FIFTH STAGE
INTERNAL MEDICINE
DR.FADHIL – LECTURE 10
1
GERIATRIC MEDICINE
AGING
DEFINITION
Aging is the progressive, universal decline first in functional reserve and then in
function that occurs in organisms over
Aging is heterogeneous.
It varies widely in different individuals and in different organs within a particular
individual.
Aging is not a disease; however, the risk of developing disease is increased, often
dramatically, as a function of age.
The biochemical composition of tissues changes with age; physiologic capacity
decreases, the ability to maintain homeostasis in adapting to stressors declines, and
vulnerability to disease processes increases with age .
DEMOGRAPHY OF AGING
Improvements in environmental (e.g., clean water and improved sanitation) and
behavioral (nutrition, reduced risk exposures) factors and the treatment and
prevention of infectious diseases are largely responsible for the 30-year increase in
life expectancy since 1900.
In the United States, by 2030, 1 person in 5 will be >65 years.
GLOBAL AGING
At present 59% of older adults live in the developing countries of Africa, Asia, Latin
America, the Caribbean, and Oceania.
The developed world has the largest absolute number of older adults and is
experiencing the largest percentage increase.
2
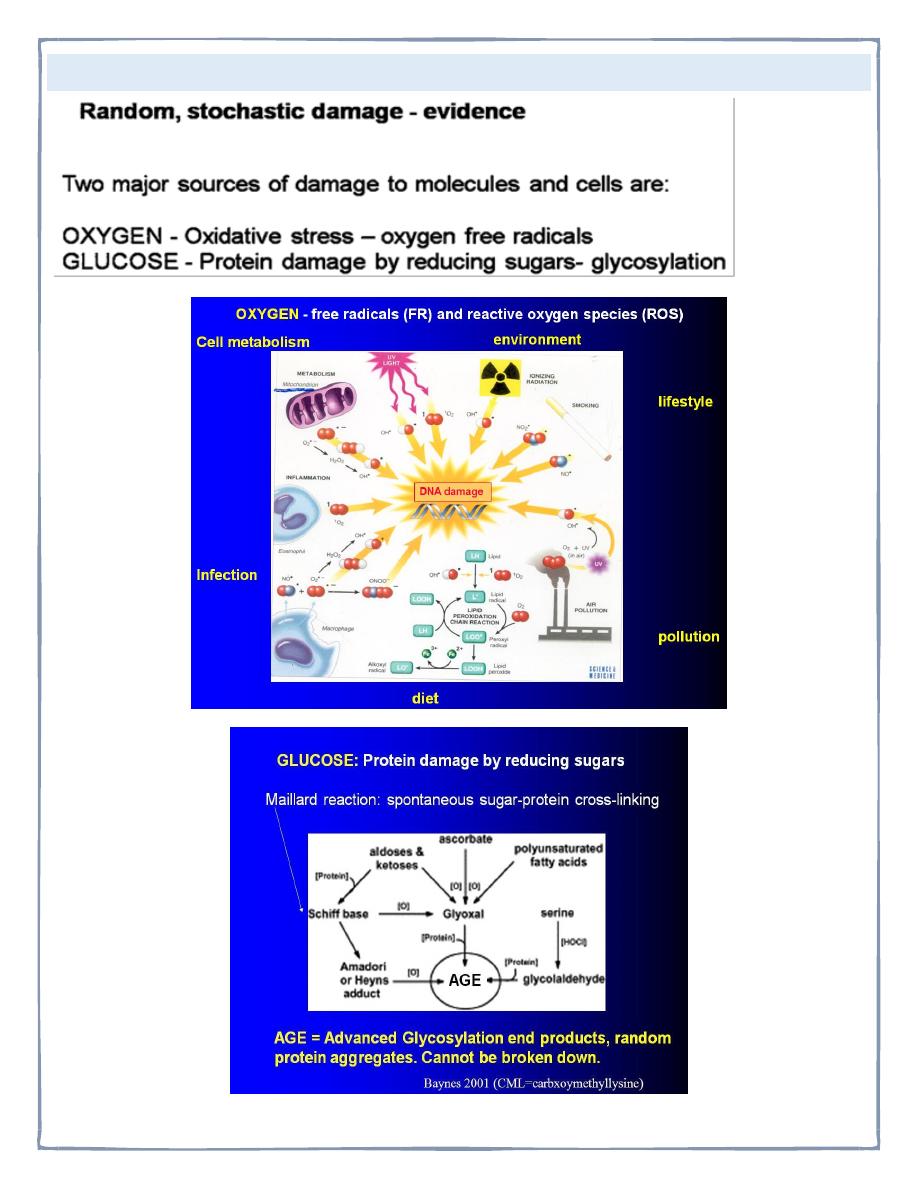
THEORIES OF AGING:
3
Elderly people are incompetent and incapable of making decisions or handling their
own affairs.
