Gall Bladder
Assist. Prof . Dr Salah aljanaby
General surgeon and laparoscopic surgeon
Babylon medical college
Anatomy
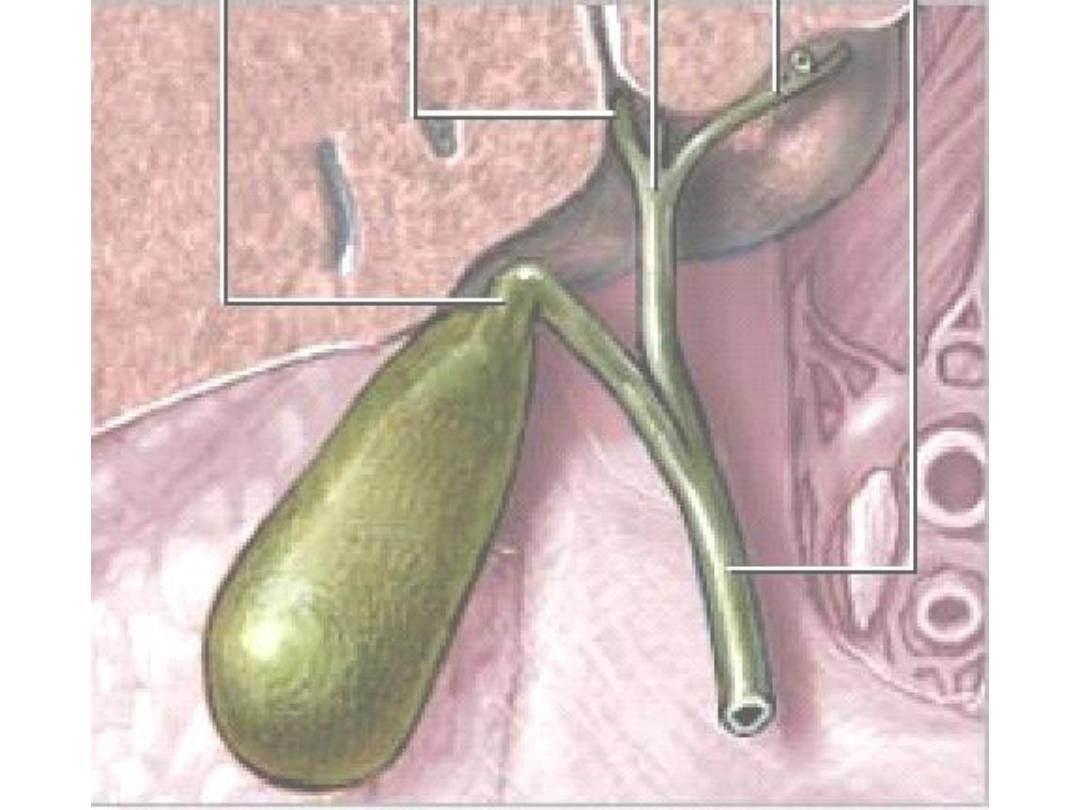
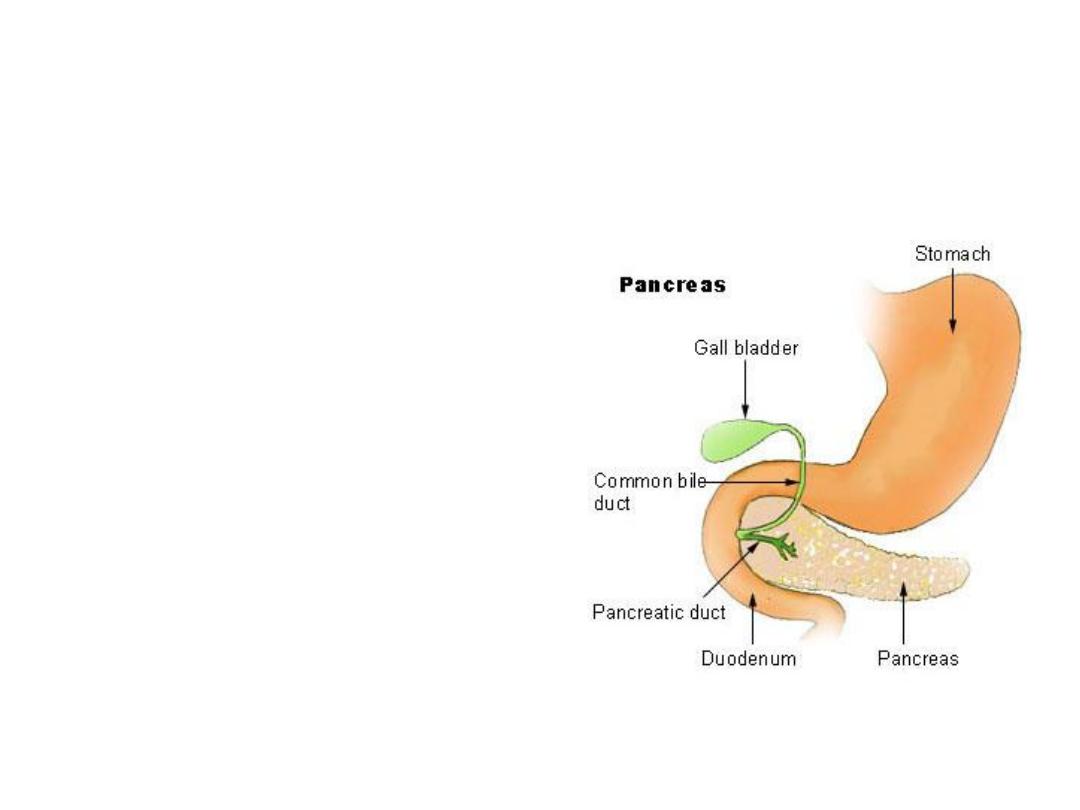
• The gallbladder (or
cholecyst, sometimes
gall bladder) is a pear-
shaped organ that
stores about 50 mL of
bile (or "gall") until the
body needs it for
digestion.
Anatomy
The gallbladder is about 7-10 cm long
in humans and appears dark green
because of its contents (bile), rather
