Pulpitis &apical periodontitis
Chapter fiveChapter six:tooth wear
A term that includes the processesof non-carious tooth damage or ‘tooth surface loss’. The processes of attrition, abrasion and erosion cause tooth wear. In any one affected patient, more than one of these processes is often active.
Tooth wear
Attrition is wear from tooth-to-tooth contact and affects the tips of cusps and incisal edges most severely.
It is a normal physiological process, and wear increases with age.
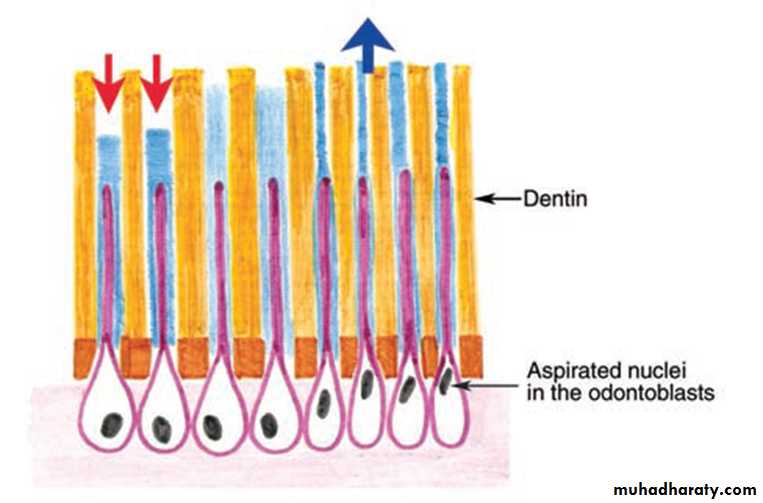
Reactionary dentine forms in response to this slow process and protects the pulp. Dentinal tubular sclerosis prevents dentine hypersensitivity resulting from pure attrition.
Attrition. Excessive wear of the occlusal surfaces of the
teeth, as a result of an abrasive diet. The site of the pulp of several teeth is marked by reactionary dentine which is porous and stained. Teeth remain vital.
Abrasion is wear of the teeth by an abrasive external agent.The most common form is occlusal wear from an abrasive diet and is frequent in developing countries and in ancient skulls.Abrasion of the necks of the teeth buccally is seen mainly in the elderly as a consequence of overly vigorous tooth brushing or use of an abrasive dentifrice.
Attrition and abrasion. Chronic physical trauma to the teeth produced by chewing and over-vigorous use of a toothbrush.
The incisal edges of the teeth have worn into polished facets, in the centres of which the yellowish dentine is visible. The necks of the two nearest teeth have been deeply incised by tooth brushing, also exposing dentine. The pulp has been obliterated by secondary dentine formation, but its original site can be seen in the centre of the exposed dentine.
Mixed pattern tooth loss. In this case, elements of erosion and abrasion are present.
Note the shiny polished surface
produced by abrasion.
Localised abrasion caused by opening hair grips.
Erosion is progressive solubilisation of tooth substance by exposure to acid. Enamel is completely dissolved and dentine demineralised, softened and rendered prone to abrasion and attrition.
Erosion. Saucer-shaped defects on the labial enamel resulting from acid drinks being trapped between the upper lip and teeth.
Features and effects of bruxism
Noise during grinding (nocturnal bruxism).Attrition, wear facets and occasionally sensitivity.
Fracture of cusps and restorations.
Increased (adaptive) mobility of teeth.
Hypertrophy of masseter and anterior temporalis muscles.
Sometimes, although rarely, myalgia and limitation of jaw movement.
Sometimes, although rarely, tenderness on palpation of masticatory muscles.
Bruxism is the term given to periodic repetitive clenching or rhythmic forceful grinding of the teeth.
Pulpitis &apical periodontitis
Chapter five
Pulpitis, inflammation of the dental pulp.
dental pulpitis: is an orofacial,acquired, inflammatory pain
condition.
Causes of pulpitis
Dental caries.Traumatic exposure of the pulp.
Fracture of a crown or cusp.
Cracked tooth.
Thermal or chemical irritation.
Are there other causes???
Traumatic exposure
The pulp has been exposed duringcavity preparation, and dentine chippings and larger fragments have been driven into the pulp. The tooth was extracted before a strong inflammatory reaction has had time to develop, but it is clear that some inflammatory cells have already localised around the debris, which will have introduced many bacteria to the pulp.
Cracked tooth:how to diagnose it???????
The pulp died beneath this crack, which was undetected clinically.
Decalcification of the tooth and
shrinkage on preparation of a section has revealed the crack.Features of ‘reversible’ and ‘irreversible’ pulpitis
Reversible pulpitisPain in short sharp stabs, after stimulus removed in seconds or a few minutes.
Stimulated by hot and cold or osmotic (sweet) stimuli
Pain resolves after stimulus removed in a few seconds or minutes.
Irreversible pulpitis
Constant throbbing pain with sharp exacerbations. Spontaneous exacerbations, as well as hot and cold or osmotic (sweet) stimuli. In late stages cold may relieve the pain.
