TREATMENT OF ACUTE PERIODONTAL DISEASE
DR. HANDREN HUNAR NAJEEBIntroduction
Acute infections are of sudden onset, limited duration & with well defined features in contrast with chronic lesions.Associated with Pain.
Early diagnosis & treatment is necessary to prevent rapid destructions of periodontal tissues.
Acute Periodontal Infections
Abscess in the PeriodontiumPericoronitis
Herpetic gingivostomatitis
Bacterial acute infections ( e.g. Streptococcal gingivostomatitis, Gonococcal stomatitis )
NUG
Abscess in the Periodontium
Classification of Periodontal Abscess• Gingival abscess.
• Periodontal abscess.
• Pericoronal abscess.
Abscess in the Periodontium
• Gingival abscess: A localized, painful, rapidly expanding lesion involving the marginal gingiva or interdental papilla, sometimes in a previously disease-free area.• Periodontal abscess: A localized accumulation of pus within the gingival wall of a periodontal pocket resulting in the destruction of the collagen fibre attachment and the loss of nearby alveolar bone.
• Pericoronal abscess: Localized accumulation of pus within the overlying gingival flap surrounding the crown of an incompletely erupted tooth.
Gingival Abscess:
Etiology:Acute inflammatory response to foreign substances forced into the gingiva.
Clinical Features:
Localized swelling involving marginal gingiva or interdental papilla.
A red, smooth, shiny surface.
May be painful and appear pointed.
Purulent exudate may be present.
No previous periodontal disease.
Gingival Abscess:
Treatment:• Topical or local anaesthesia by infiltration is administered.
• When possible, SRP to establish drainage and remove microbial deposits.
• In acute cases, the fluctuant area is incised with a #15 scalpel blade and exudate may be expressed by gentle digital pressure.
• Any foreign material is removed.
Gingival Abscess:
• The area is irrigated with warm saline water and covered with moist gauze under light pressure.
• Once bleeding has stopped, patient is dismissed with instructions to rinse with warm saline water every 2 hrs.
• After 24 hrs, the area is reassessed, and if resolution is sufficient, scaling not previously completed is undertaken.
• If the lesion is large or poorly accessible, surgical access may be required.
Periodontal Abscess
Also known as a lateral abscess or parietal abscess.Clinical Features:
Smooth, shiny swelling of the gingiva.
Painful, tender to palpation.
Purulent exudate.
Increased probing depth.
Mobile .
percussion sensitive.
Tooth usually vital.
Periodontal Abscess
TreatmentEstablish drainage – localised abscess
Via sulcus is the preferred method
Surgical access for debridement - Incision and drainage
Removal of foreign body
Extraction : poor prognosis in SPT
Local / Systemic Antibiotics – diffuse involvement
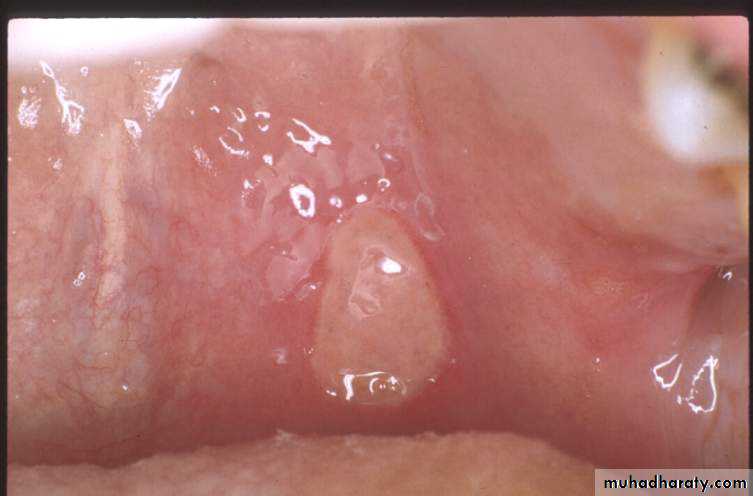
Pericoronitis
Clinical Features:
The partially erupted or impacted Mandibular third molar is the most common site. Maxillary Third molar, Mandibular First, Second Molars are also affected.
The space between the crown of the tooth and operculum (i.e. overlying gingival flap) harbours food debris and promotes bacterial growth due its relative inaccessibility to the cleansing measures.
The operculum, even in patients without any symptoms is chronically inflamed with ulcerations in the inner aspect.
Pericoronitis
Treatment:Persistent asymptomatic pericoronal flap should be removed as a preventive measure.
Gentle flushing with warm water to remove debris and exudate.
Swabbing with antiseptic after elevating the flap with a scaler.
Antibiotics, in case of diffuse microbial infiltration.
In case of fluctuant abscess drainage should be accomplished by incision.
