
1
Lec. 2 Dr.Abeer Zwain
CHRONIC NONSPECIFIC GINGIVITIS
A type of gingivitis commonly seen during the preteenage and teenage years is often referred
to as chronic nonspecific gingivitis. The chronic gingival inflammation may be localized to the
anterior region, or it may be more generalized. Although the condition is rarely painful,
the fiery
red gingival lesion is not accompanied by enlarged interdental labial papillae or closely
associated with local irritants. The gingivitis showed little improvement after aprophylactic
treatment, it may persist for long periods without much improvement.
The cause of gingivitis is complex and is considered to be based on a multitude of local and
systemic factors. Possible factors could be:
* hormonal imbalance.
* Inadequate oral hygiene, which allows food impaction and the accumulation of materia alba
and bacterial plaque, is undoubtedly the major cause of this chronic type of gingivitis.
*They discovered that the chronic gingivitis group had a larger percentage of AB blood types
and a smaller percentage of 0 blood type than the control group.
*Insufficient quantities of fruits and vegetables in the diet, leading to a subclinical vitamin
deficiency, may be an important predisposing factor. An improved dietary intake of vitamins
and the use of multiple-vitamin supplements will improve the gingival condition in many
children.
*Malocclusion, which prevents adequate function, and crowded teeth, which make oral hygiene
and plaque removal more difficult, are also important predisposing factors in gingivitis.
* Carious lesions with irritating sharp margins, as well as faulty restorations with overhanging
margins (both of which cause food accumulation), also favor the development of the chronic
type of gingivitis.
* mouth breathing is often responsible for the development of
the chronic hyperplastic form of
gingivitis, particularly in the maxillary arch.
All these factors should be considered contributory to chronic nonspecific gingivitis and
should be corrected in the treatment of the condition.
GINGIVAL DISEASES MODIFIED
BY SYSTEMIC FACTORS
GINGIVAL DISEASES ASSOCIATED
WITH THE ENDOCRINE SYSTEM
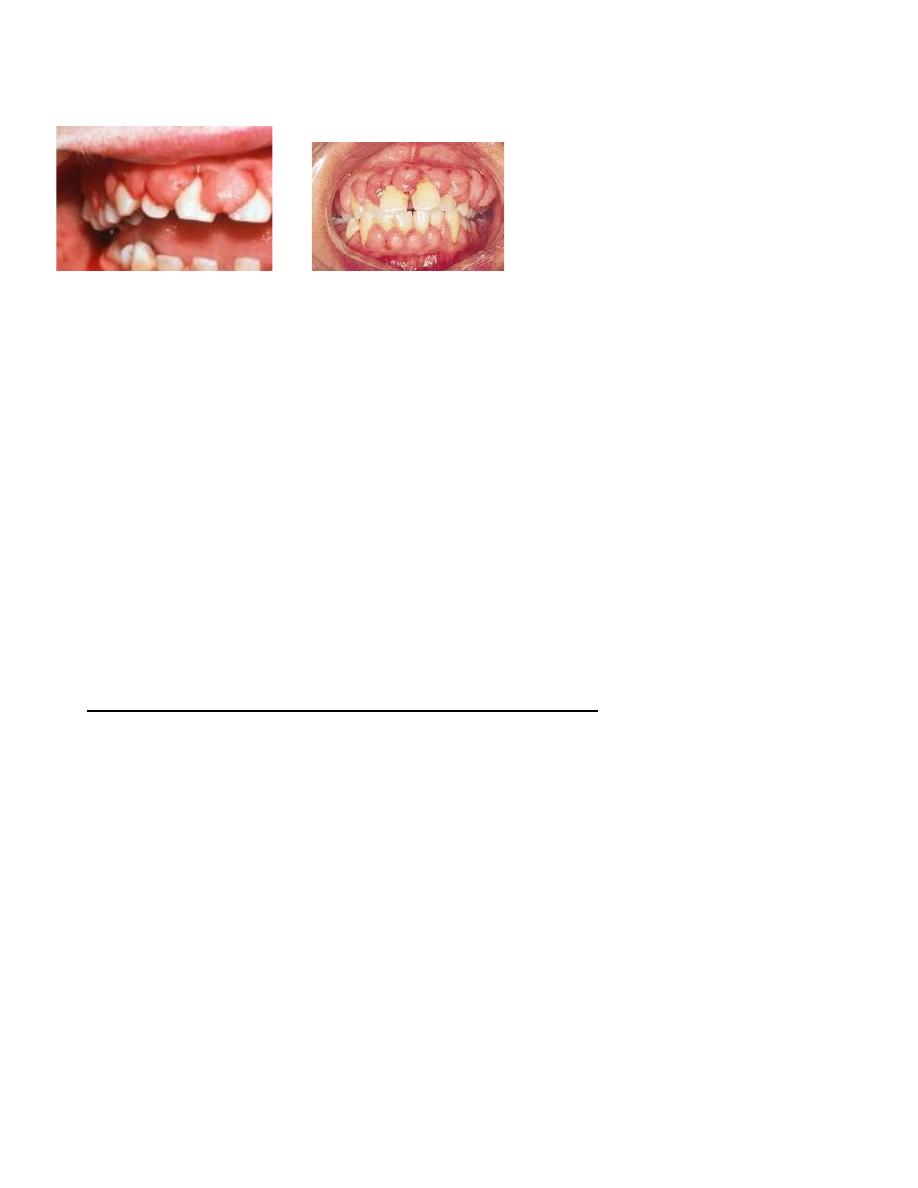
Puberty gingivitis is a distinctive type of gingivitis that occasionally develops in children in
the prepubertal and pubertal period.
The gingival enlargement is marginal in distribution and, in
the presence of local irritants, was characterized by prominent bulbous interproximal papillae
far greater than gingival enlargements associated with local factors.

2
Treatment of puberty gingivitis should be directed toward improved oral hygiene, removal of
all local irritants, restoration of carious teeth, and dietary changes necessary to ensure an
