1
دكتور حسن سالم الجميلي باطنيه كورس ثاني
lec4
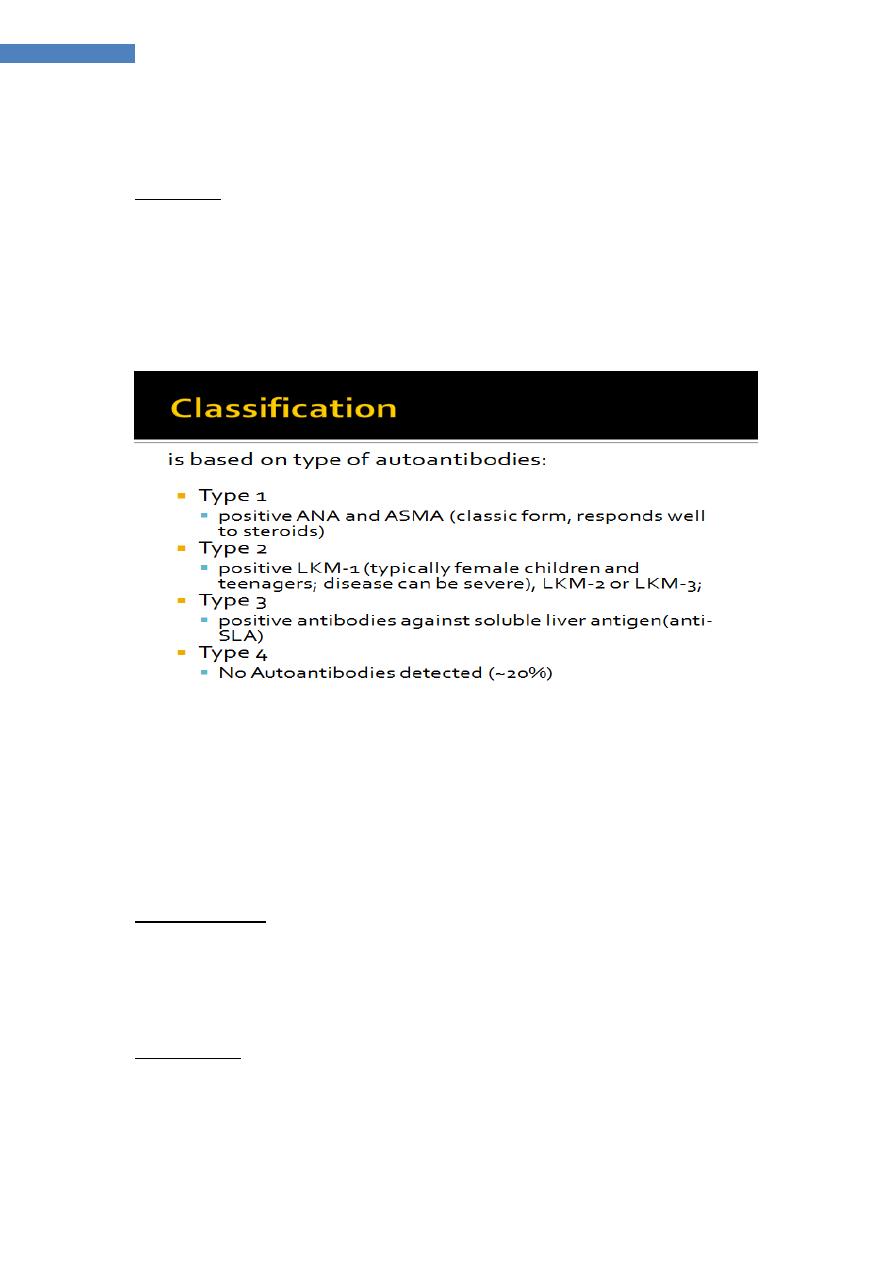
Autoimmune hepatitis
immune-mediated liver injury characterised by the presence of serum antibodies
and peripheral blood T lymphocytes reactive with self-proteins.
association
• Migrating polyarthritis• Urticarial rashes •
• Lymphadenopathy • Hashimoto’s thyroiditis
• Thyrotoxicosis • Pleurisy •
• Coombs-positive haemolyticanaemia
• Ulcerative colitis
• Glomerulonephritis &Nephrotic syndrome
Pathophysiology
The most frequently seen autoantibody pattern is high titre of ANA (antinuclear
Ab and ASMA (anti smoothmuscle Ab0
typically associated with IgGhyperglobulinaemia (type I autoimmune hepatitis),
frequently seen in young adult females.