Necrotizing PeriodontalDiseases
Necrotizing Ulcerative Gingivitis (NUG)Necrotizing Ulcerative Periodontitis (NUP)
Necrotizing UlcerativeGingivitis
Clinical Features• – Gingival necrosis, especially tips of papillae
• – Gingival bleeding
• – Pain
• – Fetid breath
• – Pseudomembrane formation
Necrotizing UlcerativeGingivitis
Predisposing Factors
• – Emotional stress
• – Poor oral hygiene
• – Cigarette smoking
• – Poor nutrition
• – Immunosuppression
***Necrotizing Periodontal diseases are common in immunocompromised patients, especially those who are HIV (+) or have AIDS
Necrotizing UlcerativePeriodontitis
An infection characterized by necrosis of gingival tissues, periodontal ligament, and alveolar bone.Clinical Features
• – Clinical appearance of NUG
• – Severe deep aching pain
• – Very rapid rate of bone destruction
• – Deep pocket formation not evident
Necrotizing PeriodontalDiseases
Treatment• – Local debridement
• – Oral hygiene instructions
• – Oral rinses
• – Pain control
• – Antibiotics
• – Modify predisposing factors
• – Proper follow-up
Necrotizing PeriodontalDiseases
– Local debridement
• »Most cases adequately treated by debridement and sc/rp
• » Anesthetics as needed
• » Consider avoiding ultrasonic instrumentation due to risk of HIV transmission
– Oral hygiene instructions
Necrotizing PeriodontalDiseases
• – Oral rinses – (frequent, at least until pain subsides allowing effective OH)• » Chlorhexidine gluconate 0.12%; 1/2 oz 2 x daily
• » Hydrogen peroxide/water
• » Povidone iodine
– Pain control
Necrotizing PeriodontalDiseases
– Antibiotics (systemic or severe involvement)• »Metronidazole
• » Avoid broad spectrum antibiotics in AIDS patients
– Modify predisposing factors
– Follow-up
• » Frequent until resolution of symptoms
• » Comprehensive periodontal evaluation
• following acute phase!!!!
Herpetic Gingivostomatitis
To be continued next lecture
Primary Herpetic GingivostomatitisClinical Features
• – Painful severe gingivitis with ulcerations, edema, and stomatitis
• – Vesicles rupture, coalesce and form ulcers
• – Fever and lymphadenopathy are classic features
• – Lesions usually resolve in 7-14 days
Primary Herpetic Gingivostomatitis
Treatment• – Bed rest
• – Fluids – forced
• – Nutrition
• – Antipyretics
• » Acetaminophen, not ASA due to risk of Reye’s
• Syndrome
Primary Herpetic Gingivostomatitis
• – Pain relief• » Viscous lidocaine
• » Benadryl elixir
• » 50% Benadryl elixir/50% Maalox
• – Antiviral medications
• » Immunocompromised patients
Recurrent Oral Herpes
“Fever blisters” or “cold sores”
Oral lesions usually herpes simplex virus type 1
Recurrent infections in 20-40% of those with primary infection
Herpes labialis common
Recurrent infections less severe than primary
Recurrent Oral Herpes
Clinical Features• – Prodromal syndrome
• – Lesions start as vesicles, rupture and leave ulcers
• – A cluster of small painful ulcers on attached gingiva or lip is characteristic
• – Can cause post-operative pain following dental treatment
Recurrent Oral Herpes
Virus reactivation• – Fever
• – Systemic infection
• – Ultraviolet radiation
• – Stress
• – Immune system changes
• – Trauma
• – Unidentified causes
Recurrent Oral Herpes
Treatment
• – Palliative
• – Antiviral medications
• » Consider for treatment of immunocompromised patients, but not for periodic recurrence in healthy patients
Bacterial acute infections
Streptococcal gingivitis or gingivostomatitis is a rare entity that may present as an acute condition.Clinical Features:
fever, malaise, and pain associated with acutely inflamed, diffuse, red, and swollen gingiva with increased bleeding and occasional gingival abscess formation.
usually preceded by tonsillitis.
Recurrent Aphthous Stomatitis
Clinical features• – Affects mobile mucosa
• – Most common oral ulcerative condition
• – Three forms
• »Minor
• »Major
• » Herpetiform
Recurrent Aphthous Stomatitis
Minor Aphthae
• »Most common
• » Small, shallow ulcerations with slightly raised erythematous borders
• » Central area covered by yellow-white pseudomembrane
• » Heals without scarring in 10 –14 days
Minor Apthae
Recurrent Aphthous Stomatitis
Major Aphthae• » Usually larger than 0.5cm in diameter
• »May persist for months
• » Frequently heal with scarring
Major Aphthae
Recurrent Aphthous Stomatitis
Herpetiform Aphthae• » Small, discrete crops of multiple ulcerations
• » Lesions similar to herpetic stomatitis but no vesicles
• » Heal within 7 – 10 days without scaring
Recurrent Aphthous Stomatitis
Predisposing Factors• – Trauma
• – Stress
• – Food hypersensitivity
• – Previous viral infection
• – Nutritional deficiencies
Recurrent Aphthous Stomatitis
Treatment - Palliative• – Pain relief - topical anesthetic rinses
• – Adequate fluids and nutrition
• – Corticosteroids
• – Oral rinses (Chlorhexidine has been anecdotally reported to shorten the course of apthous stomatitis)
• – Topical “band aids”
• – Chemical or Laser ablation of lesions
Allergic Reactions
Intraoral occurrence uncommon
Examples
– Dental restorative materials
• »Mercury, nickel, gold, zinc, chromium, and acrylics
– Toothpastes and mouthwashes
• » Flavor additives (cinnamon) or preservatives
– Foods
• » Peanuts, red peppers, etc.
Allergic Reactions
Clinical Features – Variable• – Resemble oral lichen planus or leukoplakia
• – Ulcerated lesions
• – Fiery red edematous gingivitis
Treatment
• – Comprehensive history and interview
• – Lesions resolve after elimination of offending agent