Medicaments used in the treatment ofPeriodontal Diseases
Dr. Handren Hunar Najeeb1
Definitions
An anti-infective agent is a chemotherapeutic agent that acts by reducing the number of bacteria present.An antibiotic is a naturally occurring, semisynthetic, or synthetic type of anti-infective agent that destroys or inhibits the growth of select microorganisms, generally at low concentrations.
An antiseptic is a chemical antimicrobial agent that can be applied topically or subgingivally to mucous membranes, wounds, or intact dermal surfaces to destroy microorganisms and inhibit their reproduction or metabolism.
2
In dentistry, antiseptics are widely used as the active ingredient in antiplaque and antigingivitis oral rinses and dentifrices.
Disinfectants (a subcategory of antiseptics) are antimicrobial agents that are generally applied to inanimate surfaces to destroy microorganisms.
3
When anti-infective agents are administered orally, many of these agents can be found in the gingival crevicular fluid (GCF).
this reduce the number of bacteria present in the diseased periodontal pocket; this is often a necessary because bacteria can invade periodontal tissues, thereby making mechanical therapy alone sometimes ineffective.
4
A single chemotherapeutic agent can also have a dual mechanism of action.
• For example, tetracyclines ( especially doxycycline ) are chemotherapeutic agents that can reduce collagen and bone destruction via their ability to inhibit the enzyme collagenase.
5
Systemic Administration of Antibiotics
Background and RationaleThe treatment of periodontal diseases is based on their infectious nature
Ideally, the causative microorganisms should be identified, and the most effective agent should be selected with the use of antibiotic-sensitivity testing.
this appears simple, but the difficulty lies primarily in identifying the specific etiologic microorganisms
6
Antibiotics Used to Treat Periodontal Diseases
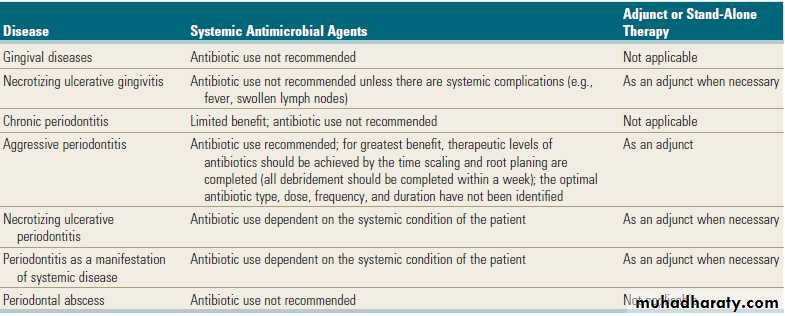
• Indications: localized aggressive periodontitis, generalized aggressive periodontitis, medically related periodontitis, and refractory periodontitis.
• Amoxicillin and clavulanate potassium.
• Indications: localized aggressive periodontitis, generalized aggressive periodontitis, medically related periodontitis, refractory periodontitis, and necrotizing ulcerative periodontitis.
7
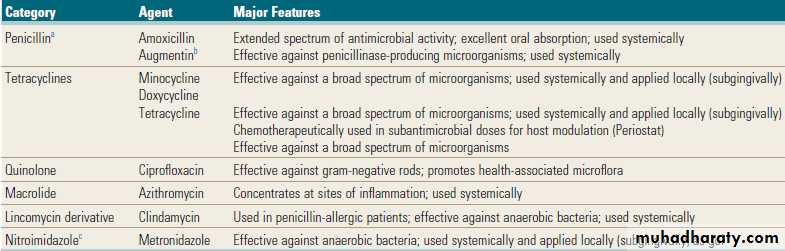
Antibiotics Used to Treat Periodontal Diseases
CategoryAgent
Major Features
Penicillin a
Amoxicillin
Augmentin b
Extended spectrum of antimicrobial activity; excellent oral absorption; used systemically
Effective against penicillinase-producing microorganisms; used systemically
Tetracyclines
Minocycline
Doxycycline
Tetracycline
Effective against a broad spectrum of microorganisms; used systemically and applied locally (subgingivally)
Effective against a broad spectrum of microorganisms; used systemically and applied locally (subgingivally)
Chemotherapeutically used in subantimicrobial doses for host modulation (Periostat)
Effective against a broad spectrum of microorganisms
Quinolone
Ciprofloxacin
Effective against gram-negative rods; promotes health-associated microflora
Macrolide
Azithromycin
Concentrates at sites of inflammation; used systemically
Lincomycin derivative
Clindamycin
Used in penicillin-allergic patients; effective against anaerobic bacteria; used systemically
Nitroimidazolec
Metronidazole
Effective against anaerobic bacteria; used systemically and applied locally (subgingivally) as gel
8
Systemic Administration of Antibiotics
An ideal antibiotic for use in the prevention and treatment of periodontal disease should be:
specific for periodontal pathogens,
nontoxic,
substantive,
not in general use for the treatment of other diseases,
inexpensive.
