
Lec: 6
Dr. Yasameen Alsaffar
Adrenal insufficiency
Adrenal insufficiency results from inadequate secretion of cortisol and/or
aldosterone. It is potentially fatal and notoriously variable in its presentation.
A high index of suspicion is therefore required in patients with unexplained
fatigue, hyponatraemia or hypotension.
Causes:
A- Secondary (
↓ACTH)
1- Withdrawal of suppressive glucocorticoid therapy.
2- Hypothalamic or pituitary disease.
B- Primary (
↑ACTH)
Addison’s disease
1- Autoimmune: either Sporadic or Polyglandular syndromes
2- Tuberculosis.
3- HIV/AIDS.
4- Metastatic carcinoma.
5- Bilateral adrenalectomy.
6- Intra-adrenal haemorrhage (Waterhouse– Friedrichsen syndrome following
meningococcal septicaemia)
7- Amyloidosis.
Clinical assessment
1- Glucocorticoid insufficiency (in all patients)
a-Weight loss, anorexia, Nausea, vomiting, and Diarrhea or constipation.
b- Malaise, weakness.
c- Postural hypotension, Shock.
d- Hypoglycaemia, hyponatraemia (dilutional) and hypercalcaemia.
2- Mineralocorticoid insufficiency: (in patient with Addison disease)
۱

a- Hypotension, Shock.
b- Hyponatraemia (depletional) and hyperkalaemia.
3- ACTH excess: (in patient with Addison disease)
Pigmentation of sun-exposed areas and pressure areas (e.g. elbows, knees),
palmar creases, mucous membranes conjunctivae, and recent scars.
4- Adrenal androgen insufficiency: (in all patients):
Decreased body hair and loss of libido, especially in female.
Features of an acute adrenal crisis include circulatory shock with severe
hypotension, hyponatraemia, hyperkalaemia and, in some instances,
hypoglycaemia and hypercalcaemia.
Investigations
Treatment should not be delayed to wait for results in patients with suspected
acute adrenal crisis. Here, a random blood sample should be stored for
subsequent measurement of cortisol and, if the patient’s clinical condition
permits, it may be appropriate to spend 30 minutes performing a short ACTH
stimulation test before administering hydrocortisone. Investigations should be
performed before treatment is given in patients who present with features
suggestive of chronic adrenal insufficiency.
All patients should be sent for electrolyte (hyponatraemia, hyperkalemia,
hypercalcaemia) and glucose may be low (hypoglycemia).
Assessment of glucocorticoids
Random plasma cortisol is usually low in patients with adrenal insufficiency but
it may be within the reference range, so more useful is the short ACTH
stimulation test, in which cortisol levels fail to increase in response to
exogenous ACTH in patients with primary or secondary adrenal insufficiency.
These can be distinguished by measurement of ACTH (which is low in ACTH
deficiency and high in Addison’s disease).
Assessment of mineralocorticoids
Hyperkalaemia.
Plasma renin increase.
۲
Plasma aldosterone low.
Assessment of adrenal androgens
This is not necessary in men.
In women, dehydroepiandrosterone (DHEA) is low.
Other tests to establish the cause
Patient with low ACTH should be investigated for any pituitary diseases.
In patients with elevated ACTH send for:
1- Adrenal autoantibodies. If –ve so continue to:
2- Imaging of the adrenal glands with CT or MRI is indicated.
3- Tuberculosis causes adrenal calcification, visible on plain X-ray or
ultrasound scan.
4- An HIV test should be performed if there are risk factors.
Management
Glucocorticoid replacement
Adrenal replacement therapy consists of oral hydrocortisone (cortisol) 15–20
mg daily in divided doses, typically 10 mg on waking and 5 mg at around 1500
hrs. These are physiological replacement doses which should not cause
cushingoid side-effects.
Special condition:
1- Febrile illness: we should double dose of hydrocortisone.
2- Surgery:
• Minor operation: hydrocortisone 100 mg IM with pre-medication
• Major operation: hydrocortisone 100 mg 4 times daily for 24 hours, then 50
mg IM 4 times daily until ready to take tablets.
3- Vomiting: Patients must have parenteral hydrocortisone if unable to take it by
mouth.
Mineralocorticoid replacement( inAddison'sdisease)
۳
Fludrocortisone is administered at the usual dose of 0.05–0.15 mg daily, and
adequacy of replacement may be assessed by measurement of blood pressure,
plasma electrolytes and plasma renin.
