Pulmonary Tumors
lungs are frequently the site of metastases from cancers in extra thoracic organsprimary lung cancer is also a common disease.
95% of primary lung tumors arise from the bronchial epithelium (bronchogenic carcinomas); the remaining 5% are a miscellaneous group that includes bronchial carcinoids, &other.Bronchogenic Carcinoma
Epidemiology:
The most frequently diagnosed cancers and the most common cause of cancer mortality .Age incidence is 40-70 years.5-year survival rate for all stages combined is only 15%The male-to-female ratio is about 2:1 but the rate of increase among males is slowing down, but it continues to accelerate among females.
At diagnosis, greater than 50% of patients already have distant metastatic disease.
Classification:
1. Squamous cell carcinoma2. Small cell carcinoma
i) Pure
ii) Combined (with any other non-small cell carcinoma )
3. Adenocarcinoma
i) Acinar predominant
ii) Papillary predominant
iii) Lepidic predominant (formerly bronchiolo-alveolar
carcinoma)
iv) Solid predominant with mucin formation
v) Micropapillary predominant
4. Large cell carcinoma
5. Adenosquamous carcinoma
For therapeutic purposes, bronchogenic carcinomas are classified into two broad groups: small cell lung cancer (SCLC) and non-small cell lung cancer (NSCLC).
WHY?
For reasons not entirely understood, adenocarcinoma has replaced squamous cell carcinoma as the most common primary lung tumor in recent years.
Adenocarcinomas are also by far the most common primary tumors arising in:
Women.In lifetime nonsmokers.
Patients younger than 45 years.
Etiology and Pathogenesis
Bronchogenic carcinomas, similar to cancers at many other anatomic sites, arise by a stepwise accumulation of genetic abnormalities that result in transformation of benign bronchial epithelium into neoplastic tissue.RISK FACTORS
SmokingAir pollution
Radiation exposureOccupational causes
Dusts containing Asbestos , arsenic, chromium, uranium, nickel, vinyl chloride, and mustard gasDietary factors
Chronic scarring Peripheral adenocarcinomas occur
more frequently in areas of chronic scarring caused by chronicinflammatory changes, old tuberculosis, asbestosis.
SMOKING:
Statistical, clinical, and experimental evidence incriminates cigarette smoking.About 90% of lung cancers occur in active smokers . Passive smoking increases the risk of developing lung cancer to approximately twice that of nonsmokers
Total dose: linear correlation between the frequency of lung cancer and pack-years of cigarette smoking. The risk becomes 60 times greater among habitual heavy smokers (two packs a day for 20 years) compared with nonsmokers.
Cessation of smoking decreases the risk of developing lung cancer over time, but it may never return to baseline levels.
PIPE smokers
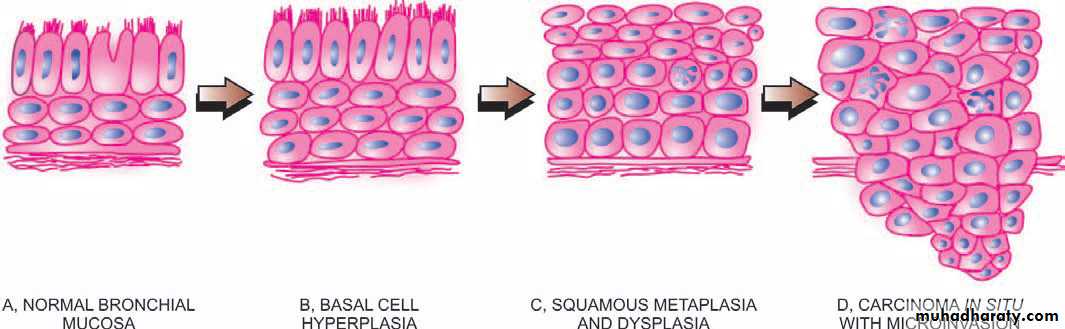
Smoking results in progressive alterations in the lining epithelium of the respiratory tract: basal cell hyperplasia and squamous metaplasia and progress to squamous dysplasia and carcinoma in situ, culminating in invasive cancer.Squamous and small cell carcinomas show the strongest association with tobacco exposure.