Currently, an ideal antibiotic for the treatment of periodontal disease does not exist.
a combination of antibiotics may be necessary to eliminate all putative pathogens from some periodontal pockets
9
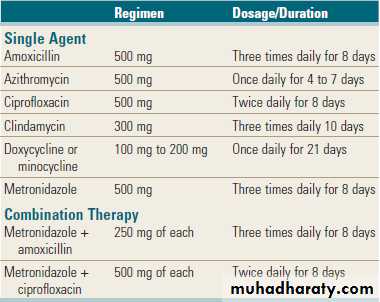
Common Antibiotic Regimens Used to Treat Periodontal Diseases
• These regimens are prescribed after a review of the patient’s medical history, periodontal diagnosis, and antimicrobial testing. Clinicians must consult pharmacology references or the manufacturer’s guidelines for warnings, contraindications, and precautions.
10
Systemic Administration of Antibiotics
Patient dentist communicationAs always, the clinician, in concert with the patient, must make the final decision regarding any treatment.
the nature of the colonizing bacteria, the ability of the agent to reach the site of infection, and the risks and benefits associated with the proposed treatment plan.
Some adverse reactions include allergic or anaphylactic reactions, superinfections of opportunistic bacteria, development of resistant bacteria, interactions with other medications, upset stomach, nausea, and vomiting. Most adverse reactions take the form of gastrointestinal upset.
Other concerns include the cost of the medication and the patient’s willingness and ability to comply with the proposed therapy.
11
Chemotherapeutic agents
Tetracyclines(Minocycline , Doxycycline, Tetracycline)
Metronidazole
Penicillins (Penicillin, Amoxicilline, Augmentin)
Clindamycin
Ciprofloxacin
Macrolides
12
Tetracyclines
Tetracyclines have the ability to concentrate in the periodontal tissues and inhibit the growth of Aggregatibacter actinomycetemcomitans, their concentration in the gingival crevice is 2 to 10 times that found in serum.Tetracyclines exert an anticollagenase effect that can inhibit tissue destruction and may help with bone regeneration.
These antibiotics are bacteriostatic and are effective against rapidly multiplying bacteria.
13
Tetracyclines
Tetracyclines have been used for the treatment of LAP, A. actinomycetemcomitans is a microorganism that is frequently associated with LAP, and it invades tissue. Therefore the mechanical removal of calculus and plaque from root surfaces may not eliminate this bacterium from the periodontal tissues.14
Tetracyclines
Side effects include:
gastrointestinal disturbances,
photosensitivity,
hypersensitivity,
increased blood urea nitrogen levels,
blood dyscrasias,
dizziness,
headache.
In addition, tooth discoloration occurs when this drug is administered to children who are 12 years old or younger.
15
Preoperative radiograph of anterior mandible in localized aggressive periodontitis patient.
Postoperative radiograph of anterior mandible in localized aggressive periodontitis patient treated with a combination of antibiotic therapy, scaling and root planing, and surgical intervention.
16
Tetracyclines
Specific Agents
• Tetracycline.(250 mg four times daily)
• minocycline. (200 mg/day)
• Doxycycline.(100 mg twice daily the first day, which is then reduced to 100 mg daily).
These are semisynthetic members of the tetracycline group that have been used in periodontal therapy.
17
Metronidazole
It is bactericidal to anaerobic organisms.Effective against P. gingivalis & P. intermedia.
Metronidazole is not the drug of choice for treating A. actinomycetemcomitans infections. However, metronidazole is effective against A. actinomycetemcomitans when used in combination with other antibiotics.
Metronidazole has been used clinically to treat acute necrotizing ulcerative gingivitis, chronic periodontitis, and aggressive periodontitis.
18
Metronidazole
Dosage/DurationThe most common regimen is 250 mg 3 times daily for 7 days.
Side Effects
Metronidazole inhibits warfarin metabolism.
produces a metallic taste in the mouth
19
Penicillins
Inhibit bacterial cell wall production and therefore are bactericidal.TYPES:
Amoxicillin
Amoxicillin–Clavulanate Potassium (Augmentin)
Side Effects
Penicillins may induce
• allergic reactions and
• bacterial resistance.
20
Amoxicillin
Amoxicillin is a semisynthetic penicillin with an extended anti-infective spectrum that includes gram-positive and gram-negative bacteria.May be useful for the management of patients with aggressive periodontitis in both localized and generalized forms.
The recommended dosage is 500 mg 3 times daily for 8 days.
Side Effects: susceptible to penicillinase
21
Amoxicillin–Clavulanate Potassium
The combination of amoxicillin with clavulanate potassium makes this anti-infective agent resistant to penicillinase enzymes produced by some bacteria.
may be useful for the management of patients with LAP or refractory periodontitis.
