1
Lec. 1 D.Abeer M. Zwain
Gingivitis and Periodontal Disease
The gingiva is the part of the oral mucous membrane that covers the
alveolar processes and the cervical portions of the teeth. It has been divided
traditionally into: the free and the attached gingiva.
The free gingiva is the tissue coronal to the bottom of the gingival sulcus.
The attached gingiva extends apically from the free gingival groove to the
mucogingival junction.
The gingival tissues are normally light pink, although the color may be
related to the complexion of the person, the thickness of the tissue, and the
degree of keratinization.
The gingival color of the young child may be more reddish due to
increased vascularity
and thinner epithelium. The surface of the gingiva of a child appears
less stippled or smoother than that of an adult. During the period of
tooth eruption in the child, however, the gingivae are thicker and have
rounded margins due to the migration and cervical constriction of the
primary teeth.
Gingivitis
is an inflammation involving only the gingival tissues next to the tooth with no
loss of attachment or bone. It occurs in response to the bacteria that live in biofilms at the
gingival margin and in the sulcus. The clinical signs of gingivitis include erythema, bleeding on
probing, and edema. In the early primary dentition, gingivitis is uncommon. Younger children
have less plaque than adults do and appear to be less reactive to the same amount of plaque.
This can be explained both by differences in bacterial composition of plaque and by
developmental changes in inflammatory response.
S I M P L E G I N G I V I T I S
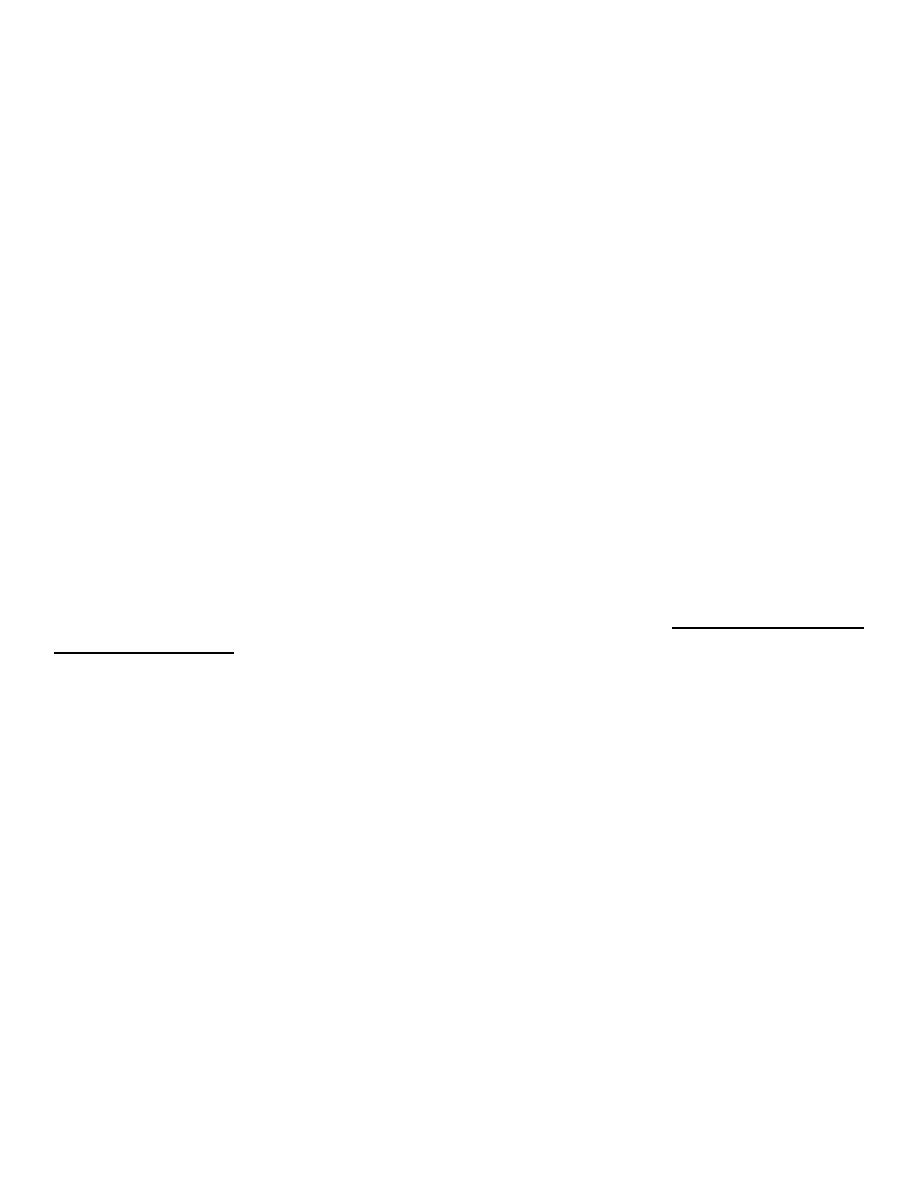
ERUPTION GINGIVITIS
A temporary type of gingivitis is often observed in young children when the primary teeth
are erupting. This gingivitis, often associated with difficult eruption, subsides after the teeth
emerge into the oral cavity
Food debris, materia alba, and bacterial plaque often collect around and beneath the free
tissue, partially cover the crown of the erupting tooth, and cause the development of an
inflammatory process . This inflammation is most commonly associated with the eruption of the
first and second permanent molars and the condition can be painful and can develop into a
pericoronitis or a pericoronal abscess. Mild eruption gingivitis requires no treatment other than
improved oral hygiene. Painful pericoronitis may be helped when the area is irrigated with a
2
counterirritant, such as Peroxyl.* Pericoronitis accompanied by swelling and lymph node
involvement should be treated with antibiotic therapy.