Squamous cell carcinomas
Men > women.Smoking.
Preceded for years by squamous metaplasia or dysplasia in the bronchial epithelium, which then transforms to carcinoma in situ.Gross:
Typically central in location (major bronchi), frequently presenting with bronchial obstruction, and may undergo central necrosis, giving rise to cavitation.cavitation.
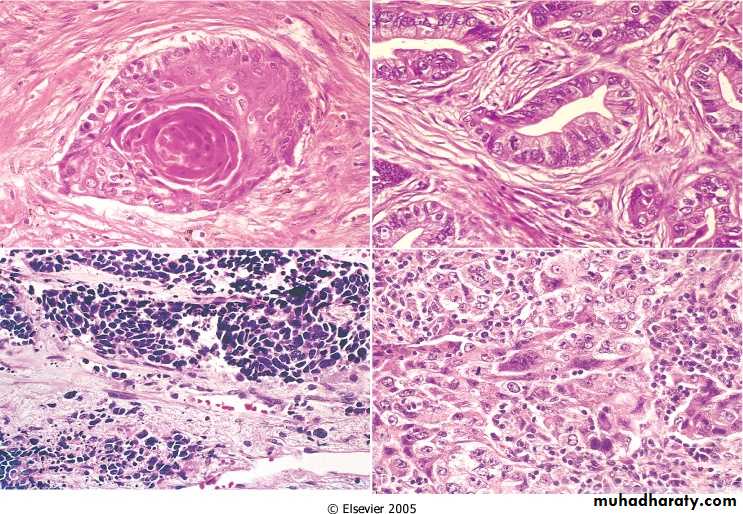
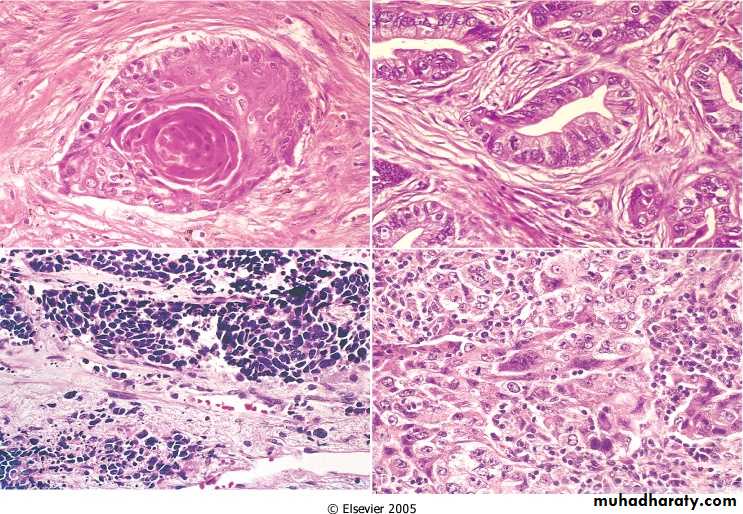
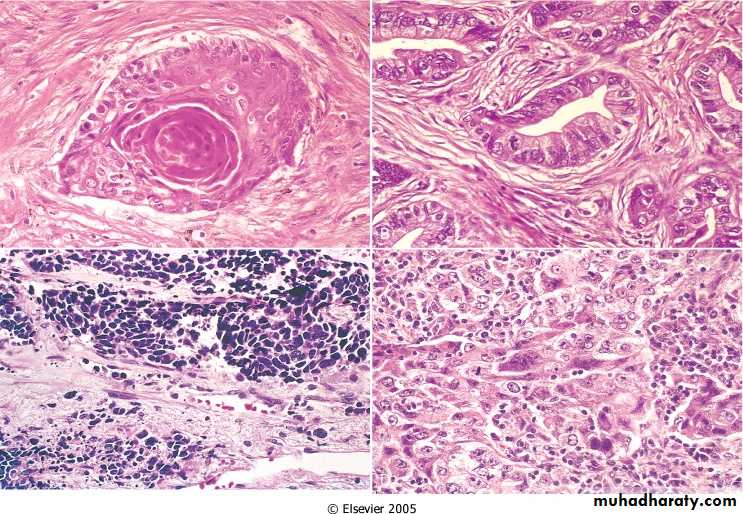
Histologically:These tumors range from well-differentiated squamous cell neoplasms showing keratin pearls and intercellular bridges to poorly differentiated neoplasms having only minimal residual squamous cell features.
