جامعة الموصل
كلية طب الاسنان/ فرع صناعة الاسنان Lec.: Mohammed A. Abdulla
المرحلة الرابعة/ صناعة اسنان
Pre-prosthetic surgical consideration
Surgical goals for the treatment of patients should address the following factors, Providing the patient with the best possible tissue contours for prosthesis support, function, and comfort, maintaining as much bone and soft tissue as possible.Theses goals can be reached through the achievement of specific objectives which includes:
1-Creating a broad ridge form.
2- Providing an adequate vestibular depth for prosthetic flange extension.
3- Establishing adequate amount of fixed tissue over the denture bearing areas.
4- Establishing proper inter-arch relationships and spacing.
5- Supporting arch integrity.
6- Providing adequate palatal vault form.
7- Provide proper ridge dimensions for implant placement.
- Patient Evaluation and Examination
Prior to the performance of any procedure. The physical examination includes through evaluation of the oral hard and soft tissues and radiographs. Radio graphically, the panoramic radiograph is the proper image for pre-prosthetic surgery , which help in visualize many of the important anatomic and structural relation ships necessary to accurately create a treatment plan for pre-prosthetic procedures.
For pre-prosthetic procedures and treatment plans which include implant placement, more radiographic studies may be required. Tomographic studies and computerized tomography (CT scans) may be used. The CT scan can provide cross-sectional detail of the maxilla in both the axial and coronal views, excellent information about alveolar height and width, facial, lingual, and palatal alveolar contours, relation ships between the maxillary crests and the sinus floor and nasal floor, and the mandibular inferior alveolar canal and mental foramina to the crestal bone.
- Treatment Planning
Goals for treatment should include the following factors:
1-Providing the patient with the best possible tissue contours for prosthetic support, function, and comfort.
2- Maintaining as much bone and soft tissue as possible.
Types of pre-prosthetic surgery can be classified in a number of different ways. One method is to categorize the surgery as resective, re-contouring or augmentation of bony or soft tissue. While many of these procedures are directed towards treatment of the patient who is completely edentulous, there are many indications for pre-prosthetic surgery for the patients who are either partially edentulous or completely dentate.
-Commonly used pre-prosthetic procedures
A- Ridge alveoloplasty with extraction:
After extraction of a tooth or teeth, the clinician must make a determination about the remaining ridge contour(s) in order to make the re-contouring at the time of the extraction or later time.
Procedure:
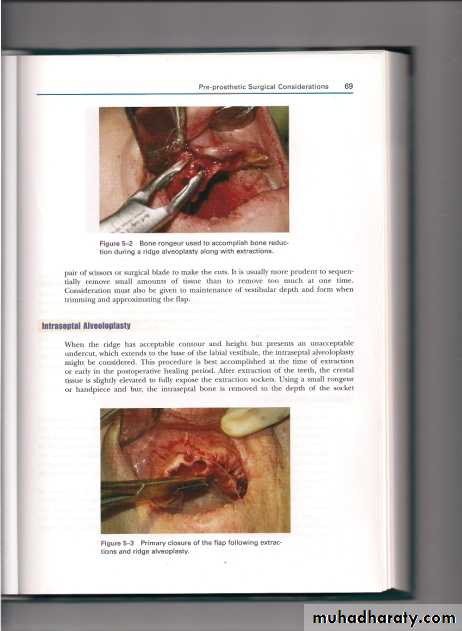
A full thickness flap should be elevated to appoint apical to the area in need of re-contouring . Depending on the amount of re-contouring needed, a bone file may be sufficient to produce the desired contours. For greater re-contouring, aside cutting rongeur or hand piece and bur can be used (Figure 1) with irrigation and cooling system to avoid over heating, bone necrosis, then cleaning the area of operation from debris. Figure(1)
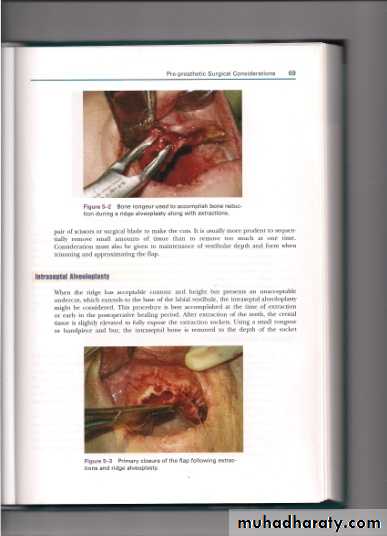
After re-contouring, a bone file is uses to "fine tune" the re-contouring. The flap then repositioned , contours palpated to verify that a desired contour reached (Figure 2), Consideration must also be given to maintain of vestibular depth and form when trimming and approximating the flap.
Figure (2)
B- Intraseptal aleveoloplasty:
When the ridge has acceptable contour and height but present an unacceptable under cut, which extend to the base of the labial vestibule, the Intraseptal aleveoloplasty might be considered. This procedure can de accomplished at the time of extraction.
-Procedure:
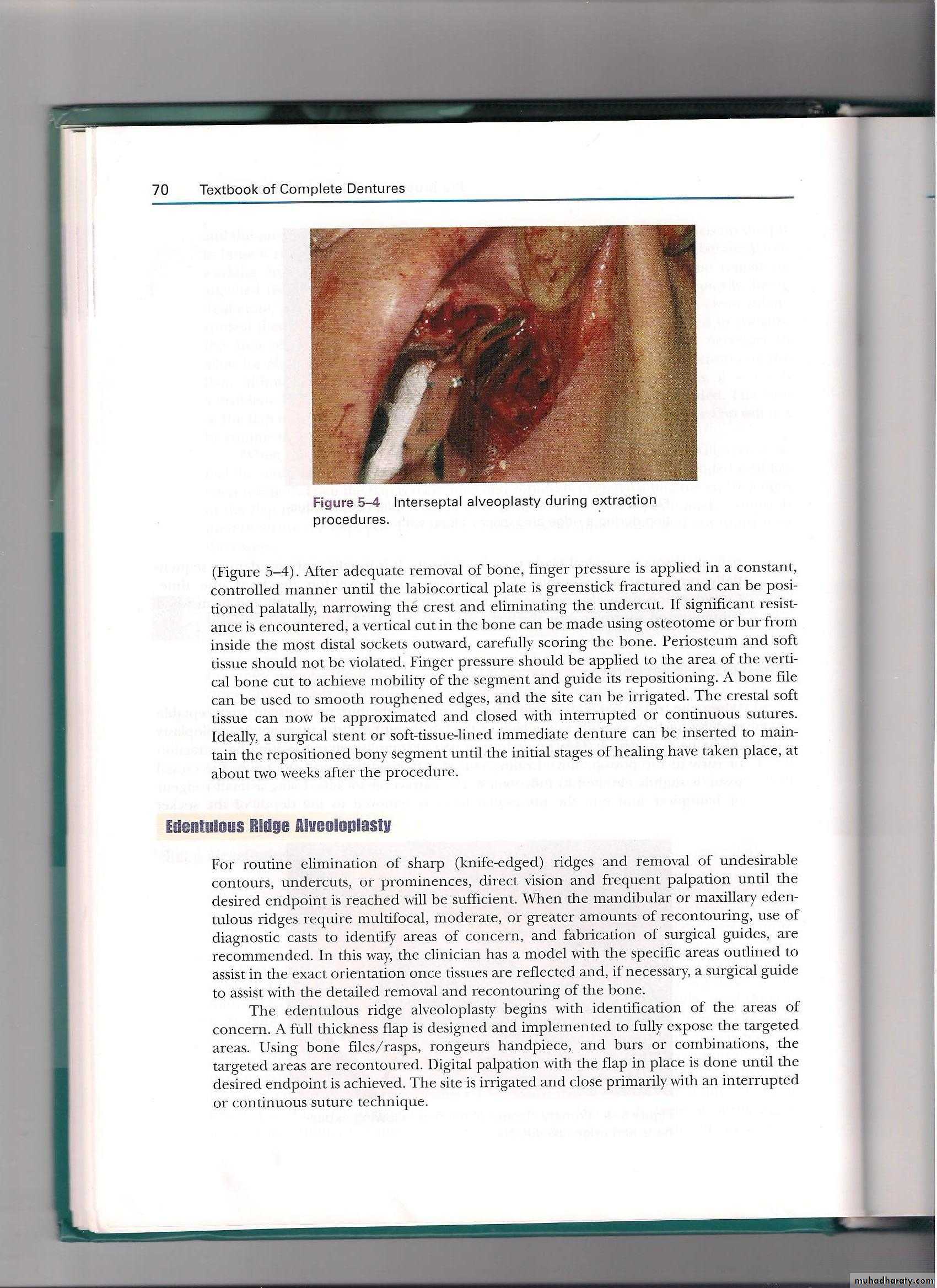
After teeth extraction, the crestal tissue is slightly elevated to fully exposed the extraction sockets. Using a small rongeur or hand piece and bur, the Intraseptal bone is removed to the depth of the socket (Figure 3) . after adequate removal of the bone, finger pressure is applied in a constant, controlled manner until the labio-cortical plate is green stick fractured and can be positioned palatally, narrowing the crest and eliminating the undesirable undercut. A bone file can be used to smooth roughened edges, suturing the area, a surgical stent of soft tissue –lined immediate denture can be inserted to maintain the positioned bony segment until healing about two weeks after procedure.