adequate nutritional status. Severe cases of hyperplastic gingivitis that do not respond to local
or systemic therapy should be treated by gingivoplasty.
GINGIVAL LESIONS OF GENETIC ORIGIN Hereditary
gingival fibromatosis (HGF) is characterized by a slow, progressive, benign enlargement of
the gingivae. Genetic and pharmacologically induced forms of gingival enlargement are known.
The gingival tissues appear normal at birth but begin to enlarge with the eruption of the primary
teeth. Although mild cases are observed, the gingival tissues usually continue to enlarge with
eruption of the permanent teeth until the tissues essentially cover the clinical crowns of the
teeth. The dense fibrous tissue often causes displacement of the teeth and malocclusion. The
condition is not painful until the tissue enlarges to the extent that it partially covers the
occlusalsurface of the molars and becomes traumatized during mastication.
Surgical removal of the hyperplastic tissue achieves a more favorable oral and facial
appearance. However, hyperplasia can recur within a few months after the surgical procedure
and can return to the original condition within a few years.
PHENYTOIN-INDUCED GINGIVAL OVERGROWTH( PIGO)
Phenytoin (Dilantin, or diphenylhydantoin), a major anticonvulsant agent used in the
treatment of epilepsy. Varying degrees of gingival hyperplasia, one of the most common side
effects of phenytoin therapy. Most investigators agree on the existence of a close relationship
between oral hygiene and PIGO. PIGO can be decreased or prevented by scrupulous oral
3
hygiene and dental prophylaxis. The relationship between plaque, local irritants, and PIGO is
also supported by the observation that patients without teeth almost never develop PIGO.
PIGO, when it does develop, begins to appear as early as 2 to 3 weeks after initiation of
phenytoin therapy and peaks at 18 to 24 months.
painless enlargement of the interproximal gingiva
The buccal and anterior segments are more often affected
As the interdental lobulations grow, clefting becomes apparent at the midline of the tooth
In some cases, the entire occlusal surface of the teeth becomes covered.
PIGO may impose problems of
esthetics,
difficulty in mastication,
speech impairment,
delayed tooth eruption, tissue trauma, and secondary inflammation leading to periodontal
disease.
dental treatment based on clinical oral signs and symptoms
Patients with mild PIGO (i.e., less than one third of the clinical crown is covered) require
daily meticulous oral hygiene and more frequent dental care.
For patients with moderate PIGO (i.e., one third to two thirds of the clinical crown is
covered)
meticulous oral home care
and the judicious use of an irrigating device may be needed.
