Renal pathology/2
Dr.Shatha Th. Ahmedassistant professor/Ninevah college
PhD pathology/UK
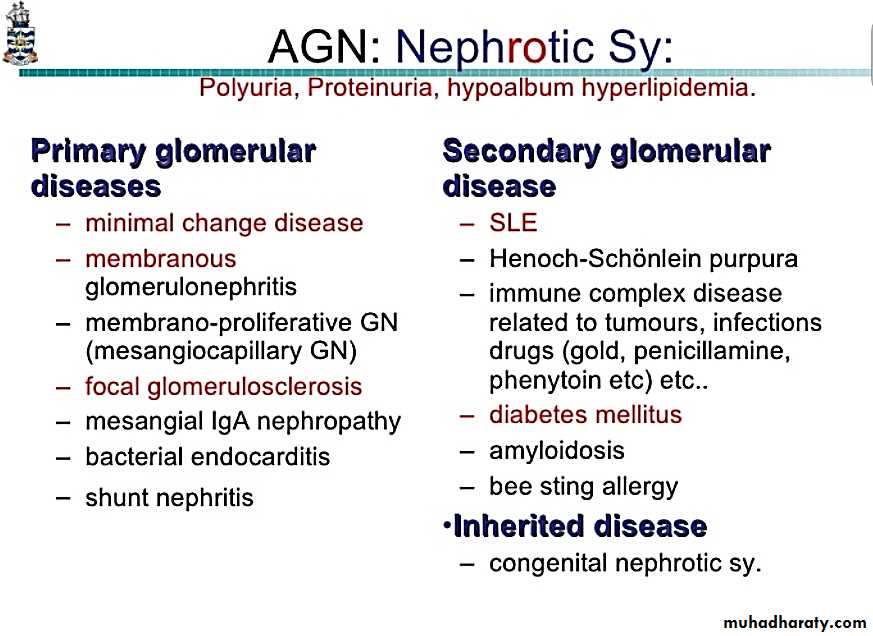
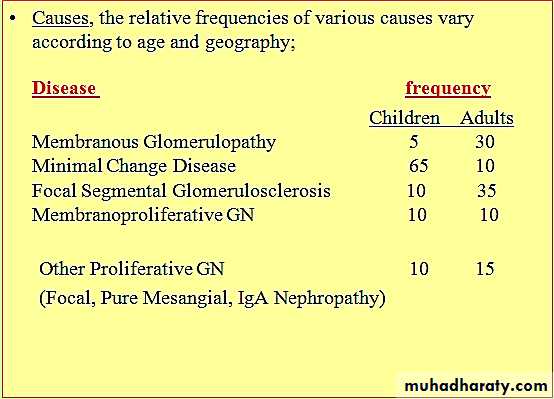
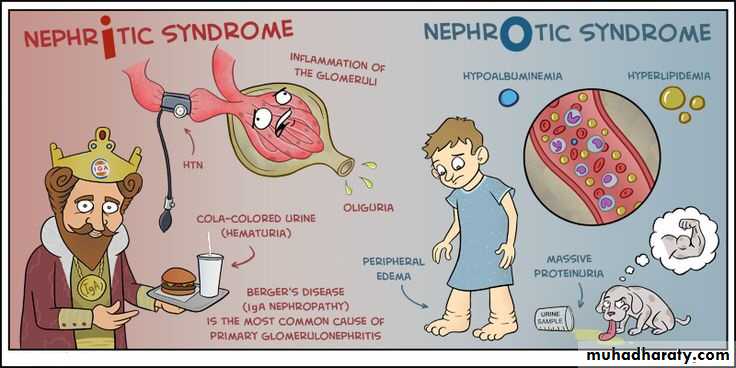
Nephrotic Syndrome
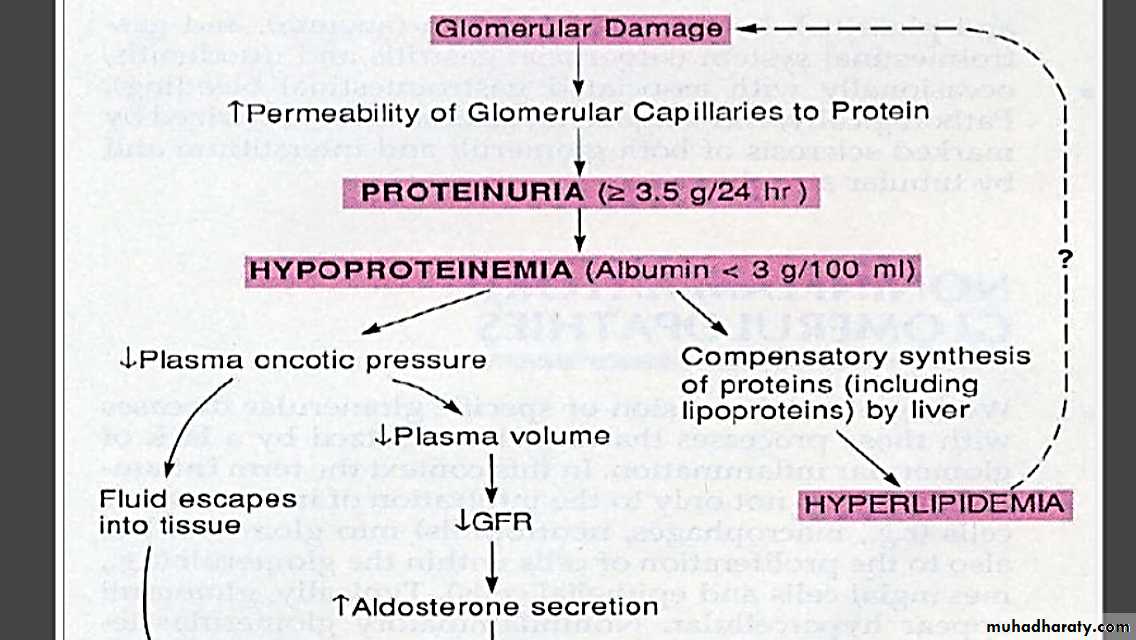
Certain glomerular diseases virtually always produce the nephrotic syndrome.The manifestations include;