Antisoluble liver antigen has been described in typically adult patients, often
with aggressive disease
Clinical features
-fatigue, anorexia
-fever, arthralgia, vitiligo and epistaxis. -Amenorrhoea.
-Jaundice is mild - moderate or occasionally absent, but signs of chronic liver
disease, especially spider naevi and hepatosplenomegaly, can be present.
Management
-corticosteroids is life-saving in autoimmune hepatitis,. Initially, prednisolone40
mg/day is given orally; the dose is then gradually reduced as the patient and LFTs
improve. -Maintenance therapy should only be instituted once LFTs are normal
2
دكتور حسن سالم الجميلي باطنيه كورس ثاني
lec4
10
–
prednisolone (< 5
dose
-
to maintenance include reduced
Approaches
mg/day), usually in the context of azathioprine 1.0–1.5 mg/kg/day .
Newer agents such as mycophenolatemofetil (cellcept) are
increasingly being used
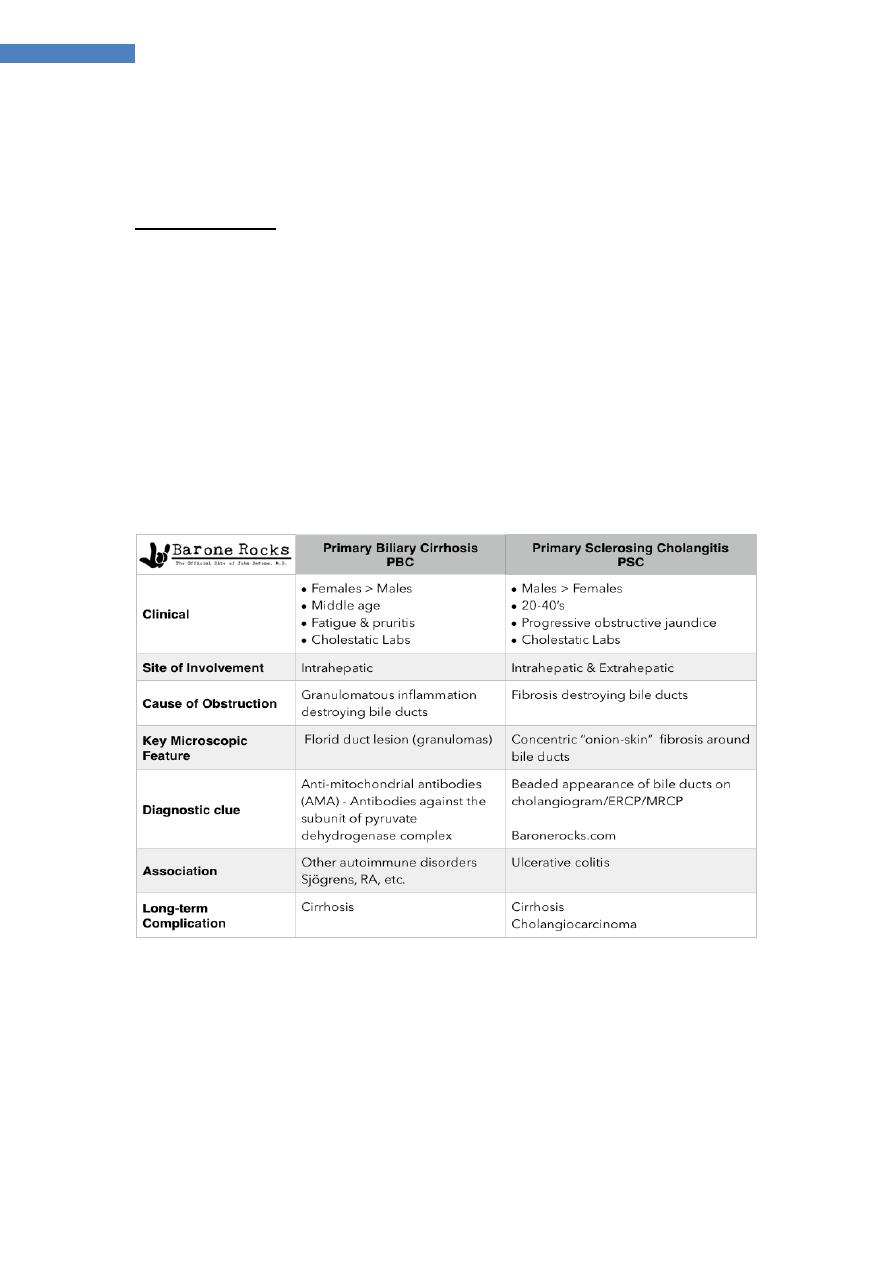
Primary biliary cirrhosis
a chronic, progressive cholestatic liver disease.Female to- male predominance of
9 : 1. more common amongst cigarette smokers
associated with the presence of anti mitochondrialAb(AMA), which are
diagnostic, and is characterised by a granulomatous inflammation of the portal
tracts, leading to progressive damage and eventually loss of the small and middle
sized bile ducts. This in turn leads to fibrosis and cirrhosis of the liver.
Pathophysiology
-Immune mechanisms are clearly involved
-there is a genetic association with HLA-DR8.
-AMA
(selectively binding to the nuclear rim or nuclear dots),
specific ANA
-
PBC
-
which means that they should not be mistaken for the homogenously
staining ANA seen in AIH.
↑ IG
levels are frequent but, unlike in autoimmune hepatitis, elevation is typically
of IgM..
`
Clinical features
fatigue are common and may precede diagnosis for years.
Pruritus, which can be a feature of any cholestatic disease, is a common may
precede jaundice by months or years. Scratch marks may be found in patients
with severe pruritus
