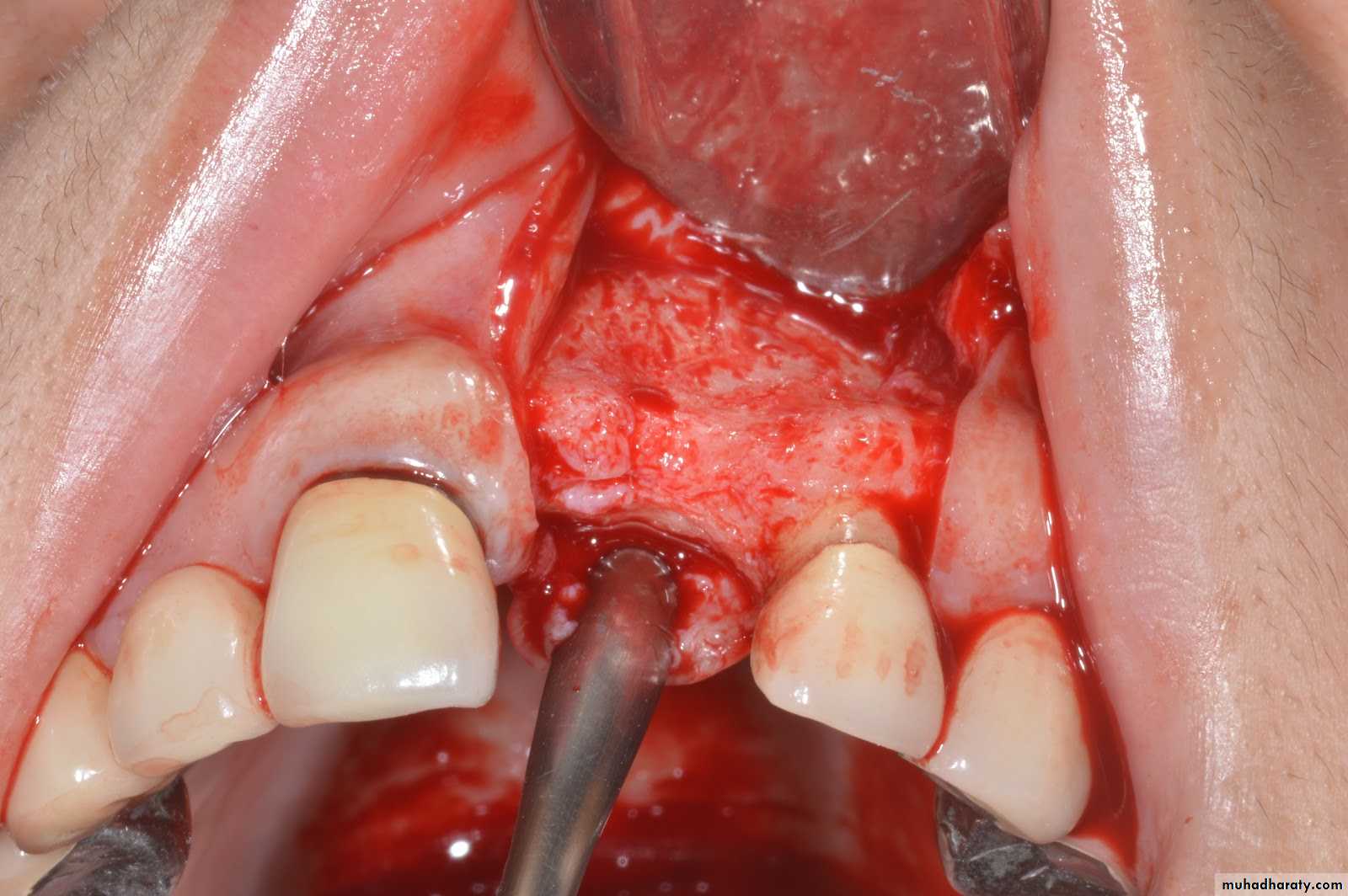
Preparation of implant site:
The implant fixtures are installed into a carefully made recipient site (osteotomy site) in the jaw bones created by:Bone drilling technique
Bone expanders and condensers (screws or osteotomes)
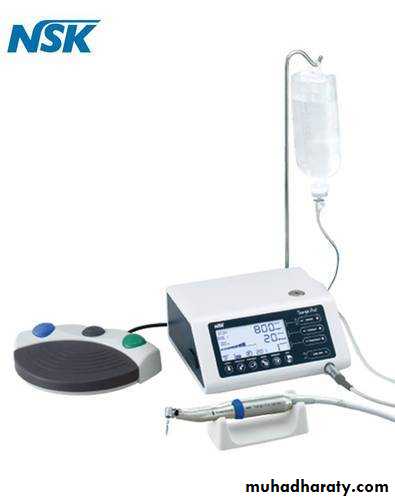
Bone drilling technique:
Atraumatic preparation and removal of bone from the recipient site must be accomplished with minimal violence. Heat production during bone preparation is a critical factor, a maximum temperature of 47 C for 1 minute is commonly quoted as a threshold temperature In order to avoid an irreversible bone damage that can lead to failure of osseointergartion, use:A low-speed (600-1000 rpm)
High-torque hand-piece
Intermittent drilling technique allow the irrigant to reach the depth of the preparation and allow the bone chips to be removed and to prevent the heat buildup
Sharp drills
Copious saline irrigation (external, internal, manual )
Procedure:
Posterior maxillary regionAnterior mandibular region
Posterior mandibular region
1.5
1.5
3mm
Exposure Procedure
The procedure selected to expose the implants (after the healing period usually 3-6 months) will depend on the esthetic and functional requirement. There are 3 basic soft tissue procedures for exposing the implant:1. Coring out the mucosa overlying the implant.
