
The orbit is a pear-shaped cavity, the stalk of which is the optic canal (Fig. 3.1).
• The roof
consists of two bones:
1. the lesser wing of the sphenoid and
2. the orbital plate of the frontal bone.
It is located subjacent to the anterior cranial fossa and the frontal sinus. A defect in
the orbital roof may cause pulsatile proptosis due to transmission of cerebrospinal
fluid pulsation to the orbit.
• The lateral wall
also consists of two bones:
1. The greater wing of the sphenoid and
2. The zygomatic.
The anterior half of the globe is vulnerable to lateral trauma since it protrudes
beyond the lateral orbital margin.
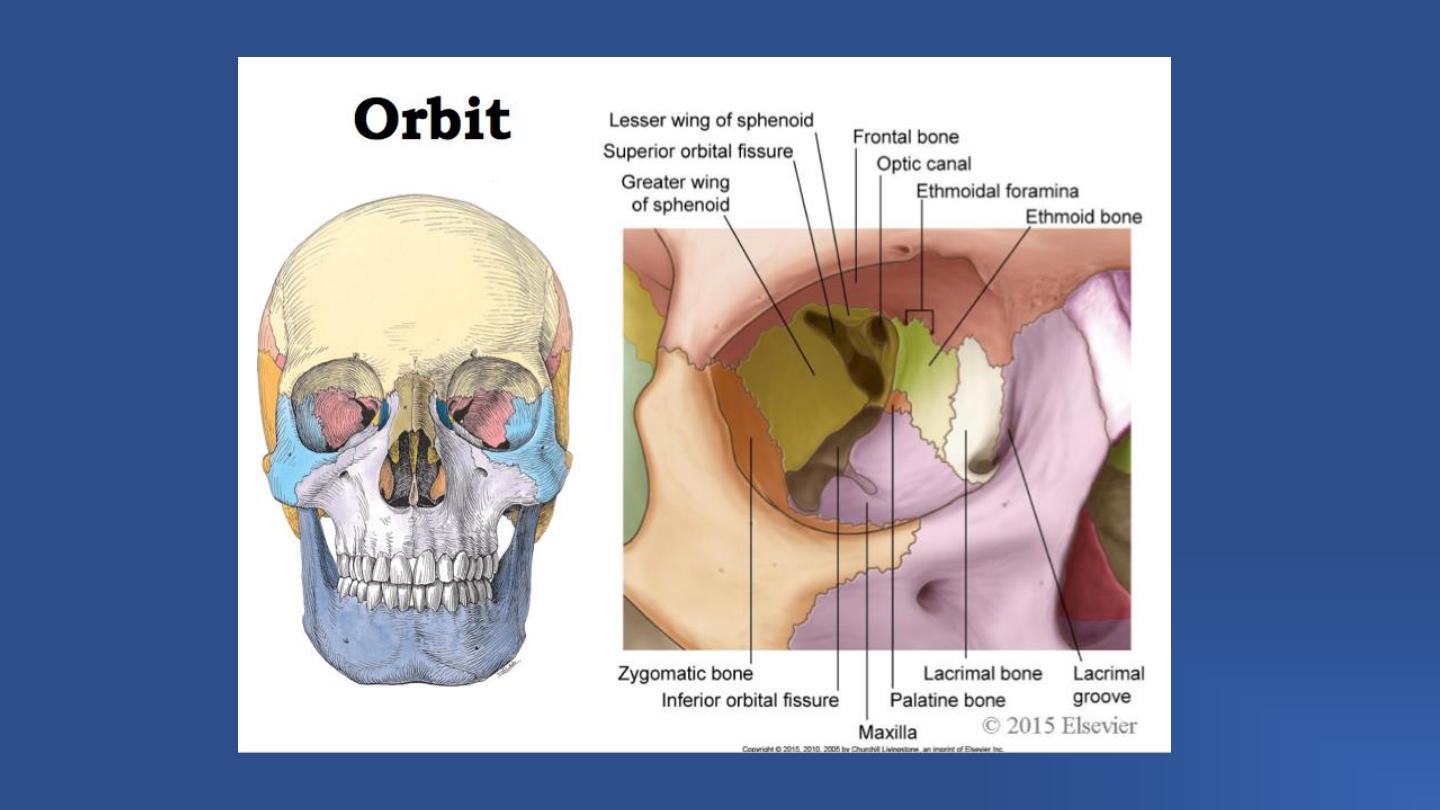

• The floor
consists of three bones:
1. The zygomatic,
2. Maxillary and
3. Palatine.
The posteromedial portion of the maxillary bone is relatively weak and may be involved
in a ‘blowout’ fracture (see Ch. 21). The orbital floor also forms the roof of the maxillary
sinus so that maxillary carcinoma invading the orbit may displace the globe upwards.
• The medial wall
consists of four bones:
1. Maxillary,
2. Lacrimal,
3. Ethmoid and
4. Sphenoid.
The lamina papyracea, which forms part of the medial wall, is paper-thin and perforated by
numerous foramina for nerves and blood vessels.
Orbital cellulitis is therefore frequently secondary to ethmoidal sinusitis.
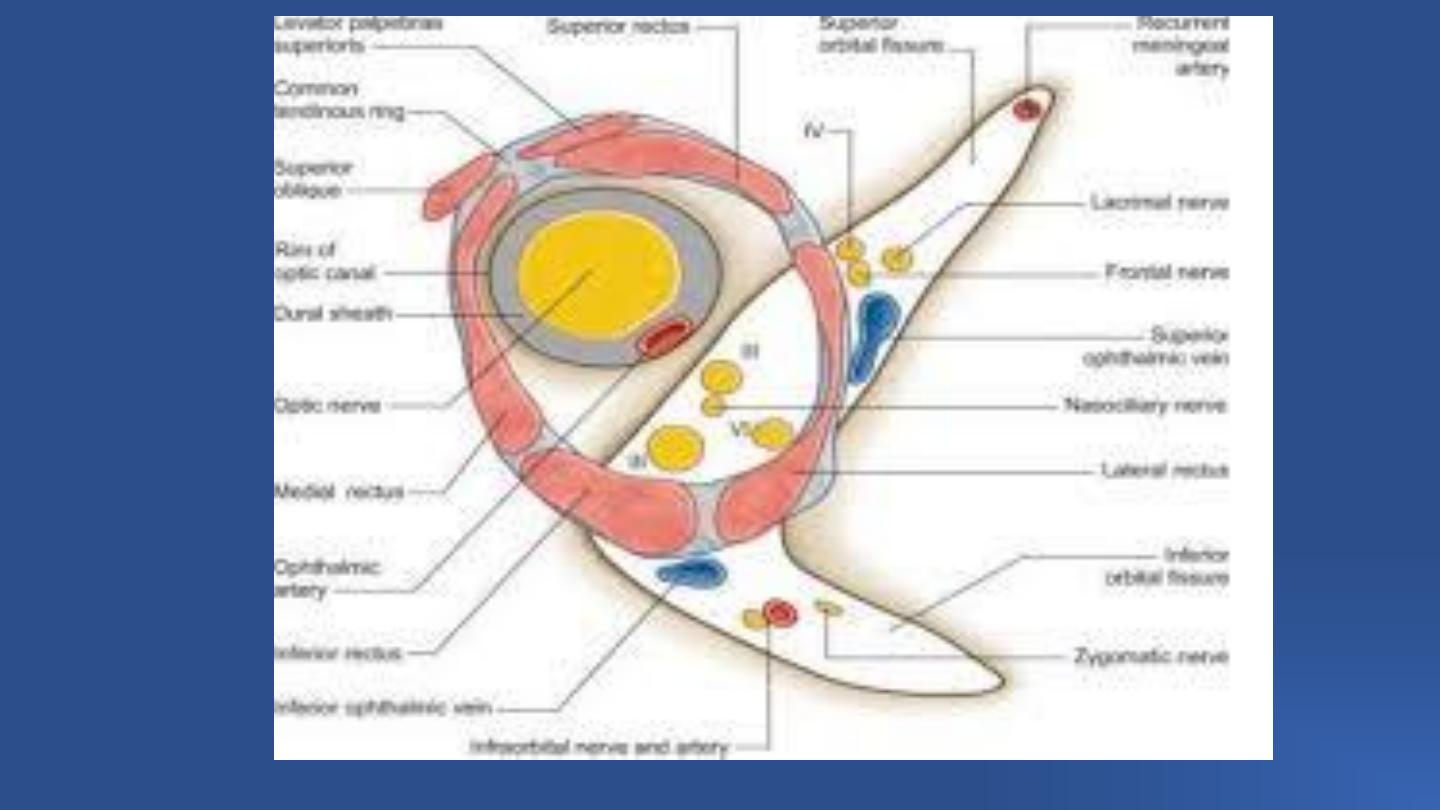
• The superior orbital fissure
is a slit linking the cranium and the orbit, between
the greater and lesser wings of the sphenoid bone; through it pass numerous important
structures.
