Cardiovascular DisordersLab 10
Myocardial InfarctionSequence of gross:
Earliest time that can detect MI = after 3 hours grossly by immersion of slices in triphenyl tetrazolium chloride, the intact area red due to effect of lactate dehydrogenase.12-24 hours visualized grossly as reddish blue discoloration.
Then progressively more sharply delineated as yellow tan soft area, that in 10-14 days become rimmed by red granulation tissue.
In succeeded weeks become fibrous in nature.
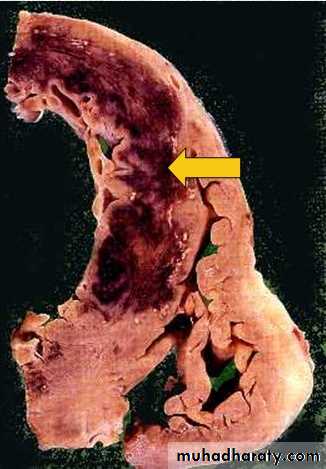
Myocardial Infarction - early
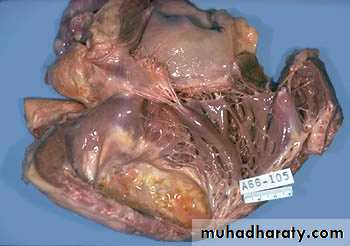
This cross section through the heart demonstrates the left ventricle on the left. Extending from the anterior portion and into the septum is a large recent myocardial infarction. The center is tan with surrounding hyperemia. The infarction is "transmural" in that it extends through the full thickness of the wall.
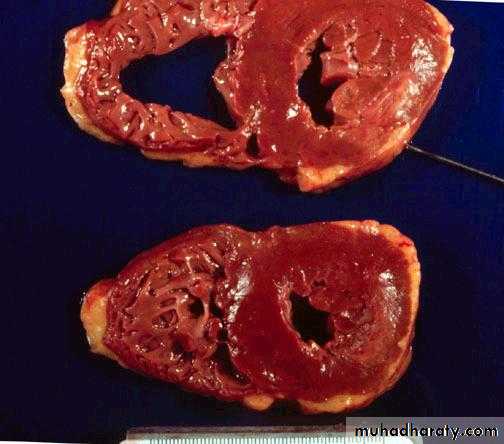
Myocardial Infarction 3d
Hemorrhage in infarction seen extended from anterior wall to septum.
Myocardial Infarction – 1 wks.
Thin, yellow infarct seen by arrowsMyocardial Infarction
2wkTough white
fibrous tissueseen by arrow
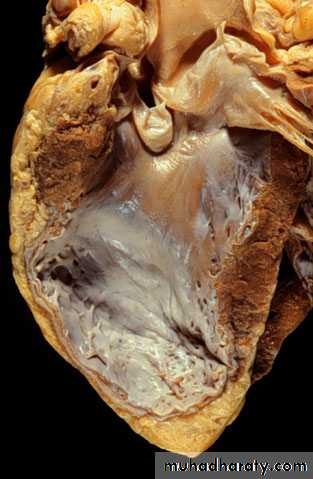
There has been a remote myocardial infarction that extensively involved the anterior left ventricular free wall and septum. The white appearance of the endocardial surface indicates the extensive scarring.
Coronary artery atherosclerosis and thrombosis:
This epicardial coronary artery is almost completely occluded by atherosclerotic plaque.The plaque looks pale and covered by eroded surface that induces release of thrombogenic substances into the narrow lumen that causes thrombus formation.
A thrombus has occluded the tiny lumen that remains.