than its tissue. It is connected to the
liver and the duodenum by the
biliary tract.
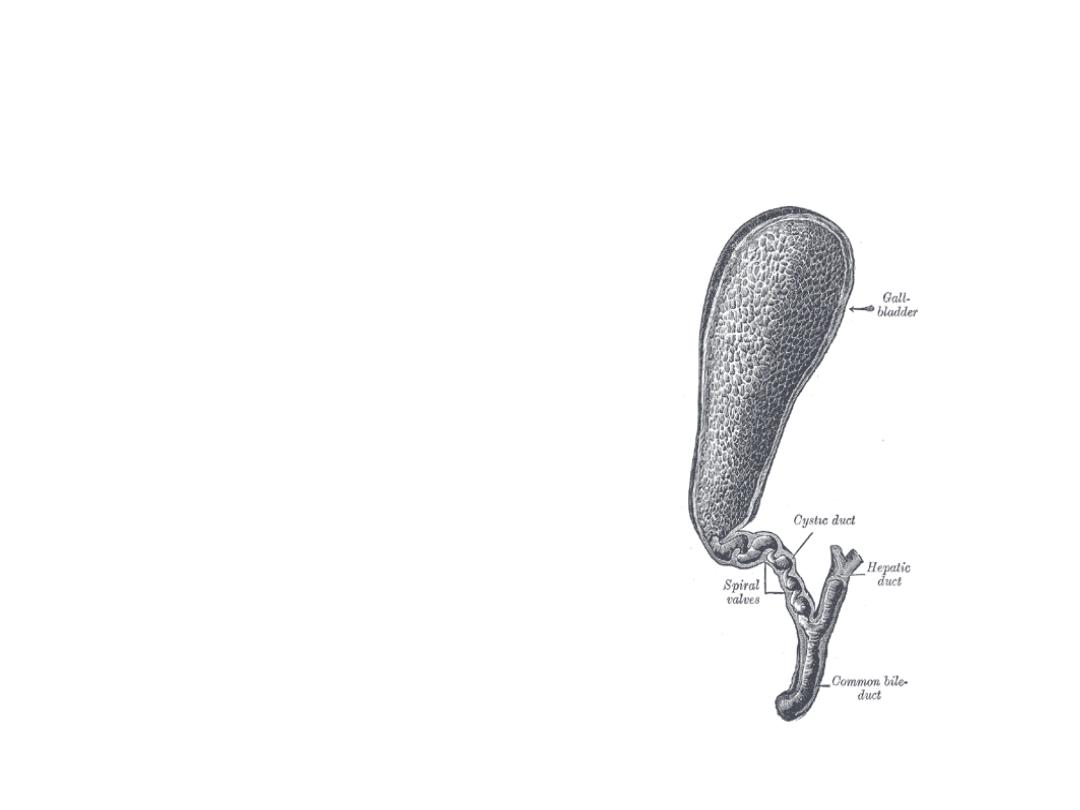
• The cystic duct leads from the
gallbladder and joins with the
common hepatic duct to form the
common bile duct.
• The common bile duct then joins
with the pancreatic duct, and enters
the duodenum through the
hepatopancreatic ampulla at the
major duodenal papilla.
Anatomy
Artery
Cystic artery
Vein
Cystic vein
Nerve
Celiac ganglia, vagus
Precursor
Foregut