○ The superior portion contains the lacrimal, frontal and trochlear nerves, and the
superior ophthalmic vein.
○ The inferior portion contains the superior and inferior divisions of the oculomotor
nerve, the abducens and nasociliary nerves, and sympathetic fibers from the
cavernous plexus.
○ Inflammation of the superior orbital fissure and apex (Tolosa–Hunt syndrome) may
therefore result in a multitude of signs including ophthalmoplegia and venous outflow
obstruction.
• The inferior orbital fissure
lies between the greater wing of
the sphenoid and the maxilla, connecting the orbit to the pterygopalatine and
infratemporal fossae. Through it run the maxillary nerve, the zygomatic nerve and
branches of the pterygopalatine ganglion, as well as the inferior ophthalmic vein.
Symptoms of orbital disease include
1. Eyelid and conjunctival swelling,
2. Redness,
3. Watering,
4. Pain (sometimes on, or exacerbated by, eye movement),
5. Increasing ocular prominence,
6. Displacement or a sunken impression of the eye,
7. Double vision and blurring, and
8. Sometimes a pulsing sensation or audible bruit.
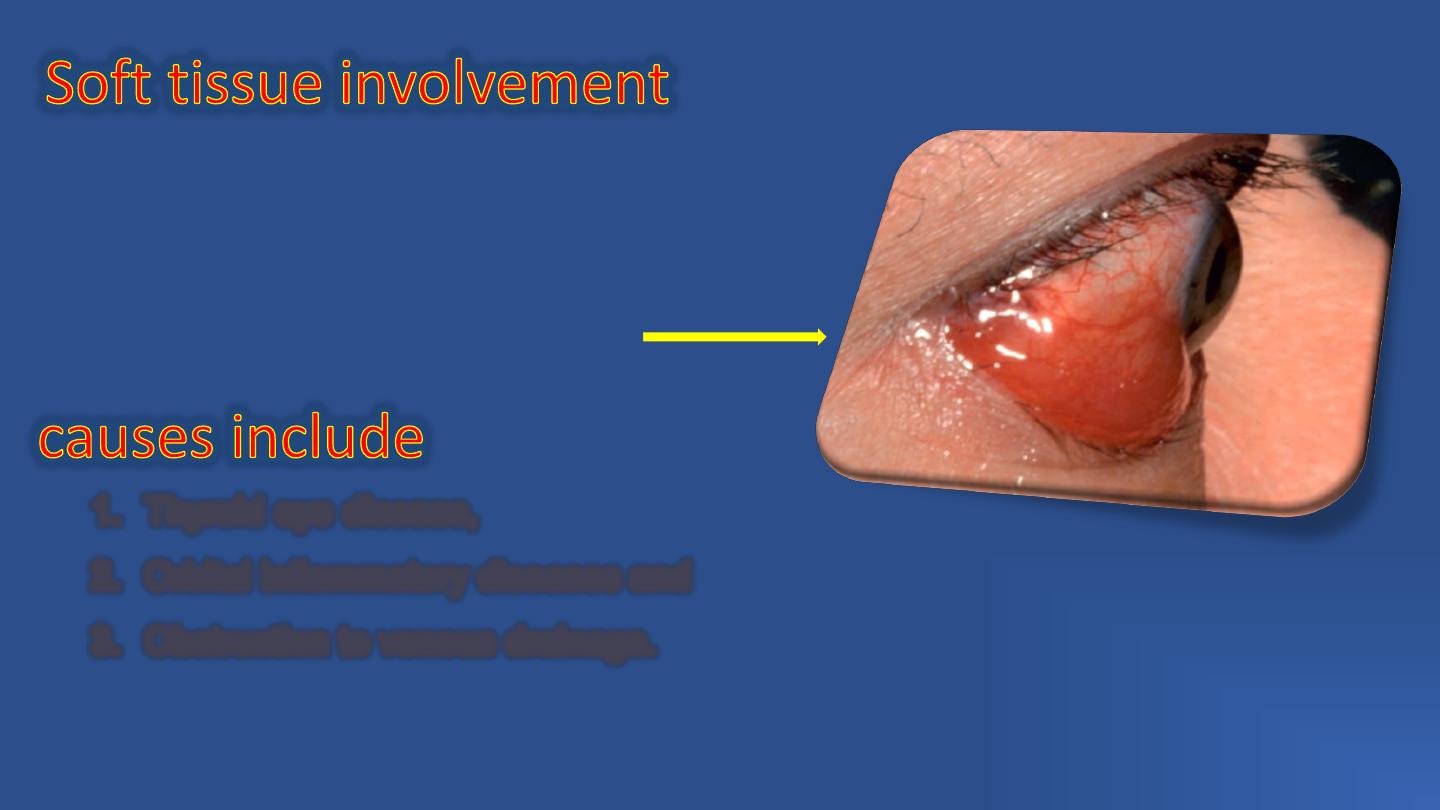
1. Eyelid and periocular oedema,
2. Skin discoloration,
3. Ptosis ,
4. Chemosis (oedema of the conjunctiva) and
5. Epibulbar injection may be seen;
1. Thyroid eye disease,
2. Orbital inflammatory diseases and
3. Obstruction to venous drainage.
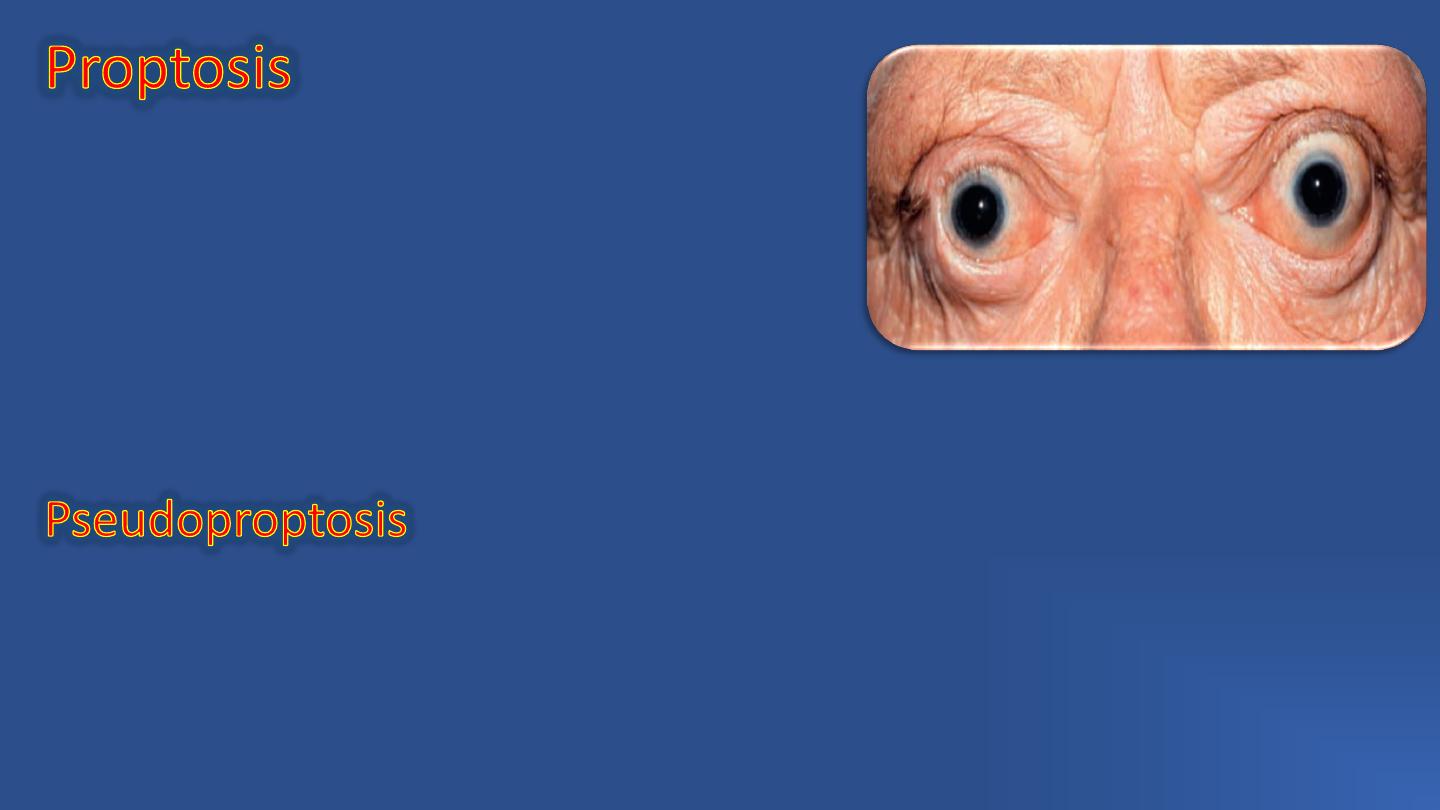
Proptosis an abnormal protrusion of the eyeball;
exophthalmos refers specifically to the eyeball
only.