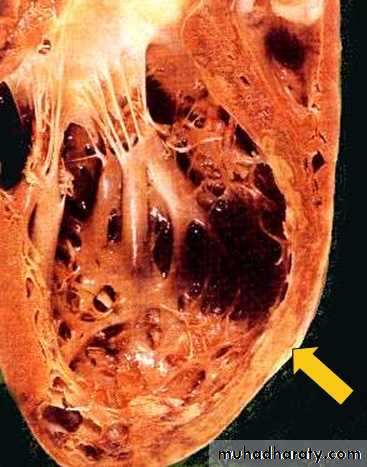
Heart, acute myocardial infarct - Gross, cut surface
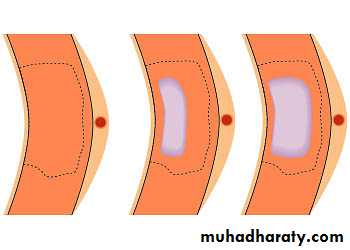
This image shows an acute myocardial infarct in the free wall of the left ventricle, which also has an element of left ventricular hypertrophy. The infarct zone is pale tan, and it is surrounded by a hyperemic area that represents an inflammatory response. The infarct is about 5-7 days old.The wavefront of myocardial necrosis - Schematic
The subendocardial zones become irreversibly damaged first. There is progressive loss of the myocardial zone at risk over the next 24 hours, with most of the damage occurring in the first 4-6 hours.Sequence of microscopical features: in routine ex.
Ultrastructural evidence of irreversible myocardial damage can be detected 20 to 40 minutes after occlusion of a major epicardial coronary artery.4-12 hours = coagulative necrosis, with wavy fibers start at edges of infarct.
1-3 days = necrotic muscle elicit acute inflammation, followed by wave of macrophage.
5-10 days most pronounced in 5-10 days.
2-3 weeks = most pronounced replacement by granulation tissue.
End of 6th week well formed scar. (vary with size).
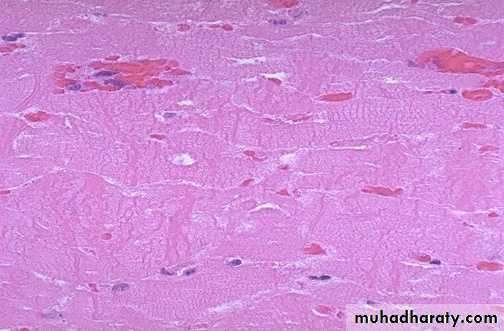
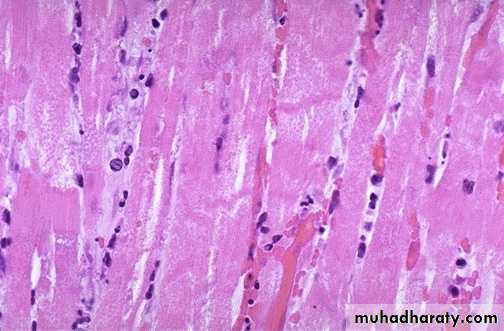
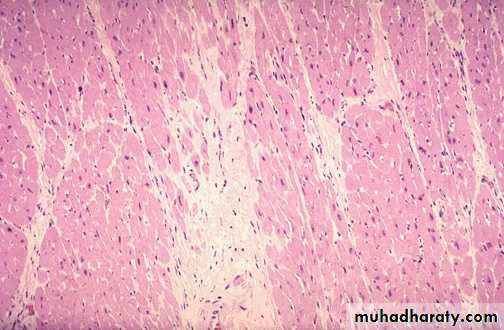
The earliest change histologically seen with acute myocardial infarction in the first day is contraction band necrosis. The myocardial fibers are beginning to lose cross striations and the nuclei are not clearly visible in most of the cells seen here. Many irregular darker pink wavy contraction bands extending across the fibers.