1. Massive proteinuria.2. Hypoalbuminemia.
3. Generalized oedema.
4. Hyperlipidemia and lipiduria.
Nephrotic Syndrome-cont
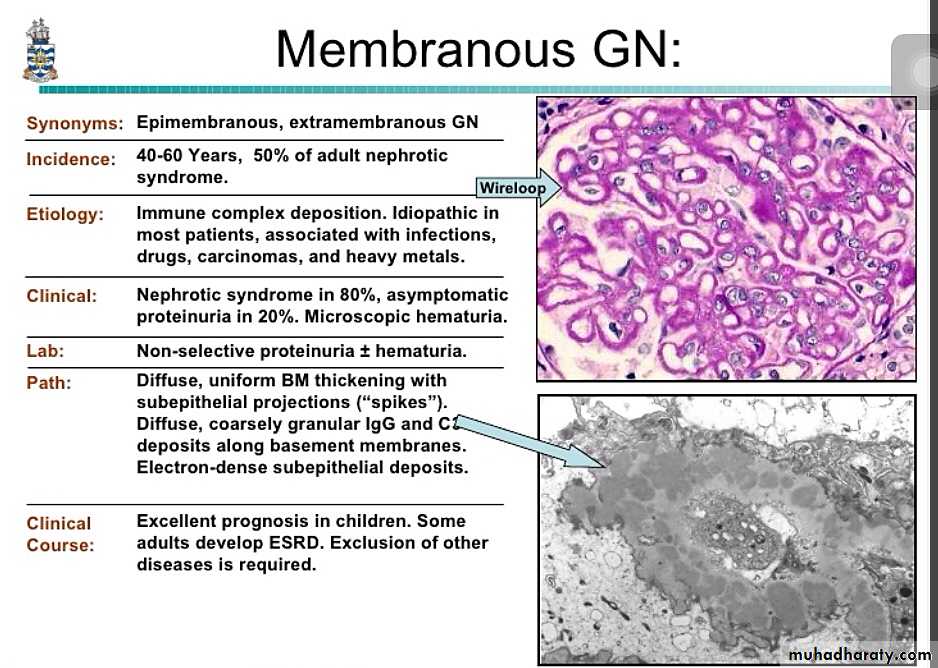
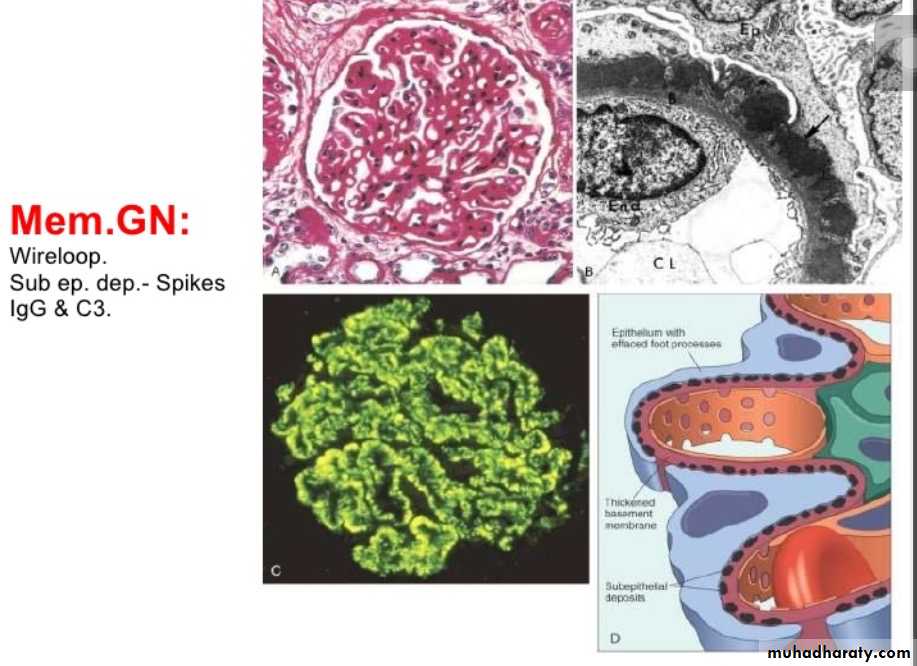
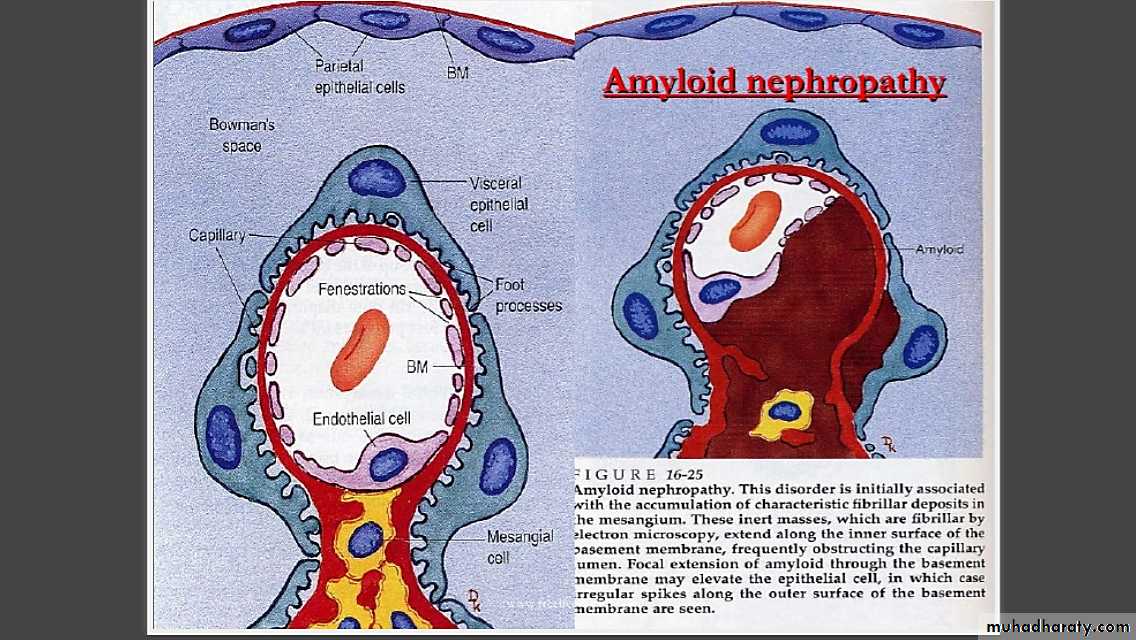