Proptosis may be caused by
Retrobulbar lesions or,
Shallow orbit.
The intraorbital portion of the optic nerve is longer (25 mm) than the distance
between the back of the globe and the optic canal (18 mm). This allows for
significant forward displacement of the globe (proptosis) without excessive stretching
of the nerve.
Pseudoproptosis (the false impression of proptosis) may be due to
:
1.Facial asymmetry,
2.Enlargement of the globe (e.g. high myopia or buphthalmos),
3.Lid retraction or
4.Contralateral enophthalmos.
Enophthalmos implies recession of the globe within the orbit. Causes include
1. Congenital and traumatic orbital wall abnormalities,
2. Atrophy of the orbital contents (e.g. radiotherapy, scleroderma, chronic eye
poking in blind infants
– the ‘oculodigital’ sign) or
3. Sclerosis
(e.g.
metastatic
scirrhous
carcinoma,
sclerosing
orbital
inflammatory disease).
Pseudoenophthalmos may be caused by a
1. Small or shrunken eye (microphthalmos or phthisis
bulbi).
2. Ptosis.
3. Contralateral proptosis or pseudoproptosis.
Defective ocular motility is very common in orbital disease. Causes include an
1. orbital mass,
2. restrictive myopathy (e.g. thyroid eye disease, orbital myositis, tethering of
muscles or tissue after orbital wall fracture),
3. ocular motor nerve involvement associated with lesions in the cavernous sinus,
orbital fissures or posterior orbit (e.g. carotid
–cavernous fistula, Tolosa–Hunt
syndrome, malignant lacrimal gland tumours).
• Increasing venous pressure
by dependent head position, the
Valsalva manoeuvre or jugular compression may induce or exacerbate proptosis
in patients with orbital venous anomalies or infants with orbital capillary
haemangioma.
• Pulsation
is caused either by an arteriovenous communication or a defect
in the orbital roof. In the former, pulsation may be associated with a bruit
depending on the size of the communication. In the latter the pulsation is
transmitted from the brain by the cerebrospinal fluid and there is no associated
bruit. Mild pulsation is best detected on the slit lamp, particularly by applanation
tonometry.
• A bruit
is a sign found with a larger carotid
–cavernous fistula. It is best heard
with the bell of the stethoscope and is lessened or abolished by gently
compressing the ipsilateral carotid artery in the neck.
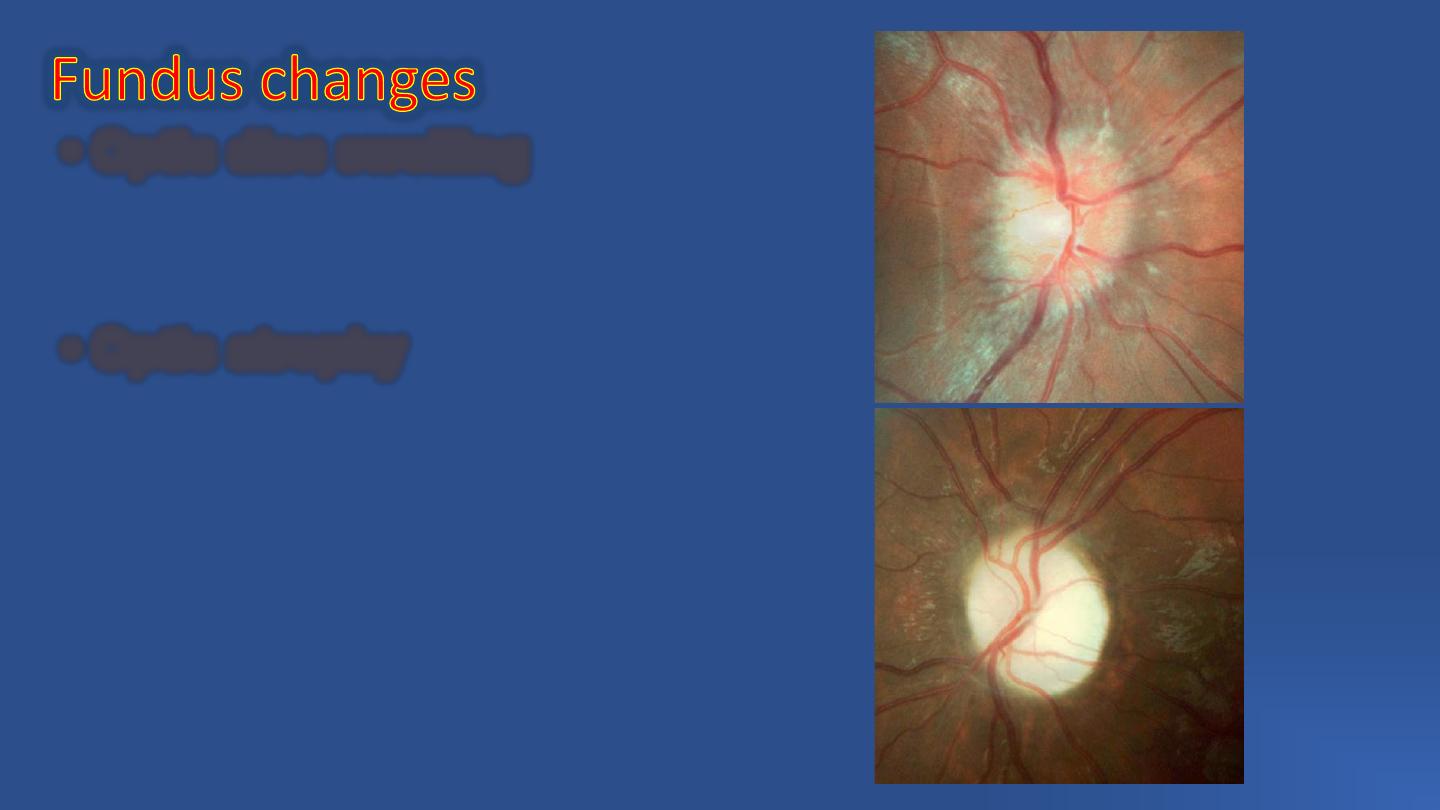
• Optic disc swelling
may be the initial
feature of compressive optic neuropathy .
• Optic atrophy
, which may be preceded
by swelling, is a feature of severe compressive
optic neuropathy. Important causes include
thyroid eye disease and optic nerve tumours.
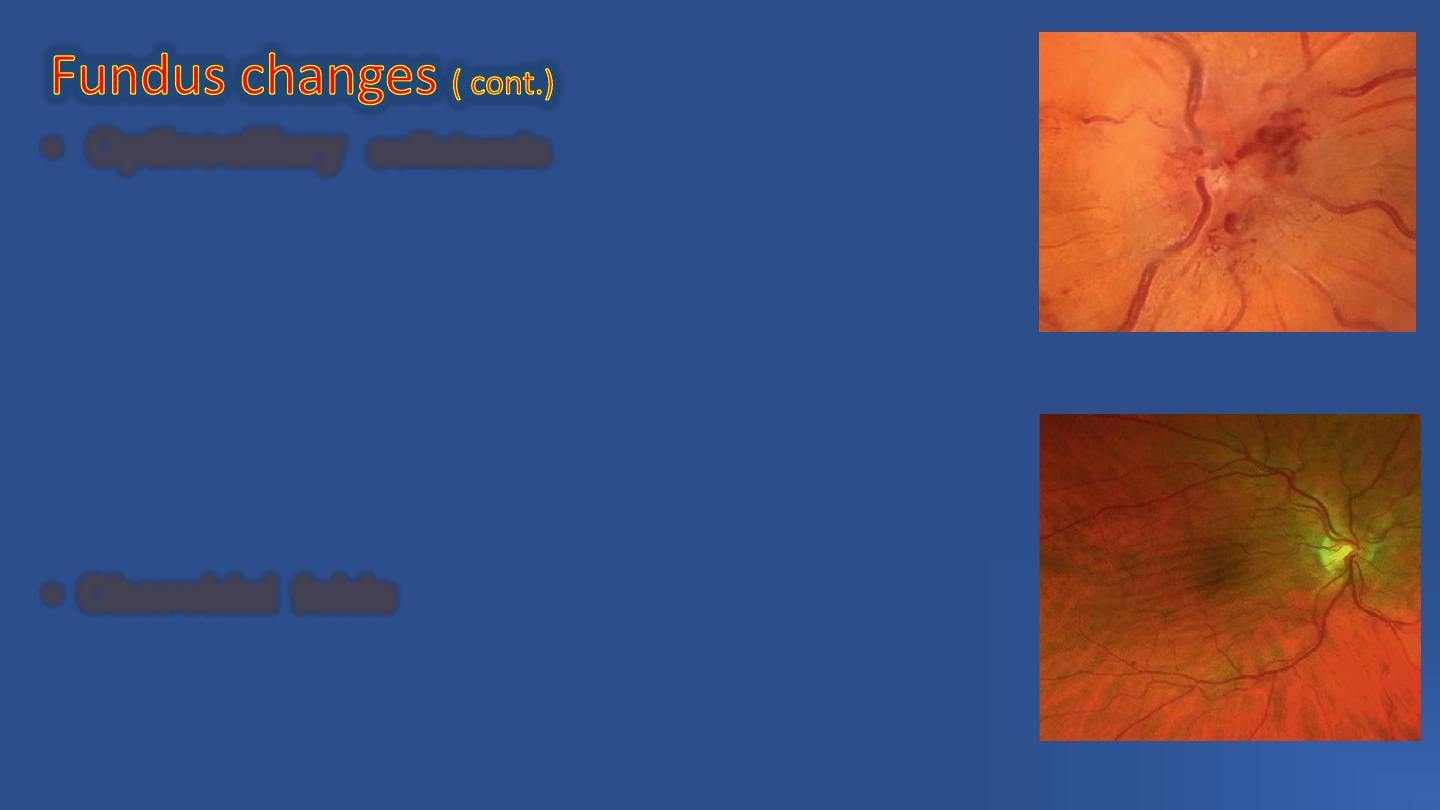
• Opticociliary
collaterals
consist of enlarged pre-existing
peripapillary capillaries that divert blood from the central retinal venous
circulation to the peripapillary choroidal circulation when there is
obstruction of the normal drainage channels. On ophthalmoscopy the
vessels appear as large tortuous channels most frequently sited
temporally, which disappear at the disc margin (Fig. 3.6C). The collaterals
may be associated with any orbital or optic nerve tumour that compresses
the intraorbital optic nerve and impairs blood flow through the central
retinal vein. The most common tumour associated with shunts is an optic
nerve sheath meningioma but they may also occur with optic nerve
glioma, central retinal vein occlusion, idiopathic intracranial hypertension
and glaucoma.