Heart, contraction band necrosis - High power
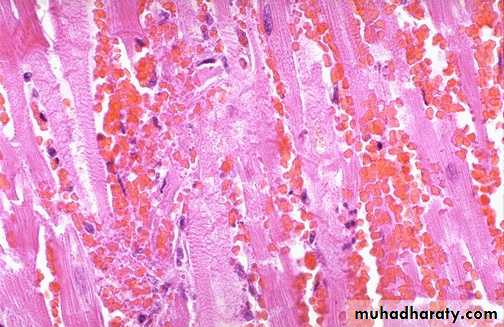
Contraction bands are bright eosinophilic bands of condensed contractile proteins that run at right angles to the long axis of the cardiac myocyte. They form in zones of myocardium irreversibly injured by ischemia and then reperfused after angioplasty or clot-lysing drugs such as tissue plasminogen activator. Hemorrhage and contraction bands are common in reperfused infarcts.Heart, acute myocardial infarction - Medium power
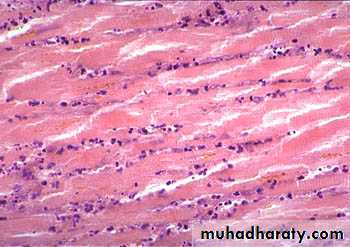
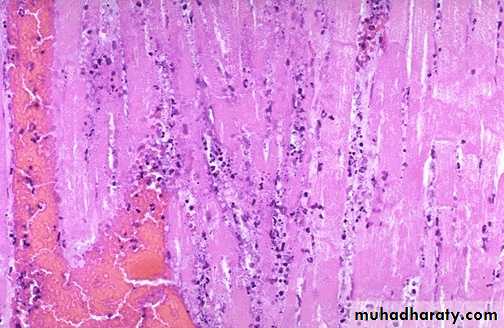
This photomicrograph shows a zone of coagulative necrosis. There are numerous neutrophils between necrotic myocytes. Neutrophils are prominent in the first few days of a myocardial infarct.Heart, contraction band necrosis - High power
Contraction bands are bright eosinophilic bands of condensed contractile proteins that run at right angles to the long axis of the cardiac myocyte. They form in zones of myocardium irreversibly injured by ischemia and then reperfused after angioplasty or clot-lysing drugs such as tissue plasminogen activator. Hemorrhage and contraction bands are common in reperfused infarcts.post myocardial infarction rupture of left ventricular free wall - Gross, cut surface
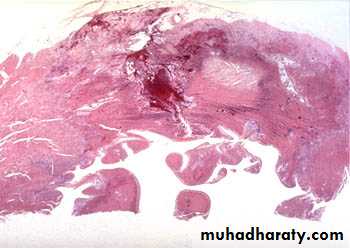
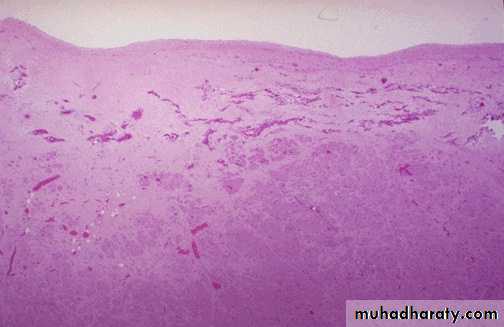
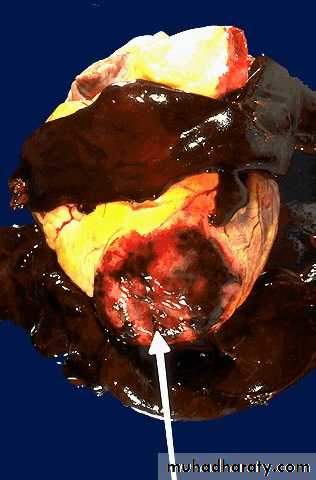
A myocardial rupture has occurred at an interface between necrotic and spared myocardium. The infarct zone is pale. The zone of rupture is dark red-black. There is left ventricular hypertrophy except in the zone of infarct, which shows significant thinning. Myocardial rupture is an uncommon but catastrophic and rapidly fatal complication of acute myocardial infarction. The pericardium rapidly fills with blood (hemopericardium). When the pericardium fills with blood, the right ventricle cannot fill, and the patient rapidly loses cardiac output. Hypertension is a risk factor for myocardial rupture.myocardial rupture - Very low power
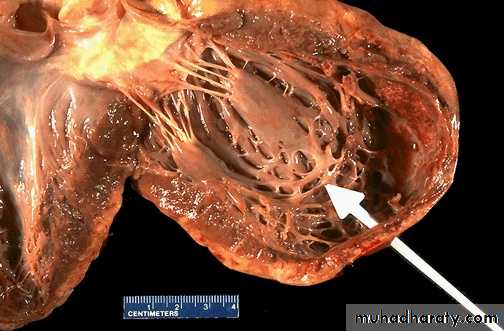
A hemorrhagic zone of rupture is located in the center of the image. On one side of the rupture channel is a region of almost transmural myocardial infarction with a central zone of coagulative necrosis. On the other side of the rupture channel is a zone of viable myocardium. Rupture often takes place where there is a sharp interface between normal and weakened necrotic myocardium.left ventricular aneurysm with thrombus - Gross, endocardial surface