Histology
The layers of the gallbladder are as follows:
• The gallbladder has a simple columnar epithelial lining
characterized by recesses called Aschoff's recesses
(lacunae of Luschka) , which are pouches inside the lining.
• Under the epithelium there is a layer of connective tissue.
• Beneath the connective tissue is a wall of smooth muscle
that contracts in response to cholecystokinin, a peptide
hormone secreted by the duodenum.
• There is essentially no submucosa.
Function
• The gallbladder stores about 50 mL of bile , which is
released when food containing fat enters the digestive
tract, stimulating the secretion of cholecystokinin (CCK).
The bile, produced in the liver, emulsifies fats and
neutralizes acids in partly digested food.
• After being stored in the gallbladder, the bile becomes
more concentrated than when it left the liver, increasing
its potency and intensifying its effect on fats. Most
digestion occurs in the duodenum.

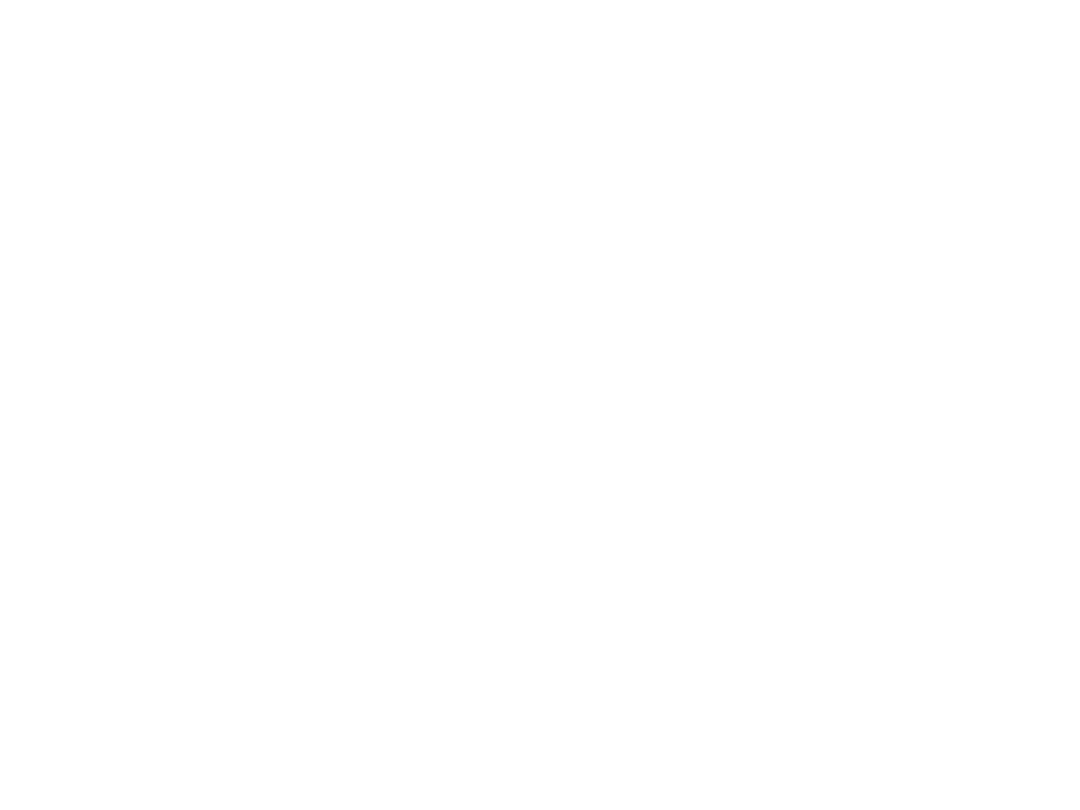
Anomalies
• The gallbladder may be absent = 0.075%
• The gallbladder and cystic duct may be absence.
• the gallbladder is irregular in form or constricted
across its middle; more rarely, it is partially
divided in a longitudinal direction.
• two distinct gallbladders, each having a cystic duct
that joined the hepatic duct. (0.026%), The cystic
duct may itself be doubled
• The gallbladder has been found on the left side (to
the left of the ligamentum teres) in subjects in
whom there was no general tranposition of the
thoracic and abdominal viscera.

• The gallbladder may be intrahepatic or
beneath the left lobe. Ectopic sites include
retrohepatic positions, or in the anterior
abdominal wall or falciform ligament, they
may be suprahepatic or transversely
position, floating, or retroperitoneal. They
may be in the midline anterior epigastric
above the left lobe or suprahepatic above
the right hepatic lobe.

Choledochal cyst
• Choledochal cysts are congenital anomalies of the
bile ducts. They consist of cystic dilatations of the
extrahepatic biliary tree, intrahepatic biliary
radicles, or both.
• Douglas is credited with the first clinical report in a
17-year-old girl who presented with intermittent
abdominal pain, jaundice, fever, and a palpable
abdominal mass.
• Pathophysiology: The pathogenesis of choledochal
cysts is most likely multifactorial.
– A congenital etiology,
– A congenital predisposition to acquiring the disease
under the right conditions.

• The vast majority of patients with
choledochal cysts have an anomalous
junction of the common bile duct with the
pancreatic duct (anomalous pancreatobiliary
junction [APBJ]). An APBJ is characterized
when the pancreatic duct enters the common
bile duct 1 cm or more proximal to where the
common bile duct reaches the ampulla of
Vater.
• APBJs in more than 90% of patients with
choledochal cysts.

• The APBJ allows pancreatic secretions and
enzymes to reflux into the common bile duct.
In the relatively alkaline conditions found in
the common bile duct, pancreatic pro-
enzymes can become activated. This results
in inflammation and weakening of the bile
duct wall. Severe damage may result in
complete denuding of the common bile duct
mucosa.
• From a congenital standpoint, defects in
epithelialization and recanalization of the
developing bile ducts during organogenesis
and congenital weakness of the duct wall
have also been implicated. The result is
formation of a choledochal cyst.