In addition, prophylaxis and topical stannous fluoride application is
recommended.
If there has been no change, consultation with the patient's physician concerning
the possibility of using a different anticonvulsant drug may be helpful.
If no improvement occurs, surgical removal of the overgrowth
may be recommended.
For patients with severe PIGO (i.e., more than two thirds of the tooth is covered) who do
not respond to the previously mentioned therapeutic regimens, surgical removal is
necessary.
Gradual recurrences of the fibrous tissue usually follow the treatment.

4
There is success in controlling the gingival overgrowth with positive-pressure appliances.
Other drugs that have been reported to induce gingival overgrowth in some patients include
cyclosporin, calcium channel blockers, valproic acid, and phenobarbital. As with all disorders
affecting periodontal tissues, maintaining excellent oral hygiene is the primary key to successful
therapy.
ASCORBIC ACID DEFICIENCY
GINGIVITIS
Scorbutic gingivitis is associated with vitamin C deficiency and differs from the type of
gingivitis related to poor oral hygiene.
The involvement is usually limited to the marginal tissues and papillae.
The child with scorbutic gingivitis may complain of severe pain,
and spontaneous hemorrhage will be evident.
Complete dental care, improved oral hygiene, and supplementation with vitamin C(the daily
administration of 250 to 500 mg of ascorbic acid ) and other watersoluble vitamins will greatly
improve the gingival condition.
PERIODONTAL DISEASES
IN CHILDREN
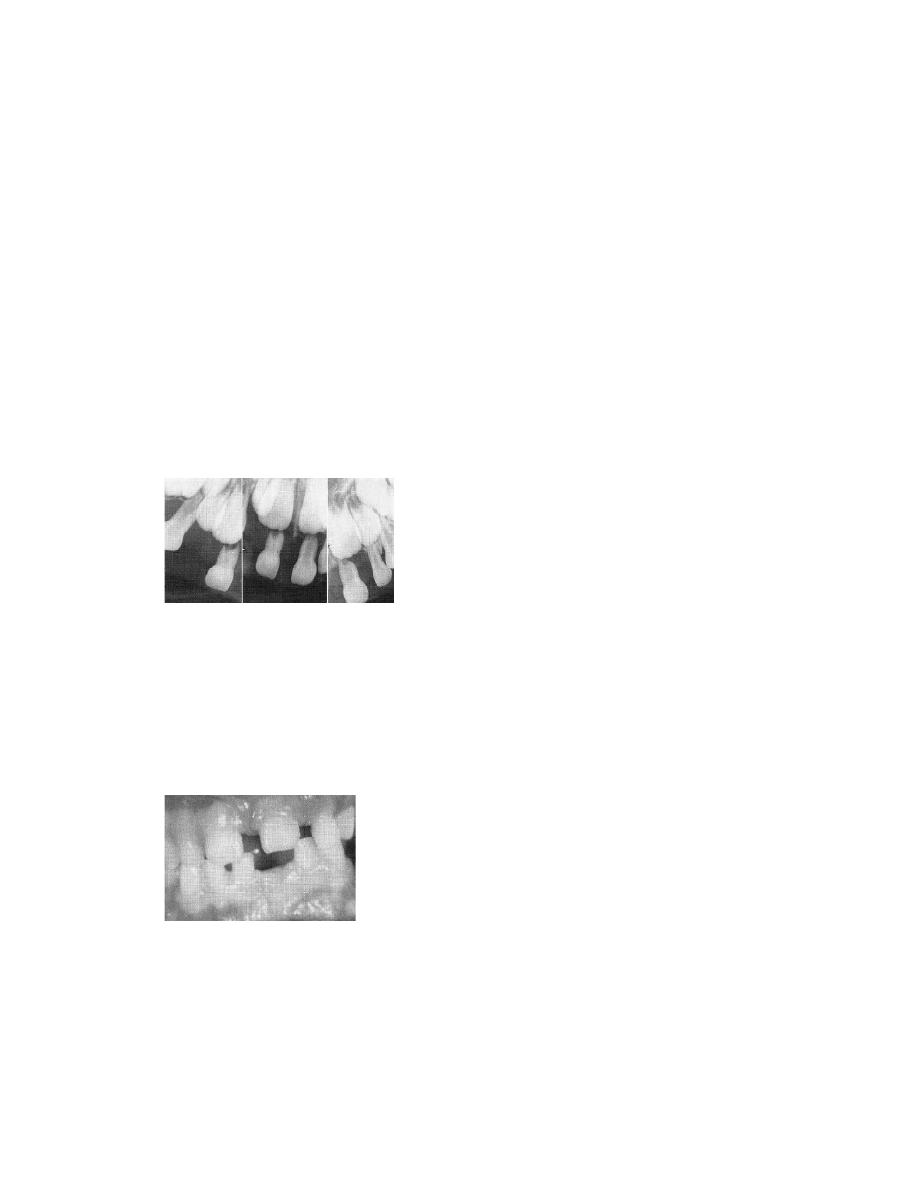
Periodontitis, an inflammatory disease of the gingiva and deeper tissues of the
periodontium, is characterized by pocket formation and destruction of the supporting alveolar
bone. Bone loss in children can be detected in bite-wing radiographs by comparing the height of
the alveolar bone to the cementoenamel junction.