Most elderly live in nursing homes
All elderly people live in poverty
Older people are lonely and unhappy
Elderly do not want to work
“Old Age” begins a 65
Retirement ends your active life
PHYSICAL CHANGES OF AGING
Most physical changes that occur with aging are gradual and take place over a long
period of time. In addition, the rate and degree of change varies among individuals.
Factors such as disease can increase the speed and degree of the changes.
Lifestyle, nutrition, economic status, and social environment can also have effects.
If an individual can recognize the changes as a/an normal part of aging, the
individual can usually learn to adapt to & cope with change
INTEGUMENTARY SYSTEM CHANGES
• Production of new skin cells decreases
• Oil and Sweat glands become less active
• Circulation decreases
• Fatty tissue layer of skin diminishes
• Lines and wrinkles appear
• Nails become thick, tough, and brittle
• Increased sensitivity to temperature
4
CIRCULATORY SYSTEM CHANGES
With circulatory changes:
Avoid strenuous exercise or over exertion
Periods of rest
Moderate exercise, according to individual’s tolerance
High Blood Pressure =
Diet low in salt
Decrease fat intake
Exercise as recommended by physician
RESPIRATORY CHANGES
• Respiratory muscles become weaker
• Rib cage more rigid
• Alveoli thinner & less elastic which decreases exchange of gases - emphysema
Changes may cause the elderly to experience:
• Dyspnea
• Breathing increases in rate
• Difficulty coughing up secretions
• Increases susceptibility to infections such as a cold or pneumonia
NERVOUS SYSTEM CHANGES
Blood flow to brain decreases & there is a progressive loss of brain cells - - Interferes
with -Thinking
- Reacting -Interpreting
- Remembering
Senses of taste, smell, vision, & hearing are diminished
Nerve endings less sensitive
Decreased ability to respond to pain and other stimuli
Decrease in taste& smell frequently affects appetite
5
Changes in vision
• Problems reading small print
• Seeing objects at a distance
• Decrease in peripheral vision
• Decrease in night vision
• Increased sensitivity to glare
• Cataracts
• Glaucoma
Changes in hearing
• Hearing loss usually gradual
• Person may speak louder than usual
• Ask for words to be repeated
• Not hear high frequency sounds
• May not hear well in crowded places
Decreased sensation to pain & other stimuli = more susceptible
• Burns
• Frostbite
• Cuts
• Fractures
• Muscle strain and other injuries
DIGESTIVE CHANGES
• Fewer digestive juices and enzymes produced
• Muscle action becomes slower & peristalsis decreases
• Teeth are lost
• Liver function decreases
Dysphagia is frequent complaint:
• Less saliva
• Slower gag reflex
• Loss of teeth
• Poor fitting dentures
6
• Slower digestion of food
• indigestion
URINARY CHANGES
• Kidneys decrease in size & become less efficient
• Bladder becomes less efficient
• May not hold as much
• May not empty completely
• incontinence
ENDOCRINE CHANGES
• Increased production of some hormones and decreased of others
• Immune system less effective
• BMR decreases
• Intolerance to glucose
REPRODUCTIVE SYSTEM CHANGES
• Decrease of estrogen / progesterone in female
• Thinning of vaginal wall
• Decrease vaginal secretions
• Inflammation of vagina common
PSYCHOSOCIAL CHANGES
Some individual cope with psychosocial changes, and others experience extreme
frustration and mental distress
Fears of a sick person:
• Death
• Chronic illness
• Loss of function
• Pain
Confusion and Disorientation
Talking incoherently
7
Not knowing their name
Not recognizing others
Wandering aimlessly
Lacking awareness of time or place
DISEASES:
CVA
Arteriosclerosis
Atherosclerosis
Cause TIA’s ministrokes which result in temporary periods of diminished blood flow
to the brain.