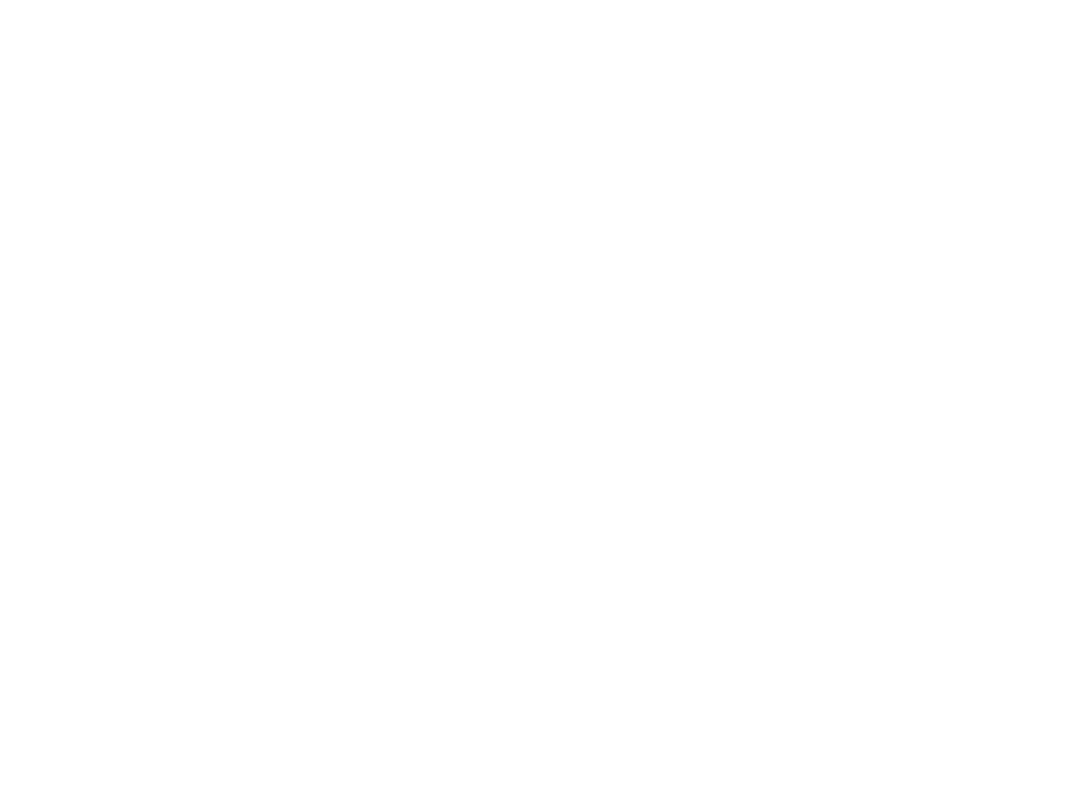
Anatomy of Choledochal cyst
based on the Todani classification published
in 1977.
• Type I choledochal cysts
– most common ; 80-90% of the lesions.
– Type I cysts are dilatations of the entire common
hepatic and common bile ducts or segments of each.
– They can be saccular or fusiform in configuration.
• Type II choledochal cysts
– isolated protrusions or diverticula that project from the
common bile duct wall. They may be sessile or may be
connected to the common bile duct by a narrow stalk.
• Type III choledochal cysts are found in the
intraduodenal portion of the common bile duct.
Another term used for these cysts is
choledochocele.

• Type IVA cysts are characterized by multiple
dilatations of the intrahepatic and extrahepatic biliary
tree. Most frequently, a large solitary cyst of the
extrahepatic duct is accompanied by multiple cysts of
the intrahepatic ducts. Type IVB choledochal cysts
consist of multiple dilatations that involve only the
extrahepatic bile duct.
• Type V choledochal cysts are defined by dilatation of
the intrahepatic biliary radicles. Often, numerous
cysts are present with interposed strictures that
predispose the patient to intrahepatic stone
formation, obstruction, and cholangitis. The cysts are
typically found in both hepatic lobes. Occasionally,
unilobar disease is found and most frequently
involves the left lobe.

• The patient may present at any age with
1. Obstructive jaundice
2. Cholangitis and
3. Abd signs, with RUQ swelling in some cases
• It is a premalignant condition
• Diagnosis by US and MRI
• Radical excision of the cyst is the treatment
of choice with Roux – en –Y reconstruction

Gall stones
• Gall stones are the most common abdominal reason for
admission to hospital in developed countries and account
for an important part of healthcare expenditure. Around
5.5 million people have gall stones in the United Kingdom,
and over 50 000 cholecystectomies are performed each
year.
• Normal bile consists of 70% bile salts (mainly cholic and
chenodeoxycholic acids), 22% phospholipids (lecithin), 4%
cholesterol, 3% proteins, and 0.3% bilirubin.
• There are two major types of gallstones, which seem to
form due to distinctly different pathogenetic mechanisms.