GIENGINGIVITIS ASSOCIATED WITH POOR
ORAL HYEGINE
The degree of dental cleanliness and the condition of the gingival tissues in children are
definitely related,
adequate mouth hygiene and cleanliness of the teeth are related to frequency of brushing
and the thoroughness with which bacterial plaque is removed from the teeth.
Favorable occlusion
and the chewing of course, detergent-type foods, such as raw carrots, celery, and apples,
have a beneficial effect on oral cleanliness..
Gingivitis is quickly reversible and can be treated with a good oral prophylactic treatment and
instruction in good tooth brushing and flossing techniques to keep the teeth free of bacterial
plaque.
Children under 8 to 10 years old are not yet capable of performing effective oral
hygiene measures and require assistance.
Older children and even adolescents probably need at least some oversight from the
parents.
ALLERGY AND GINGIVAL INFLAMMATION
An enhanced gingival inflammatory reaction in the allergic children during the pollen seasons
was found by the researchers.
ACUTE GINGIVAL DISEASE
HERPES SIMPLEX VIRUS INFECTION
Herpesvirus causes one of the most widespread viral infections. The primary infection usually
occurs in a child under 6 years of age who has had no contact with the type 1 herpes simplex
virus (HSV-1) and who therefore has no neutralizing antibodies. It is believed that 99% of all
primary infections are of the subclinical type. The infection may also occur in susceptible
adults who have not had a primary infection. In some preschool children the primary infection
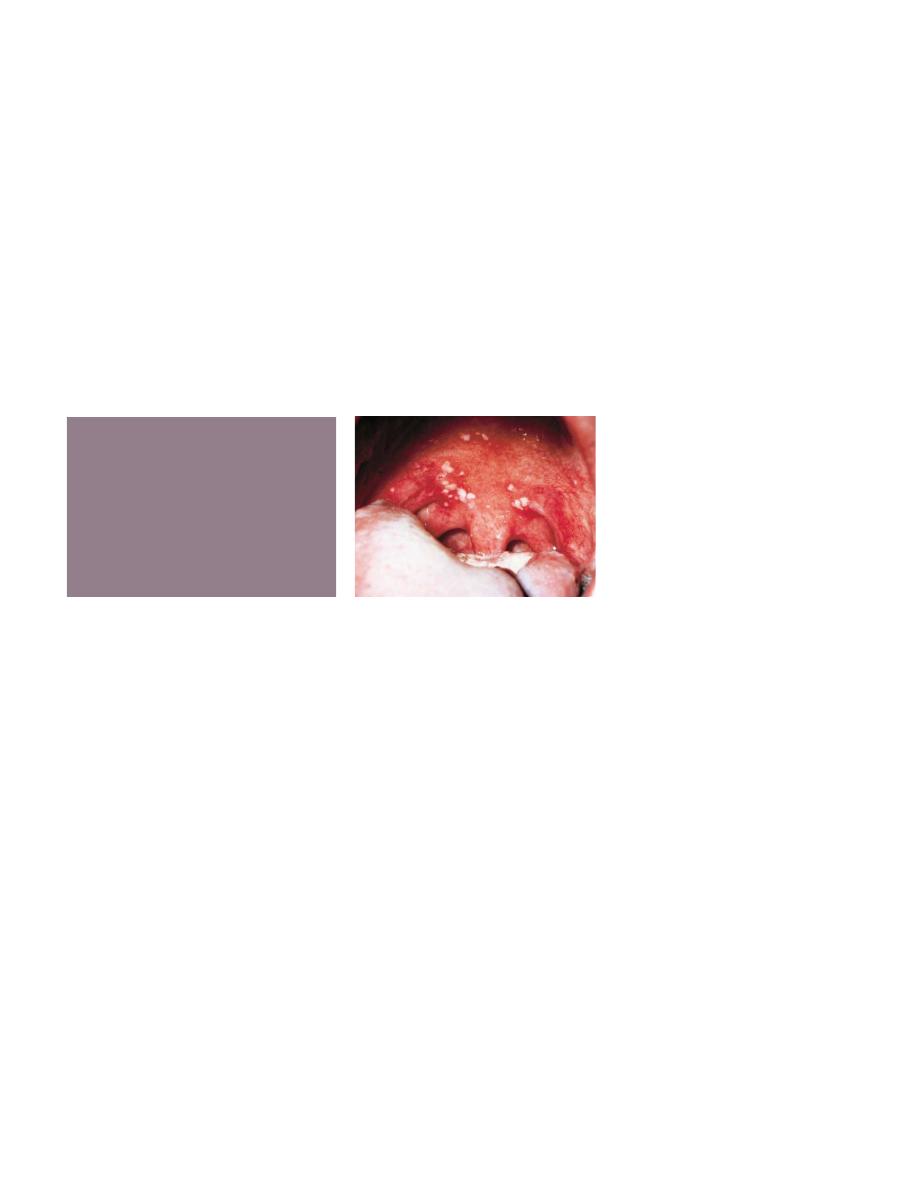
3
may be characterized by only one or two mild sores on the oral mucous membranes, which
may be of little concern to the child or may go unnoticed by the parents. In other children the
primary infection may be manifested by acute symptoms (acute herpetic gingivostomatitis).
The symptoms of the disease develop suddenly running a course of 10 to 14 days and
include, in addition to the fiery red gingival tissues, malaise, irritability, headache, and pain
associated with the intake of food and liquids of acid content.
A characteristic oral finding in the acute primary disease is the presence of yellow or
