Oral Cavity &Gastrointestinal Tract
Oral cavityOral mucosa
Salivary glands
Jaws
Oral Inflammatory Lesions
Aphthous Ulcers (Canker Sores)Superficial mucosal ulcerations
40% of the population.
Extremely painful, & recurrent.
Cause ?
Familial cases, with IBD, celiac, Behçet disease.
Solitary or multiple
Mostly resolve spontaneously in 7 to 10 days.
Herpes Simplex Virus Infectionsherpes stomatitis
HSV type 1 (HSV-1) oralHSV-2 (genital)
Self-limited infection but leave latent virus in nerve ganglia.
Presents with vesicles (cold sores, fever blisters) Heal, without scarring
Reactivation can occur precipitated by:
• Trauma
• Allergies
• UV
• Upper respiratory tract infections
• Pregnancy
• Menstruation
• Immunosuppression
• Exposure to extremes of temperature.
Oral Candidiasis (Thrush)
Oral candidiasis may occur when the oral microbiota is altered (e.g., after antibiotic use).
Invasive disease may occur in immunosuppressed individuals.
Leukoplakia & Erythroplakia
LeukoplakiaWHO definition : “a white patch or plaque that cannot be scraped off .”
candidiasis is not considered leukoplakia.
5% to 25% progress to squamous cell carcinoma.
Erythroplakia
Red, velvety, possibly eroded ,flat50% risk for CA
Multifactorial etiology
Tobacco (cigarettes, pipes, cigars, & chewing tobacco) is the most common risk factor for leukoplakia & erythroplakia.
Oral cancer
95% of are squamous cell CATobacco
Alcohol
HPV
Salivary gland diseases
XerostomiaAgeing.
Autoimmune disorder e.g. Sjögren syndrome.
Radiation therapy.
Drugs : anti-cholinergic, antidepressant/ antipsychotic, diuretic, antihypertensive, sedative, muscle relaxant, analgesic, & antihistaminic agents
Complication:
• Dental caries
• Candidiasis
• Difficulty in swallowing & speaking.
• Sialadenitis
• Trauma• Viral: e.g. mumps
• Bacterial infection e.g. Staphylococcus aureus & Streptococcus viridans complicationg sialolithiasis)
• Autoimmune e.g. Sjögren syndrome
Neoplasms
65% to 80% occur in parotid
10% in the sub-mandibular gland
15% to 30% of tumors in the parotid glands are malignant.
50% of minor salivary gland, & 70% to 90% of sublingual tumors are cancerous.
The likelihood that a salivary gland tumor is malignant is inversely proportional, roughly, to the size of the gland.
Pleomorphic Adenoma
60% of tumors in the parotidBenign slow-growing neoplasm
Composed of a heterogeneous mixture of epithelial & mesenchymal cells
Recurrence rates approach 25%
Carcinoma arising in a pleomorphic adenoma is referred to variously as a carcinoma.
pleomorphic adenoma or malignant mixed tumor ( 2% of tumors present for less than 5 years to almost 10% for those present for more than 15 years) & are aggressive mostly adenocarcinoma
Mucoepidermoid carcinoma
Malignant neoplasm of variable biologic aggressiveness that is composed of a mixture of squamous & mucous cells.Odontogenic Cysts & Tumors
The jaws are a common site of epithelium-lined cysts derived from odontogenic remnants.The odontogenic keratocyst is locally aggressive, with a high recurrence rate.
The periapical cyst is a reactive, inflammatory lesion associated with caries or dental trauma.
The most common odontogenic tumors are ameloblastoma & odontoma.
Esophagus
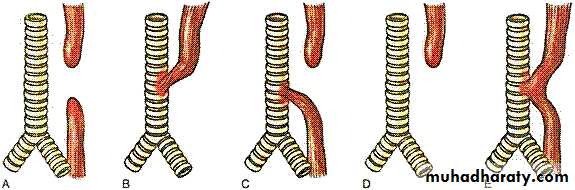
Congenital anomalies
• ECTOPIC TISSUE (gastric, sebaceous, pancreatic)• Atresia/Fistula/Stenosis/”Webs”
• Schiatzki “Ring” in lower esophagus
MOST COMMON
EsophagusEsophageal obstruction
Mechanical(developmental defects, fibrotic strictures, & tumors) or functional anomalies
Achalasia
Triad of• Incomplete LES relaxation
• Increased LES tone
• Esophageal aperistalsis
Functional esophageal obstruction.