(Figure 3 )
C- Edentulous ridge aleveoloplasty( without extraction):
This procedure is indicated when there is knife edged ridges , undesirable contour or under cuts, prominences. Diagnostic cast was made to identify areas of concern. The areas were outlined to the exact tissues reflected .A full thickness flap is designed and implemented to fully exposure of the area. Using bone files/rongeur hand piece, and burs or combinations, the target areas are re-contoured, the site is irrigated and close primary with suture.D- Buccal exostosis:
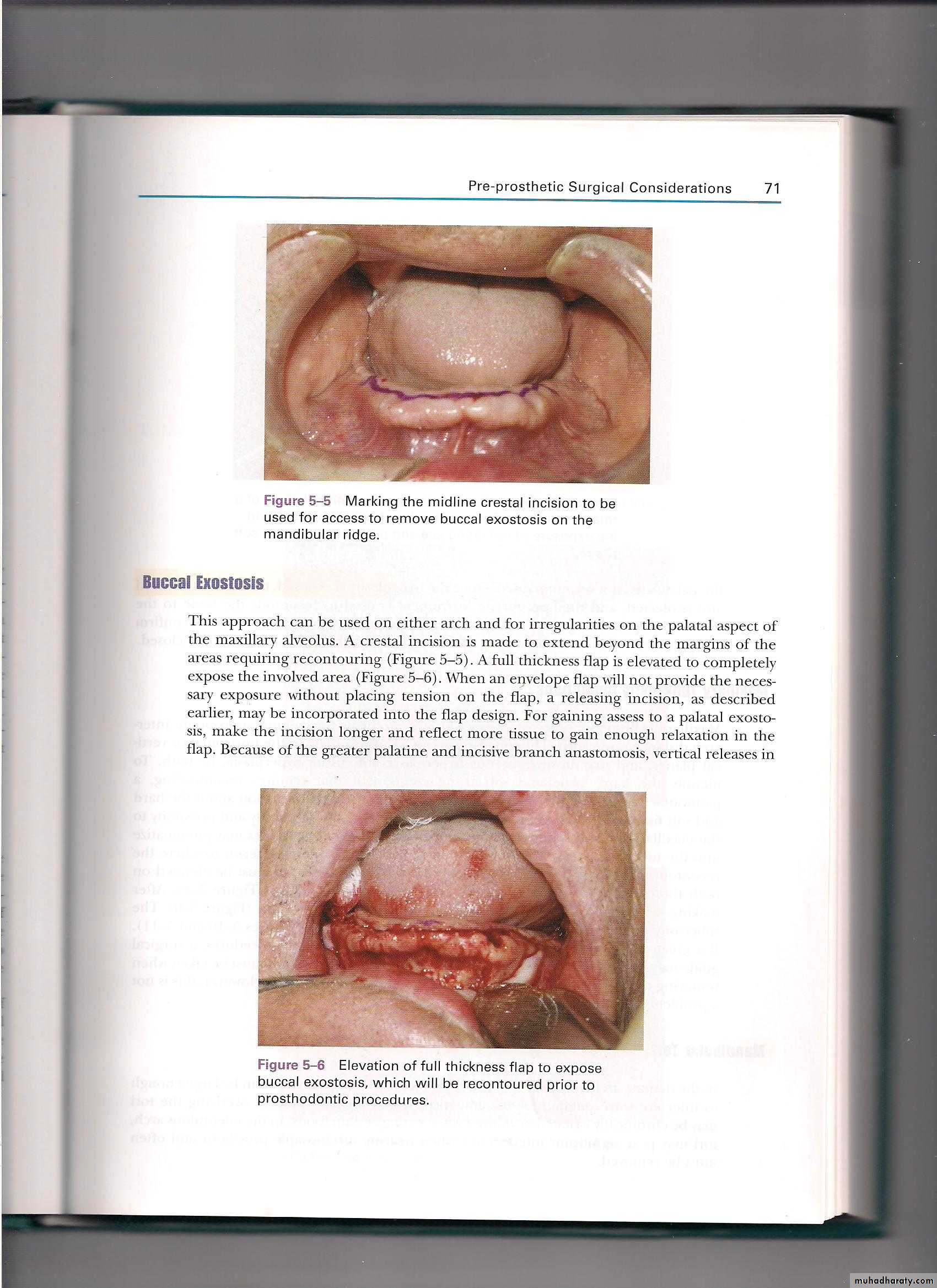
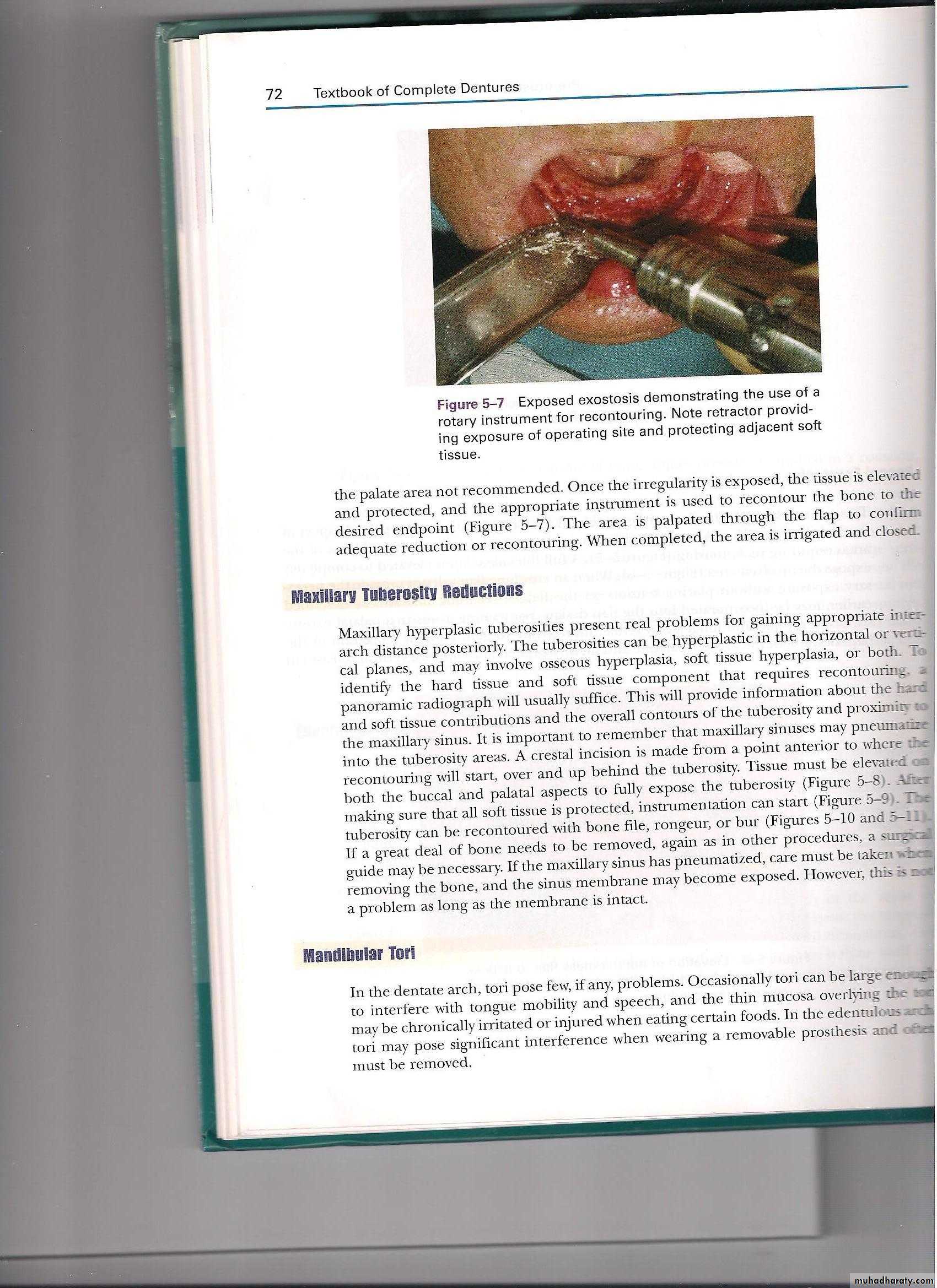
This approach can be used on either arch for irregularities on the palatal aspect of the maxillary alveolus. A crestal incision is made extend beyond the margins of the areas requiring re-contouring (Figure 4) . A full thickness flap is elevated to completely expose the involved area (Figure 5), once the irregularities is exposed, the tissue is elevated and protected, and the appropriate instrument is used to re-contour the bone to the desired endpoint (Figure 6) after completion of re-contouring the area is irrigated and closed.
