Orofacial pain
Orofacial painpain : is a complex human psychophysiologic experience associated with actual or potential tissue damage.
Classification of orofacial pain
Somatic pain: arises from musculoskeletal or visceral structures interpreted through an intact pain transmission and modulation systems.Neuropathic pain is defined as pain caused by a lesion or disease of the somatosensory nervous system. The etiology includes trauma, ischemia, infection, or metabolic disturbances. It arises from damage or alteration to the pain pathways; it can be classified into paroxysmal (episodic) and continuous neuropathic pain.
Diagnostic evaluation:
The formal diagnostic evaluation contains the following components:chief complaint, history of present complaint, medical history, physical
examination, diagnostic imaging, and psychosocial evaluation.
Chief complaint
It is the patient's description of the pain. It may provide valuable information to reach diagnosis; pulpal pains are usually provoked by thermal stimulation, neuralgias are frequently described as sharp and lancinating, vascular headaches are throbbing, a and muscle pain is described as a deep, dull ache. Many of these descriptions may overlap.History of present complaint
It should include the following points:• The intensity of the pain needs to be measured against the patient's own experience of pain, need for medication, and effect on lifestyle.
• The patient should be asked to indicate the site of the pain or the site of maximum pain intensity .
• The patient should be encouraged to remember the events surrounding the onset of the pain.
-
• The time relations of the pain should be clarified in terms of duration and frequency.
• Aggravating and relieving factors should be determined.
• The presence or absence of associated factors (redness or swelling of the face, flushing, tearing, nasal congestion, eyelid ptosis, facial numbness, or facial weakness) needs to be ascertained.
Medical history
A careful medical history should be taken. A thorough review of organ system disease should be performed, including surgical history, hospitalizations with special emphasis to history of trauma to the face, mouth or head, allergies, current medical treatments, and current medications, habit history, and psychosocial historyPhysical examination
Patients with orofacial pain should undergo a complete oral cavity, face,head, and neck examination which should include:
inspection.
palpation,
Percussion.
Auscultation.
Imaging
Plain radiographs :like panoramic (OPG) and periapical radiographsprovide detailed evaluation for the jaws and teeth.
More detailed imaging for the maxillofacial skeleton can be provided by computed tomography scan (CT scans),
Magnetic resonance imaging (MRT) is best for soft tissue evaluation
Ultrasonography can be used to evaluate the major salivary glands, carotid arteries, and masses in the neck.
Scintigraphy or bone scan with technetium-99m will highlight areas of
increased metabolic activity within the bone and can help to identify
infection, tumor, or degenerative changes in the TMJ.
Other investigations
These may include blood investigations, microbiological studies, diagnostic injections like local anesthetic, and biopsy of any suspicious mass or lesion.Odontogenic pain
Odontogenic painDental pain is usually well localized, a and the quality of the pain can range from a dull ache to severe, depending on the specific cause and extent of disease. NSAIDs and non-opiate analgesics can be used to alleviate most odontogenic pain but definitive treatment is dental.
Pulpal
Pain may be sharp, throbbing, or dull, it can be spontaneous or provoked or exacerbated by percussion, thermal or electrical stimuli. It is associated with compromised dental pulp due to deep caries, crown fracture or recent dental work. Treatment is by removal of carious lesion, tooth restoration, endodontic treatment., or tooth extraction.Periodontal
Pain is localized, deep continuous associated with compromised periodontium (gingiva or periodontal ligament) exacerbated by biting, chewing or percussion. Usually here are Signs of periodontal inflammation or abscess with or without tooth mobility, periapical radiographs may aid in diagnosis Treatment options include: drainage and debridement of periodontal pocket, scaling and root planning, periodontal surgery, endodontic treatment, or tooth extraction.Cracked tooth
It is associated with fractured tooth with history of trauma or restorativedental work, pain is usually sharp, spontaneous or brief provoked by biting, chewing or percussion. Fractured tooth can usually be detected
by clinical examination or periapical radiograph. Treatment depends on the level of the tooth fracture; restoration or extraction of the tooth.