Androgen replacement
Androgen replacement with DHEA (50 mg/day) is occasionally given to women
with primary adrenal insufficiency.
Adrenal crises:
Correct volume depletion
• IV saline as required to normalise blood pressure and pulse.
• In severe hyponatraemia (<125 mmol/L) avoid increases of plasma Na >10
mmol/L/day to prevent pontine demyelination.
• Fludrocortisone is not required during the acute phase of treatment.
Replace glucocorticoids
• IV hydrocortisone succinate 100 mg stat, and 100 mg 4 times daily for first
12–24 hours
• Continue parenteral hydrocortisone (50–100 mg IM 4 times daily) until patient
is well enough for reliable oral therapy.
Correct other metabolic abnormalities
• Acute hypoglycaemia: IV 10% glucose
• Hyperkalaemia: should respond to volume replacement but occasionally
requires specific therapy.
Incidental adrenal mass
It is not uncommon for a mass in the adrenal gland to be identified on a CT or
MRI scan of the abdomen that has been performed for another indication. Such
lesions are known as adrenal ‘incidentalomas’. They are present in up to 10% of
adults and the prevalence increases with age.
Eighty-five per cent of adrenal incidentalomas are non-functioning adrenal
adenomas. The remainder includes functional tumours of the adrenal cortex
(secreting cortisol, aldosterone or androgens), phaeochromocytomas, primary
and secondary carcinomas.
There are two key questions to be resolved: is the lesion secreting hormones,
and is it benign or malignant?
Clinical signs and symptoms:
٤

Including feature of excess glucocorticoids, mineralocorticoids, catecholamines,
and in women, androgens should be sought.
Investigations
Include a dexamethasone suppression test, urine or plasma metanephrines and,
in virilised women, measurement of serum testosterone, DHEA. Patients with
hypertension should be investigated for mineralocorticoid excess.
CT and MRI are equally effective in assessing the malignant potential of an
adrenal mass, using the following parameters:
1- Size:The larger the lesion, the greater the malignant potential.
2- Configuration:Homogeneous and smooth lesions are more likely to be
benign.
3- Presence of lipid:Adenomas are usually lipid-rich, resulting in an attenuation
of below 10 Hounsfield Units (HU), so low density lesion tend to be benign.
4- Enhancement: malignant lesion tends to take more contrast (enhanced).
Management
Functional lesions and tumours of more than 4 cm in diameter should be
considered for removal by adrenal surgery.
The Endocrine Pancreas & GIT
These include:
a- Hormonal excess:
1- Insulinoma.
2- Gastrinoma (Zollinger–Ellison syndrome).
3- Carcinoid syndrome (secretion of 5-HT).
4- Glucagonoma.
5- VIPoma.
٥
6- Somatostatinoma.
b- Hormone deficiency
Diabetes mellitus.
c- Hormone resistance
Insulin resistance syndromes (e.g. type 2 diabetes mellitus)
Presenting problems in endocrine pancreas disease
Spontaneous hypoglycaemia:
Hypoglycaemia most commonly occurs as a side-effect of treatment with
insulin or sulphonylurea drugs in people with diabetes mellitus. In non-diabetic
individuals, symptomatic hypoglycaemia is rare, but it is not uncommon to
detect venous blood glucose concentrations below 3.0 mmol/L in asymptomatic
patients. Hypoglycemic disorder should only be diagnosed if all three
conditions of Whipple’s triad are met.
Symptoms occurring while fasting (such as before breakfast) or following
exercise are much more likely to be representative of pathological
hypoglycaemia than those which develop after food (post-prandial or ‘reactive’
symptoms). Hypoglycaemia should be considered in all comatose patients.
Investigations
Does the patient have a hypoglycaemic disorder?
In acute presentation: Patients who present acutely with confusion, coma or
convulsions should be tested for hypoglycaemia at the bedside with a capillary
blood sample and an automated meter.
At the same time, a sample should be taken for later measurement, if necessary,
of alcohol, insulin, C-peptide, cortisol and sulphonylurea levels.
In episodic presentation: Patients who attend the outpatient clinic with
episodic symptoms suggestive of hypoglycaemia present a more challenging
problem. The main diagnostic test is the prolonged (72-hour) fast. If symptoms
of hypoglycaemia develop during the fast, then blood samples should be taken
to confirm hypoglycaemia and for later measurement of insulin and C-peptide.
Hypoglycaemia is then corrected with oral or intravenous glucose and
Whipple’s triad completed by confirmation of the resolution of symptoms.