(Figure 5)
(Figure 4)
(Figure 6)
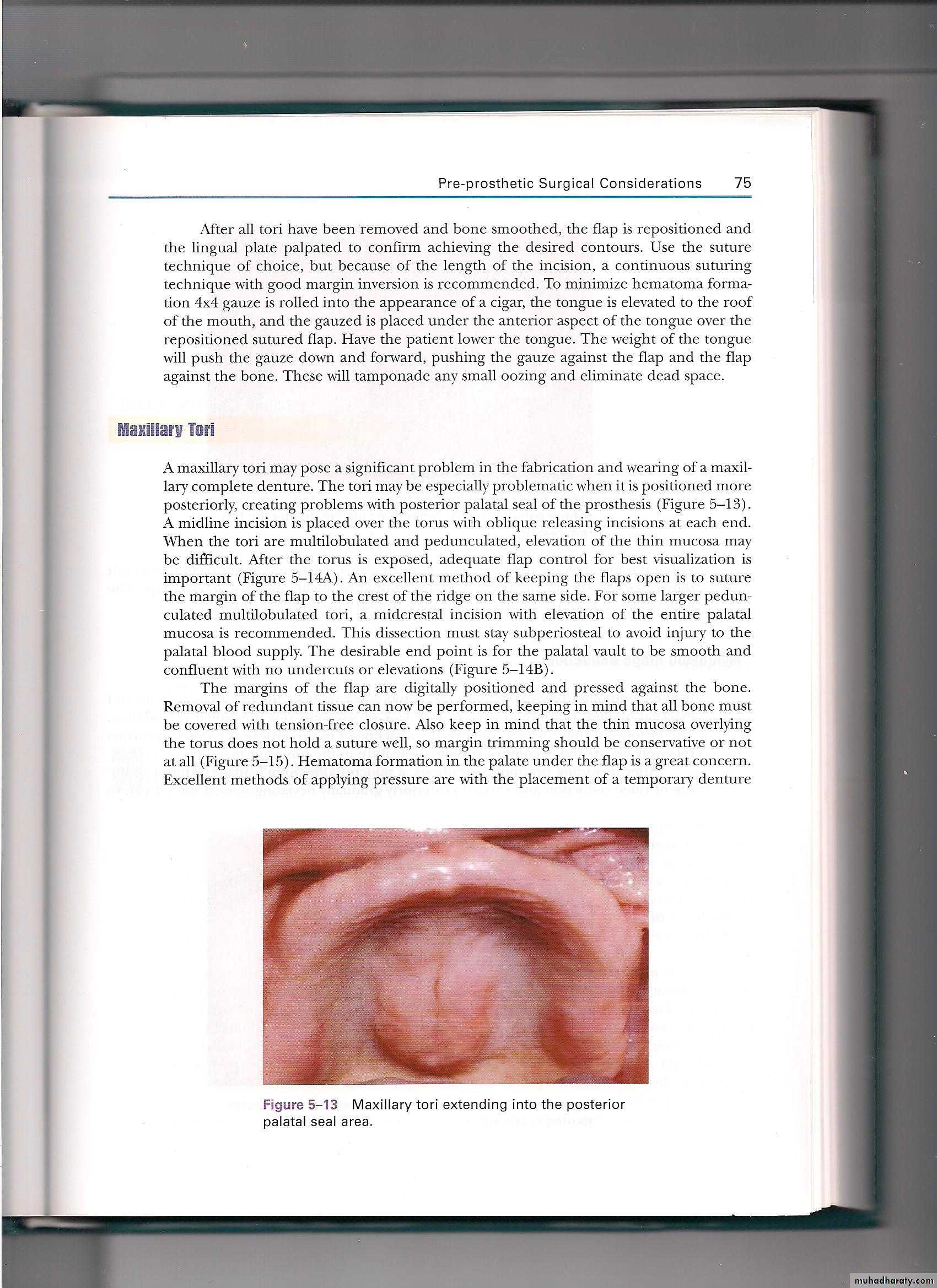
- Maxillary tuberosity reduction:
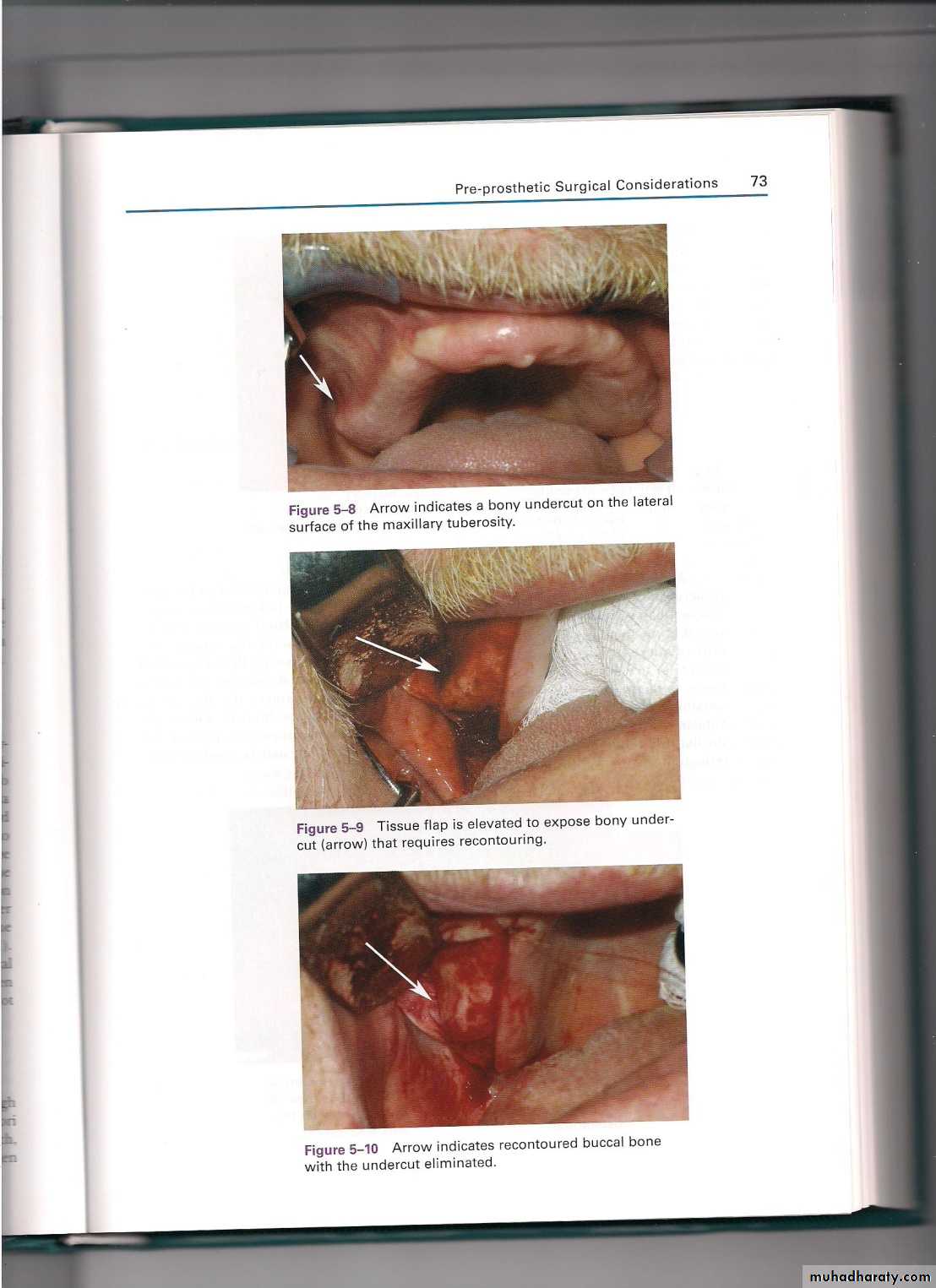
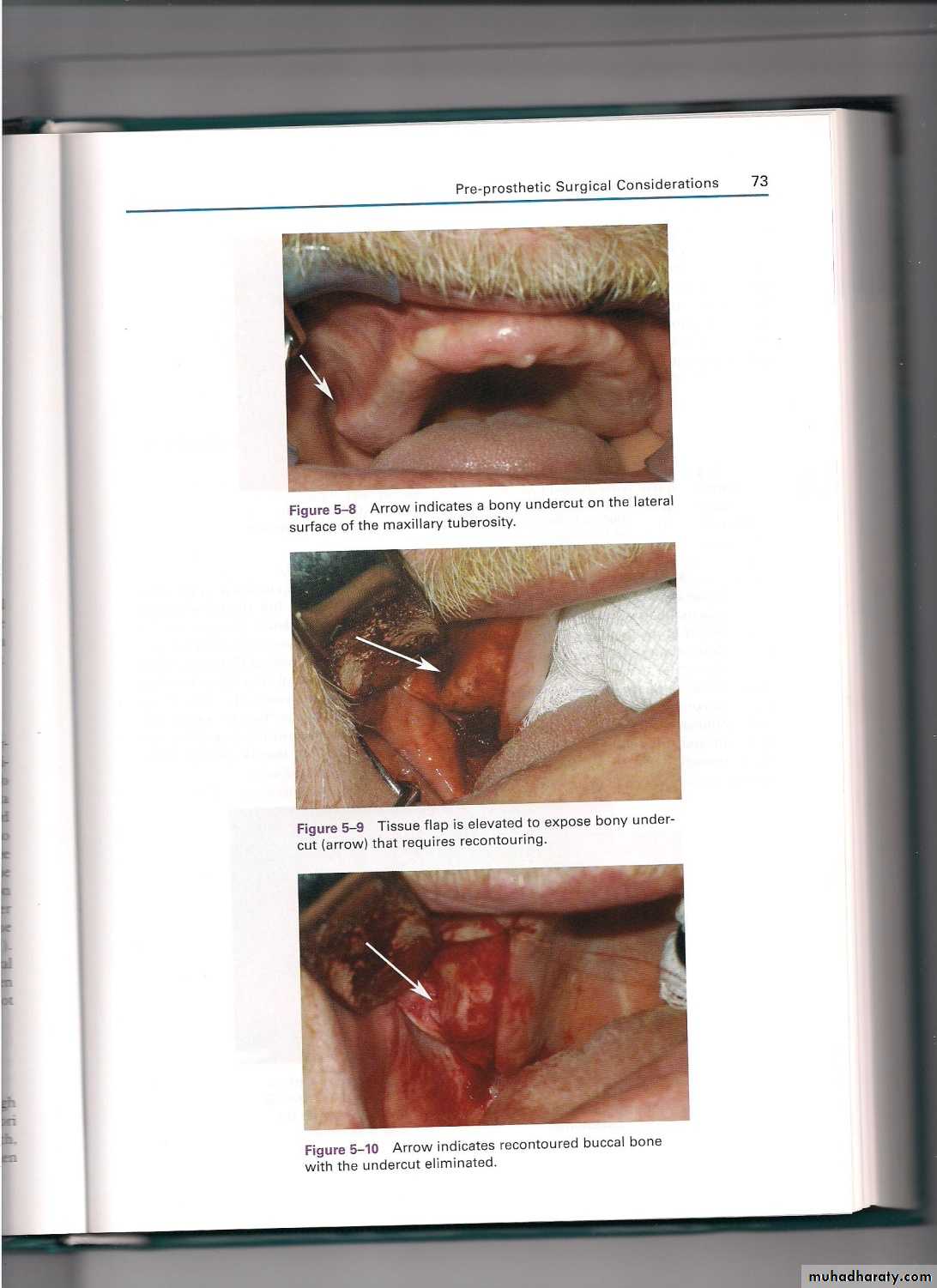
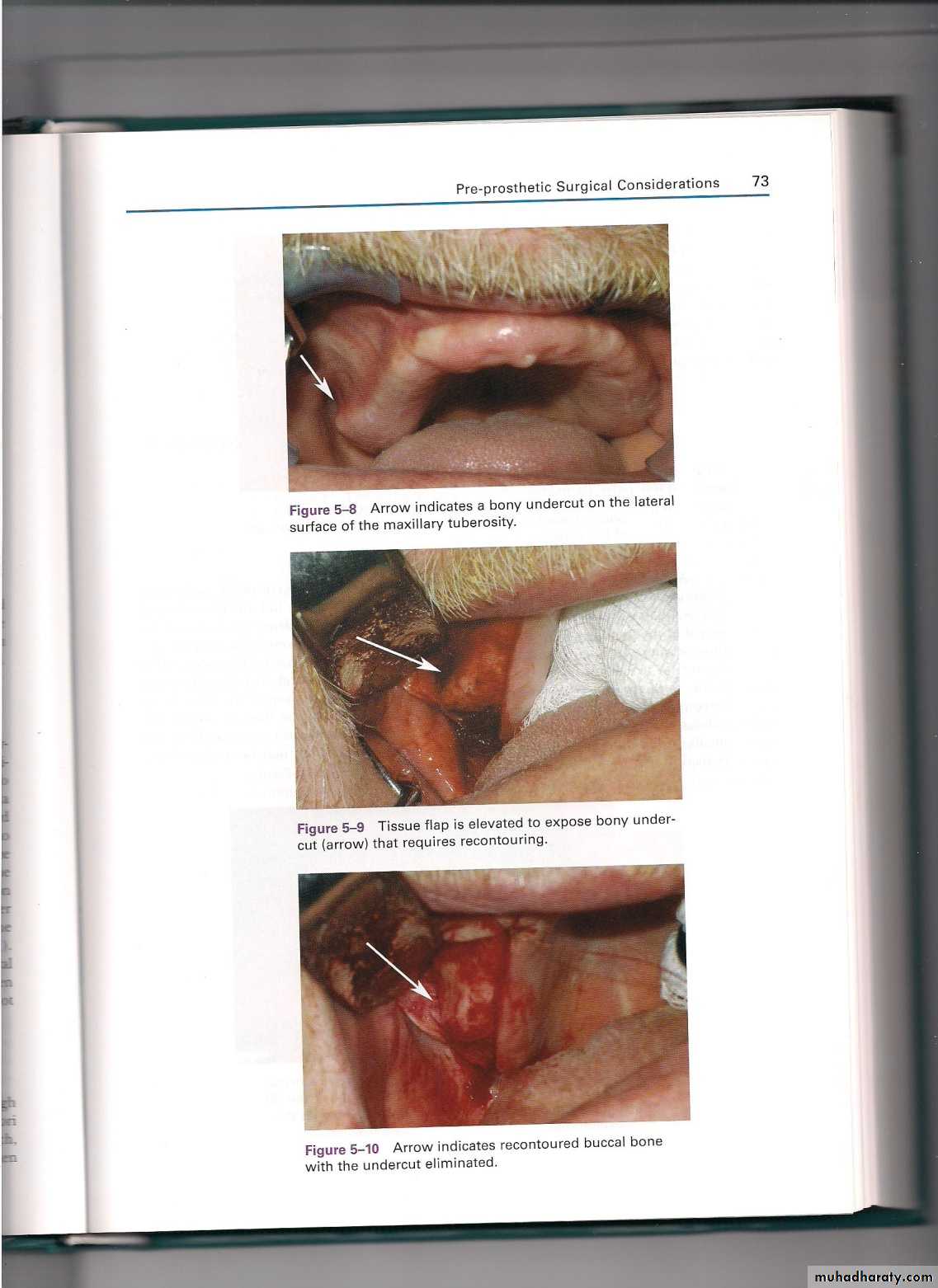
The maxillary tuberosities can be hyperplasic in the horizontal or vertical planes may involve tissue hyperplasia. To identify both hard or tissue that require re-contouring, a panoramic radiograph will usually important to identify the location of the maxillary sinuses. A crestal incision is made from a point anterior to where the re-contouring will start. Tissue must be elevated on both the buccal and palatal aspects to fully exposure the tuberosity (Figure 7), instrumentation can start (Figure 8) , the tuberosity can be re-contoured by using bone file, rongeur, or bur (Figure 9) care must be taken when removing the bone, and the sinus membrane may become exposed.
(Figure 7) (Figure8) (Figure9)
-Tori removal:A torus is a slowly growing osseous formation of unknown etiology. They can be variable in size, shape, location, and pattern. Usual locations are along the midline of the palate, and along the lingual aspect of the mandible.