Dentinal pain
Brief, sharp pain provoked by different kinds of stimuli to the dentin (e.g., hot or cold drinks), it is caused by stimulation exposed dentin or cementum that may result from recession of periodontium or possible erosion of dentinal structure. Treatment options may include: mouthwash (fluoride), desensitizing toothpaste, tooth restoration, endodontic treatment. Patient should be educated about diet, tooth- brushing force and frequency, and proper toothpaste.
Oral mucous membrane disorders
Diseases of the oral mucosa are numerous and have a variety of local and systemic causes. Pain may be a symptom of the disease process, secondary to an associated process (infection), or related to damaged oral mucosa (chewing food, thermal, chemical stimuli). Typically, pain is associated with oral mucosal lesions including; ulcers, vesicles, bullae, erosions, erythema, or red and white patches. Treatment depends on the proper diagnosis; options may include topical or systemic analgesics and corticosteroidsTemporomandibular disorders (TMD)
TMJ disordersDisorders of the TMJ include mainly;
The internal derangements, such as disc displacements with and without reduction, these disorders are the result of disc-condyle incoordination that influences the TMJ biomechanics
TMJ subluxation and dislocation.
Inflammatory disorders (e.g., capsulitis or synovitis).
Osteoarthritis.
Rheumatoid arthritis.
In TMJ disorders pain is localized to the preauricular area during jaw function with presence of painful click or crepitus during mouth opening, in addition to limited mouth opening (35 mm) and deviated or painful jaw movements. There is pain on palpation of the TMJ with possible swelling in the acute phase. CT and MRI may be needed to reach the diagnosis.
Treatment is by:
Patient education and self-care instructions.Medication: NSAIDs, non-opiate analgesics.
Physical therapy through exercise program.
Occlusal splints.
Surgery; is only indicated when non-surgical therapy has been ineffective, and it is not indicated in patients who are asymptomatic or mildly symptomatic or as a preventive measure. Surgical interventions include; arthrocentesis, arthroscopic surgery, and open surgery.
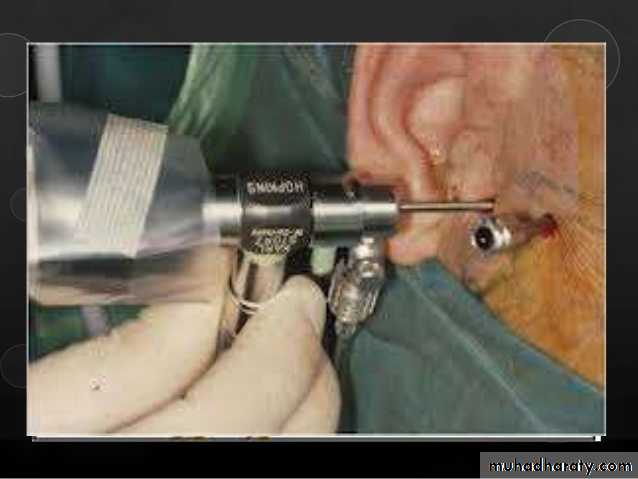
Arthrocentesis is a conservative surgical intervention that involves an intra-articular lavage with or without deposition of hyaluronic acid or corticosteroids: it is mainly indicated in cases of disc displacement without reduction
Arthroscopy is a closed surgical procedure that allows direct observation joint tissue. It is performed mainly in the upper joint space and is utilized primarily for lysis and lavage but also for ablation of adhesions.
Open surgery also called arthotomy is a procedure that modifies joint anatomy, such as total or partial joint reconstruction or replacement, which is required for the patient who has advanced TMD that meets the
surgical criteria and has been refractory to other modalities. It is used in cases of neoplasia, bony or fibrous ankyloses, severe chronic arthritis, and severe chronic dislocations.