white liquid filled vesicles. In a few days the vesicles rupture and form painful ulcers, 1 to 3
mm in diameter, which are covered with a whitish gray membrane and have a circumscribed
area of inflammation. The ulcers may be observed on any area of the mucous membrane,
including buccal mucosa, tongue, lips, hard and soft palate, and the tonsillar areas. Large
ulcerated lesions may occasionally be observed on the palate or gingival tissues or in the region
of the mucobuccal fold. This distribution makes the differential diagnosis more difficult. An
additional diagnostic criterion is a fourfold rise of serum antibodies to HSV-1. The lesion
culture will also show positive results for HSV-1.
Treatment of acute herpetic gingivostomatitis in children:
1. Specific antiviral medication such as, acyclovir, famciclovir, and valacyclovir. These
medications inhibit viral replication in cells infected with the virus. Acyclovir (Zovirax*)
should be administered in 5 daily doses to equal 1000 mg per day for 10 days. Acyclovir is
available in capsules or
Suspension.
2.
Bed rest and isolation from other children in the family are also recommended.
3.
provision for the relief of the acute symptoms so that fluid and nutritional intake can be
maintained.
The application of a mild topical anesthetic, such as dyclonine hydrochloride
(0.5%) (Dyclone) before mealtime will temporarily relieve the pain and allow the child to take
in soft food. Another topical anesthetic, lidocaine ( Xylocaine Viscous), can be prescribed for
the child who can hold 1 teaspoon of the anesthetic in the mouth for 2 to 3 minutes and then
expectorate the solution
4. systemic analgesics (acetaminophen or ibuprofen)
5. Because fruit juices are usually irritating to the ulcerated area, ingestion of a vitamin
supplement during the course of the disease is indicated.

4
After the initial primary attack during early childhood, the herpes simplex virus becomes
inactive and resides in sensory nerve ganglia. The virus will often reappear later as the familiar
cold sore or fever blister, usually on the outside of the lips. Thus the disease has been
commonly referred to as recurrent herpes labialis (RHL). However, approximately 5% of
recurrences are intraoral. With the recurring attacks, the sores develop in essentially the same
area.