• Choroidal folds
Choroidal folds are parallel grooves or striae
involving the inner choroid, Bruch membrane, the RPE and sometimes
the retina (chorioretinal folds). they may occur in a wide variety of orbital
lesions. Although tending to be more common with greater amounts of
proptosis and anteriorly located tumours, in some cases their presence
can precede the onset of proptosis.
is useful for depicting bony structures and the
location and size of space-occupying lesions. It is of particular value in patients with
orbital trauma because it can detect small fractures, foreign bodies, blood, herniation
of extraocular muscle and emphysema (see Ch. 21). It is, however, unable to
distinguish different pathological soft tissue masses that are radiologically isodense.
Confirmation of an orbital abscess in cellulitis is a relatively common indication.
can demonstrate orbital apex lesions
and intracranial extension of orbital tumours, and is useful for imaging orbital
inflammatory disease. Serial short T1 inversion recovery (STIR) scans are valuable in
assessing inflammatory activity in thyroid eye disease (see Ch. 19).
are little used except for the initial diagnosis of traumatic bony injury.
can provide useful information, particularly with high-grade
apparatus and an experienced operator, but does not image the orbital apex well.
is sometimes performed, particularly in suspected
neoplastic disease. Potential problems include haemorrhage and ocular penetration.
TED, also known as
and
,
Is a very common orbital disorder, and is the most common cause of both bilateral
and unilateral proptosis in an adult.
Thyrotoxicosis (hyperthyroidism) is a condition involving excessive secretion of
thyroid hormones.
Graves disease, the most common form of hyperthyroidism, is an autoimmune
disorder in which IgG antibodies bind to thyroid stimulating hormone (TSH)
receptors in the thyroid gland and stimulate secretion of thyroid hormones.
It is more common in
and may be associated with other autoimmune
disorders.
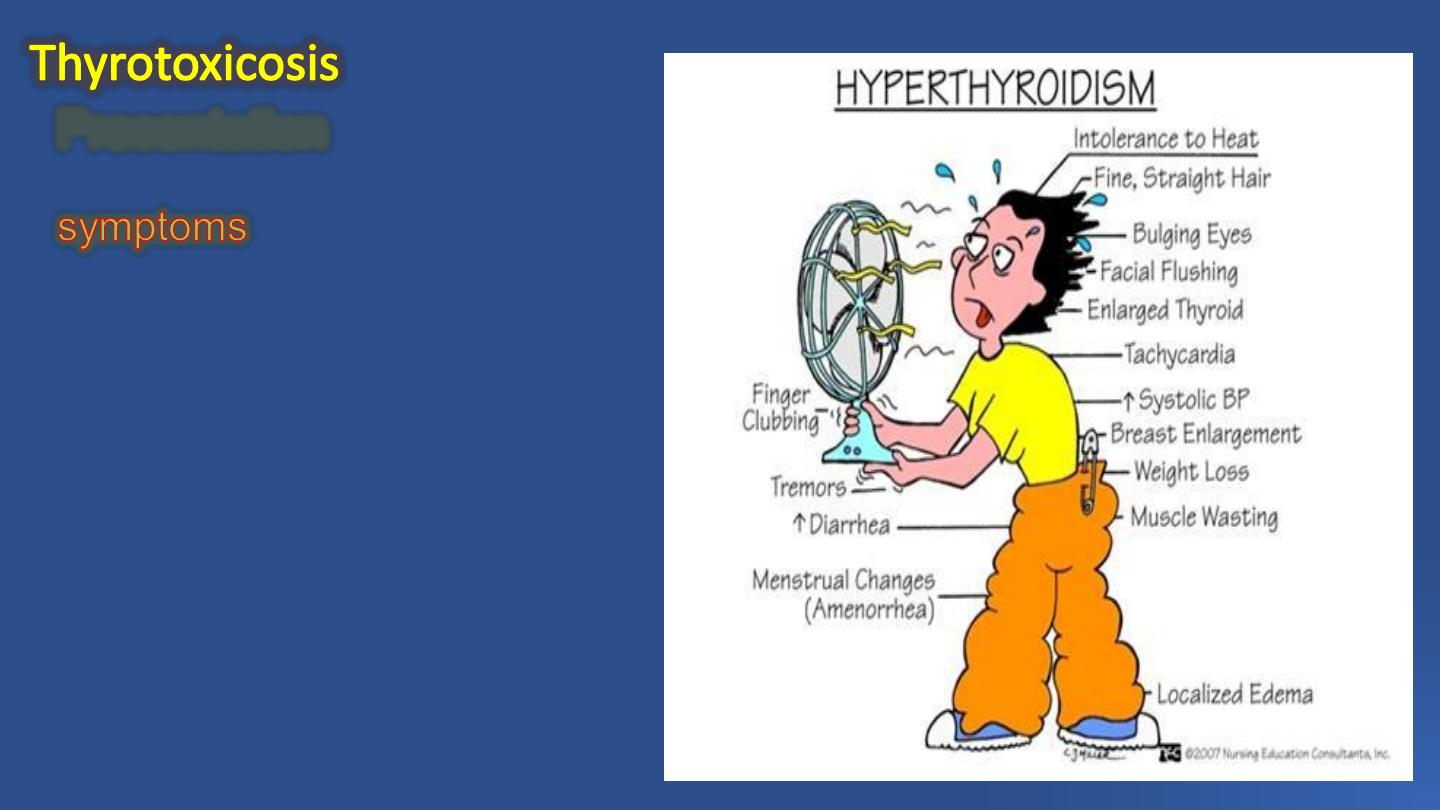
Presentation
In the fourth or fifth decades.
including
Weight loss despite good appetite,
Increased bowel frequency,
Sweating,
Heat intolerance,
Nervousness,
Irritability,
Palpitations,
Weakness and fatigue.
There may be
enlargement of the thyroid gland,
Tremor,
Palmar erythema, and
Warm and sweaty skin.
is a phenomenon similar to clubbing of the fingers.
is indurated thickening of the skin of the shins.
may include sinus tachycardia and other arrhythmias.
can be associated.
Thyroid function is commonly tested initially with a TSH level; if this is low, or
normal but thyroid disease is still suspected, a range of additional investigations
can be carried out.
Presentation

Treatment options include
1. Carbimazole,
2. Propylthiouracil,
3. Propranolol,
4. Thyroid ablation with radioactive iodine
5. Partial thyroidectomy.
Treatment

Risk factors for ophthalmopathy
The major clinical risk factor for developing TED is
S MOK IN G.
Wo men
are five times more likely to be affected by TED than men, but this
largely reflects the increased incidence of Graves disease in women.
R a d io a c tive io d in e
used to treat hyperthyroidism can worsen TED.
TED can also, though less commonly, occur in euthyroid and hypothyroid (including
treated hyperthyroid) patients.
Thyroid ophthalmopathy involves an organ-specific autoimmune reaction in
which an antibody that reacts against thyroid gland cells and orbital fibroblasts
leads to inflammation of extraocular muscles, interstitial tissues, orbital fat and
lacrimal glands characterized by pleomorphic cellular infiltration, associated
with increased secretion of glycosaminoglycans and osmotic imbibition of
water.