Adenocarcinomas
They have the weakest association with a previous history of smoking.Female & young.
Mostly peripheral in location, sometimes originating in areas of pre-existing lung scarring ("scar carcinomas").In general, these tumors grow slowly and form smaller masses.
Histologically:
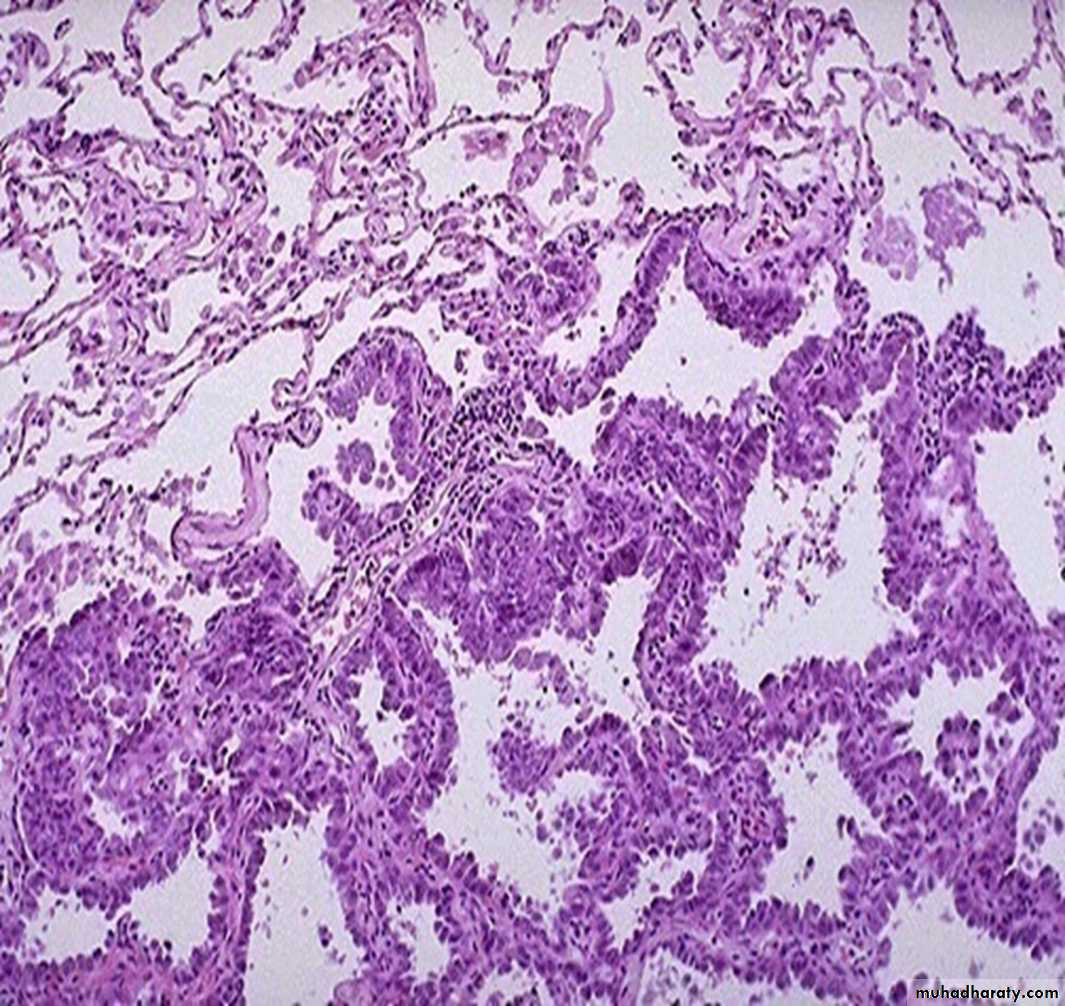
They assume a variety of forms, including acinar (gland forming), papillary, and solid types.Bronchiolo-Alveolar Carcinoma-A type of adenocarcinoma that arises from the bronchiolo-alveolar regions Forms single or multiple nodule(s) which may coalesce to produce pneumonia- like consolidation
Morphology:
solid, glistening, and mucoid, reflects a diffusely infiltrating tumor
atypical cuboidal to lowcolumnar cells proliferating along the existing alveolar walls
Large cell carcinomas
The lesions may be central or peripheral.Histological features: insufficiently differentiated to permit further classification by light microscope; pleomorphic cells, frequently very large.