Cholesterol Stones
• About 90% of gallstones are of this type.
These stones can be either;
– almost pure cholesterol {Cholesterol stones}
– or mixtures of cholesterol and other
substances{ cholesterol predominant (mixed)
stones}.

• The key event leading to formation and
progression of cholesterol stones is
precipitation of cholesterol in bile.
• Unesterified cholesterol is virtually
insoluble in aqueous solutions and is kept
in solution in bile largely by virtue of the
detergent-like effect of bile salts.

Imbalance lead to stone formation
• Hyper-secretion of cholesterol into bile due
to
– obesity,
– acute high calorie intake,
– chronic polyunsaturated fat diet, contraceptive
steroids or pregnancy,
– diabetes mellitus and
– certain forms of familial hypercholesterolemia.

• Hypo-secretion of bile salts due to
– impaired bile salt synthesis and
– abnormal intestinal loss of bile salts (e.g. recirculation
failure due to ileal disease).
• Impaired gallbladder function with incomplete
emptying or stasis.
– seen in late pregnancy
– with oral contraceptive use,
– in patients on total parenteral nutrition and
– due to unknown causes, perhaps associated with
neuro-endocrine dysfunction.

• There are clearly important genetic
determinants for cholesterol stone
formation. For example, the prevelance of
the disease in descendents of Chilean,
Indians and in American Indians is
extraordinarily high and not accounted for by
environment.
• There is also an important sex bias in
development of stones - the prevelance in
adult females is two to three times that seen
in males
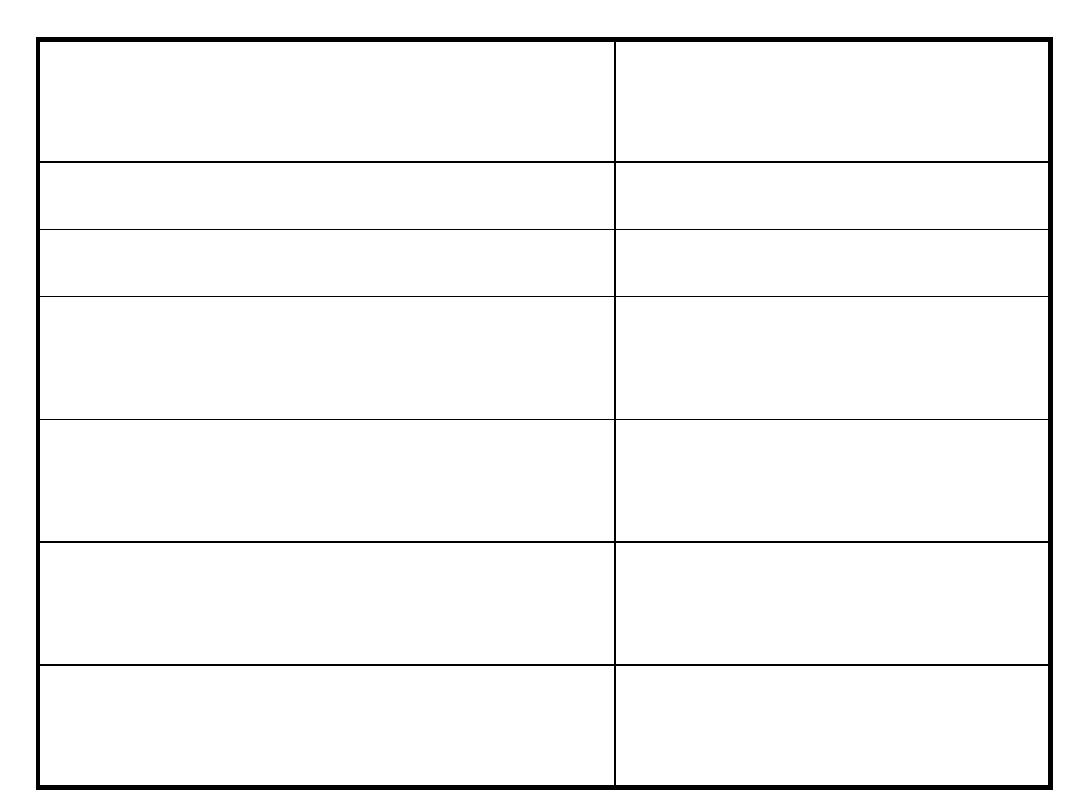
Age >40 years
Bile salt loss (ileal
disease or resection)
Female sex (twice risk in men)
Diabetes mellitus
Genetic or ethnic variation
Cystic fibrosis
High fat, low fibre diet
Antihyperlipidaemic
drugs(clofibrate)
Obesity
Gallbladder dysmotility
Pregnancy (risk increases with
number of pregnancies)
Prolonged fasting
Hyperlipidaemia
Total parenteral
nutrition
•

Pigment Stones
• Roughly 10% of gallstones are pigment
stones
composed of large quantities of bile pigments,
along with lesser amounts of cholesterol and
calcium salts.
• Black pigment stones
– consist of 70% calcium bilirubinate and are
more common in patients with haemolytic
diseases (sickle cell anaemia, hereditary
spherocytosis, thalassaemia) and cirrhosis.