The indications for removal of tori:
Extremely large torus 2. Torus that extends beyond denture periphery 3. Torus with traumatized mucosal coverage 4. Torus with deep undercuts 5. Torus that interferes with speech or mastication
6. Psychological reasons
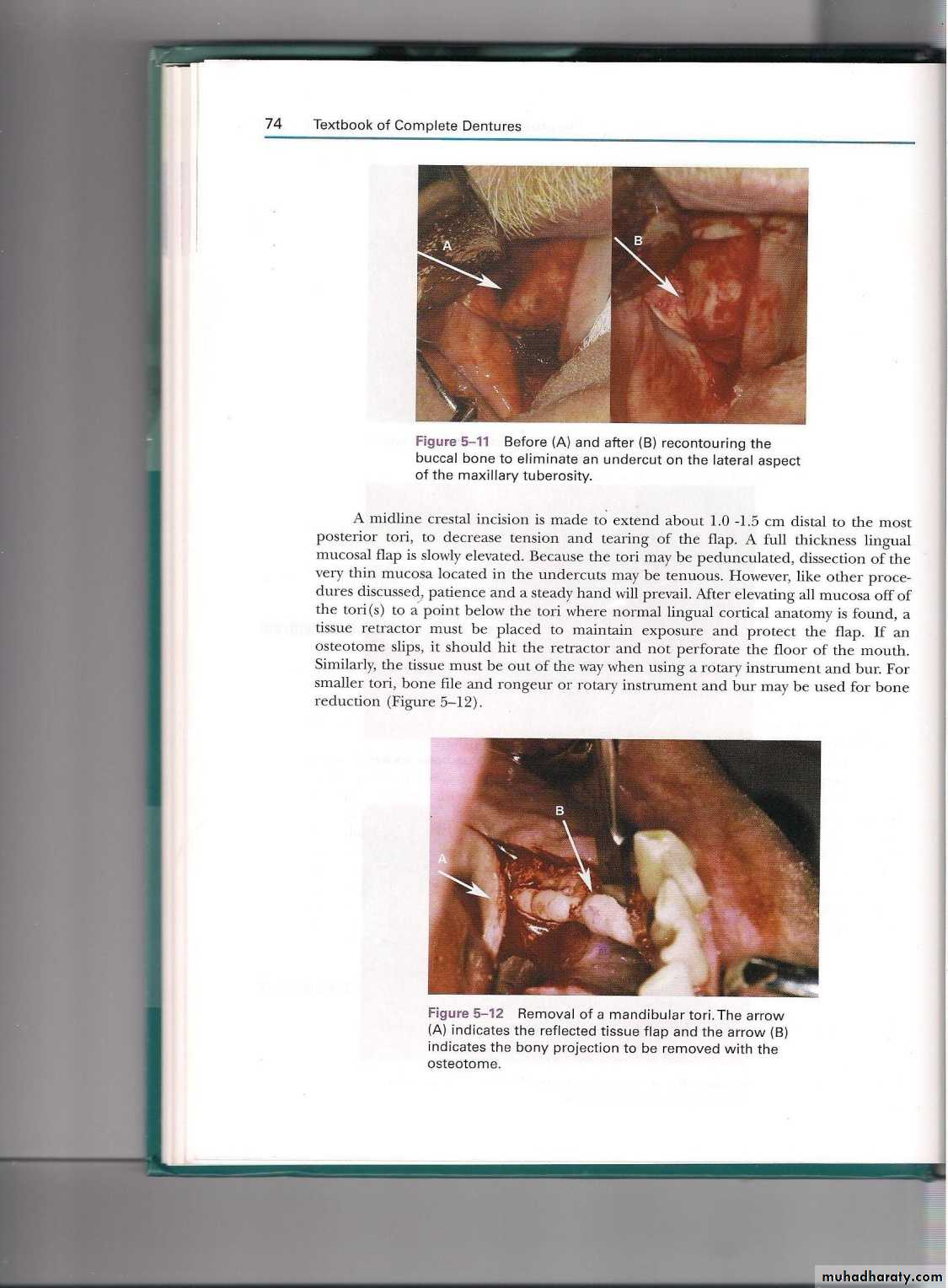
-Mandibular Tori
Tori in the mandibular arch may be large enough to interfere with tongue movement and speech, and the tori may be irritated or injured when eating certain foods. In the edentulous arch tori may pose significant interference when wearing a removable prosthesis and often must be removed. A midline crestal incision is made to extend about 1.0- 1.5 cm distal to the most posterior tori. A full thickness lingual mucosal flap is slowly elevated. Because the tori may be pedunculated, dissection of the very thin mucosa located in the under cuts may be tenous. After elevating the mucosa the tissue must be out of the way when using a rotary instrument and bur may be used for bone reduction (Figure10). After all tori have been removed and bone smoothed, the flap is repositioned and the lingual plate palpated to confirm a chewing the desire contours. Gauze is placed under the anterior aspect of the tongue to minimize the hematoma formation. The weight of the tongue will push the gauze down and forward, pushing the gauze against the flap and the flap against the bone.(Figure10)
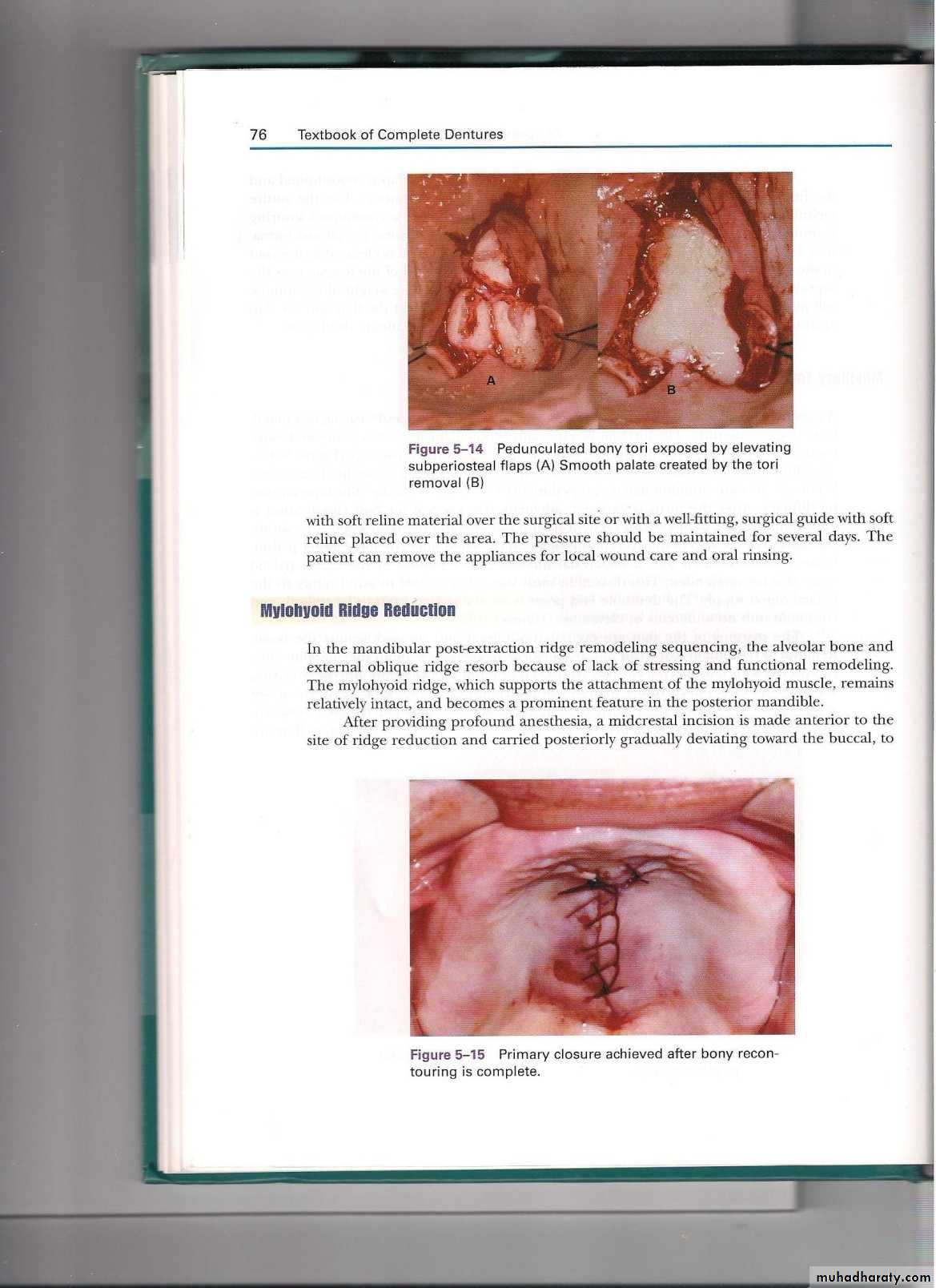
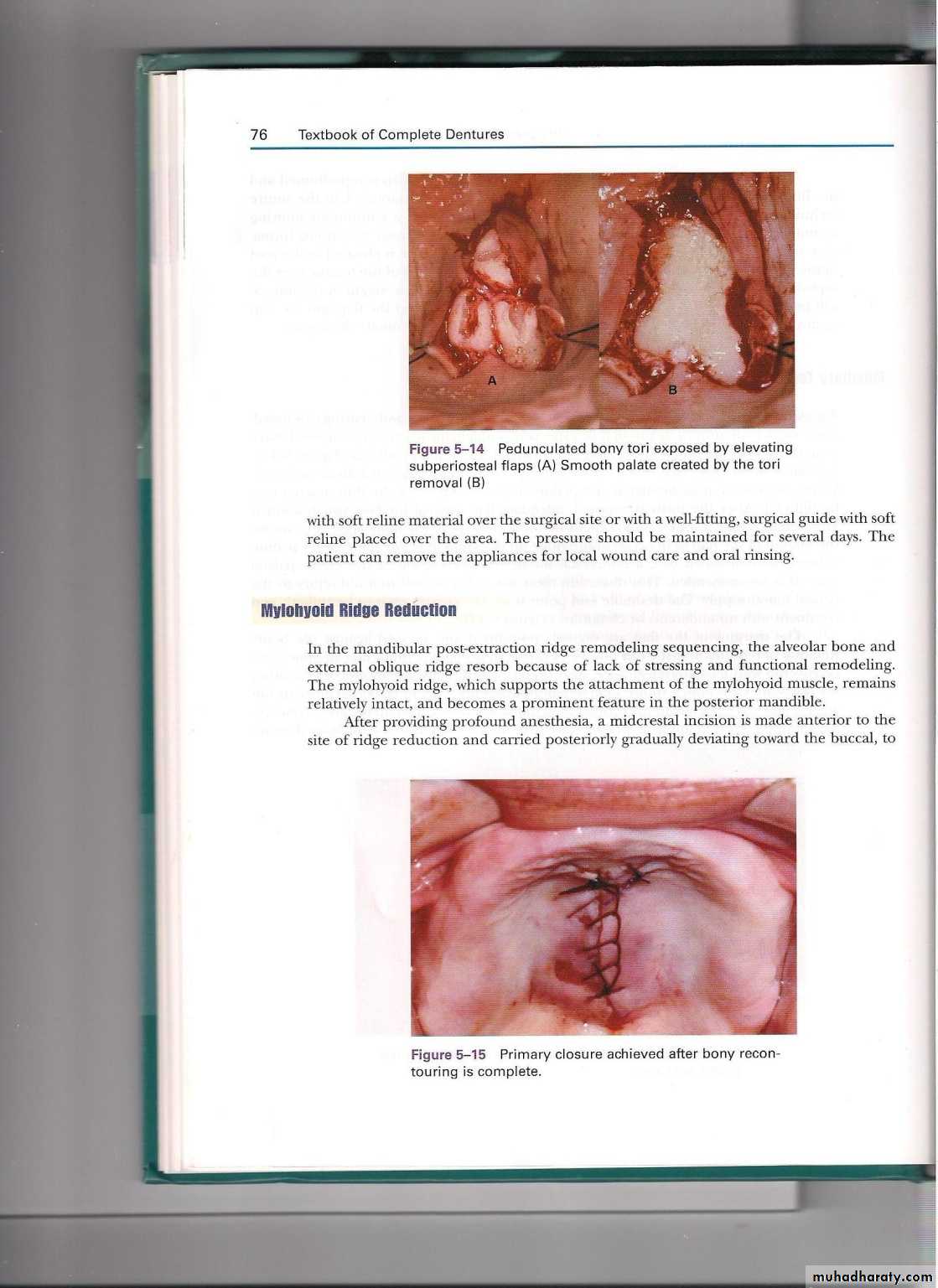
-Maxillary tori:
A maxillary tori may a significant problem in the fabrication and wearing of a maxillary complete denture. The tori may be more problematic when it is positioned more posteriorly, creating problems with posterior palatal seal of the prosthesis ( Figure11). A midline incision is placed over the torous with oblique releasing incisions at each end, when the tori multi-lobulated , elevation of the thin mucosa may be difficult. After the torus is exposed ( Figure 12) removal of the bony tissue can be performed. Hematoma formation in the palate under the flap is a great concern. A temporary denture lined with soft liner or tissue conditioner placed to be over the surgical site , the pressure should be maintained for several days ( Figure 13).
( Figure 11) ( Figure12) ( Figure 13)
-Mylohyoide ridge reduction:
In the mandibular post –extraction ridge remodeling sequencing, the alveolar bone and external oblique ridge resorb because of lack of stressing and functional remodeling, the mylohyiod ridge, which supports the attachment of the mylohyiod muscle, remains relatively intact, and becomes a prominent feature in the posterior mandible, a mid crestal incision is made anterior to the site of ridge reduction and carried posteriorly gradually deviating toward the buccal to avoid potential injury to the lingual nerve. The flab is elevated to expose the mylohyiod ridge and attached muscle. The tendenous attachments of the mylohyiod muscle are stripped. The muscle will retract into the floor of the mouth and re-attach during healing by using a bur can be used to reduce the ridge to the desired height or using the bone file to fin-tune the contouring, the area then irrigated and closed by suturing. The denture with a soft liner is placed to allow for the lingual flange to help with displacement of the de-attached mylohyiod muscle.