The recurrence of the disease has often been related to conditions of
emotional stress
and lowered tissue resistance resulting from various types of trauma.
Excessive exposure to sunlight may be responsible for the appearance of the recurrent
herpetic lesions on the lip. Use of sunscreen can prevent sun-induced recurrences.
Lesions on the lip may also appear after dental treatment and may be related to irritation
from rubber dam material or even routine daily procedures.
Dentists and dental auxiliaries without a history of herpetic lesions might benefit from
serologic testing. Considering the occupational disability that
often accompanies HSV-1 infection of the finger or eye, effective barrier protection for health
professionals is important.
RECURRENT APHTHOUS ULCER (CANKER SORE)
The recurrent aphthous ulcer (RAU)
—also referred to as recurrent aphthous stomatitis
(RAS)
—is a painful ulceration on the unattached mucous membrane that occurs in school-aged
children and adults. The peak age for RAU is between 10 and 19 years of age. It has been
reported to be the most common mucosal disorder in people of all ages and races in the world.
This disorder , is characterized by
recurrent ulcerations on the moist mucous membranes of the mouth,
in which both discrete and confluent lesions form rapidly in certain sites and feature a
round to oval crateriform base,
raised reddened margins,
and pain.
They may appear as attacks of minor or single, major or multiple, or herpetiform
lesions.
They may or may not be associated with ulcerative lesions elsewhere.
The description
of RAU frequently includes the term canker sores

5
The cause of RAU is unknown.
Local and systemic conditions and genetic,
immunologic,
nutritional
deficiencies of iron, vitamin B72, and folic acid.
and infectious microbial factors
are the most common precipitating factors.
Local factors include trauma
and injuries caused by cheek biting and minor facial
irritations ,
allergy to toothpaste constituents (sodium lauryl sulfate),
and salivary gland dysfunction considered to be
the most common precipitating factors.
Stress may prove to be an important precipitating factor, particularly in stress-prone
groups, such as students in professional schools and military personnel.
Treatment of RECURRENT APHTHOUS ULCER (CANKER SORE)
Current treatment is focused on promoting ulcer healing, reducing ulcer duration and
patient pain, maintaining the patient's nutritional intake, and preventing or reducing the
frequency of recurrence of the disease.
1.Topical antiinflammatory and analgesic medicines and/or
2. systemic immunomodulating and immunosuppression agents have been used for RAU.
The primary line of treatment uses topical gels, creams, and ointments
as antiinflammatory agents. Currently, a topical corticosteroid is applied to the area with a
mucosal adherent (e.g., isobutyl cyanoacrylate, Orabase). For example, the application of
triamcinolone acetonide ( Kenalog in Orabase) to the surface of the lesions before meals and
before sleeping may also be helpful
Topical rinses have also been helpful for relief of RAU. Sucralfate has proved useful by
coating the area.
The topical application of tetracyclines to the ulcers is often helpful in reducing the pain
and in shortening the course of the disease.
ACUTE NECROTIZING ULCERATIVE GINGIVITIS (VINCENT
INFECTION)
The infectious disease commonly referred to as acute necrotizing ulcerative gingivitis
(ANUG) is rare among preschool children, occurs occasionally in children 6 to 12 years old, and
is common in young adults.
ANUG can be easily diagnosed because of the involvement of the interproximal papillae and
the presence of a pseudomembranous necrotic covering of the marginal tissue
6
The clinical manifestations of the disease include
inflamed,
painful,
bleeding gingival tissue,
poor appetite,
fever as high as 40° C (104° F),
general malaise,
and a fetid odor.
The disease responds dramatically within 24 to 48 hours to
subgingival curettage, debridement,
and the use of mild oxidizing solutions.
If the gingival tissues are acutely and extensively inflamed when the patient is first seen,
antibiotic therapy is indicated.
Improved oral hygiene, the use of mild oxidizing mouthrinses after each meal, and twice-daily
rinsing with chlorhexidine will aid in overcoming the infection.