There is an increase in the volume of the orbital contents, particularly the
muscles, which can swell to eight times their normal size. There may be a
secondary elevation of intraorbital pressure, and the optic nerve may be
compressed.
Subsequent degeneration of muscle fibres eventually leads to fibrosis, which
exerts a tethering effect on the involved muscle, resulting in restrictive
myopathy and diplopia.

TED typically proceeds through a
in
which the eyes are red and painful; this tends to remit within 1–3 years and
only about 10% of patients develop serious long term ocular problems.
follows in which the eyes are white,
although a painless motility defect may be present.
Clinical features broadly can be categorized into
(i) soft tissue involvement,
(ii) lid retraction,
(iii) proptosis,
(iv) optic neuropathy and
(v) restrictive myopathy.
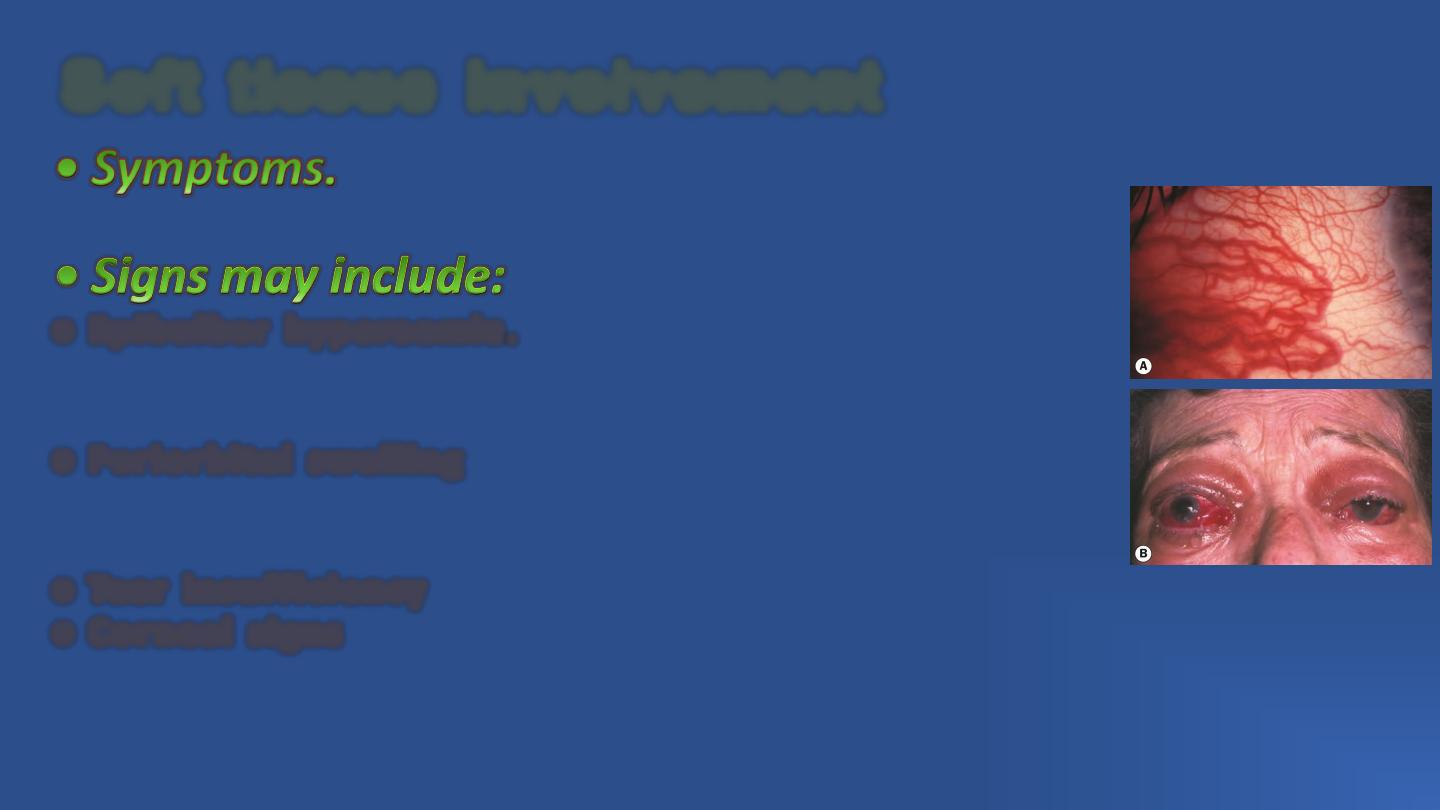
Grittiness, red eyes, lacrimation, photophobia, puffy
lids and retrobulbar discomfort.
○ E p i b u l b a r h y p e r a e m i a . This is a sensitive sign of inflammatory
activity. Intense focal hyperaemia may outline the insertions of the
horizontal recti.
○ P e r i o r b i t a l s w e l l i n g is caused by oedema and infiltration behind
the orbital septum; this may be associated with chemosis and prolapse
of retroseptal fat into the eyelids (Fig. 3.7B).
○ Te a r i n s u f f i c i e n c y and instability is common.
○ C o r n e a l s i g n s are exacerbated by lid retraction and can include
punctate epithelial erosions, superior limbic keratoconjunctivitis, and
occasionally bacterial keratitis, thinning and scarring.
S o f t t i s s u e i n v o l v e m e n t
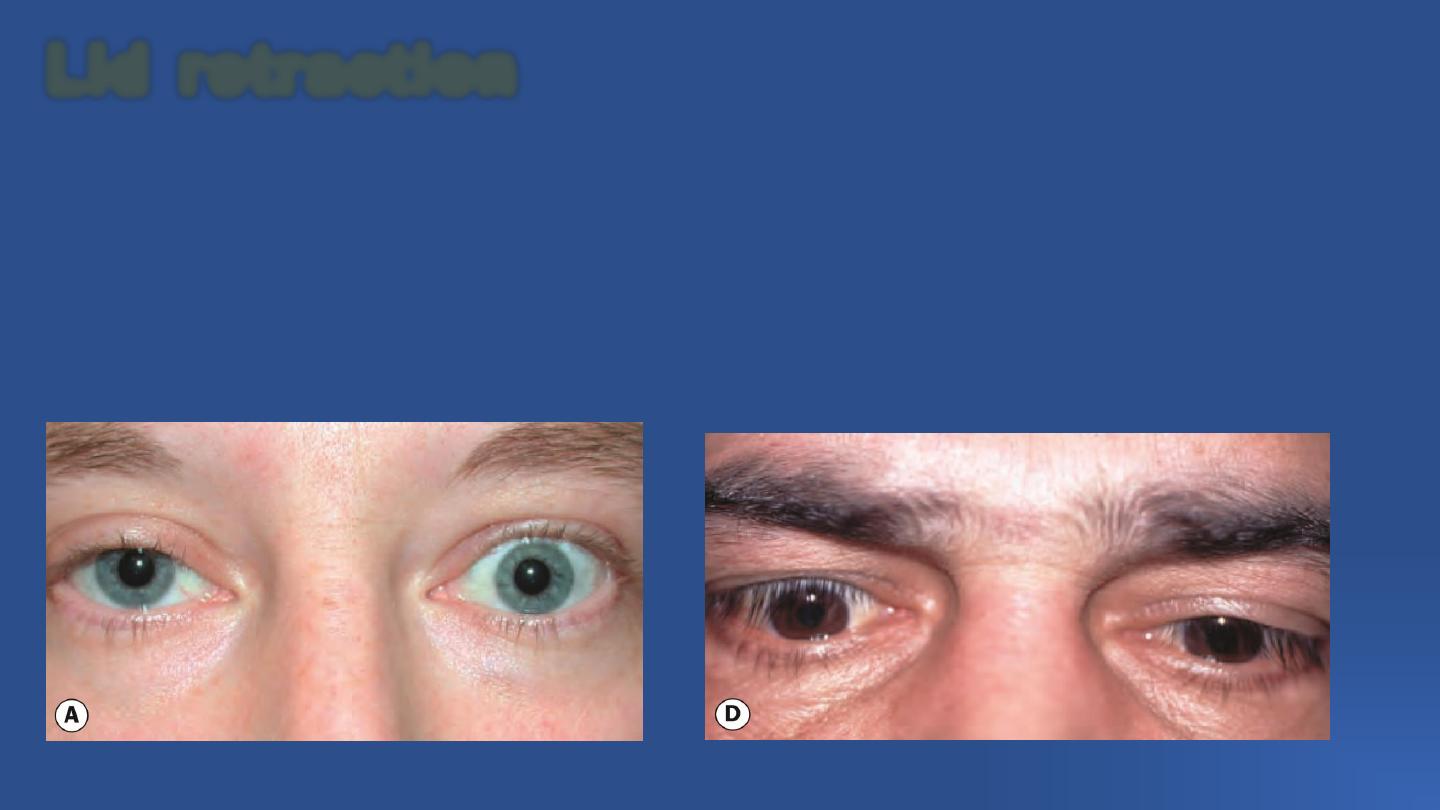
L i d r e t r a c t i o n
Retraction of upper and lower lids occurs in about 50% of patients with Graves disease.