DEMENTIA
Loss of mental ability characterized by a decrease in intellectual ability, loss of
memory, impaired judgement, personality change, and disorientation
ACUTE DEMENTIA
When the symptoms are caused by temporary reason:
High fever, dehydration, hypoxia
Chronic dementia
When symptoms are caused by permanent, irreversible damage to brain cells
TYPES OF DEMENTIA
PRIMARY NEURODEGENERATIVE
CORTICAL
Alzheimer’s disease
Fronto-temporal dementias (Pick’s disease)
8
SUBCORTICAL
Progressive supra nuclear palsy
Huntington’s
Lewy Body Disease
VASCULAR
Multi-infarct
Biswangers disease
INFECTIVE
Creutzfeld-jacob
AIDS
Neurosyphilis
TRAUMA
Sub dural
Dementia pugulistica
radiotherapy
NORMAL PRESSURE HYDROCEPHALUS
ASSOCIATED WITH OTHER DISEASES
Parkinson’s
Wilson’s
Multiple sclerosis
Tumors
Vasculitis
9
ALZHEIMER’S DISEASE
Form of dementia that causes progressive changes in brain cells
The patient may develop seizures
Loses weight despite eating a balanced diet
Becomes totally dependent
Lapses into a coma
Dies
FALLS
CONSEQUENCES
10 –15% fracture
Decrease in functional status
2% injurious falls result in death
Falls usually occur when a threat to the normal homeostatic mechanisms that
maintain postural stability is superimposed on age-related declines in balance,
ambulation and cardiovascular function.
THREAT
Acute illness
Environmental stress
Unsafe walking surface
RISK FACTORS
Age
Female
Past fall
Cognitive impairment
10
Lower limb weakness
Balance disturbance
AGE RELATED FUNCTIONAL DECLINE
Visual
Proprioceptive
Vestibular
MECHANISM
SYNCOPE /HYPOTENSION
SEIZURE
DIZZINESS / BALANCE
GAIT DISTURBANCE
PAIN / WEAKNESS
MECHANICAL FALL
DELIRIUM
Sepsis
Hypoxia
Biochemical disturbances
Calcium, sodium, glucose,urea,hepatic
DEFINITION
An acute organic mental syndrome characterized by:
Global cognitive impairment
Reduced consciousness
11
Disturbed attention
Psychomotor activity
Sleep-wake cycle disturbance
COMPARISON DELIRIUM AND DEMENTIA
Delirium
Dementia
Sudden onset
Usually reversible
Short duration
Fluctuations
Altered consciousness
Associated illness
Inattention
Always worse at night
Impaired variable recall
Insidious onset
Slowly progressive
Long duration
Relatively stable
Normal consciousness
Not associated
Attention not sustained
Can be worse at night
Memory loss
TREATMENT
Treat Memory
Cholinergics
?estrogens
Vitamin E
Selegeline
Treat Symptoms
Treat family
Non pharmacological
Antipsychotics
Benzodiazepines
ANTIDEPRESSANTS
12
WEIGHT LOSS IN ELDERLY PEOPLE
The Nine “Ds” of Inadequate Food Intake and Weight Loss In The Elderly:
• Disease
• Dentition
• Depression
• Dysgeusia
• Drugs
• Dysfunction
• Dementia
• Diarrhea/ Malaborption
• Dysphagia
In about 25% of cases, there is no clear etiology for weight loss.
When etiology is established the most frequent reasons are:
• Depression
• GI (peptic ulcer or motility disorders)
• Cancer
APPETITE
Q/ Which of the following medications may cause loss of appetite in the elderly?
• NSAIDS
• Psuedoephedrine
• Theophylline
• Megestrol Acetate
• Antineoplastics
• Antihistamines
APPETITE LOSE:
Psuedoephedrine, Theophylline, Antineoplastics.
INCREASED APPETITE:
NSAIDS, “Megace” and Antihistamines.
Thank you,,,