• Brown pigment stones (accounting for <5%
of stones)
– They form as a result of stasis and infection
within the biliary system, usually in the
presence of Escherichia coli and Klebsiella spp,
which produce β glucuronidase that converts
soluble conjugated bilirubin back to the
insoluble unconjugated state leading to the
formation of soft, earthy, brown stones.
– Ascaris lumbricoides and Opisthorchis senensis
have both been implicated in the formation of
these stones, which are common in South East
Asia.

Effects and complications of Gall Stones
In the GB:
• Silent stones
• Chronic cholecystitis
• Acute cholecystitis
• Gangrene
• Perforation
• Empeyma
• Mucocele
• carcinoma
In the bile ducts:
• Obstructive jaundice
• Cholangitis
• Acute pancreatitis
In the intestine:
• Acute intestinal
obstruction (Gall
stone ileus)

Cholecystitis
Definition
• Cholecystitis refers to a painful inflammation of the
gallbladder's wall. The disorder can occur a single
time (acute), or can recur multiple times (chronic).
• Cholecystitis is defined as inflammation of the
gallbladder that occurs most commonly because of an
obstruction of the cystic duct from cholelithiasis.
Ninety percent of cases involve stones in the cystic
duct (ie, calculous cholecystitis), with the other 10%
representing acalculous cholecystitis. Although bile
cultures are positive for bacteria in 50-75% of cases,
bacterial proliferation may be a result of cholecystitis
and not the precipitating factor.

Causes
• Risk factors for calculous cholecystitis mirror
those for cholelithiasis and include the
following:
– Female sex
– Certain ethnic groups (Race)
– Obesity or rapid weight loss
– Drugs (especially hormonal therapy in women)
– Pregnancy
– Increasing age

• Acalculous cholecystitis is related to
conditions associated with biliary stasis,
to include the following:
–Critical illness
–Major surgery or severe trauma/burns
–Sepsis
–Long-term TPN
–Prolonged fasting

• Other causes of acalculous cholecystitis
include the following:
– Cardiac events, including myocardial infarction
– Sickle cell disease
– Salmonella infections
– Diabetes mellitus
– Patients with AIDS with cytomegalovirus,
cryptosporidiosis, or microsporidiosis
• Idiopathic cases exist.

History
• Typical gallbladder colic is 1-5 hours of constant
pain, most commonly in the epigastrium or right
upper quadrant. Pain may radiate to the right
scapular region or back. Peritoneal irritation by
direct contact with the gallbladder localizes the
pain to the right upper quadrant. Pain is severe,
dull or boring, and constant (not colicky). Patients
tend to move around to seek relief from the pain.
Onset of pain develops hours after a meal, occurs
frequently at night, and awakens the patient from
sleep.
• Associated symptoms include nausea, vomiting,
pleuritic pain, and fever.

• Indigestion, belching, bloating, and fatty food
intolerance are thought to be typical
symptoms of gallstones; however, these
symptoms are just as common in people
without gallstones and frequently are not
cured by cholecystectomy.

• Most gallstones (60-80%) are asymptomatic
at a given time. Smaller stones are more
likely to be symptomatic than larger ones.
Almost all patients develop symptoms prior
to complications.
• Symptoms of cholecystitis are steady pain in
the right hypochondrium or epigastrium,
nausea, vomiting, and fever. Acute attack
often is precipitated by a large or fatty meal.

Physical
• Vital signs parallel the degree of illness. Patients
with cholangitis are more likely to have fever,
tachycardia, and/or hypotension. Patients with
gallbladder colic have relatively normal vital signs.
• Patients with cholecystitis are usually more ill
appearing than simple biliary colic patients, and
they usually lie still on the examination table since
any movement may aggravate any peritoneal
signs.

• Abdominal examination;
– Epigastric or RUQ tenderness and abdominal
guarding.
– The Murphy sign (an inspiratory pause on
palpation of the right upper quadrant) can be
found on abdominal examination.
– Positive Murphy sign was extremely sensitive
(97%) and predictive (PPV, 93%) for
cholecystitis. However, in elderly patients, this
sensitivity may be decreased.

• peritoneal signs should be taken seriously. Most
uncomplicated cholecystitis does not have
peritoneal signs; thus, search for complications
(eg, perforation, gangrene) or other sources of
pain.
• Gallbladder gangrene can be a complication in up
to 20% of cases of cholecystitis and is usually in
diabetics, elderly, or immunocompromised
persons.
• A palpable fullness in the RUQ may be
appreciated in 20% of cases.

• As in all patients with abdominal pain, perform a
complete physical examination, including rectal
and pelvic examinations in women.
• In elderly patients and those with diabetes, occult
cholecystitis or cholangitis may be the source of
fever, sepsis, or mental status changes.
• Jaundice is unusual in the early stages of acute
cholecystitis and may be found in fewer than 20%
of patients.
• A very high bilirubin =think for common bile duct
and pancreatic region disease.

