Periapical microbiology & immunology
There are many different ways for microorganisms to invade the dental pulp. either through an• dental caries,
• trauma that has removed the barrier of enamel and the dentine.
• their entry might be through the salivary contamination during dental preparation.
• another way is through the gingival sulcus or periodontal ligament
Periapical microbiology & immunology
Failure of root canal treatment or retreatment could be caused either by presence of bacteria in the root canal system, or occurrence on the apical part surface and occasionally in the periradicular tissue near to the apical foramina.Periapical microbiology & immunology
As the Periapical disease progress, resorption of the root can often be seen and extension in to the osseous support is depicted in a radiograph as loss of the bone pattern with rarefactionThe spread of infection depend on the anatomic relationships, resistance of the host, the no. and virulence of MO, resistance of MO.
The inflammation may be acute or chronic and may involve apical cementum, dentine, periodontal ligament, lamina dura and the cortical bone of the alveolar process.
Endodontic Surgery
Endodontic surgery is the management of periradicular disease by a surgical approach.• Abscess drainage/Cortical trephination
• Periapical surgery
• Hemisection or root amputation
• Intentional replantation
• Corrective surgery
Drainage of an Abscess
Drainage releases transudates or exudates from a focus of liquefaction necrosis.Goals of Draining an abscess :
relieves signs and symptoms, increases circulation, promote healing , for culture and sensitivity and decrease a potent irritant,.
The abscess may be confined to bone or may have eroded through bone and the periosteum to invade soft tissue.
Draining the infection does not eliminate the cause of the infection, so definitive treatment of the tooth is still needed.
Drainage of an Abscess
An abscess in bone resulting from an infected tooth may be drained by two methods?
A?? coronally
B??I&D
Choosing between them??
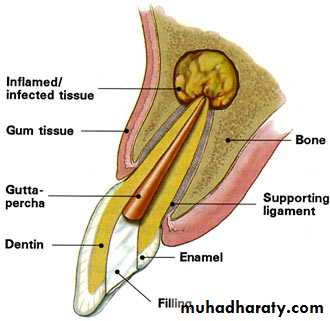
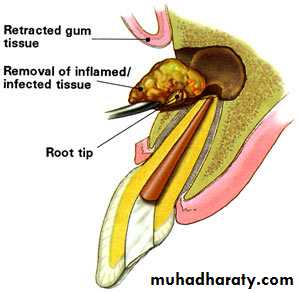
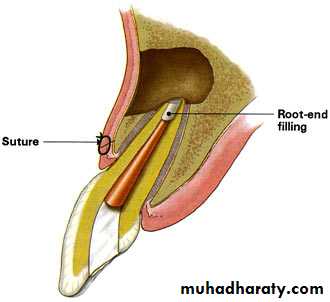
Periapical SurgeryPeriapical (i.e., periradicular) surgery includes a series of procedures performed to eliminate symptoms.
Periapical surgery includes the following:
1. Appropriate exposure of the root and the apical region
2. Exploration of the root surface for fractures or other pathologic conditions.
3. Curettage of the apical tissues
4. Resection of the root apex
5. Retrograde preparation with the ultrasonic tips
6. Placement of the retrograde filling material
7. Appropriate flap closure to permit healing and minimize gingival recession
Indications for Periapical Surgery
• Anatomic problems preventing complete debridement or obturation• Restorative considerations that compromise treatment
• Horizontal root fracture with apical necrosis
• Irretrievable material preventing canal treatment or retreatment
• Procedural errors during treatment
• Large periapical lesions that do not resolve with root canal treatment
Contraindications (or Cautions) forPeriapical Surgery
A. Patient's Medical Status1. Uncontrolled Hypertension
2. Recent Myocardial Infarction
3. Uncontrolled Diabetes
4. Dialysis Patients
5. Uncontrolled Bleeding Disorders
6. Immuno-compromised Patients
B. Patient's Mental/Psychological Health
1. Patient does not desire surgery2. Patient unable to handle stress of long complicated procedure
3. Patient extremely apprehensive
C. NONRESTORABLE TOOTH
D. POOR PERIODONTAL PROGNOSIS
E. INADEQUATE ACCESS TO SURGICAL AREA
1. Thick buccal cortical plate/external oblique ridge
2. Limited opening
3. Shallow palatal vault
4. Shallow vestibule
PRESURGICAL CONSIDERATIONS
• A- Success Of Nonsurgical Treatment And Retreatment• If the quality of the non-surgical endodontic therapy can be improved by re-treatment, this should be accomplished prior to periapical surgery as this will enhance the overall prognosis.