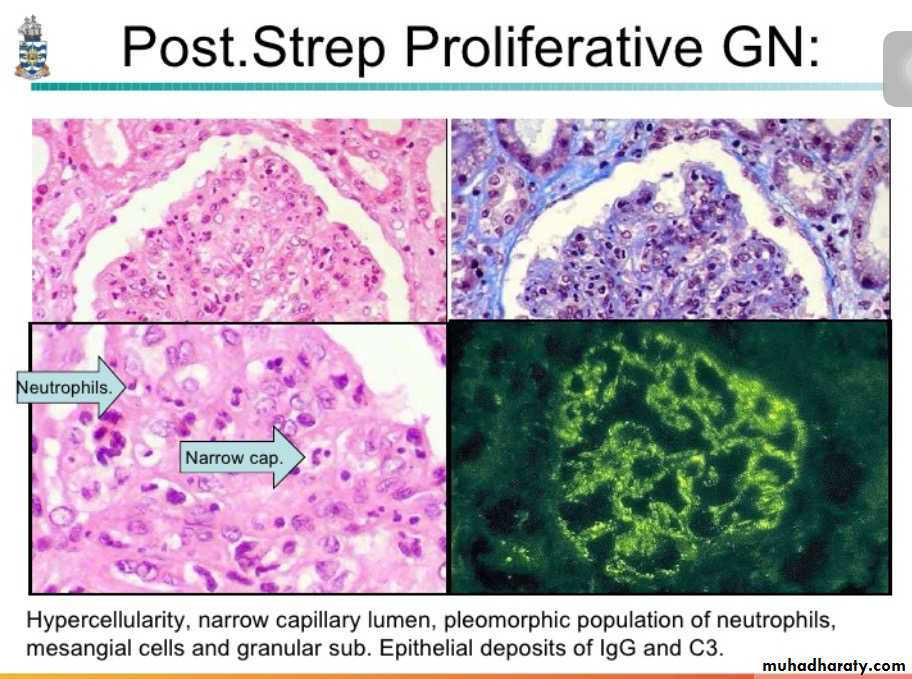
Immunofluorescence microscopy demonstrates the granular deposits to contain immunoglobulins and various amounts of complement.
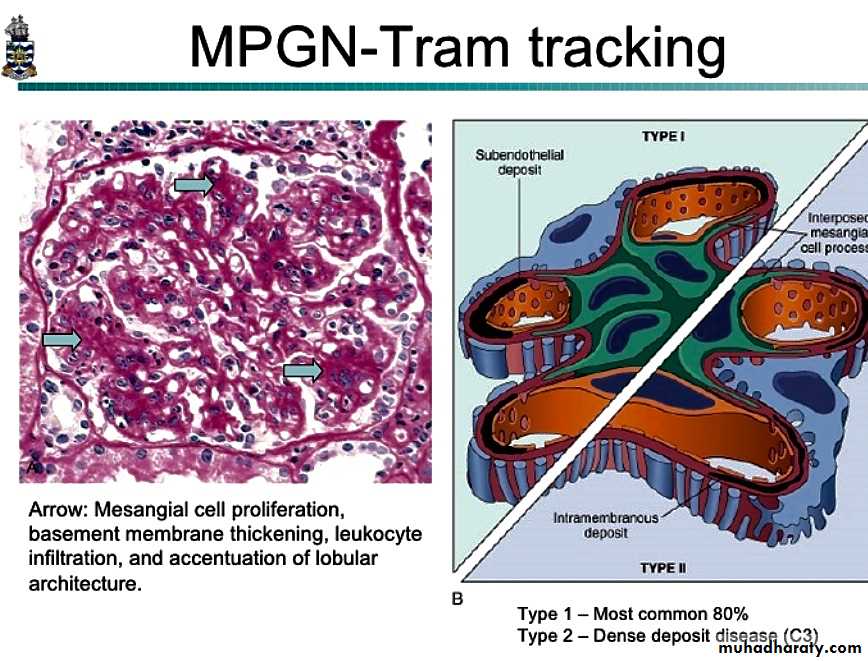
Sometimes referred as mesangioproliferative GN.
