Getting Started
As anesthesiologists we recognize that passively watching a procedure does not give us the understanding or skills required to perform it.Accordingly, the more active a role you take in the anaesthetic management of the patient, the more you will get out of the rotation, in terms of understanding, sense of accomplishment, and development of technical skills.
Of all the specialties, anaesthesia is one of the few which can offer intensive one-on-one teaching, and you should try to take as much advantage of this as possible.
Monitoring
The guidelines for patient monitoring are:An anaesthetist present: "The only indispensable monitor is the presence at all times, of an appropriately trained and experienced physician.
A completed preanaesthetic checklist which ensure that you are ready when the patient arrives to the operating room.
An anaesthetic record: include
HR and BP measured at least every 5 minutes.
The time, dose, and route of all drugs and fluids should be charted.
• Oxygenation, ventilation, circulation, and temperature are continually evaluated both clinically and quantitatively. (Continual is defined as 'repeated regularly').
Intraoperative Monitoring
Non
invasive
Pulse Rate
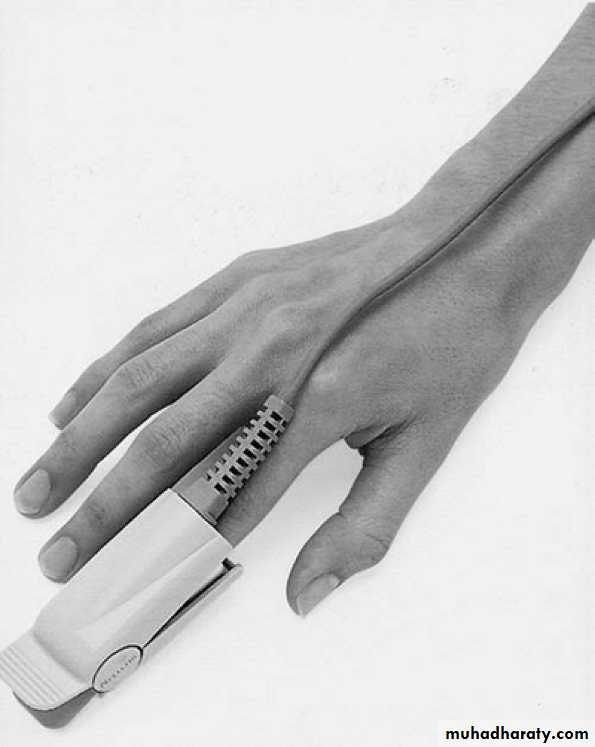
SpO2Wave
Blood volume
Pulse oximetry
Non
invasive
Ischemia
Arrhythmia
Noninvasive Blood Pressure Monitor (NIBP)
Frequent blood pressure determinations during anesthesia aid drug titration and fluid management and provide warning of conditions that could affect patient safety
Temperature monitor
EtCO2
Confirmation of tracheal intubation
Recognition of an inadvertent esophageal intubationAssessment of the adequacy of ventilation and an indirect estimate of Pa CO2
Indirect measurement of airway reactivity
(eg., bronchospasm)
Aids the recognition of a partial airway obstruction (e.g., kinked ETT)
Recognition of an inadvertent extubation or disconnection.
Aids the diagnosis of a pulmonary embolism (e.g., air or clot)
Assessment of the effect of cardiopulmonary resuscitation efforts
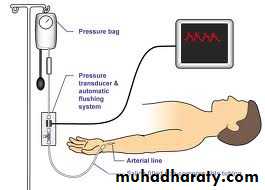
invasive
for beat-to-beat measurement of BPand
arterial blood gas sampling (ABG)
Arterial catheter
central venous catheter
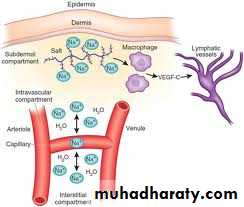
invasiveThe CVP reflects the patients' blood volume, venous tone, and right ventricular performance.
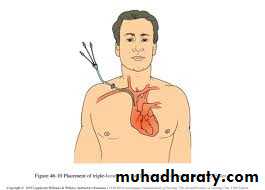
invasive
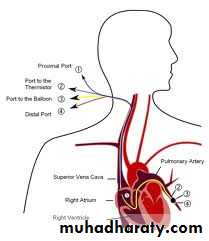
Pulmonary artery catheterfor measurement of the pulmonary artery wedge pressure (PCWP) which reflects the left atrial filling pressure
GeneralAnesthesia
General anesthesiaIt is a reversible loss of conscious with whole body (general) analgesia , element of amnesia with or without muscle relaxation.