Distances between 2 and 3 mm can be defined as questionable bone loss and distances
greater than 3 mm indicate definite bone loss.
5
AGGRESSIVE PERIODONTITIS
(EARLY-ONSET PERIODONTITIS)
EOP is used as a generic term to describe a heterogeneous group of periodontal disease
occurring in young individuals who are otherwise healthy. EOP can be viewed as :
(1) a localized form (localized juvenile periodontitis [LJP]),
(2) a generalized form (generalized juvenile periodontitis [ GJPI)
the prevalence of aggressive periodontitis in adolescent schoolchildren in the United States is
more in African Americans than in whites and more in boys than in girls.
Aggressive periodontitis of the primary dentition can occur in a localized form but is
usually seen in the generalized form.
LAP is localized attachment loss and alveolar bone loss only in the primary
dentition in an otherwise healthy child.
The exact time of onset is unknown, but it appears to arise around or before 4 years
of age, when the bone loss is usually seen on radiographs around the primary
molars and/or incisors.
Abnormal probing depths with minor gingival inflammation, rapid bone loss, and
minimal to various amounts of plaque have been demonstrated at the affected sites
of the child’s dentition.
Abnormalities in host defenses (e.g., leukocyte chemotaxis), extensive proximal
caries facilitating plaque retention and bone loss, and a family history of
periodontitis have been associated with LAP in children.
As the disease progresses, the child’s periodontium shows signs of gingival
inflammation, with gingival clefts and localized ulceration of the gingival margin.
GENERALIZED AGGRESSIVE PERIODONTITIS
The onset of GAP is during or soon after the eruption of the primary teeth.
It results in severe gingival inflammation and generalized attachment loss,
tooth mobility, and rapid alveolar bone loss with premature exfoliation of
the teeth.
The gingival tissue may initially demonstrate only minor inflammation with
plaque accumulation at a minimum.

6
It often affects the entire dentition.
Alveolar bone destruction proceeds rapidly, and the primary teeth may be
lost by 3 years of age.
Because of its wide distribution and rapid rate of alveolar bone destruction,
the GAP was previously known as generalized juvenile periodontitis, severe
periodontitis, and rapidly progressive periodontitis.
Chronic cases display the presence of clefting and pronounced recession
with associated acute inflammation.
Affected teeth harbor more nonmotile, facultative, anaerobic, gram-negative
rods (especially Porphyromonas gingivalis) in GAP than in LAP.
Microorganisms predominating in the gingival pockets include
Aggregatibacter
actinomycetemcomitans
(Aa),
Porphyromonas
(Bacteroides) gingivalis (Pg), Bacteroides melaninogenicus, Prevotella
intermedia, Capnocytophaga sputigena, and Fusobacterium nucleatum.
the major periodontal pathogens are transmitted among family members.
The past medical history of the child often reveals a history of recurrent
infections (e.g., otitis media, skin infections, upper respiratory tract
infections).
LAP and GAP are distinctly different radiographically and clinically.
Neutrophils in GAP patients have suppressed.
Individuals with GAP exhibit marked periodontal inflammation and have
heavy accumulations of plaque and calculus. Testing may reveal a high
prevalence of leukocyte adherence abnormalities and an impaired host
response to bacterial infections.