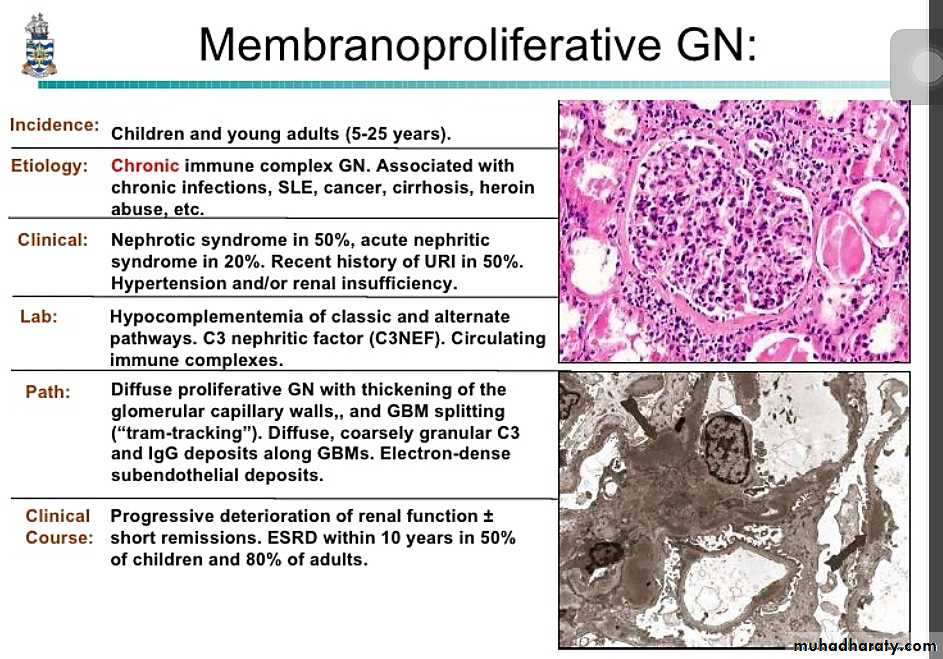
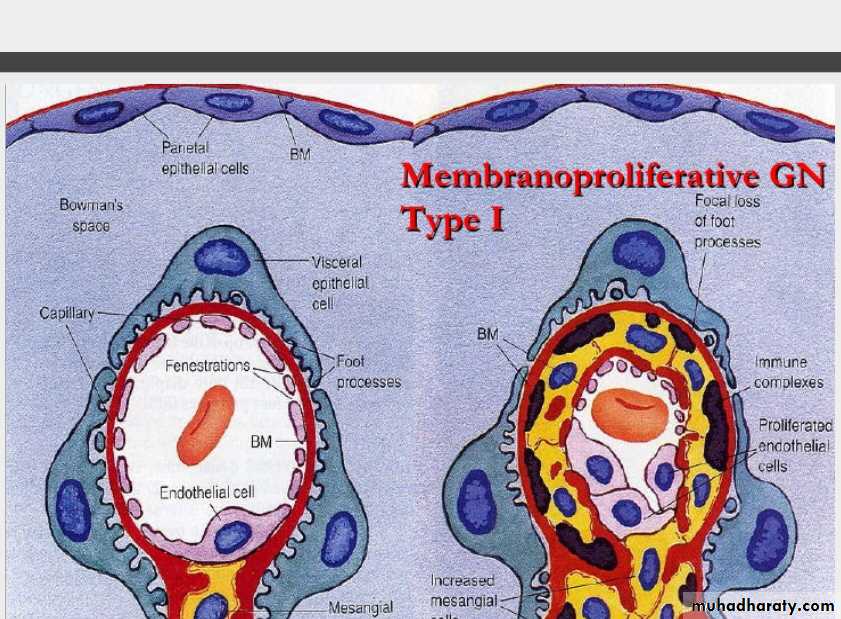
MPGN is classified into; 1. Primary (idiopathic). 2. secondary, associated with;Chronic immune complex disorders (SLE, hepatitis B and C infection, HIV infection).
Alfa1-antitrypsin deficiency.
Malignant tumors (leukemia, lymphoma).
Hereditary deficiency of complement regulatory proteins.