DD
Abdominal Aortic Aneurysm
Acute Mesenteric Ischemia
Amebic Hepatic Abscesses
Appendicitis
Biliary Colic
Biliary Disease
Cholangiocarcinoma
Cholangitis
Choledocholithiasis
Cholelithiasis
Gallbladder Cancer
Gallbladder Mucocele
Gallbladder Tumors
Gastric Ulcers
Gastritis, Acute
Gastroesophageal Reflux Disease
Hepatitis, Viral
Myocardial Infarction
Nephrolithiasis
Pancreatitis, Acute
Peptic Ulcer Disease
Pneumonia, Bacterial
Pregnancy and Urolithiasis
Pyelonephritis, Acute
Renal Disease and Pregnancy
Renal Vein Thrombosis

Lab Studies
• Labs with cholelithiasis and gallbladder colic
should be completely normal.
• Because biliary obstruction is limited to the
gallbladder in uncomplicated cholecystitis,
elevation in the serum total bilirubin and alkaline
phosphatase concentrations may not be present.
• An elevated WBC is expected but not reliable. Only
61% of patients with cholecystitis had a WBC
greater than 11,000. A WBC greater than 15,000
may indicate perforation or gangrene.

• Mild elevation of amylase up to 3 times normal
may be found in cholecystitis, especially when
gangrene is present.
• Prothrombin time (PT) and activated partial
thromboplastin time (aPTT) are not expected to be
elevated unless sepsis or underlying cirrhosis is
present. Coagulation profiles are helpful if the
patient needs operative intervention.
• For febrile patients, send 2 sets of blood cultures
to attempt to isolate the organism.
• Although expected to be normal, urinalysis is
essential in the workup of patients with abdominal
pain to exclude pyelonephritis and renal calculi.
• Conduct a pregnancy test for women of
childbearing age.

Imaging Studies
• Ultrasound and nuclear medicine studies
are the best imaging studies for the
diagnosis of both cholecystitis and
cholelithiasis. Plain radiography, CT scans,
and endoscopic retrograde
cholangiopancreatography (ERCP) are
diagnostic adjuncts.

Abd. radiographs (Plain X-Ray)
• Adominal radiographs have low
sensitivity and specificity in
evaluating biliary system pathology,
but
• They can be helpful in excluding
other abdominal pathology such as
renal colic, bowel obstruction,
perforation. Between 10 and 30% of
stones have a ring of calcium and,
therefore, are radiopaque. A
porcelain gallbladder also may be
observed on plain films.

• Emphysematous cholecystitis, cholangitis,
cholecystic-enteric fistula, or postendoscopic
manipulation may show air in the biliary
tree. Air in the gallbladder wall indicates
emphysematous cholecystitis due to gas-
forming organisms such as clostridial species
and Escherichia coli.

Computed tomography scan
• CT scan is recommended only for the evaluation of
abdominal pain if the diagnosis is uncertain. CT scan can
demonstrate gallbladder wall edema, pericholecystic
stranding and fluid, and high-attenuation bile.
• Advantages: For complications of cholecystitis and
cholangitis, gallbladder perforation, pericholecystic fluid,
and intrahepatic ductal dilation, CT scan may be
adequate. CT scan provides better information of the
surrounding structures than sonogram and HIDA. CT scan
is also noninvasive.
• Disadvantages: CT scan misses 20% of gallstones because
the stones may be of the same radiographic density as
bile. CT scan is also more expensive and takes longer since
the patient usually has to drink oral contrast. Also, given
the radiation dose, it may not be ideal in the pregnant
patient.

Ultrasound
• An ultrasound is the most common test used
for the diagnosis of biliary colic and acute
cholecystitis. It is 90-95% sensitive for
cholecystitis and 78-80% specific. For simple
cholelithiasis, it is 98% sensitive and specific.
Findings include gallstones or sludge and
one or more of the following conditions
• Gallbladder wall thickening (>2-4 mm) - False-
positive wall thickening found in
hypoalbuminemia, ascites, congestive heart
failure, and carcinoma
• Gallbladder distention (diameter >4 cm, length
>10 cm)
• Pericholecystic fluid from perforation or exudate
• Air in the gallbladder wall (indicating gangrenous
cholecystitis)
• Sonographic Murphy sign (86-92% sensitive, 35%
specific), pain when the probe is pushed directly
on the gallbladder (not related to breathing)

• Some sonographers recommend the diagnosis of
cholecystitis if both a sonographic Murphy sign
and gallstones (without evidence of other
pathology) are present.
• Additional findings in the presence or absence of
gallstones: Dilated common bile duct or dilated
intrahepatic ducts of the biliary tree indicate
common bile duct stones. In the absence of
stones, a solitary stone may be lodged in the
common bile duct, a location difficult to visualize
sonographically.