Muscle disorders (MFPDS)
Neuropathic painIt has been estimated that the incidence of orofacial neuropathic pain is 5-10 per 100,000 people. It is divided into:
Episodic (paroxysmal) pain disorders, including trigeminal neuralgia and glossopharyngeal neuralgia,
and continuous pain disorders that frequently result from differentiation after injury in the peripheral and central nervous system, which is the case in neuromas and idiopathic trigeminal neuropathic pains such as atypical odontalgia.
Trigeminal neuralgia
It is a chronic paroxysmal neuropathic pain condition that is described as:
a severe, lancinating, and electric-like unilateral pain. It is localized most often to the second and third distributions of the trigeminal nerve (V2 and V3) intraorally and extra-orally and can present in both distributions at the same time. The ophthalmic division is affected alone in only 4% of cases.
There is usually a trigger zone in the trigeminal distribution which, when stimulated, can result in an excruciatingly painful attack. Pain will occur following mild stimulation of this trigger area (e.g., washing the face, shaving, catting, brushing one's teeth, or being exposed to a breeze). The pain attacks last seconds to minutes (about 2 minutes) followed by a refractory period in which stimulation of the trigger zone will not elicit another attack.
It typically affects individuals older than 50 years of age, although it can
develop at any age, including young children. Women are affected moreoften than men by a ratio of 1.5: 1. The majority of cases occur sporadically; however, Several reports of familial trigeminal neuralgia have been described.
Etiology
• Primary or idiopathic (classical) trigeminal neuralgia has no definite cause but localized demyelination may be implicated, the Superior cerebellar artery compression on the trigeminal root has been shown to be responsible for attacks of trigeminal neuralgia pain.• Nonvascular compression by a cerebellopontine angle neoplasm, such as acoustic neuromas, meningiomas, cholesteatomas, and neurofibromas, has also been shown to result in trigeminal neuralgia. Therefore, MRI and CT scan of the brain should be requested in order to rule out any intracranial pathology.
• Myelin loss due to multiple sclerosis has been shown to be a causative disorder related to the trigeminal neuralgia. The trigeminal neuralgia that results from multiple sclerosis or compression of a tumor or malformation is termed secondary or symptomatic trigeminal neuralgia.
Treatment
Medical treatmentAnticonvulsants (e.g., carbamazepine which is the drug of first choice, gabapentin).
Antidepressants (e.g., amitriptyline, nortriptyline).
Non-opiate analgesics.
Botulinum toxin injection.
Combination of baclofen (muscle relaxant) and anticonvulsants when anticonvulsants alone are not effective, or if the therapeutic range cannot be achieved due to side effects.
Surgical treatment
If medical therapy is unsuccessful or not tolerated, surgical treatment should be considered which consists of numerous peripheral and intracranial procedures.
Peripheral procedures all have the goal of inducing nerve damage:
Trigeminal nerve block which provide only temporary relief, high concentration lidocaine (10%) have been used.Alcohol injection may be effective for about 1 year but are painful, and fibrosis makes repeat injections technically difficult. The use of alcohol is associated with many complications include tissue toxicity, inflammation, and fibrosis.
Peripheral neurectomy involves the avulsion or severing of the terminal branches of the trigeminal nerve with or without obturation of the foramen. Pain may recur after 2 years
Cryotherapy of peripheral branches may provide pain relief for 6 months and may be repeated with good results.