Membranoproliferative Glomerulonephropathy:
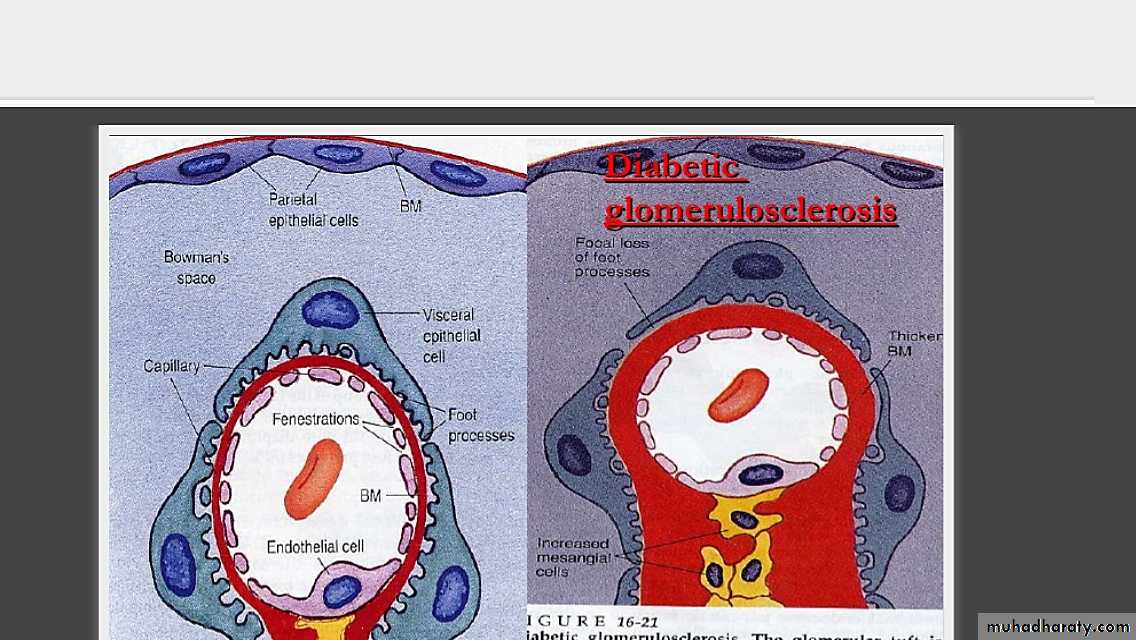
Diabetic nephropathy
It accounts for 40% of end -stage renal disease in the united states.patient present with persistant proteinurea and hypertension with high GFR at early stages followed by decline in GFR and renal function.
M/S diffuse glomerulosclerosis which is a diffuse thickening of the GBM.
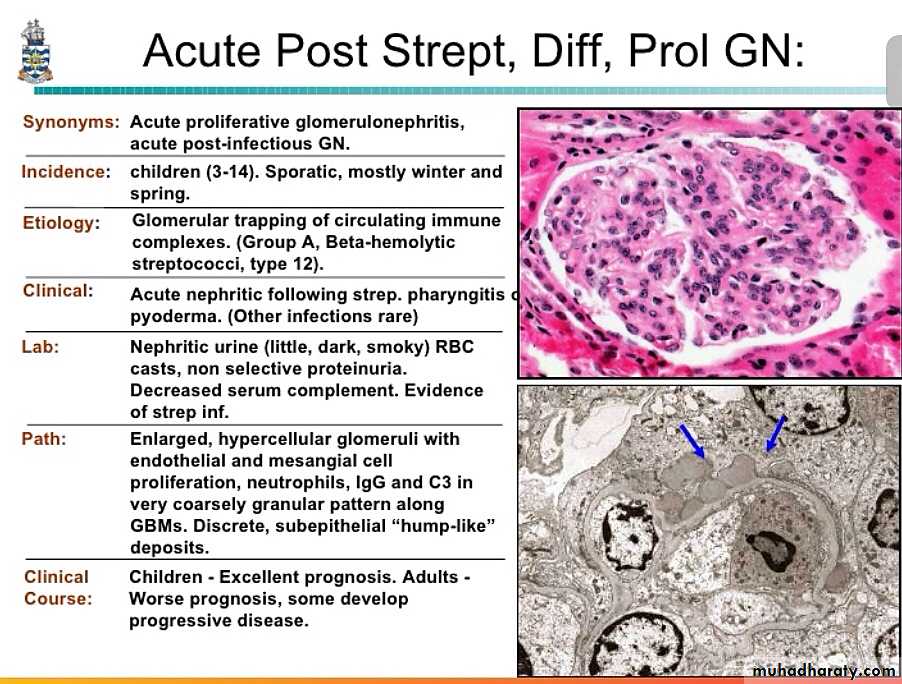
The Nephritic Syndrom
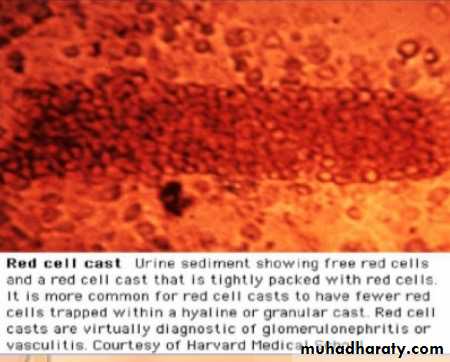
This is a clinical complex, characterized by acute renal failure,hematurea, oligurea with azotemia, , hypertension , with
oedema &proteinurea but much less severe than in nephrotic syndrome.