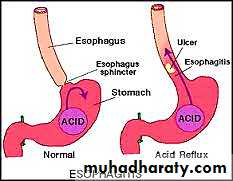
Esophagitis
chemical or infectious mucosal injury.
Infections are most frequent in immunocompromised persons.
The most common cause of esophagitis is gastroesophageal reflux disease (GERD), which must be differentiated from eosinophilic esophagitis.
Barrett esophagus
Patient with chronic GERD
Associated with increased risk of esophageal adenocarcinoma.
Esophageal squamous cell carcinoma
Alcohol
Tobacco
Poverty
Caustic esophageal injury
Achalasia
Tylosis
Plummer-Vinson syndrome.
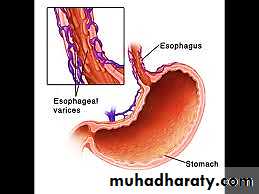
Esophageal Varices
Esophagus is one of the few sites where the splanchnic & systemic venous circulations can communicatePortal hypertension induces development of collateral channels that allow portal blood to shunt into the caval system.
However, these collateral veins enlarge the subepithelial & submucosal venous plexi within the distal esophagus.
Varices
90% in cirrhosis(alcoholic)
Hepatic schistomiasis.
Esophagitis
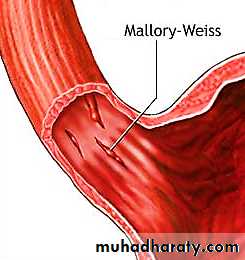
Mallory- Weiss tearsAssociated with vomiting e.g. acute alcohol intoxication.
Patient presented with Hematemesis
There is Linear superficial lacerations
Boerhaave syndrome
Transmural esophageal tears & mediastinitisChemical & Infectious Esophagitis
Pill-induced esophagitis causes odynophagiaChemotherapy
Radiation therapy
Graft-versus host disease.
Infectious
HSV,CMV or fungal (Candida, mucormycosis & aspergillosis) in immunocompromised
Inflammatory e.g. bullous diseases & Crohn disease.
Reflux Esophagitis
Pathogenesis:
↓LES tone &/or ↑abdominal pressure
Causes
Alcohol
Tobacco
Obesity
CNS depressants
Pregnancy
Hiatal hernia
Many cases, no definitive cause is identified.
Complications
• Esophageal ulceration
• Hematemesis
• Melena
• Stricture
• Barrett esophagus.
Barrett Esophagus
Barrett esophagus( Intestinal metaplasia within the esophageal squamous mucosa)It is usually a Complication of chronic GERD ( 10% of persons with symptomatic GERD).
Males 40 & 60 years of age.
There is Increases risk of esophageal adenocarcinoma.
Metaplasia……>>> dysplasia considered to be a pre-invasive lesion develops in 0.2% to 1.0%
Risk increases with duration of symptoms & increasing patient age.
Esophageal tumors
Benign e.g….Leiomyoma is the most common.Malignant
Adenocarcinoma
On Barrett esophagus & long-standing GERD.
Risk increases by tobacco, obesity, & previous radiation therapy.
Reduce is associated with diets rich in fresh fruits & vegetables.( anti-oxidants)
Esophageal adenocarcinoma occurs most frequently in White
7x more in males
Squamous Cell Carcinoma
Highlights:Old age
Males 4X more
Alcohol
Tobacco
Poverty
Achalasia
Plummer-Vinson syndrome
Radiation therapy to the mediastinum.
Black more than white people
Common in rural & underdeveloped areas.
The countries with highest incidences are Iran, central China, Hong Kong, Argentina, Brazil, & South Africa.
The overall 5-year survival rate remains a dismal 9%
STOMACH
Acute gastritis.is usually transient in nature. The inflammation may be accompanied by hemorrhage into the mucosa (acute hemorrhagic gastritis) and, sometimes by sloughing (erosions) of the superficial mucosa (acute erosive gastritis)
acute gastritis is frequently associated with
1. Heavy use of nonsteroidal anti-inflammatory drugs (NSAIDs) particularly aspirin, cancer chemotherapeutic drugs, or radiation2. Excessive consumption of alcohol, heavy smoking, and ingestion of strong acids or alkali as in suicidal attempts