-Genial tubercle reduction:
In the post extraction ridge remodeling of the mandible, the alveolar ridge and tooth-bearing areas resorb because of lack of stressing and functional loading. Because the constant movement of the tongue and stressing of the tubercles once the alveolus has resorbed and remodeled, the genial tubercles can become very prominent structures in the anterior mandible and interfere with denture seating , a full thickness flap is elevated to expose the genial tubercle and genioglosussus muscle attachments. The tendons are de-attached from the bone to more inferiorly , the bone height can be reduced with the instrument of choice to the desired level, the area irrigated and closed for healing.
-Augmentation surgeries:
Augmentation with synthetic graft materials. Hydroxyapatite (H.A) is a non-resorbable ceramic bone substitute, which comes in a granular form in a syringe, and may be placed alone, or combined with autogenous bone to augment the atrophic ridge.-Procedure Incisions are made down to the periosteum, and a subperiosteal tunnel developed on the crest of the alveolar ridge. The hydroxyapatite is injected, filling the tunnel. The incisions are then sutured closed. The hydroxyapatite is then molded with finger pressure to form an ideal ridge, and a stent placed.
H.A crystals
2- Onlay Bone grafting:
3- Interpositional bone graft: This procedure can be used to augment the atrophic maxilla or mandible. It was developed in an attempt to overcome the main disadvantage of mandibular onlay grafting, i.e., rapid resorption.
- Procedure The maxilla or mandible is "split", elevated, positioned and supported by interposed grafts of autogenous bone or cartilage, freeze dried bone, alloplastic material, or combinations of these grafts.
Synthetic bone
-Soft tissue related surgery
A-Hypermobile tissue: Excessive tissue is usually the result of the resorption of the underlying bone. If adequate alveolar height will remain after reduction of hypermobile tissue, then excision may be indicated. If the ridge is atrophic and the bone is thin and sharp, excision may result in a greater deficiency. If the alveolar height is inadequate ridge augmentation or vestibuloplasty were done.
B-Papillary hyperplasia: When hyperplastic tissue forms on the hard palate, it usually takes a papillary form. The condition usually begins as a series of tiny papillary projections that gives the palate a velvety appearance. Later it assumes a more nodular form.
Some potential causes of papillary hyperplasia: Mechanical irritation, ill fitting dentures, poor oral hygiene, fungal infections, and the associated inflammation.
Options in the treatment of papillary hyperplasia:Non surgical treatment such as proper denture adjustment and tissue conditioning, surgical excision, electrosurgery, or abrasion of the superficial layer of palatal mucosa.