Humorally induced overaction of Müller muscle is postulated to occur as a result of
sympathetic overstimulation secondary to high levels of thyroid hormones.
Fibrotic contracture of the levator palpebrae and inferior rectus muscles associated with
adhesion to overlying orbital tissues is another probable mechanism, together with
secondary overaction in response to hypo- or hypertropia produced by fibrosis.

• Symptoms.
Patients may complain of a staring or bulgingeyed appearance, difficulty closing the eyes
and ocular surface symptoms.
• Signs
○ The upper lid margin normally rests 2 mm below the limbus (Fig. 3.8A, right eye). Lid
retraction is suspected when the margin is either level with or above the superior limbus,
allowing sclera to be visible (‘scleral show’; Fig. 3.8A, left eye).
○ The lower eyelid margin normally rests at the inferior limbus; retraction is suspected
when sclera shows below the limbus. Lid retraction may occur in isolation or in
association with proptosis, which exaggerates its severity.
○ The Dalrymple sign is lid retraction in primary gaze (Fig. 3.8B).
○ The Kocher sign describes a staring and frightened appearance of the eyes which is
particularly marked on attentive fixation (Fig. 3.8C).
○ The von Graefe sign signifies retarded descent of the upper lid on downgaze (lid lag –
Fig. 3.8D).

• Symptoms
are similar to those
of lid retraction.
• Signs.
Proptosis is axial, unilateral
or bilateral, symmetrical or asymmetrical,
and frequently permanent.
Severe proptosis may compromise lid
closure and along with lid retraction and
tear dysfunction can lead to exposure
keratopathy, corneal ulceration and
infection.
P r o p t o s i s
Between
30%
and
50%
of
patients
with
TED
develop
ophthalmoplegia and this may be permanent. Ocular motility is
restricted initially by inflammatory oedema, and later by fibrosis.
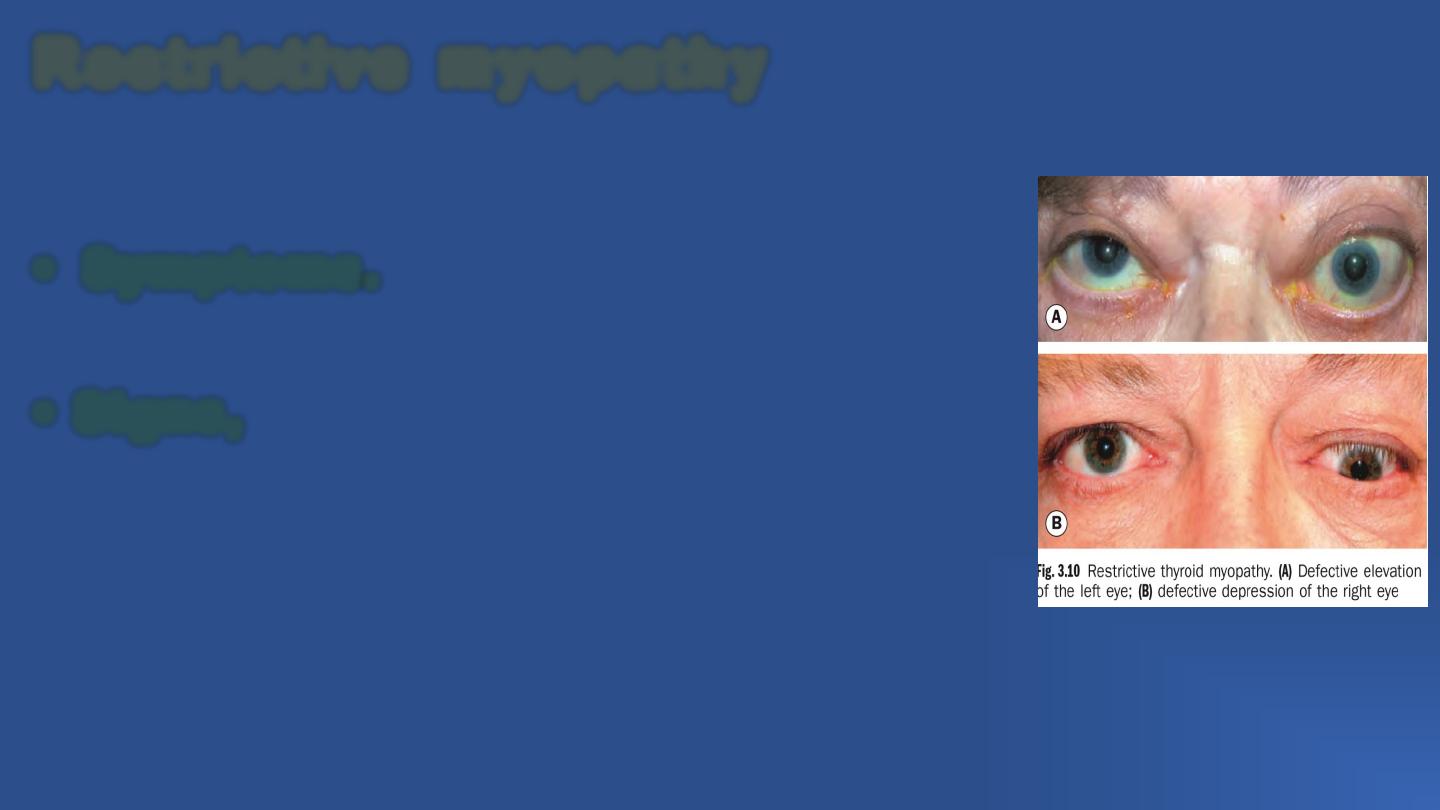
• Symptoms.
Double vision, and often discomfort in
some positions of gaze.
• Signs,
in approximate order of frequency:
○ Elevation defect (Fig. 3.10A) caused by fibrotic contracture of the
inferior rectus, may mimic superior rectus palsy and is the most
common motility deficit.
○ Abduction defect due to fibrosis of the medial rectus, which may
simulate sixth nerve palsy.
○ Depression defect (Fig. 3.10B) secondary to fibrosis of the
superior rectus.
○ Adduction defect caused by fibrosis of the lateral rectus.
R e s t r i c t i v e m y o p a t h y
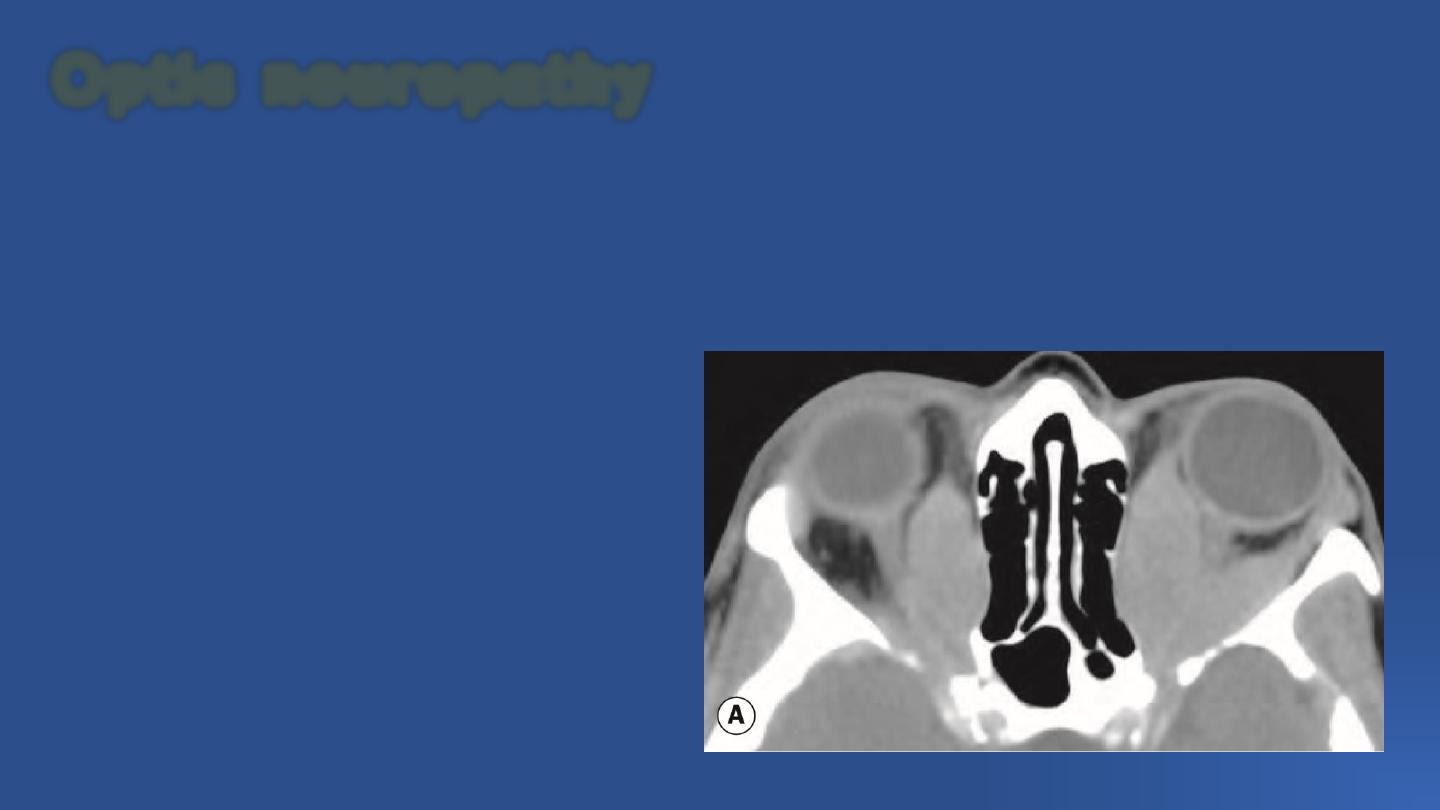
Optic neuropathy is a fairly common (up to 6%) serious complication caused by compression
of the optic nerve or its blood supply at the orbital apex by the congested and enlarged recti
(Fig. 3.11) and swollen orbital tissue. Such compression, which may occur in the absence of
significant proptosis, may lead to severe visual impairment if adequate and timely treatment
is not instituted.