What is the cause of the hypoglycaemia?
٦
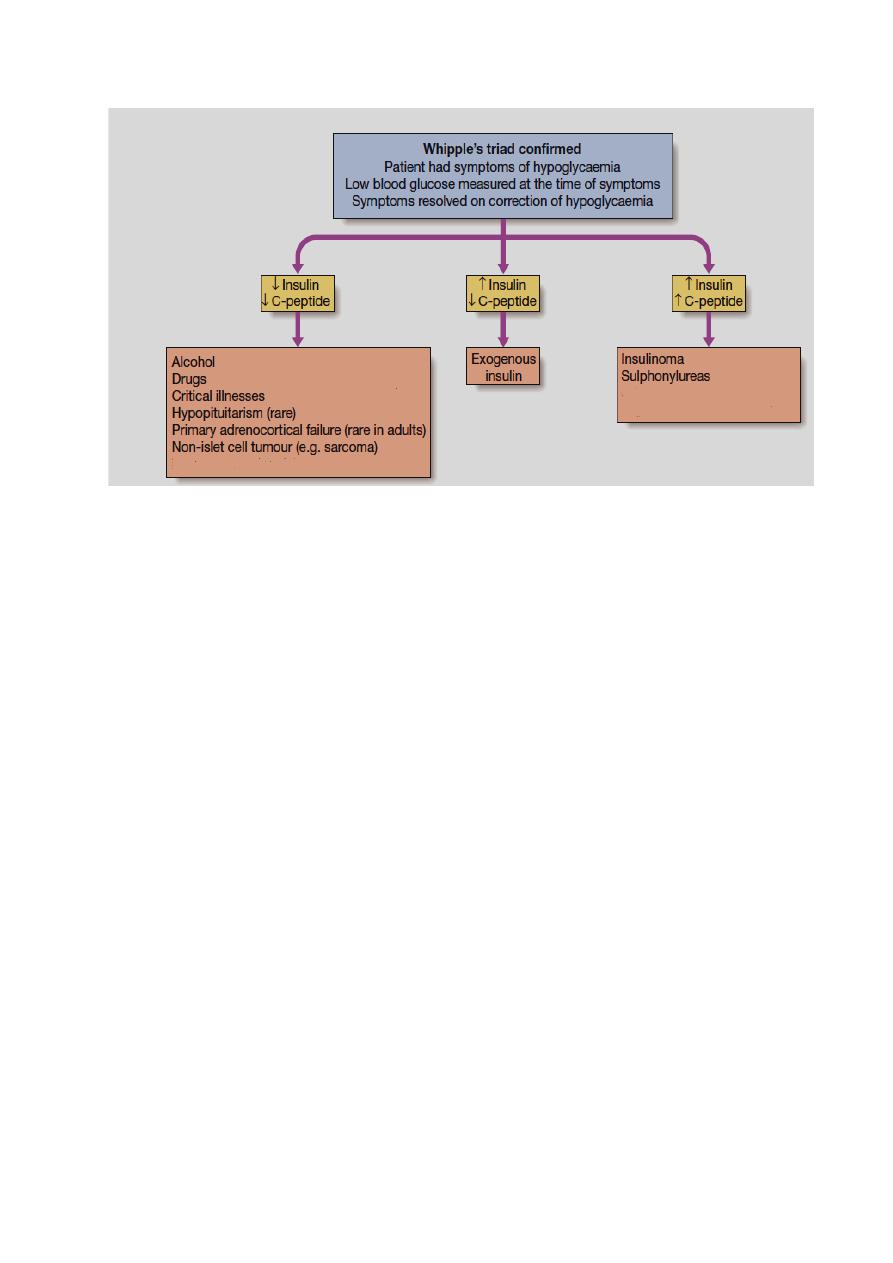
In the acute setting, the underlying diagnosis is often obvious. In non-diabetic
individuals, alcohol excess is the important cause of hypoglycemia.
Hypoglycaemia is one of many metabolic derangements which occur in patients
with hepatic failure, renal failure, sepsis or malaria.
insulinomas in the pancreas are small (<5 mm diameter) but can be identified by
CT, MRI or ultrasound (endoscopic or laparoscopic). Imaging should include
the liver since around 10% of insulinomas are malignant. Rarely, large non
pancreatic tumours, such as sarcomas, may cause recurrent hypoglycaemia
because of their ability to produce excess pro-insulin-like growth factor-2 (pro-
IGF-2).