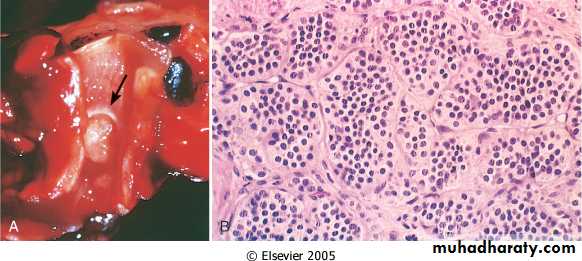
SMALL CELL CARCINOMA (oat cell carcinoma)
Usually centrally located with early involvement of the hilar and mediastinal nodes.
These tumors are derived from neuroendocrine cells of the lung, and hence they express a variety of neuroendocrine markers and secrete a host of polypeptide hormones that may result in paraneoplastic syndromes.
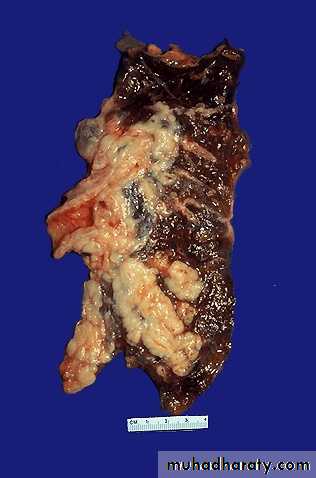
Small cell carcinoma. The cut surface of this tumor has a white appearance. The tumor seen here has caused obstruction of the main bronchus to left lung so that the distal lung is collapsed.
Histologically:
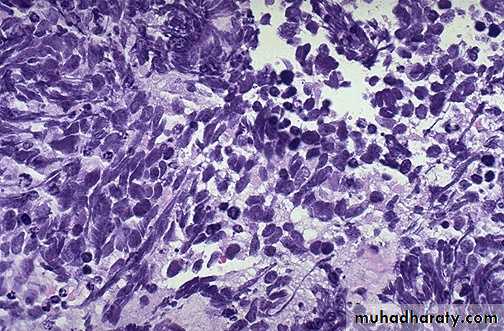
Tumor cells are round to oval, and have little cytoplasm; and finely granular chromatin.Clinical presentation of lung cancer:
Clinical presentation of lung cancer:Silent, features of metastasis.
Cough.Haemoptysis (ulceration of tumour in bronchus).
Dyspnoea.
Chest pain (involvement of pleura and chest wall).
Wheeze (narrowing of airway).
weight loss, anemia, anorexia, malaise.
Paraneoplastic syndromes (10% of cases) include:
Hypercalcemia why?
Cushing syndrome why?
Syndrome of inappropriate secretion of antidiuretic hormone (ADH).Neuromuscular syndromes, including a myasthenic-like syndrome, peripheral neuropathy, and polymyositis.
Clubbing of the fingers and hypertrophic pulmonary osteoarthropathy.