O p t i c n e u r o p a t h y

• Symptoms.
Impairment of central vision occurs in conjunction with other
symptoms of TED. In order to detect early involvement, patients should be advised to
monitor their own visual function by alternately occluding each eye, reading small print and
assessing the intensity of colours, for example on a television screen.
• Signs.
A high index of suspicion should be maintained for optic neuropathy, and it is
important not to mistakenly attribute disproportionate visual loss to minor disease.
○ Visual acuity (VA) is usually reduced, but not invariably.
○ Colour desaturation is a sensitive feature.
○ There may be diminished light brightness appreciation.
○ A relative afferent pupillary defect, if present, should give cause for marked concern.
○ Visual field defects can be central or paracentral and may be combined with nerve fibre
bundle defects. These findings, in concert with elevated IOP, may be confused with primary
open-angle glaucoma.
○ The optic disc may be normal, swollen or, rarely, atrophic.

Investigations other than blood tests for thyroid disease are not necessary if the diagnosis
is evident clinically, but
the exclusion of other conditions
is sometimes indicated.
Vis u a l fie ld te s tin g
is carried out if there is a suspicion of optic nerve
compromise, and may be performed as part of a baseline evaluation even if there is no
apparent visual impairment.
MR I,
C T
and
U ltraso n o g rap h ic
imaging of the orbits are indicated in some
circumstances, such as helping to confirm an equivocal diagnosis by identification of the
typical pattern of extraocular muscle involvement in TED, consisting of muscle belly
enlargement with tendon sparing. Imaging is also used in the assessment of optic nerve
compression and prior to orbital wall surgery.
Visual evoked potentials are sometimes utilized in optic neuropathy.
I n v e s t i g a t i o n

Treatment can be classified into that of
Mild disease (most patients),
Moderate to severe active disease, and
Treatment of post inflammatory complications.
The first measure taken in all cases should be
The cessation of smoking.
Thyroid dysfunction should also be managed adequately; if radioiodine treatment is
administered in patients with pre-existing TED, a short course of oral steroids should be
given in concert.
• Mild disease
○ Lubricants for superior limbic keratoconjunctivitis, corneal exposure and dryness.
○ Topical anti-inflammatory agents (steroids, non-steroidal anti-inflammatory drugs
(NSAIDs), ciclosporin) are advocated by some authorities.
○ Head elevation with three pillows during sleep to reduce periorbital oedema.
○ Eyelid taping during sleep may alleviate mild exposure keratopathy.
T r e a t m e n t

• Moderate to severe active disease
○ Clinical activity score. EUGOGO suggests calculating a ‘clinical activity score’ to aid in
determining a threshold for the use of immunosuppressives, assigning one point for each
feature present from the following list and considering treatment for a score of 3 or more
out of 7.
1. Spontaneous orbital pain.
2. Gaze-evoked orbital pain.
3. Eyelid swelling considered to be due to active (inflammatory phase) TED.
4. Eyelid erythema.
5. Conjunctival redness considered to be due to active (inflammatory phase) TED.
6. Chemosis.
7. Inflammation of caruncle or plica.

During subsequent review, a point is allocated for an increase in proptosis of 2 mm or
more, a decrease in uniocular excursion in any one direction of 8° or more, or a decrease
in Snellen acuity of one line.
are the mainstay of treatment for moderate to severe
disease. Oral prednisolone 60–80 mg/ day may be given initially, and tapered depending
on response. Intravenous methylprednisolone is often reserved for acute compressive
optic neuropathy, but tolerability is better and outcomes may be superior compared with
oral treatment; a lower-intensity regimen in the absence of acute sight-threatening
disease is 0.5 g once weekly for 6 weeks followed by 0.25 g once weekly for 6 weeks. A
reduction in discomfort, chemosis and periorbital oedema usually occurs within 24 hours,
with a maximal response within 2–8 weeks. Ideally, oral steroid therapy should be
discontinued after several months, but long-term low-dose maintenance may be
necessary.
are occasionally used in selected cases to
minimize systemic side effects, but are typically considerably less effective than systemic
treatment.
may be used in addition to
steroids or when steroids are contraindicated or ineffective, but because of the delayed
effect is not used as the sole treatment of acute optic nerve compression. A positive
response is usually evident within 6 weeks, with maximal improvement by 4 months;
around 40% will not respond. Adverse effects include cataract, radiation retinopathy,
optic neuropathy and an increased risk of local cancer; the threshold for its use should
be higher in younger patients and diabetics, the latter because of a possibly increased
risk of retinopathy.
may be more effective than steroids or radiotherapy alone.
○ Optic neuropathy, and less commonly intractable corneal exposure, requires aggressive
treatment.
is commonly used,
regimens including 0.5–1 g on three successive days with conversion to oral treatment (e.g.
40 mg/day prednisolone) or 0.5–1 g on alternate days, 3–6 times, keeping the maximum
dose below 8 g to reduce the risk of liver compromise, followed by oral prednisolone;
appropriate monitoring should be instituted, including liver function tests, as well as gastric
protective treatment and osteoporosis prophylaxis if necessary.
may be considered if steroids are ineffective (20% receiving
intravenous treatment) or contraindicated. Orbital radiotherapy may also be administered,
but is generally only used as an adjunct to other modalities.
○ Several drugs targeting specific aspects of the immune response in TED are under
investigation, notably
noclonal antibody treatment with rituximab.

Eyelid surgery should be performed only after any necessary orbital and then strabismus
procedures have been undertaken, as orbital decompression may impact both ocular
motility and eyelid position, and extraocular muscle surgery may affect eyelid position.
After active inflammation has remitted, the patient can be left with
cosmetically and functionally significant proptosis, the treatment of which is essentially
surgical. Surgical decompression increases the volume of the orbit by removing the bony
walls and may be combined with removal of orbital fat. Most surgery is undertaken via an
external approach, though the medial wall and the medial part of the floor can be reached
endoscopically. One-wall (deep lateral) decompression is effective (approximately 4–5 mm
reduction in proptosis) and may reduce the risk of postoperative diplopia; two-wall
(balanced medial and lateral – Fig. 3.12) decompression provides a greater effect but with
a significant risk of inducing diplopia; three-wall decompression includes the floor with a
reduction in proptosis of 6–10 mm but may lead to hypoglobus and carries a higher risk of
infraorbital nerve damage and diplopia; very severe proptosis may require removal of part
of the orbital roof in addition (four-wall decompression).
P o s t - i n f l a m m a t o r y c o m p l i c a t i o n s .
Surgery is required in most cases experiencing
persistent diplopia in the primary or reading positions of gaze, provided the inflammatory
stage has subsided and the angle of deviation has been stable for at least 6–12 months.
Until these criteria are met, diplopia may be alleviated, if possible, with prisms or
sometimes botulinum toxin. The goal of operative treatment is to achieve binocular single
vision in the primary and reading positions; restrictive myopathy often precludes
binocularity in all positions of gaze, though with time the field of binocular single vision may
enlarge as a result of increasing fusional vergence. Recession of the inferior and/or medial
recti is the most commonly indicated surgery (a rectus muscle is never resected, only
recessed in TED), generally utilizing adjustable sutures (see Ch. 18). The suture is adjusted
later the same day or on the first postoperative day to achieve optimal alignment, and the
patient is encouraged subsequently to practise achieving single vision with a consistently
accessible target such as a television.