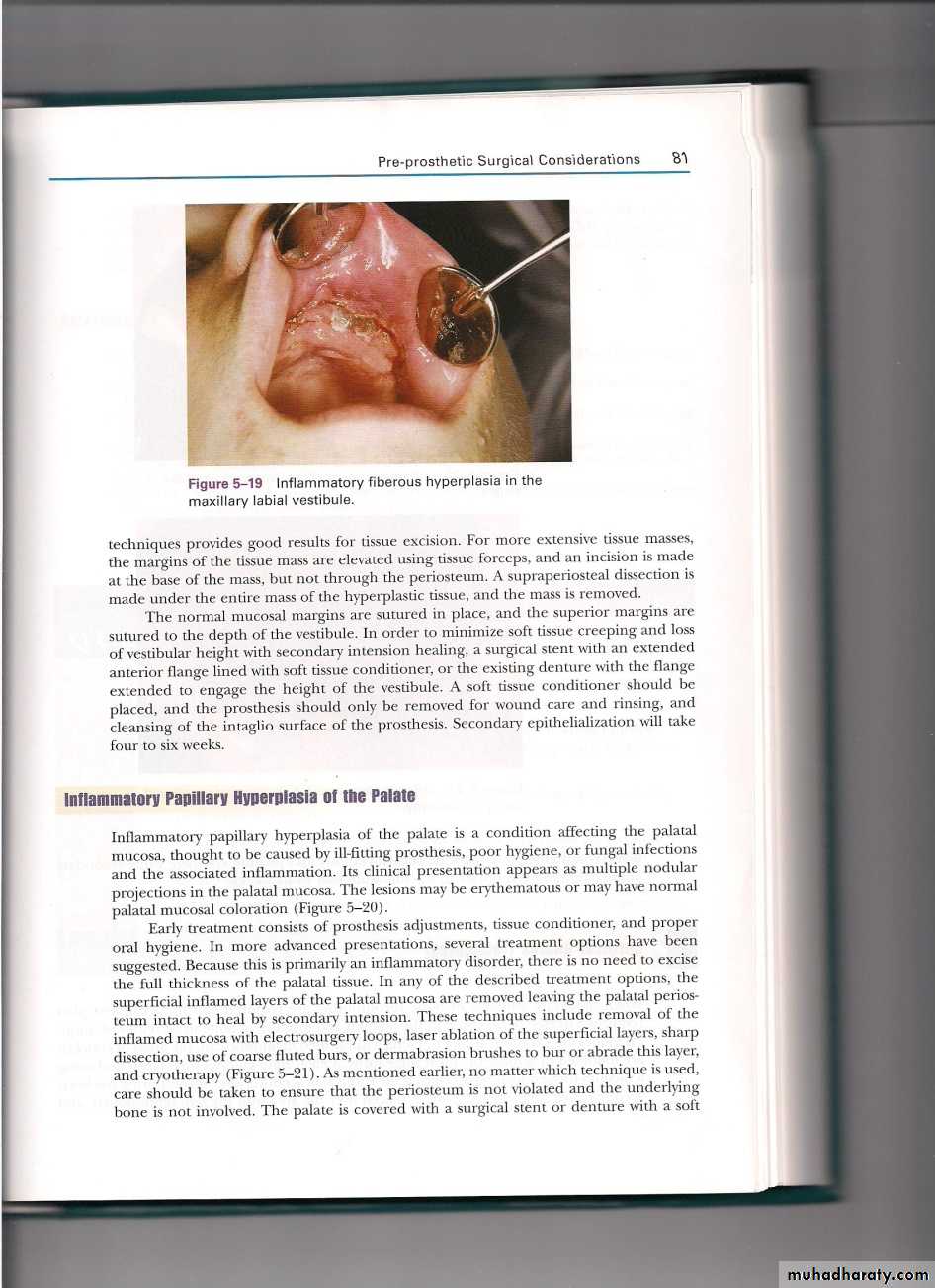
C-Inflammatory fibrous hyperplasia (epulis fissuratum): A continuous fold of hyperplastic tissue may form to fill the space between an ill fitting denture and the alveolus. It may appear as a lobulated localized mass which can be hidden under the denture, extending both behind and in front of the flange. In long-standing cases, multiple folds may form.
The most common cause: denture irritation from an ill fitting denture, allergic or chemical reactions to the denture material, or carcinoma. All excised tissue should be submitted for histological examination.
Treatment: Correction of denture irritation, placement of a soft liner, electrosurgery(if small) or conventional surgery (if larger)
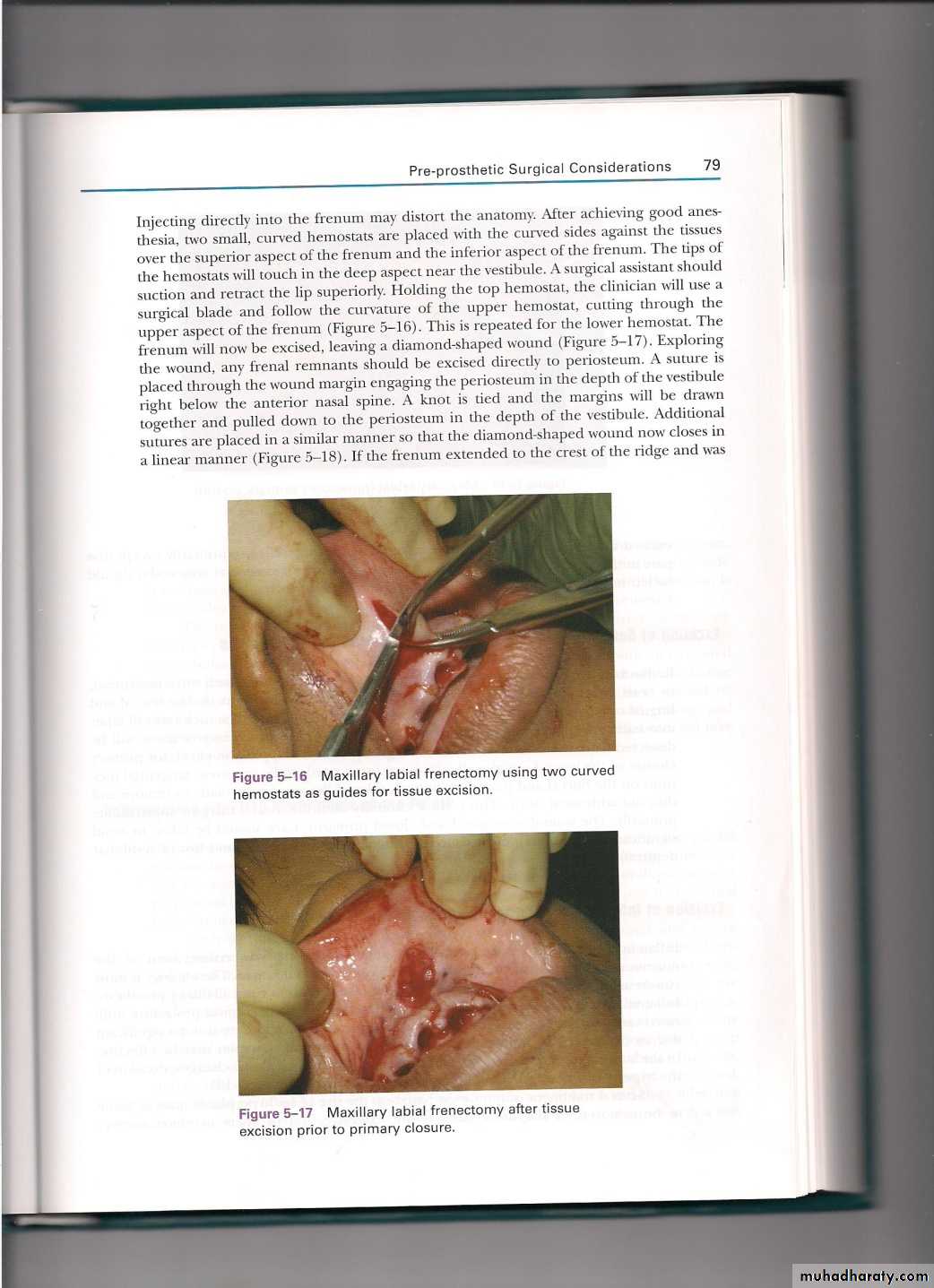
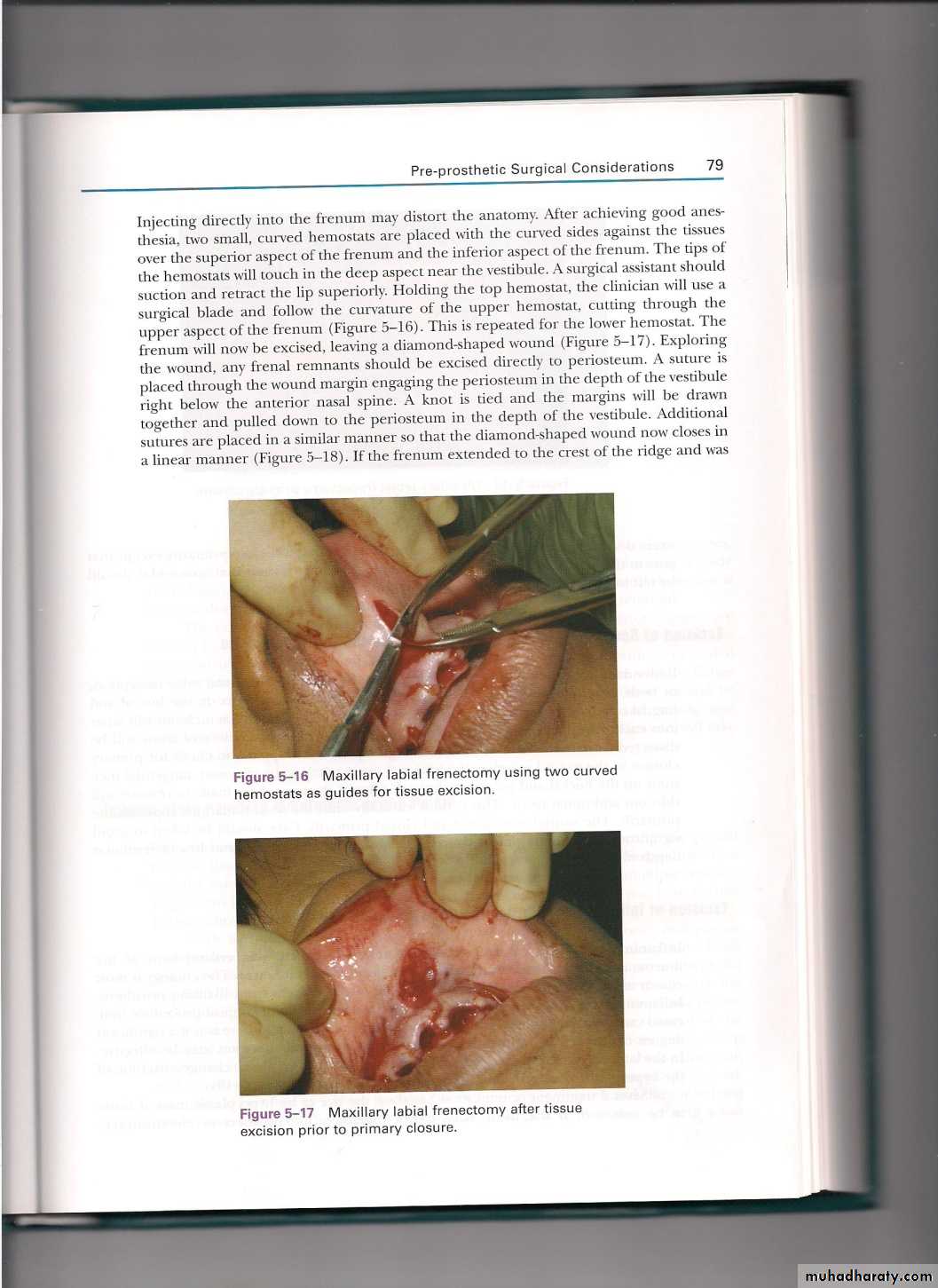
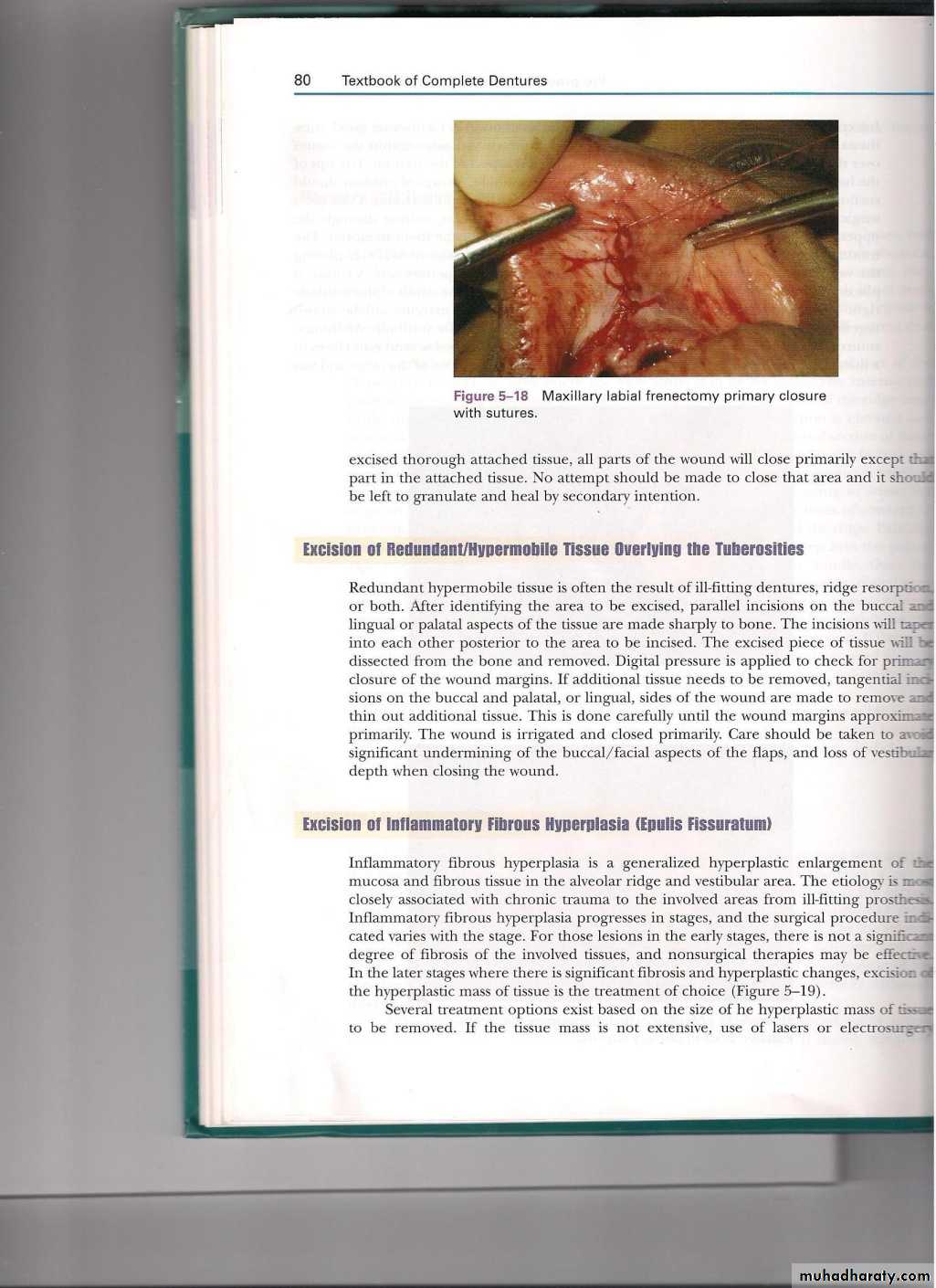
Frenectomy The labial frenum is usually not a problem in the dentate patient unless associated with a diastema. In the edentulous patient, it may be irritated by the flange of the denture. Movement of the soft tissue adjacent to the frenum may create discomfort and ulceration and may interfere with the peripheral seal and dislodge the denture. An abnormal lingual frenum may bind the tip of the tongue to the posterior surface of the mandibular alveolar ridge, and can affect speech and interfere with denture stability.
Treatment: Simple excision, Z-plasty, or localized vestibuloplasty with secondary epithelialization, localized supraperiosteal dissection removing the fibrous attachment.
Maxillary tuberosity reduction of soft tissue. The amount of soft tissue available for reduction can often be determined radiographically, or with a sharp probe after local anesthesia. It may be necessary to remove both soft tissue and bone to achieve the desired result.
Vestibuloplasty: goal of the vestibuloplasty is to expose and make available for denture construction that bone which is still present.
Procedure