Central procedures:
- Percutaneous trigeminal rhizotomy. These procedures are directed at the trigeminal ganglion aims to use controlled injury to interfere with the nerve's ability to transmit signals, They include radiofrequency thermal rhizotomy, glycerol injection, or balloon compression. The three modalities provide approximately equal initial pain relief (around 90%) but are each associated with different rates of recurrence and complications. Overall, radiofrequency rhizolysis consistently provides the highest rates of sustained pain relief but is associated with high frequencies of facial and corneal numbness.-
Posterior fossa exploration and microvascular decompression of the trigeminal root. It is based on the premise that trigeminal neuralgia caused by vascular compression of the nerve root, and surgically separating them may offer a permanent cure. Initial success rates for microvascular decompression are very high (approximately 90%), but long-term follow-up shows that after 10 years 30% to 40% of patients will experience a relapse
-
Gamma Knife stereotactic radiosurgery; it is a minimally invasive technique that precisely delivers radio-surgical doses of 70 to 90 Gy to the trigeminal nerve root at the point of vascular compression as mapped using MRI, it provides good to excellent (60%-90%) initial pain relief.
Glossopharyngeal neuralgia
Glossopharyngeal neuralgia is a rare condition (0.2-1.3% of facial pain syndromes) associated with pain in area supplied by the glossopharyngeal nerve (9th cranial nerve). Painful sites may include the nasopharynx, posterior part of the tongue, throat, tonsil, larynx, and ear.Atypical odontalgia
Pain that occurs when damage to the afferent pain transmission system has occurred (deafferentation). Usually, this condition is caused by trauma or surgery, including extraction and endodontic treatment. The patient usually complains of a spontaneous or provoked pain described as burning, nagging or boring pain.
Pain that result from peripheral neural damage can be relieved by local anesthetic blocks but in some cases the peripheral neural damage leads to central changes in the trigeminal nucleus causing ongoing pain transmission to higher cortical centers despite minimal or even no peripheral input. Local anesthetic block does not arrest pain in this case.
Treatment :is by anticonvulsants, antidepressants and non-opiate analgesics. rhyzotomy and Gamma knife may be indicated in nonresponsive cases.
Post-herpetic neuralgia
It is a potential sequela of shingles, also known as herpes zoster which is the clinical manifestation of the reactivation of a lifelong latent infection with varicella zoster virus, usually contracted after an episode of chicken pox in early life where the virus lay dormant in the ganglia of peripheral nerves but in 10-15% of the cases the trigeminal nerve is involved in which the dermatome of the ophthaimic branch ) is affected in about 80% of the cases.Treatment :is by acyclovir 1n the acute phase, anticonvulsants, antidepressants, non-opiate analgesics. Rhyzotomy and Gamma knife may be indicated in nonresponsive cases.
Vascular pain
Giant cell arteritis (Temporal arteritis)It is an immune-mediated vasculitis that affects medium-sized and larger arteries, leading to vascular occlusion and ischemia, although it is considered as a systemic condition and can affect any vessel but the superficial temporal artery is the most commonly affected site. Patients are usually above 50 years of age with female predilection, presenting with symptoms of severe headache and scalp tenderness.
Treatment
Treatment is by high-dose systemic corticosteroid therapy, the dose can be reduced as the ESR starts to fall. Methotrexate or azathioprine Sometimes will be added for their steroid-sparing effects.Migraine
It is vascular or neurovascular in origin. It is described as recurrent headache attacks lasting 4-72 hours, the pain is unilateral, of pulsating quality, moderate or severe intensity, aggravated by routine physical activity, certain foodstuffs . chocolate, bananas), alcohol, stress, hormonal changes during the menstrual cycle, the contraceptive pill or noise. It may be preceded by an aura which may include nausea, vomiting, visual disturbances (photophobia, Hashing lights) and other disturbances of sensory and/or motor function. It occurs in females more than males with wide age range from childhood onwards.Treatment
Medical treatment include: NSAIDs, Ergotamine derivatives, such as dihydroergotamine, Serotonin 5-HD receptor agonists), such as sumatriptan. Other medications that have proven beneficial are beta adrenergic blockers such as propranolol and atenolol, calcium channel blockers such as verapamil and flunarizine, tricyclic antidepressants such as amitriptyline, serotonin antagonists such as methysergide, and antiepileptics such as topiramate and valproate.