Pain persists several minutes or
hours after an exacerbating stimulus.
Pulpal hyperaemia:reversible?Pulpitis:could be ______ or _____.
Pulpal hyperaemia. While bacteria are still some distance from the pulp, acid permeating along the dentinal tubules gives rise to dilation of the blood vessels, oedema and a light cellular inflammatory infiltrate in the pulp.Acute pulpitis: could be ______ or ______.
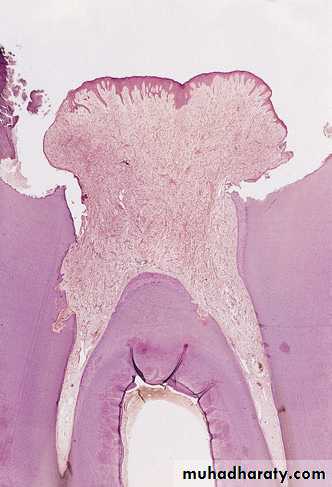
Acute pulpitis. Low-power view showing occlusal caries penetrating to the pulp through a layer of reactionary dentine.There is a focus of acute inflammatory cells beneath the carious exposure in the pulp horn.
Acute pulpitis:
Acute pulpitis. Beneath the carious exposure (top right).a dense inflammatory infiltrate is accumulating. More deeply, the pulp is hyperaemic, with dilated blood vessels.
Acute pulpitis:
Acute pulpitis: Infection seen as, (dark lines of bacteria along tubules) & has penetrated a thin layer of reactionary dentine on the roof of the pulp chamber causing inflammation throughout the pulp and pus to form in the pulp horn.Acute pulpitis:
Acute caries and pulpitis. Infection has penetrated to the pulp. Part of the pulp has been destroyed, and an abscess has formed, containing a bead of pus.Acute pulpitis:
Acute pulpitis: terminal stage. The entire pulp has beendestroyed and replaced by inflammatory cells and dilated vessels.
Calcific barriers: Pulpitis with formation of a barrier of thick reactionary dentine in the pulp horn, but with an abscess immediately below it. The rest of the pulp is inflamed. Higher-power view of a calcific barrier induced by calcium hydroxide directpulp capping. In this case the barrier is thin, inflammation in the underlying pulp has not subsided and the pulp cap has failed.
Pulp capping:can be _____ or _______.
This pulp capping has induced a thick layer of reactionary dentine (with regular tubules, best seen on the left hand side of the pulp chamber wall coronally) and reparative dentine with a more irregular structure (on the right ofthe pulp wall). Unfortunately these reactions do not produce a complete barrier, and failure of the procedure is indicated by the inflammatory cells concentrated below a gap in the barrier.
Chronic hyprtplastic pulpitis: Pulp polyp:what are its characteristic features???
Open pulpitis: Beneath the wide exposure the pulp has survived in the form of granulation tissue, with the most dense inflammatory infiltrate immediately beneath the open surface.Why did it form?
Pulp polyp. An inflamed nodule of granulation tissue can be seen growing from the pulp chamber of this broken down first permanent molar.How to treat it?Pulp polyp & ______polyp.How to differentiate between both?
Pulp polyp. A hyperplastic nodule of granulation tissue is growing out through a wide exposure of the pulp. The surface is ulcerated, and the loose pulp has been replaced by the proliferation of fibrous tissue and vessels with inflammatory cells.Where did the epithelial covering come from??
Pulp polyp. In this broken-down molar, granulation tissue is proliferating from the pulp cavity and has acquired an epithelial covering over much of its surface, probably by shed epithelial cells from the mucosa seeding onto the surface. Note also the internal resorption (left) as a result of pulpal inflammation.Treatment options for pulpitis:
If fractured or cracked,stabilize and seal pulp temporarily.• RemovaI fracture al of caries, obtundent or steroid dressing • Removal of caries and pulp capping
• Pulpotomy in deciduous teeth.
• Endodontic treatment.
• Extraction.
• Analgesics are largely ineffective.
Why are analgesics ineffective?
Why does acute pulpitis takes place at night?
PERIAPICAL PERIODONTITIS, ABSCESS AND GRANULOMA
Causes of apical periodontitis:
• Infection
• Trauma
• Chemical irritation
What are the differences between it & pulpitis?
Acute apical periodontitis:
In this early acute lesion, inflammatory cells, mainly neutrophils & polymorphonuclear leucocytes, are seen clustered around the apex of a non-vitaltooth. The inflammatory cells are spreading around and into bone, and there has only been time for a small amount of bone resorption to develop.
This would be seen radiographically only as slight fuzziness of the apical lamina dura.
Possible complications of acute apical periodontitis:
• Suppuration• Regional lymphadenopathy
• Spreading infection
Differences between cellulitis & Ludwig’s angina?What is cavernous sinus thrombosis?
Oedema due to acute apical periodontitis. An acuteperiapical infection of a canine has perforated the buccal plate of
bone causing oedema of the face; this quickly subsided when the
infection was treated
pulp stones (A) The dystrophic or diffuse pulp mineralisations often found as an age change. (B) Rounded nodules of calcified tissue, in this case resembling bone rather than dentine.