STAGES OF
GENERAL ANESTHESIAStage I : Analgesia
From induction of anesthesia to loss of consciousness (loss of eyelid reflex).Stage II : Excitement
excitation, Pupils dilated and eyes divergent, Agitation, delirium, irregular respiration, and breatholding. Potentially dangerous responses can occur during this stage including vomiting, laryngospasm, HTN, tachycardia, and uncontrolled movement.
Stage III : Surgical anesthesia
Central gaze,constricted pupils, and regular respirations, and have 4 planes.
Stage IV : Impending Death/Overdose
Onset of apnea, dilated and nonreactive pupils, and hypotension to complete circulatory failure.
Anaesthetic Strategies
Induction
ofanaesthesia
Is the process that produces a state of surgical anaesthesia in a patient.
Intravenous induction
Pulse oximetry and ECG monitoring should be established before intravenous access because occasionally a cardiovascular event (e.g. vasovagal syncope) occurs during cannulation.Intravascular access should be established.
Pre-oxygenation: some anaesthetists routinely pre-oxygenate their patients before induction.
Intravenous drugs: slow, smooth injection of an intravenous anaesthetic agent usually results in loss of consciousness in less than 1 minute.
muscle relaxant : the induction agent may be followed by a muscle relaxant, particularly if tracheal intubation is planned.
Intubation: the trachea is intubated with a cuffed tube following unconsciousness and muscle relaxation. Uncuffed tubes are used in children to avoid local pressure on the tracheal wall and to maximize the internal diameter of tube available.
Inhalational induction
maintenanceof
anaesthesia
Usually done by using volatile anesthetics
1- Maintenance of unconsciousness
It is usually achieved by anaesthetic drug delivery via the inhalational or intravenous route, or both.
Inhalational route – this is the most widely used technique, using a volatile anaesthetic agent with or without nitrous oxide.
Intravenous route – a popular alternative to inhalational anaesthesia is total intravenous anaesthesia (TIVA).
2- Analgesia
modern inhalational or intravenous anaesthetic drugs possess little analgesic activity, with the exception of ketamine.Analgesia has several effects.
• It reduces the required of co-administered anaesthetic drugs. Analgesia is an important component of the balanced anaesthetic technique.
• It reduces the immediate autonomic activity in response to pain.
• It reduces the neuroendocrine ‘stress response’ caused by surgery.
3- Providing the best possible operating conditions
The surgeon hopes for two things from his patient during the operation: not to move, and not to bleed.If the anesthetist has succeeded in keeping the patient relaxed (using appropriate muscle relaxant drugs) then the patient is unlikely to move.
The anesthetist can also help to minimize bleeding by:
Tourniquets
Positioning
Hypotensive anaesthesia
Blood gases
RECOVERY
FROM
anaesthesia
recover the patient to consciousness, orientation and resuming the preoperative vital state.
Recovery component
Emergence from General AnesthesiaTransport from the Operating Room
Arrival into recovery room
Management of postanesthetic problems
Discharge
postanesthetic problems
Airway ObstructionHypotension
Hypertension
Agitation & Delirium
Shivering & Hypothermia
Nausea and Vomiting
Pain control
Discharge Criteria
All patients must be evaluated by an anesthesiologist prior to discharge from the PACU unless strict discharge criteria are adopted
discharge criteria are based on Aldrete postanesthetic recovery score.
Ideally, the patient should be discharged when the total score is 10 but a minimum of 9 is required.
• Point Value
Criteria• Oxygenation
2SpO2 > 92% on room air
1
• SpO2 > 90% on oxygen
0
• SpO2 < 90% on oxygen
• Respiration
• 2• Breathes deeply and coughs freely
• 1
• Dyspneic, shallow or limited breathing
• 0
• Apnea
• Circulation
2
• Blood pressure ± 20 mm Hg of normal
1
• Blood pressure ± 20–50 mm Hg of normal
0
• Blood pressure more than ± 50 mm Hg of normal
• Consciousness
2• Fully awake
1
• Arousable on calling
0
• Not responsive
• Activity
2• Moves all extremities
1
• Moves two extremities
0
• No movement