Jaundice is rarely a presenting feature. The itching is usually worse on the limbs.
Jaundice is only prominent late in the disease
fever and rigors do not occur.
BUT
right upper abdominal discomfort
Bone pain or fractures can rarely result from osteomalacia (fat-soluble vitamin
malabsorption) or, more commonly, from osteoporosis (hepatic osteodystrophy.
Xanthomatous deposits occur in a minority, especially around the eyes.
Mild hepatomegaly is common .splenomegaly becomes increasingly common as
portal hypertension develops.
Diagnosis and investigations
-The LFTs →cholestasis.
-Hypercholesterolaemia
- AMA >95% of patients
-(MRCP or ERCP) to exclude other biliary disease.
-ANA and ASMA →15% of patients .
- US→no sign of biliary obstruction.
3
دكتور حسن سالم الجميلي باطنيه كورس ثاني
lec4
-Liver biopsy is if diagnostic uncertainty.
orrelate poorly with the clinical features;
The histological features of PBC c
.
portal hypertension can develop before the histological onset of cirrhosis
Management
(UDCA), at a dose of 13–15 mg/kg/day improves bile flow, replaces toxic
hydrophobic bile acids in the bile acid pool, and reduces apoptosis of the biliary
epithelium.
Immunosuppressants, such as corticosteroids, azathioprine, penicillamine and
ciclosporin, have all been trialled in PBC.
Liver transplantation should be considered once liver failure has developed and
may be indicated in patients
with intractable pruritus.. Transplantation is associated with an excellent 5-year
survival of over 80%, although the disease will recur in over 1/3 of patients at 10
years
Pruritus
1-colestyramine, which probably acts by binding potential
pruritogens in the intestine and increasing their excretion in the stoolmain dose
(8 g) taken before and after breakfast,. -
2-rifampicin (150 mg/day, titrated up to a maximum of 600 mg/day
3-naltrexone (an opioid antagonist; 25 mg/day initially, ↑to 300 mg/day)
4-plasmapheresis and a liver support device (e.g. a molecular adsorbent
recirculatingsystem(MARS)).