The aneurysm is a large oval zone located toward the apex of the left ventricle. An aneurysm forms when a region of the left ventricular wall is weakened by infarction and then thinned by the constant pressure of systolic contractions. Aneurysms at any site are often areas of abnormal flow and thus are predisposed to thrombosis. The aneurysm in this case has been filled by an organizing thrombus. Left ventricular thrombi can generate systemic emboli. Ventricular wall aneurysms may also cause congestive heart failure and dangerous arrhythmias.This high power microscopic view of the myocardium demonstrates an infarction of about 1 to 2 days in duration. The myocardial fibers have dark red contraction bands extending across them. The myocardial cell nuclei have almost all disappeared. There is beginning acute inflammation
In this microscopic view of a recent myocardial infarction, there is extensive hemorrhage along with myocardial fiber necrosis with contraction bands and loss of nuclei (1-2days).
This myocardial infarction is about 3 to 4 days old. There is an extensive acute inflammatory cell infiltrate and the myocardial fibers are so necrotic that the outlines of them are only barely visible.
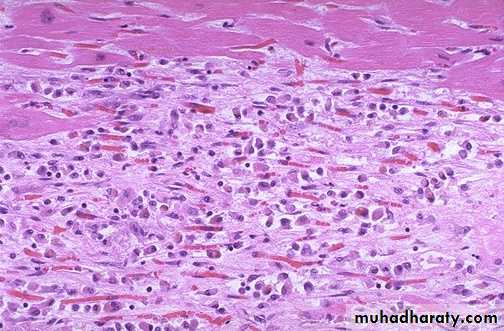
This is an intermediate myocardial infarction of 1 to 2 weeks in age. Note that there are remaining normal myocardial fibers at the top. Below these fibers are many macrophages along with numerous capillaries and little collagenization (Resorption, fibrosis).
There is pale white collagen within the interstitium between myocardial fibers. This represents an area of remote infarction (remote)
The myocardium beneath the endocardial surface at the top demonstrates pale fibrosis with
collagenization following healing of a subendocardial myocardial infarction (remote}.• One complication of a transmural myocardial infarction is rupture of the myocardium. This is most likely to occur in the first week between 3 to 5 days following the initial event, when the myocardium is the softest. The white arrow marks the point of rupture in this anterior-inferior myocardial infarction of the left ventricular free wall and septum. Note the dark red blood clot forming the hemopericardium. The hemopericardium can lead to tamponade.
In cross section, the point of rupture of the myocardium is shown with the arrow. In this case, there was a previous myocardial infarction 3 weeks before, and another myocardial infarction occurred, rupturing through the already thin ventricular wall 3 days later.
There has been a previous extensive transmural myocardial infarction involving the free wall of the left ventricle. The thickness of the myocardial wall is normal superiorly, but inferiorly is only a thin fibrous wall. The infarction was so extensive that, after healing, the ventricular wall was replaced by a thin band of collagen, forming an aneurysm. Such an aneurysm represents non-contractile tissue that reduces stroke volume and strains the remaining myocardium. The stasis of blood in the aneurysm predisposes to mural thrombosis.