2. Elevation of facial flaps with some slight release of the lingual and palatal mucosa.
3. Mobilizing and moving of facial &/or lingual flaps with or without mucosal or skin grafting
Various treatment options devised over the years for inadequate ridge width are:
1.Increase width by osteoplasty2.utilize narrower diameter implants
4.Bone expansion
5.Ridge splitting
3. Increase width by augmentation
6. Horizontal distraction osteogenesis
Treatment Protocols (Treatment Sequence)
The timing of implant placement falls into 3 categories:
A. Delayed Placement (late implant placement, traditional protocol) in which delay placement until an extraction site was completely filled with bone (6 month or longer). A covered non loaded healing phase requiring a stress-free Ol period of approximately 4 months. Edentulous patients have also been required to go out their removable prosthesis for the 1st 2 weeks after implant placement.
Healing Phase: Today 3 - 6 months non-loaded phase for dental implants is generally accepted for safe bone apposition to implant interface. The resulting loading periods of 3 months for the mandible and 6 months for the maxilla.
The process is influenced by
1. Biocompatibility of the implant material2. Implant surface structure
3. The application of atraumatic surgical protocol
4.Prevention of micro-movement at the interface
B. Immediate Placement : placing the implant at the same time as tooth extraction. The advantage preserve more residual alveolar bone .also the time between extraction and implant placement will be significantly reduced. This technique is most often used when multiple teeth to be extracted /or primary soft-tissue closure can easily be achieved (usually in anterior mandible or maxilla).
Contraindications:
1. Bony or soft tissue infection2. Inadequate bone apical to extraction site for implant stabilization
3. Chronic problems such as granuloma or radicular cyst
Technique. once the tooth is removed as a traumatically as possible, intra-bony soft tissue should be carefully excavated (periodontal ligament C.T. & epithelial remnants may interfere with implant integration process, extracted tooth can be used as a template for implant selection and preparation size, the tooth root can be a very helpful guide to implant length by measuring root length + length of available bone apical to the tooth socket. To fill the void between portion of the implant and the wall of alveolus, autogenous, allogeneic or xenografting materials may be used with same success, this may:
1. Minimize soft-tissue ingrowth
2. Improve bony apposition3. Aid in alveolar bone preservation.
When primary closure cannot obtained a:
1. Collagen material such as collagen can be considered over the graft2. Barrier membrane
C. semi-immediate Placement : placement of implant is delayed until the mucosa has regenerated over the socket. This frequently occurs when one or two teeth are lost adjacent to natural teeth this require 2 months of epithelial healing and maturation. There will be some bone resorption which make necessary to position the implant slightly more apically (additional depth of 1-2 mm is usually adequate).
complications of Dental Implants:
A-Intraoperative:1. Poorly positioned Implant
2. Damage to mucosa and adjacent teeth
3. Damage to bone ( lateral perforation, alveolar bone fracture or jaw fracture)
4. Perforation into adjacent areas ( lower border of the mandible, nasal cavity or maxillary antrum)
5. Damage to nerves
6. Loose implant (poor primary stability7. Contamination of implant and bone during surgery
8. Damage to the implant ( crossed threads or surface defect)
9. Hemorrhage during surgery ( especially in the anterior mandible and possible airway compromise)
B- Postoperative:
1. Pain
2. Swelling
3. Reactionary or secondary hemorrhage
4. Infection of implant soft tissue or bone ( peri-implant mucositis or peri-implantitis)
5. Exposed or loose cover screw ( healing screvw)
C- Late:
1. Mucosal recession2. Bone resorption
3. Mobility
4. Implant fracture
Criteria for Success
The term implant success may be used to describe ideal clinical conditions. It should include a time period of at least 12 months for implant serving an implant as prosthetic abutments. Implant success is suggested for a span of:1-3 years early implant success
3-7 years intermediate implant success
More than 7 years long-term implant success
The primary function of a DI is to act as an abutment for a prosthetic device, similar to a natural tooth root and crown. Any success criteria, therefore, must include first and foremost support of a functional prosthesis. Assessment of failure according to the time when occurred:
(1) Early failures or failures during the osseointegration period (usually within the first year after an implant insertion, during the healing period and initial loading)
(2) Late failures or failures after the osseointegration period (usually about a year after implant insertion, when an osseointegration process is complete and implant function is established).
Causes of early implant failures:
1. Poor quality and quantity of bone and soft tissue2. Patient medical condition
3. Unfavorable patient habits (bruxism, heavy long-term smoking, poor oral hygiene, others)
4. Inadequate surgical analysis and technique
5. Inadequate prosthetic analysis and technique
6. Suboptimal implant design and surface characteristics
7. Implant position or location (functional implant zones)
8. Unknown factors