Hematologic manifestations, including migratory thrombophlebitis, nonbacterial endocarditis, and disseminated intravascular coagulation.Diagnosis:
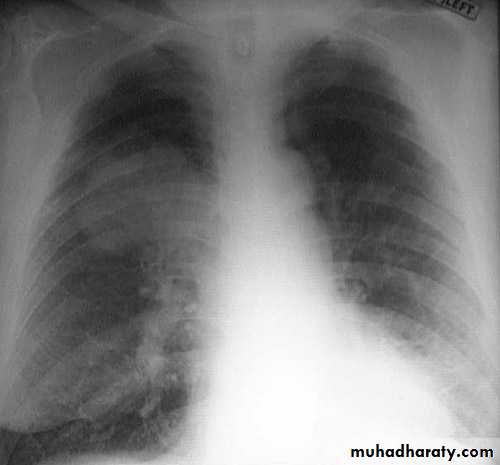
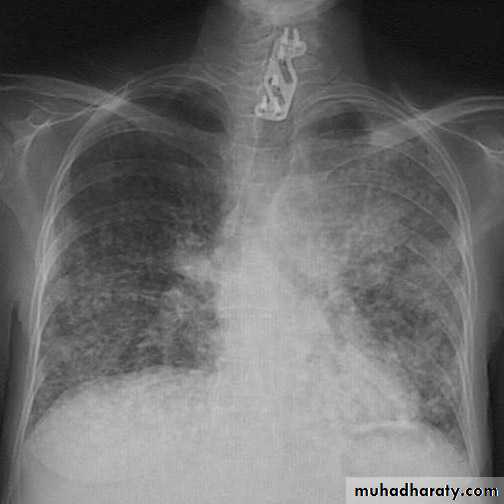
History and examinationRadiology
Cytology: sputum
- Positive in 80% of central tumors.
- Positive in 50% of peripheral tumors.
Biopsy - a number of ways:
- Bronchoscopy (very good for central tumors)
- Needle (very good for peripheral tumors)
- Mediastinoscopy
Prognosis
The prognosis of lung cancer is dismal: the 5-year survival rate for all stages of lung cancer combined is about 14%; even patients with disease localized to the lung have a 5-year survival of approximately 45%.SCC: relative good - slow growing and often resectable.
Adenocarcinoma: poor, because most tumors do not present signs of airway obstruction (because of there peripheral location) and therefore are highly advanced before presentation; bronchioloalveolar carcinoma has a good prognosis.
small cell carcinoma: poor, because tumors are fast growing and highly malignant.
Large cell carcinoma: poor; tumors usually widely disseminated at time of diagnosis.
Secondary tumors of the lung
Etiology: any malignancy may reach lung from lymph spread or vascular spread.
Clinical presentation: same as primary lesions
Macroscopic features:
There are 3 common patterns:
Miliary pattern (many small neoplasms)Cannon ball pattern (one large, spherical, well demarcated neoplasm).
Lymphangitis carcinomatosis (spread along lymphatics - white lines through lungs instead of black lines marking lymphatics.
Metastatic RCC
Bronchial carcinoid:
Account for 5% of all pulmonary neoplasms.Arise from the Kulchitsky cells (neuroendocrine cells that line the bronchial mucosa).
The neoplastic cells may rarely secrete hormones & polypeptides and may induce carcinoid syndrome.Affect adult of both sexes.
Originate in mainstem bronchi, protrude into lumen and often present with early airways obstruction.Histologically, composed of nests of uniform cells that have regular round nuclei, rare mitoses, and little pleomorphism.
Prognosis:
Slowly growing may spread to the hilar nodes but distant metastasis is rare. The reported 5- to 10-year survival rate ranges from 50% to 95%.Pleural lesions:
Lesions of the pleura may be inflammatory or neoplastic.
Malignant mesothelioma
A rare cancer of mesothelial cells, arising in the pleura, & much less commonly in the peritoneum and pericardium.It is related to occupational exposure to asbestos in the air.
The latent period for developing malignant mesotheliomas is long, often 25 to 40 years after initial asbestos exposure.The combination of cigarette smoking and asbestos exposure greatly increases the risk of bronchogenic carcinoma.
Asbestos is not removed or metabolized from the lung, and hence the fibers remain in the body for life. Asbestos fibers gather near the mesothelial cell layer, where they generate reactive oxygen species that cause DNA damage and potentially oncogenic mutations.