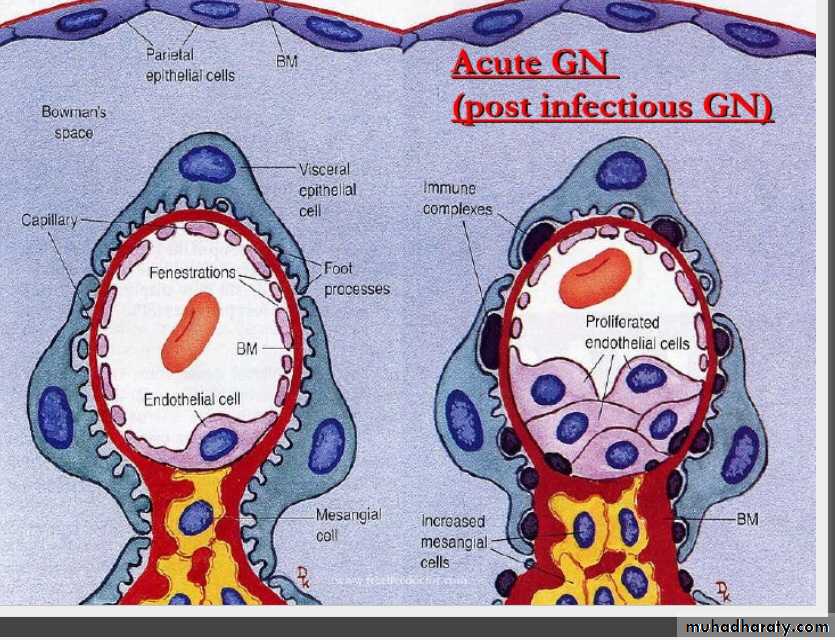
The lesions that cause nephritic syndrom is inflammatory reaction injures the capillary wall leading to escape of red blood cells,reduced GFR>oligurea, fluid retention and azotemia and hypertension.
are commonly associated with proliferation of glomerular cells+leukocyte infiltration
causes of Nephritic syndrom
• Acute nephritic syndrom may be produced by systemic disorders like SLE , or it may be the result of primary glomerular diseaaes. Most common causes are immunologically mediated chx by proliferative changes and inflammation in glomeruli .• • post infectious GN
rapidly progressive GN
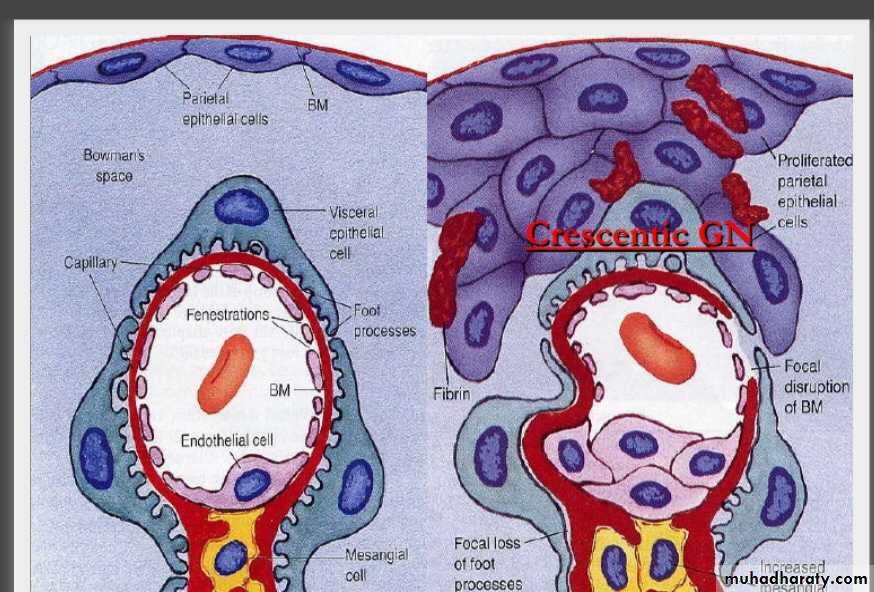
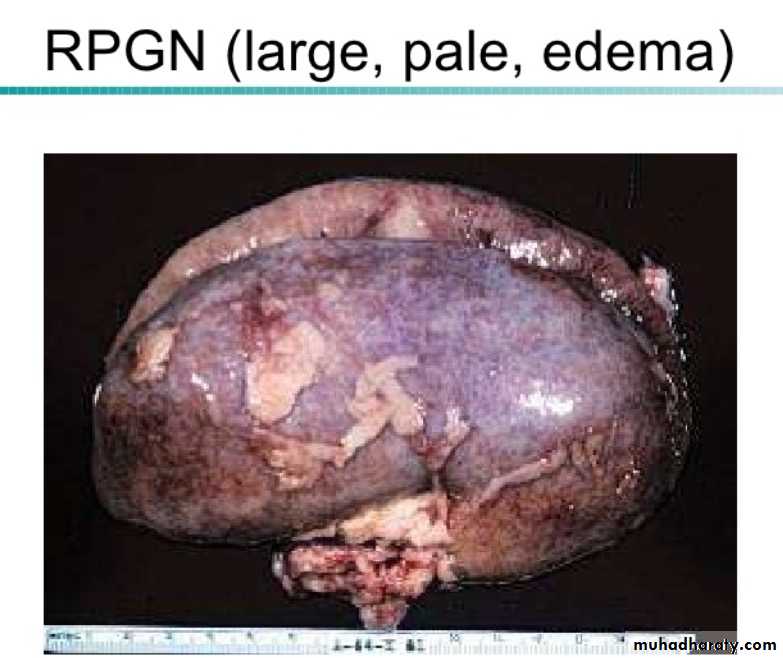
Rapidly Progressive (Crescentic) Glomerulonephropathy
It is a syndrome associated with severe glomerular injury and is characterized clinically by rapid and progressive loss of renal function, and if untreated, death from renal failure within weeks or months.Classification and pathogenesis
RPGN causes nephritic syndrome . Although It can occurs as a primary disease ,often it occurs secondary to another glomerular disease . Immunologic injury of the glomeruli is present. Accordingly 3 groups are identified1. Type I RPGN (Anti-GBM AB-Mediated)
* Idiopathic
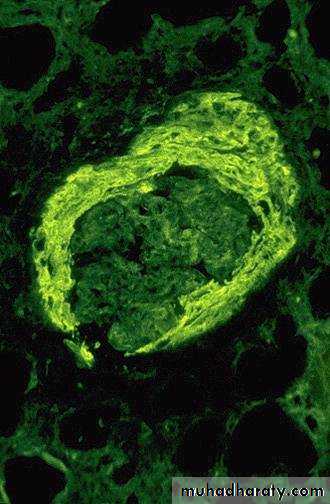
*Goodpasture Syndrome:characterized by linear IgG deposits along theGBM. In some of these individuals the anti-GBM antibodies also bind to pulmonary alveolar capillary basement membranes to produce the clinical picture of pulmonary hemorrhages associated with renal failure
2. Type II RPGN (Immunecomplex-Mediated)
immune complex mediated *Idiopathic * Postinfectious * Systemic lupus erythemotosus SLE *Henoch-Schonlein purpura (IgA) and others
3.