3. Uremia
4. Severe stress (e.g., trauma, burns, surgery)
5. Mechanical trauma (e.g., nasogastric intubation)
6. Distal gastrectomy (reflux of duodenal contents).
• Chronic Gastritis
Is defined as "chronic inflammation of the gastric mucosa that eventuates in mucosal atrophy and intestinal metaplasia". The epithelial changes may progress to dysplasia, which constitute a soil for the development of carcinomaPathogenesis
The major etiologic associations of chronic gastritis are:1. Chronic infection by H. pylori
2. autoimmune damage
3. Excessive alcohol consumption & heavy cigarette smoking
4. Post-antrectomy (due to reflux of bile-containing duodenal secretions)
5. Outlet obstruction, uremia, and other rare causes
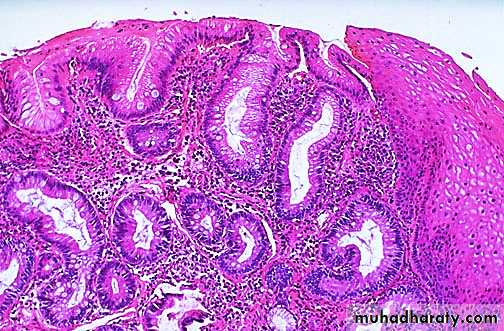
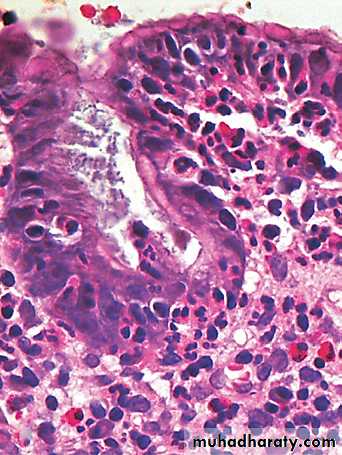
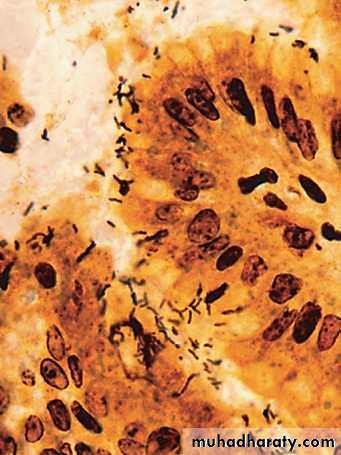
• Helicobacter pylori Gastritis
Spiral-shaped or curved bacilli
Almost all patients with duodenal ulcers & a majority of those with gastric ulcers or chronic gastritis.
Present in 70% of patients with chronic gastritis affecting the antrum.
H. pylori infection also confers increased risk of gastric cancer.
Serologic test for anti–H. pylori Ab
Fecal bacterial detectionUrea breath test
Gastric biopsy specimens also can be analyzed by the rapid urease test, bacterial culture, or polymerase chain reaction (PCR) assay for bacterial DNA.
Effective treatments include : AB & proton pump inhibitors.
Autoimmune Gastritis
Less than 10% of cases of chronic gastritis.In contrast with that caused by H. pylori autoimmune gastritis typically spares the antrum & induces hyper-gastrinemia.
Antibodies to parietal cells & intrinsic factor that can be detected in serum & gastric secretions
Reduced serum pepsinogen I levels
Antral endocrine cell hyperplasia
Vitamin B12 deficiency
Defective gastric acid secretion (achlorhydria)
Microscopic features
The mucosa is infiltrated by lymphocytes & plasma cells.
Frequently the lymphocytes are disposed into aggregates i.e. follicles, some with germinal centers.
Neutrophils may or may not be present.
Additional features.
Intestinal metaplasia: the mucosa may become partially replaced by metaplastic columnar cells and goblet cells of intestinal morphology.Atrophy as evidenced by marked loss of the mucosal glands. Parietal cells, in particular, may be absent in the autoimmune form.
Dysplasia: with long-standing chronic gastritis, the epithelium develops dysplastic changes
Peptic Ulcer Disease
H. pylori infection or NSAIDGastric hyperacidity is fundamental to the pathogenesis:
H. pylori infection play a major role.
Parietal cell hyperplasia
Excessive secretory responses
Impaired inhibition of stimulatory mechanisms such as gastrin release e.g. Zollinger-Ellison syndrome:---
Multiple :stomach, duodenum, & even jejunum
Caused by uncontrolled release of gastrin by a tumor & the resulting massive acid production.
Predisposing factors in PU :
• Chronic NSAID• Smoking
• High-dose corticosteroids
• Alcoholic cirrhosis
• COPD
• CRF
• Hyperparathyroidism.
6 & 7 associated with hypercalcemia stimulates gastrin production….>>> PU
• 8. Psychologic stress
Proximal duodenum > stomach.
Few centimeters of the pyloric valve
Anterior duodenal wall.