The surgeon detaches the origin of muscles on either facial or lingual side of the edentulous ridge. Healing occurs by secondary epithelialization or by skin or mucosal graft. Vestibuloplasties with skin grafts do not seem to accelerate bony resorption. If healing occurs by secondary epithelialization, bone resorption changes of 4-20% may occur over a 2 year period.
Complications: Loss of sensation if the mental nerve is dissected, sagging of the chin if the mentalis muscle is completely dissected, and hypotonia
The indications for performing a transpositional flap vestibuloplasty: This procedure is indicated primarily for patients with sufficient mandibular bony height and an adequate vestibular sulcus on the lingual aspect of the mandible. It can be accomplished successfully without a splint or can be combined with immediate reinsertion of a modified relined denture or splint in order to maintain tissue adaptation in the depth of the vestibule.
The indications for lowering the floor of the mouth: As the alveolar bone is resorbed, the attachments of the mylohyoid and genioglossus muscles may interfere with the lingual aspect of the denture.
Miscellaneous:
Nerve relocation: In the case of severe atrophy of mandibular alveolar bone, the mental neurovascular bundle may occupy a position at the superior aspect of the mandible.
Complication: Trauma from the denture on the superior portion of the alveolar ridge in this area can produce pain. When the discomfort is persistent, relocation of the mental neurovascular bundle may be required.
Sinus grafting: Placement of endosteal implants in the posterior edentulous maxilla often requires grafting of the floor of the maxillary sinus. Also commonly referred to as a sinus lift procedure, materials may be used are Alloplastic material, allogenic bone, autogenous bone, or a combination of these materials.
Tissue sclerosing: As an alternative to other procedures for treating the hypermobile alveolar ridge, injection of a sclerosing agent (sodium morrhuate) can produce fibrosis in soft hyperplastic tissue.