Classification and pathogenesis
Type III RPGN (Pauci-Immune) i.e., no immune comples• ANCA associated • Idiopathic • Wegener granulomatosis • Microscopic polyarteritis nodosa
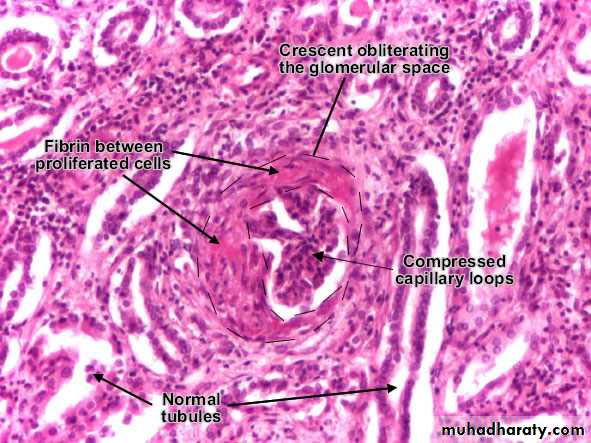
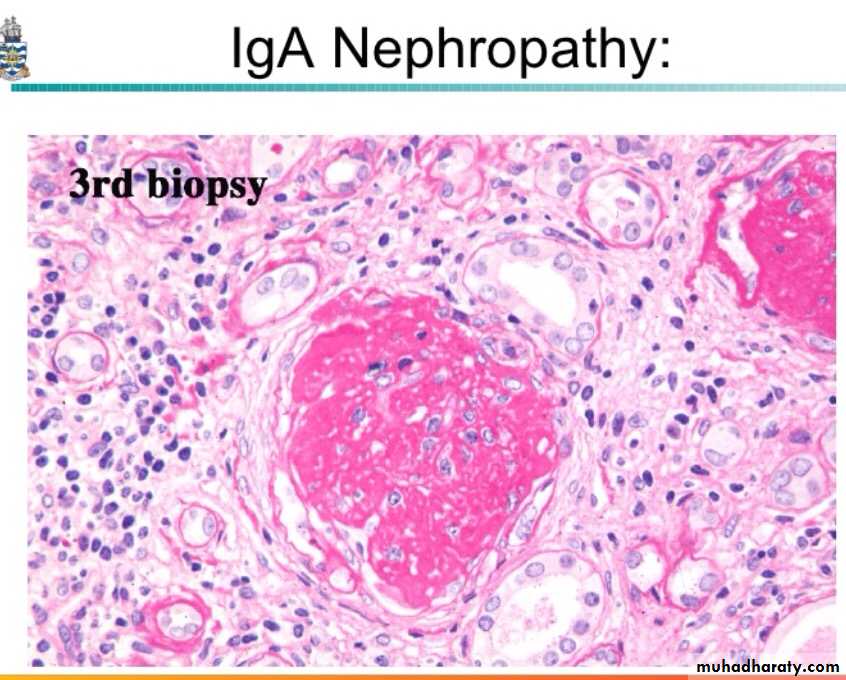
Regardless of the cause, the classic histologic picture is the presence of crescents in most of the glomeruli these are produced by proliferation of the parietal epithelial cells associated with infiltration by monocytes and macrophages
By immunofluorescence microscopy, postinfectious cases exhibit granular immune deposits; Goodpasture syndrome cases show linear deposits while pauci-immune cases have little or no deposits.
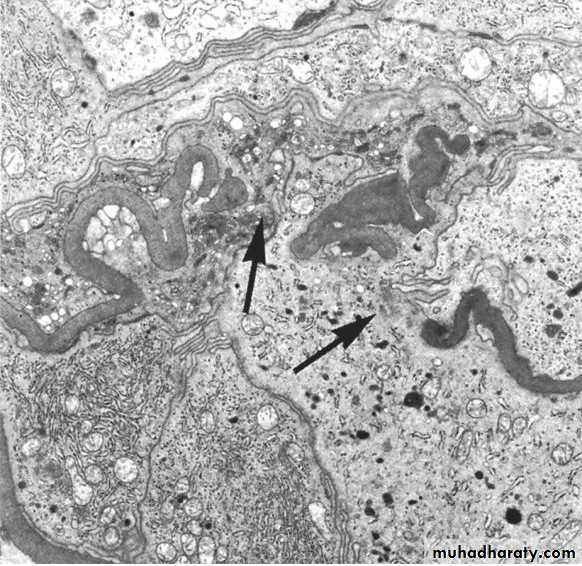
Electron microscopy shows distinct rupture in the basement membrane.