Management
Treatment of acute hypoglycaemia should be initiated as soon as laboratory
blood samples have been taken, and should not be deferred until formal
laboratory confirmation has been obtained.
1- Intravenous dextrose (5% or 10%): is effective in the short term in the
obtunded patient, and should be followed on recovery with oral unrefined
carbohydrate (starch). Continuous dextrose infusion may be necessary,
especially in sulphonylurea poisoning.
2- Intramuscular glucagon (1 mg): stimulates hepatic glucose release, but is
ineffective in patients with depleted glycogen reserves, such as in alcohol
excess or liver disease.
3- for chronic recurrent hypoglycaemia: in insulin-secreting tumours can be
treated by regular consumption of oral carbohydrate combined with agents that
inhibit insulin secretion (diazoxide or somatostatin analogues). Insulinomas are
resected when benign.
Gastroenteropancreatic neuro-endocrine tumours:
۷

Neuro-endocrine tumours (NETs) are a heterogeneous group derived from
neuro-endocrine cells in many organs, including:
1- The gastrointestinal tract (insulinoma).
2- Lungs ((small-cell carcinoma of the lung).
3- Adrenals (phaeochromocytoma).
4- Thyroid (medullary carcinoma).
Most NETs occur sporadically, but a proportion is associated with genetic
cancer syndromes, such as MEN 1, MEN 2 and neurofibromatosis type 1.
The majority of gastroenteropancreatic NETs behave in an intermediate manner,
with relatively slow growth but a propensity to invade and metastasise to remote
organs, especially the liver.
Clinical features
Patients with gastroenteropancreatic NETs often have a history of abdominal
pain over many years prior to diagnosis and usually present with local mass
effects, such as small-bowel obstruction, appendicitis, and pain from hepatic
metastases.
Carcinoid tumor: The classic ‘carcinoid syndrome’ occurs when vasoactive
hormones (such as serotonin and bradykinin) reach the systemic circulation. In
the case of gastrointestinal carcinoids, this invariably means that the tumour has
metastasised to the liver or there are peritoneal deposits, which allow secreted
hormones to gain access to the systemic circulation; hormones secreted by the
primary tumour into the portal vein are metabolised and inactivated in the liver.
It characterized by the following clinical feature:
1- Episodic flushing, wheezing and diarrhea.
2- Facial telangiectasia.
3- Cardiac involvement (tricuspid regurgitation, pulmonary stenosis, right
ventricular endocardial plaques) leading to heart failure.
The clinical feature of each pancreatic endocrine tumor:
1- Gastrinoma secretes Gastrin and cause Peptic ulcer and steatorrhoea
(Zollinger–Ellison syndrome).
2- Insulinoma secretes Insulin and cause recurrent hypoglycemia.
3- VIPoma secretesvasoactive intestinal peptide (VIP) and cause Watery
diarrhoea and hypokalaemia.
4- Glucagonoma secretesGlucagon and cause Diabetes mellitus, and necrolytic
migratory erythema.
5- Somatostatinoma secretesSomatostatin and cause Diabetes mellitus and
steatorrhoea.
۸

Investigations
A combination of imaging with ultrasound, CT, MRI and/or radio-labelled
somatostatin analogue will usually identify the primary tumour and allow
staging, which is crucial for determining prognosis.
Biopsy of the primary tumour or a metastatic deposit is required to confirm the
histological type. Carcinoid syndrome is confirmed by measuring elevated
concentrations of 5-hydroxyindoleacetic acid (5-HIAA), a metabolite of
serotonin, in a 24 hour urine collection.
Plasma chromogranin A can be measured in a fasting blood sample, along with
the hormones listed above.
Management
Treatment of solitary tumours is by surgical resection. If metastatic or
multifocal primary disease is present, then surgery is usually not indicated,
unless there is a complication such as gastrointestinal obstruction. Diazoxide
can reduce insulin secretion in insulinomas, and high doses of proton pump
inhibitors suppress acid production in gastrinomas. Somatostatin analogues are
effective in reducing the symptoms of carcinoid syndrome and of excess
glucagon and vasoactive intestinal peptide (VIP) production. The slow-growing
nature of NETs means that conventional cancer therapies, such as chemotherapy
and radiotherapy, have limited efficacy.
Other treatments, such as interferon, targeted radionuclide therapy with
131
I-
MIBG and radio-labelled somatostatin analogues (which may be taken up by
NET metastases) and resection/embolisation of hepatic metastases may have a
role in the palliation of symptoms but there is little evidence that they prolong
life.
With best regard
۹