• Advantages of sonography include the following:
– Images other structures (eg, aorta, pancreas, liver)
– Identifies complications (eg, perforation,
empyema, abscess)
– Rapidly performed at the bedside
– No radiation (important in pregnancy)
• Disadvantages of sonography include the following:
– Operator dependent and patient dependent
– Inability to image the cystic duct
– Decreased sensitivity for common bile duct stones

• Biliary scintigraphy (HIDA, diisopropyl
iminodiacetic acid [DISIDA]), nuclear
medicine studies
– Sonography or nuclear medicine testing is the
test of choice for cholecystitis. HIDA scans have
sensitivity (94%) and specificity (65-85%) for
acute cholecystitis. They are sensitive (65%) and
specific (6%) for chronic cholecystitis. Oral
cholecystography is not practical for the ED.
– HIDA and DISIDA scans are functional studies of
the gallbladder. Technetium-labeled analogues
of iminodiacetic acid (IDA) or diisopropyl IDA-
DISIDA are administered intravenously (IV) and
secreted by hepatocytes into bile, enabling
visualization of the liver and biliary tree.

– Normal scans are characterized by normal
visualization of gallbladder in 30 minutes.
– With cystic duct obstruction (cholecystitis), the
HIDA scan shows nonvisualization (ie,
considered positive) of the gallbladder at 60
minutes and uptake in the intestine as the bile is
excreted directly into the duodenum.
– Obstruction of the common bile duct causes
nonvisualization of the small intestine.
– The rim sign is increased tracer adjacent to the
gallbladder at 60 minutes and suggests
gangrenous cholecystitis.

• Advantages of HIDA/DISIDA scans include the
following:
– Assessment of function
– Normal-appearing gallbladder (by ultrasound);
obstructed cystic duct abnormal on DISIDA scan but
not ultrasound.
– Simultaneous assessment of bile ducts
• Disadvantages of HIDA/DISIDA scans include the
following:
– High bilirubin (>4.4 mg/dL) possibly decreases
sensitivity
– Recent eating or fasting for 24 hours also possibly
affects study
– No imaging of other structures in the area

• Other Tests:
– Endoscopic retrograde
cholangiopancreatography (ERCP)
• ERCP provides both endoscopic and radiographic
visualization of the biliary tract. It can be diagnostic
and therapeutic by direct removal of common bile
duct stones.
– Magnetic Resonance cholangiopancreatography
(MRCP)
TREATMENT; Conservative treatment
followed by cholecystectomy
Symptoms of acute cholecystitis subside with
conservative treatment in 90 % of cases
– Four principles
1. Naso-gastric suction & IV fluid
2. analgesics
3. Antibiotics (broad spectrum effective against Gm –
ve aerobes)
4. Subsequent management ( if inflame. Subside→
oral fluids → fat free diet)

Cholecystectomy on the next available list or after 4-
6 wks
• Conservative treatment is not advised if there is:
1. Uncertain diagnosis
2. The possibility of high retrocecal appendix or
3. Perforated DU cannot be excluded
• Conservative treatment must be abandoned if
pain and tenderness increased →percutaneous
cholecystostomy → subsequent cholecystectomy

TREATMENT; Routine early operations
Indications:
1. Within 24 hrs of the onset of the attack
2. Experienced surgeons
3. Excellent operating facilities
• cholecystectomy can be done either by
open or laparoscopic approaches

Acalcuolous cholecystitis
• Some patients have non-specific inflammation of
the GB , wherease other have one of the
Cholecystoses
• Diagnosis either by oral cholecystography (
chronic cases) or by isotopic scanning (acute
cases)
• Cholesterol crystal in the duod. aspirate may help
diagnosis

Acute acalcuolous cholecystitis is seen more
frequently in:
• Critical illness
• Major surgery or severe trauma/burns
• Sepsis
• Long-term TPN
• Prolonged fasting

The Cholecystoses
• Not uncommon conditions affecting
the GB where there is chronin
inflamm. Changes with hyperplasia
of of all tissue elemnts
Cholesterosis (Strawberry GB)
• Submucous aggregations of
cholesterol crystals and cholesterol
esters (yellow seeds) in the red
mucosa

Cholesterol polyposis of the GB
• These are either cholesterol polyposis or
adenomatous changes
Cholecystitis glandularis proliferans (polyp,
adenomyomatosis and intramural diverticuolosis)
• MM polyps- fleshy and granuolomatous
• All layer of GB may be thickened
• Sometimes incomplete septums forms
• Intraparietal mixed calculi may be present

Diverticuolosis of the GB
• Usually manifest as black pigment stones
impacted in the out-pouchings of the lacunae of
Luschka
Typhoid GB
• S. Typhi or occasionally S Typhimurium can infect
the GB leading to acute cholecystitis and more
commonly chronic cholecystitis
• The patient being typhoid carrier excreting the
bacteria in the bils
• Gall stones may be present

GB cancer
• Rare ( common in certain area as India where it reaches 9% of
biliary tract disease
• Found in less than 1% of GB operations
• In over 90 % of cases gall stones are present
Presentations
• Age= 70s
• Sex= female (F-M= 5-1)
Pathology
• Scirrhous, but may be squamous cell & mixed squamous
adenocarcinoma
• Spread= direct, lymphatics and veins

Clinical P
• Either extensive mass in the liver during
investigations for jaundice or
• At cholecystectomy at the time the histology is
received
Treatment
• Those diagnosed at cholecystectomy and
confined to the mucosa have a good prognosis
(add wide excision & LN clearance or not ??)
• Large T reaching serosa= chemoradiotherapy
• Median survival 1 year