• Do not “seal in” necrotic debris and/or contaminated canal contents with a root-end filling.
PRESURGICAL CONSIDERATIONS
B. SYSTEMIC CONSIDERATIONS1. Review of medical history
2. Consultations
C. PSYCHOLOGICAL EVALUATION
1. Patient motivation
2. Patient apprehension
PRESURGICAL CONSIDERATIONS
D. ESTHETICS
1. Scarring
2. Exposure of crown margins
E. PROSTHETIC CONSIDERATIONS
1. Presence of crowns and bridges
2. Restorability
PRESURGICAL CONSIDERATIONS
F. Clinical evaluation1. Evaluation of radiographs - Periapical films at different angles and panoramic films to evaluate root length, location of adjacent roots, and location of major anatomical structures.
Occlusal films may also be useful, especially for palatal lesions.
PRESURGICAL CONSIDERATIONS
The mental foramen is generally located at a point that is 60% of the total distance from the buccal cusp tip of the 2nd premolar to the inferior border of the mandible. Possible involvement of the sinus must be evaluated and the patient informed about potential for sinus exposure and displacement of foreign bodies into the sinus. Maxillary 2nd premolar has the highest incidence of sinus involvement, followed by the maxillary molars.PRESURGICAL CONSIDERATIONS
2 . Limitations of opening3. Pre-existing scar tissue
4. Extent of tori/exostoses
5. Vestibular depth
6. Quality of existing restoration (s)
7. Depth of palatal vault - (is a stent necessary?)
PRESURGICAL CONSIDERATIONS
G. Periodontal evaluation
- pocket depths
- status of gingival health
- Height and width of alveolus
PRESURGICAL PREPARATION
a. Review medical historyb. Verbal and written informed consent
c. Vital signs - (bp, pulse, respirations)
d. Pre-operative therapeutics
1. chlorhexidine mouth rinses
2. pre-operative nsaid - ibuprofen 800mg one hour pre-op
3. antibiotics, if needed
4. sedation, if needed
5. steroids, if needed
PRESURGICAL PREPARATION
E. ANESTHESIA1. Regional blocks
2. Long acting anesthetic
3. Local infiltration using vasoconstrictors for increased hemostasis.
F. STERILE FIELD AND ASEPTIC TECHNIQUE
1. Surgical draping of patient.
2. Surgical scrubs for surgeon and assistant.
3. Betadine swab extraorally and intraorally.
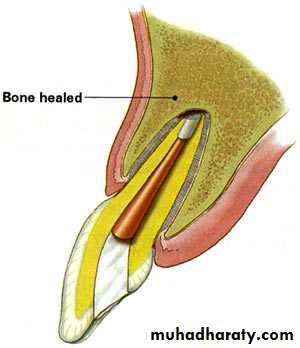
Factors Associated With Success and Failure in Periapical Surgery
Success
• Healthy periodontal status.
• No dehiscence
• Adequate crown-root ratio
• Radiolucent defect isolated to apical one-third of the tooth
• Dense orthograde fill
• Postoperative factors:
• Radiographic evidence of bone fill following surgery
• Resolution of pain and symptoms
• Absence of sinus tract
• Decrease in tooth mobility
Failure
• Clinical or radiographic evidence of lesion is still• Poor or lack of orthograde filling
• Marginal leakage of crown or post
• Poor preoperative periodontal condition
• Postoperative factors:
• Lack of bone repair following surgery
• Lack of resolution of pain
• Fistula does not resolve or returns