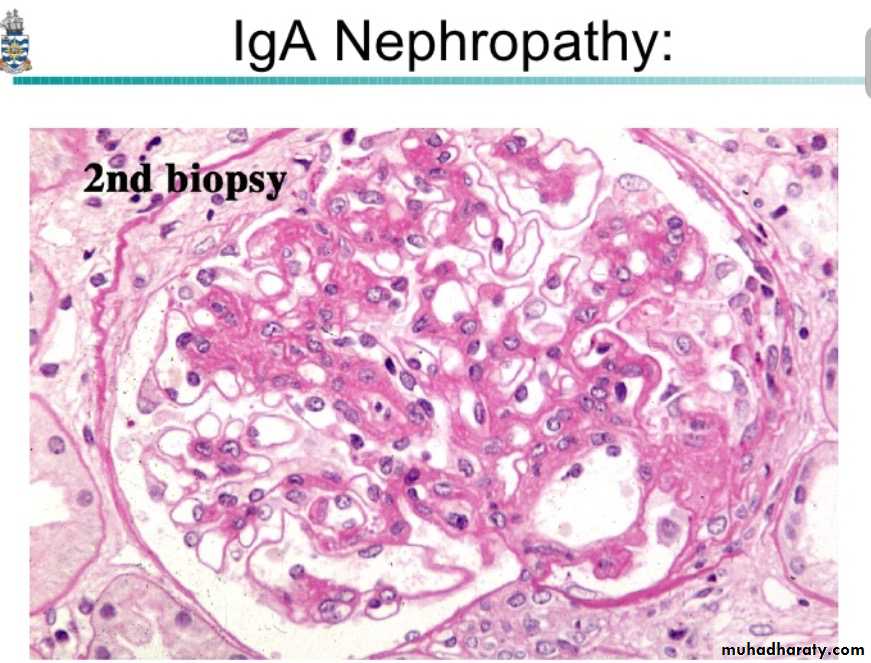
By light microscope, there is variable mesangial proliferation +/- sclerosis.
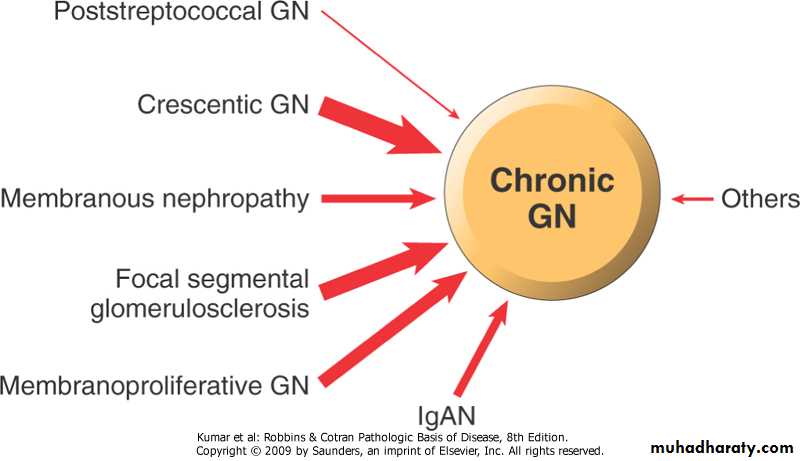
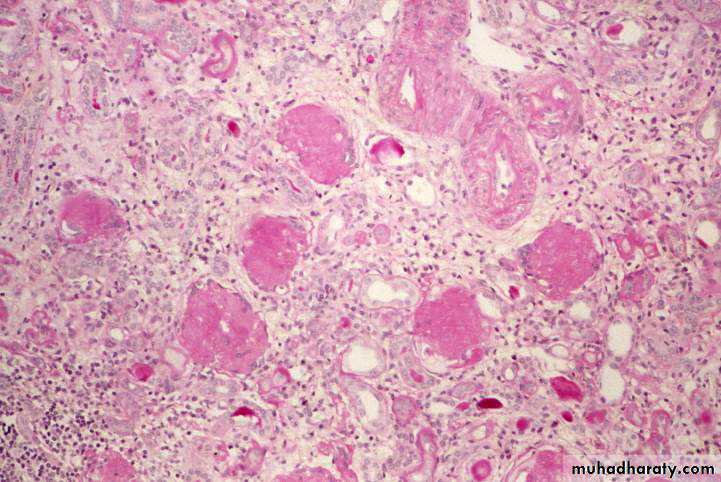
Is best considered as a pool of end-stage glomerular disease.Morphology;
The kidneys are asymmetrically contracted and have diffusely granular cortical surfaces.
The cortex is thinned,
Light microscopically, there is hyaline obliteration of many glomeruli, arterial with arteriolar sclerosis, marked atrophy of associated tubules, and interstitial inflammation and fibrosis.
Chronic Glomerulonephropathy
Clinical features include anemia, anorexia, malaise, proteinuria, hypertension and azotemia.
In most patients, chronic glomerulonephropathy develops insidiously and slowly progresses to renal insufficiency.
Grossly there is presence of small, shrunken kidneys. There is fine and symmetrical scars.
Microscopically, there is hyalinization of glomeruli, interstitial fibrosis, atrophy of tubules, and a lymphocytic infiltrate.
Management is done by dialysis and renal transplantation.
Clinical course
Grossly there is presence of small, shrunken kidneys,diffuse granular surface and thin cortex .
Chronic GN: Defined by the presence of > 2/3 sclerotic glomeruli. Microscopically, there is hyalinization of glomeruli, interstitial fibrosis, atrophy of tubules, and a lymphocytic infiltrate.