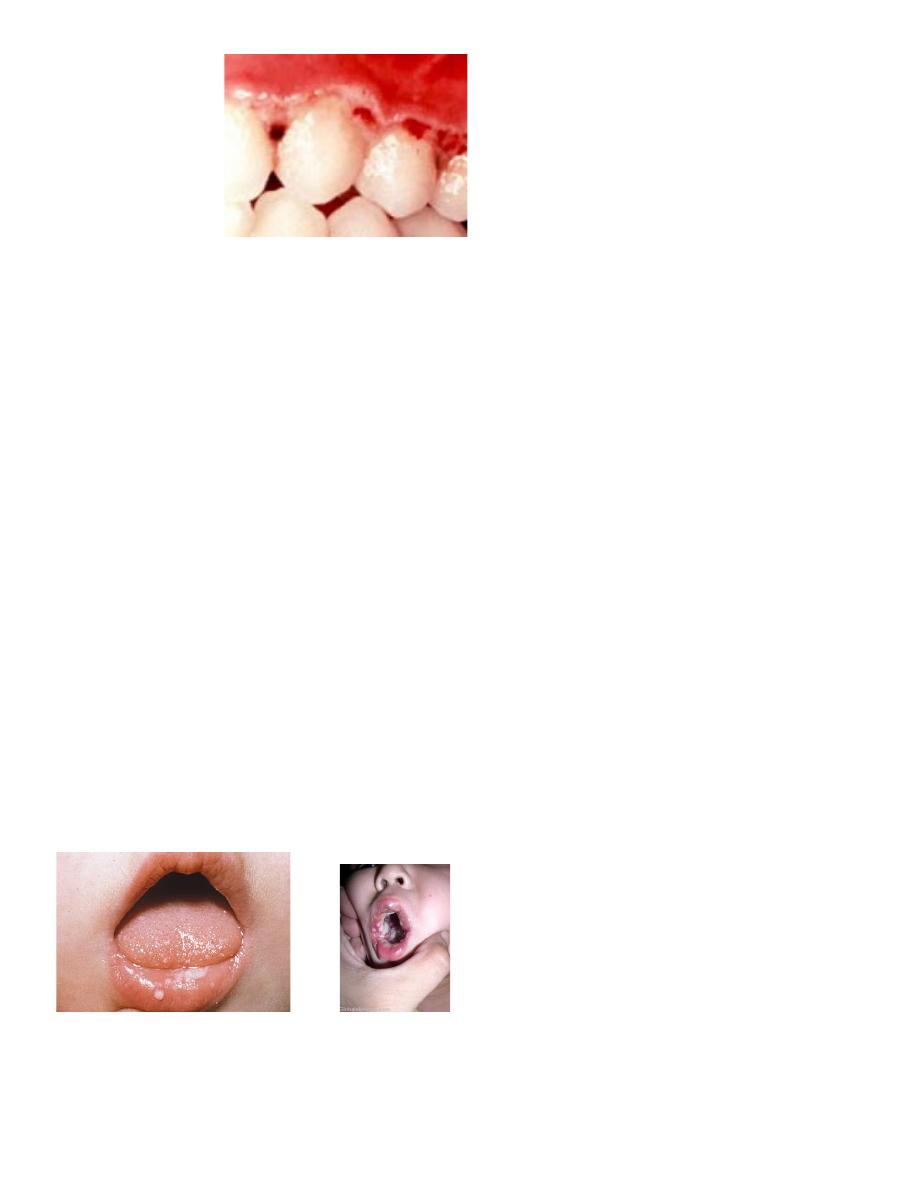
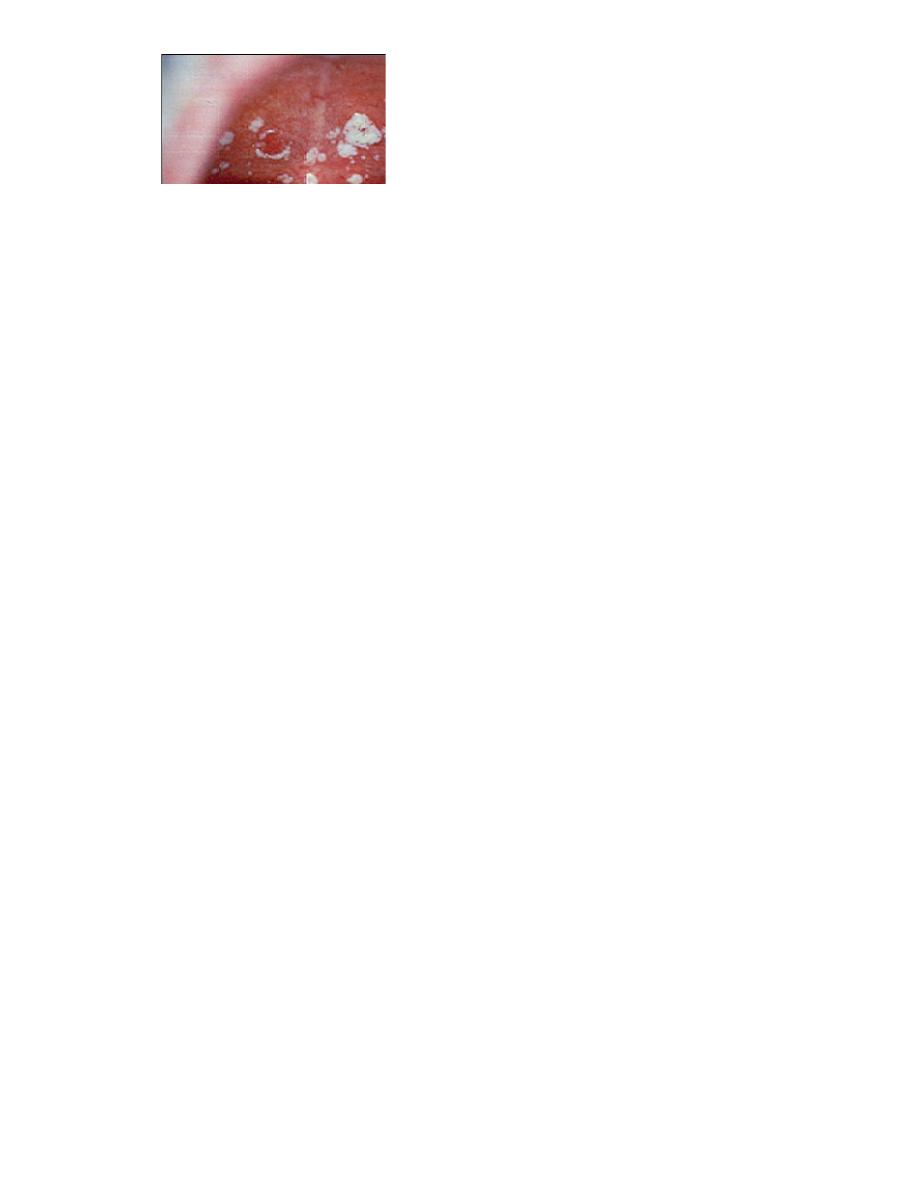
ACUTE CANDIDIASIS (THRUSH, CANDIDOSIS, MONILIASIS)
Candida (Monilia) albicans is a common inhabitant of the oral cavity but may multiply
rapidly and cause a pathogenic state when tissue resistance is lowered. Young children
sometimes develop thrush after local antibiotic therapy, which allows the fungus to proliferate.
The lesions of the oral disease appear as raised, furry, white patches, which can be removed
easily to produce a bleeding underlying surface. Neonatal candidiasis, contracted during
passage through the vagina and erupting clinically during the first 2 weeks of life, is a common
occurrence. This infection is also
common in immunosuppressed patients.
7
Antifungal antibiotics are available to control thrush.
*For infants and very young children, a suspension of 1 ml (100,000 U) of nystatin
(Mycostatin) may be dropped into the mouth for local action four times a day. The drug is
nonirritating and nontoxic. Clotrimazole sus-pension (10 mg/ml), 1 to 2 ml applied to affected
areas four times daily, is an effective antifungal medication.* Systemic fluconazole suspension
(10 mg/ml) is safe to use in infants at a total dosage of 6 mg/kg or less per day.
* For children old enough to manage solid medication allowed to dissolve in the mouth,
clotrimazole troches or nystatin pastilles are recommended, because the therapeutic agent
remains in the saliva longer than with the liquid medication.
*For children old enough to swallow, systemic fluconazole (100-mg tablets) in a 14-day
course may be prescribed for patients whose infection has not responded to topical antifungal
agents.
ACUTE BACTERIAL INFECTIONS
The prevalence of acute bacterial infection in the oral cavity is unknown. Researchers
reported acute streptococcal gingivitis with painful, vivid red gingivae that bled easily, The
papillae had enlarged, and gingival abscesses had developed. Cultures showed a predominance
of hemolytic streptococci. Acute infections of this type may be more common than was
previously realized. Littner et al reported five cases, all in adults between 20 and 27 years of
age.- The diagnosis is difficult to make, however, without extensive laboratory tests.
1.Broadspectrum antibiotics are recommended if the infection is believed to be bacterial in
origin.
2.Improved oral hygiene is important in treating the infection. As with any acute microbial
oral infection,
3.chlorhexidine mouthrinses are also appropriate.
4.The placement of dental restorations to restore adequate function and contour after the
reduction of acute symptoms is equally important.