Bone disease
Malabsorption
Overlap syndromes
)
’
autoimmune cholangitis
‘
negative PBC (
-
AMA
clinical, biochemical and histological features of PBC ,no
AMA in the serum. Serum transaminases, serum Ig levels and titres of ANA tend
to be higher than in AMA positive PBC. →considered to have a variant of PBC
PBC/autoimmune hepatitis overlap
A few patients with AMA and cholestatic LFTs have elevated transaminases, high
serum immunoglobulins
and interface hepatitis on liver histology→ a trial of corticosteroid therapy
Primary sclerosing cholangitis
a cholestatic liver disease caused by diffuse inflammation and fibrosis; it can
involve the entire biliary tree and leads to the gradual obliteration of intrahepatic
and extrahepatic bile ducts
Cholangiocarcinoma→10–30% of patients.
PSC is twice as common in young men.
4
دكتور حسن سالم الجميلي باطنيه كورس ثاني
lec4
-age25–40 years, although the condition may be diagnosed at any age and is an
important cause of chronic liver disease in children.
diagnostic criteria are:
•generalised beading and stenosis of the biliary system on cholangiography
• absence of choledocholithiasis (or history of bile duct surgery)
• exclusion of bile duct cancer.
Pathophysiology
- 2/3 had ulcerative colitis
-3% and 10% of patients with UC develop PSC.
-Patients with PSC and UC are at greater risk of colorectal neoplasiathan those
with UC alone, and those who develop colorectal neoplasia are at greater risk of
CC ( cholangiocarcinoma)
. Perinuclear (ANCA) have been detected in the sera of 60–80% of patients with
PSC with or without ulcerative colitis, and in 30–40% of patients with ulcerative
colitis alone.
Clinical features
-incidentally ↑ALP is discovered in an individual with UC (ulcerative colitis).
-fatigue, intermittent jaundice, weight loss, right upper quadrant abdominal pain
and pruritus.
-common findings are jaundice and HSM (hepatosplenomegally)
Investigations
1-cholestatic picture
2- ↓albuminaemia and clotting abnormalities at a late stage.
3-ANCA, low titres of serum ANA and ASMA may be found in PSC but have no
diagnostic significance;
4-serum AMA is absent.
5-The key investigation ---MRCP, which is usually diagnostic, revealing multiple
irregular stricturing and dilatation .
6-ERCP should be reserved for patients in whom therapeutic intervention is
likely to be necessary and should follow MRCP.
7 -liver biopsy the characteristic early features of PSC are periductal‘onion-skin’
fibrosis and inflammation
; obliterative cholangitis leads to the so-called‘vanishing bile duct syndrome’.
Management
There is no cure for PSC, but management of cholestasis and its complications
and specific treatment of the disease process are indicated.
UDCA may have benefit in terms of reducing colon carcinoma risk. . Most patients
die from liver failure, about 30% die from bile duct carcinoma, and the remainder
die from colonic cancer or complications of colitis. –
5
دكتور حسن سالم الجميلي باطنيه كورس ثاني
lec4
-Immunosuppressive agents, including prednisolone, azathioprine, methotrexate
and ciclosporin, have been tried; generally, results have been disappointing.
Surgical treatment
1-Surgical resection of the extrahepatic bile duct and biliary reconstruction have
a limited role in the management of non-cirrhotic patients .
2-transplantation is the only surgical option in patients with advanced liver
disease
IgG4-associated cholangitis
obstructive jaundice (due to either hilarstricturing/ intrahepatic sclerosing
cholangitis or a low bile duct stricture.
-cholangiographic appearances suggest PSC with or without cholangiocarcinoma.
-IgG4 is often raised and liver biopsy shows a lymphoplasmacytic infiltrate
respond well to steroid therapy.