Gastric PU
At the interface of the body & antrum.
PU > 80% are solitary
Oval or round sharply punched-out
Gross features
The vast majority of peptic ulcers are located in the first portion of the duodenum or in the stomach, in a ratio of about 4:1. Gastric and duodenal ulcers may coexist in up to 20% of the cases.Gastric ulcers are predominantly located along the lesser curvature.
Although over 50% of peptic ulcers have a diameter less than 2 cm but about 10% are greater than 4 cm. Ulcerated carcinomas (which tend to be large) may be less than 4 cm in diameter and may be located anywhere in the stomach. Thus, size and location do not differentiate a benign from a malignant ulcer.
The classic peptic ulcer is a round to oval with sharply demarcated crater. The margins are usually level with the surrounding mucosa or only slightly elevated. Heaping-up of these margins is rare in the benign ulcer but is characteristic of the malignant ones.
Peptic ulcers penetrate the wall to a variable extent. When the entire wall is penetrated, the base of the ulcer may be formed by adherent pancreas, omental fat, or liver.
The base of a peptic ulcer is smooth and clean, owing to peptic digestion of any exudate that may form. Sometimes, thrombosed or patent blood vessels (the source of life threatening hemorrhage) are evident at the base of the ulcer.
Ulcer-related scarring may involve the entire thickness of the gastric wall; puckering of the surrounding mucosa creates mucosal folds that radiate from the crater in spoke-like fashion. This is different from malignant ulcers where there is flattening of the mucosal folds (because of malignant infiltration) in the immediately surrounding of the ulcer.
Microscopic features
In active ulcers four zones are recognized1. The base and walls have a superficial thin layer of necrotic fibrinoid necrosis.
2. Beneath this layer is a zone of predominantly neutrophilic inflammatory infiltrate.
3. Deeper still, there is granulation tissue infiltrated with inflammatory cells. This rests on
4. Fibrous or collagenous scar.
The complications of peptic ulcer
1. Bleeding is the most frequent complication (20%). It may be life-threatening; fatal in 25% of the affected patients. It may be the first warning of an ulcer.
2. Perforation is much less frequent (5% of patients) but much more serious being fatal in 60% of patients.
3. Obstruction (from edema or scarring) occurs in 2%, most often due to pyloric channel ulcers but may occur with duodenal ulcers. Total obstruction with intractable vomiting is rare.
4. Malignant transformation does not occur with duodenal ulcers and is extremely rare with gastric ulcers. When it occurs, it is always starts as malignant.
possible mechanisms by which this tiny organism impairs mucosal defenses include
H. pylori induces intense inflammatory and immune responses. As a result there is increased production of pro-inflammatory cytokines, most notably, IL-8, by the mucosal epithelial cells. This recruits and activates neutrophils with their damaging properties.Several bacterial products cause epithelial cell injury; this is mostly caused by a vacuolating toxin called VacA. H. pylori also secrete urease, proteases and phospholipases, which also cause direct epithelial damage.
H. pylori enhance gastric acid secretion and impair duodenal bicarbonate production, thus reducing luminal pH in the duodenum with its damaging effects on the duodenal mucosa.
Thrombotic occlusion of surface capillaries is provoked by a bacterial platelet-activating factor. Thus, an additional ischemic element may contribute to the mucosal damage
Other factors may act alone or in concert with H. pylori to encourage peptic ulceration:
1. Gastric hyperacidity: this when present, may be strongly ulcerogenic. The classic example is Zollinger-Ellison syndrome, in which there are multiple peptic ulcerations in the stomach, duodenum, and even jejunum. This is due to excess gastrin secretion by a gastrinoma and, hence, excess gastric acid production.2. Chronic use of NSAIDs: this suppresses mucosal prostaglandin synthesis; aspirin also is a direct irritant.
3. Cigarette smoking: this impairs mucosal blood flow and healing of the ulcer.
4. Corticosteroids: these in high doses and with repeated use encourage ulcer formation.5. Rapid gastric emptying: this is present in some patients with duodenal ulcers.
6. Patients with the following diseases are more prone to develop duodenal ulcer exposes
a. alcoholic cirrhosis
b. chronic obstructive pulmonary disease
c. chronic renal failure
d. hyperparathyroidism
We have also:
Stress ulcers: in critically ill patients with shock, sepsis, or severe trauma
Curling ulcers: proximal duodenum ,associated with severe burns or trauma
Cushing ulcers, arising in the stomach, duodenum, or esophagus of persons with intracranial disease, have a high incidence of perforation