The recommended dosage
625 mg 3 times daily for 8 days.
22
Clindamycin
Clindamycin is effective against anaerobic bacteria and has a strong affinity for osseous tissue.Clinical Use
Clindamycin has demonstrated efficacy in patients with periodontitis that is refractory to tetracycline therapy.
the dosage: 150 mg 4 times daily for 10 days.
Side Effects
associated with pseudomembranous colitis.
Diarrhea or cramping.
23
Ciprofloxacin
active against gram-negative rods,ciprofloxacin therapy may facilitate the establishment of a microflora that is associated with periodontal health.
Side Effects
Nausea, headache, metallic taste in the mouth, and abdominal discomfort, enhance the effects of warfarin and other anticoagulants
24
Macrolides
Macrolides can be bacteriostatic or bactericidal, depending on the concentration of the drug and the nature of the microorganism.
Include:
erythromycin.
spiramycin.
azithromycin.
25
Macrolides
Erythromycin does not concentrate in GCF and is not effective against most putative periodontal pathogens. For these reasons, erythromycin is not recommended as an adjunct to periodontal therapy.Spiramycin is active against gram-positive organisms; it is excreted in high concentrations in saliva.
26
Macrolides
Azithromycin is effective against anaerobes and gram-negative bacilli.The concentration of azithromycin in tissue specimens from periodontal lesions is significantly higher than that of normal gingiva.
Therapeutic use requires a single dose of 250 mg/day for 5 days after an initial loading dose of 500 mg.
27
Macrolides
US Food and Drug Administration issued a warning that Azithromycin can alter the electrical activity of the heart, which may lead to a potentially fatal heart rhythm.28
Serial and Combination Antibiotic Therapy
Because periodontal infections may contain a wide variety of bacteria, no single antibiotic is effective against all putative pathogens, it may be necessary to use more than one antibiotic, either serially or in combination
Antibiotics that are bacteriostatic (e.g., tetracycline) generally require rapidly dividing microorganisms to be effective. They do not function well if a bactericidal antibiotic (e.g., amoxicillin) is given concurrently.
29
The metronidazole–amoxicillin and metronidazole–Augmentin combinations provided excellent elimination of many organisms in adults with LAP who had been treated unsuccessfully with tetracyclines and mechanical debridement.
The metronidazole–ciprofloxacin combination is effective against A. actinomycetemcomitans; metronidazole targets obligate anaerobes, and ciprofloxacin targets facultative anaerobes.
30
Therapeutic Uses of Systemic Antimicrobial Agents for Various Periodontal Diseases
31
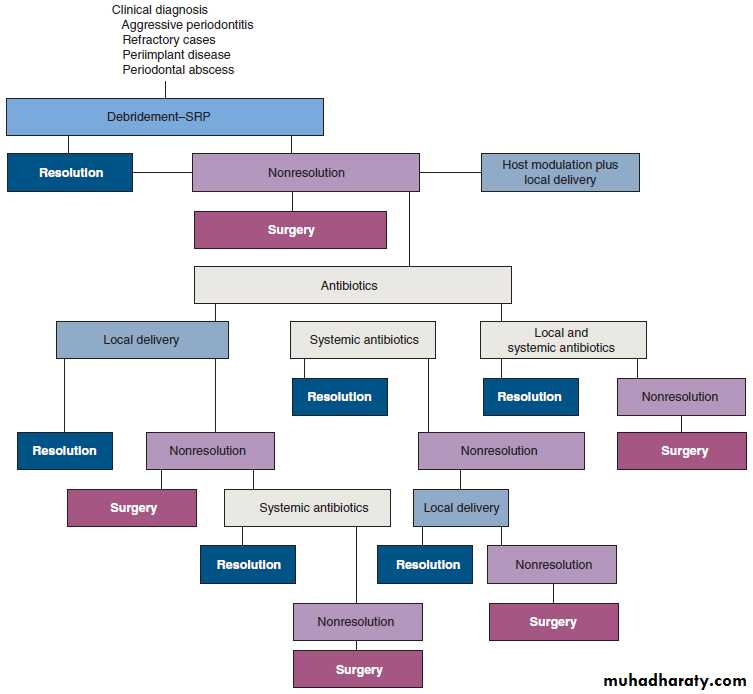
A decision tree for the selection of antibiotic therapy.
32Conclusion
Scaling and root planing alone are effective for reducing pocket depths, gaining increases in periodontal attachment levels, and decreasing inflammation levels (i.e., bleeding with probing).
When systemic antibiotics are used as adjuncts to scaling and root planing, the evidence indicates that some systemic antibiotics (e.g., metronidazole, tetracycline) provide additional improvements in attachment levels (0.35 mm for metronidazole; 0.40 mm for tetracycline) when used as adjuncts to scaling and root planing.
33