Mild lid retraction frequently improves spontaneously so does
not require treatment. Control of hyperthyroidism may also be beneficial. Botulinum
toxin injection to the levator aponeurosis and Müller muscle may be used as a
temporary measure in patients awaiting definitive correction. Müllerotomy
(disinsertion of Müller muscle) is effective for mild lid retraction, but more severe cases
may also require recession/disinsertion of the levator aponeurosis and the suspensory
ligament of the superior conjunctival fornix. Recession of the lower lid retractors, with
or without a hard palate graft, can be used when retraction of the lower lid is 2 mm or
more (see also Ch. 1).
Purulent inflammation of the cellular tissue of the orbit.
Causes of Orbital Cellulitis:
Spread of infection from neighboring structures like nasal
sinuses, eyelids, eyeball (like in case of panophthalmitis) facial
erysiplas etc
Also due to deep penetrating injuries (specially in cases of
retained Foreign body) and metastatic infection in cases of
pyaemia
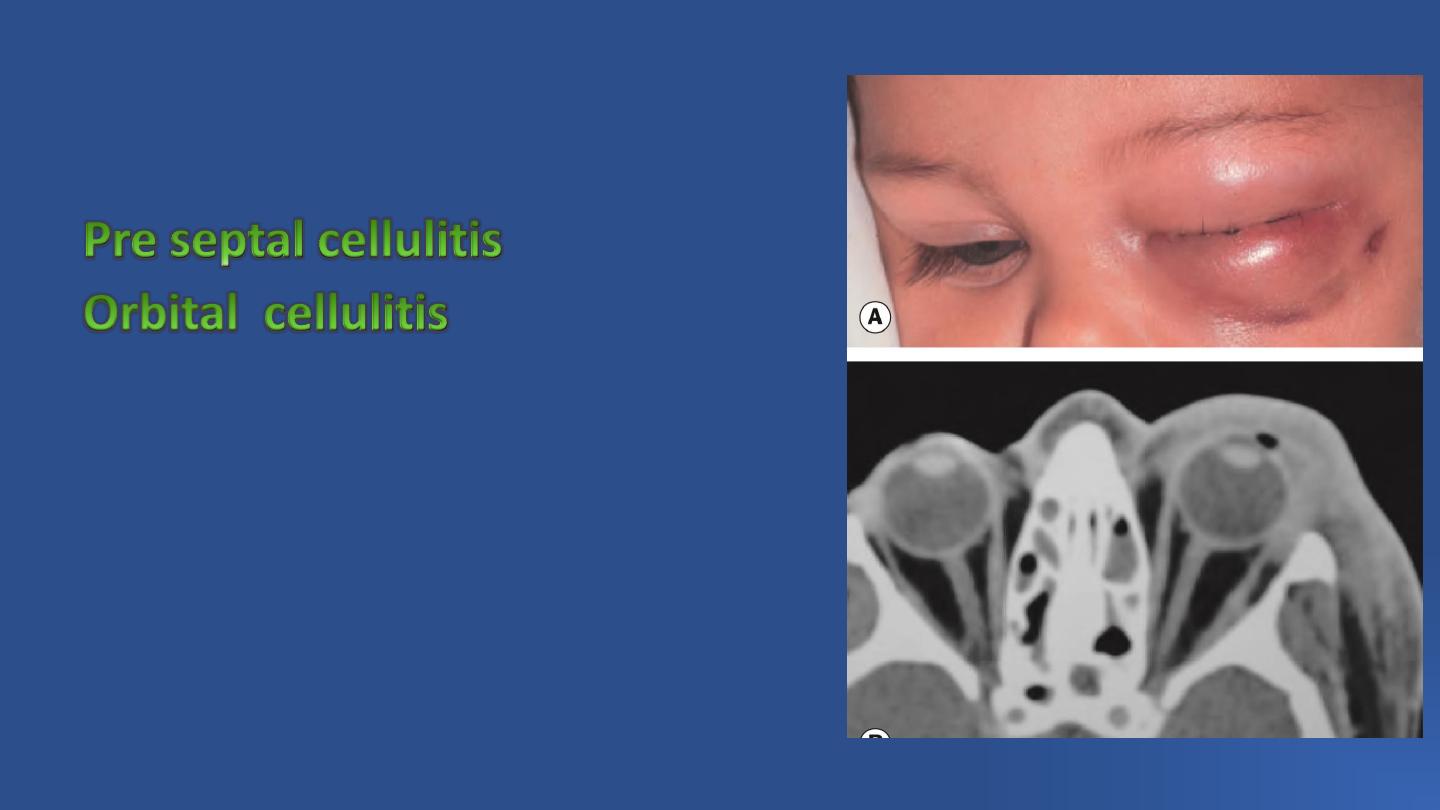
Types of Orbital Cellulitis
and
A-Pre septal –structures anterior to orbital
septum, characterized by erythema,
chemosis, conjunctival discharge without
restriction of ocular movements and visual
impairment
:
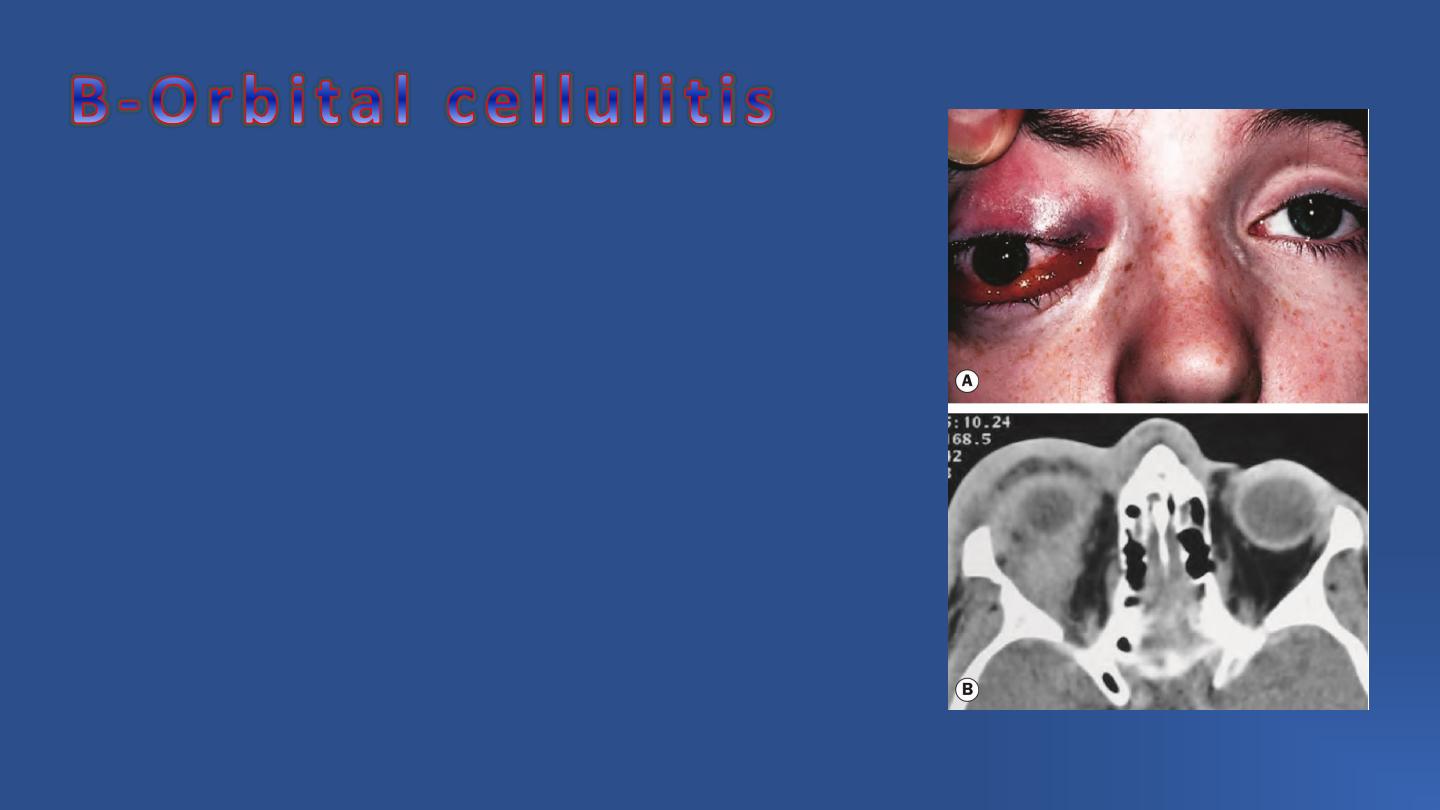
–
behind orbital septum, characterized
severe pain,
fever,
diminution of vision (due to retrobulbar
neuritis or compression of optic nerve and /or
its blood supply),
massive swelling of lids,
chemosis,
proptosis,
restriction of ocular movements.

Complications
-Panophthalmitis
-Extension into brain through meninges , cavernous
sinus thrombosis may develop
-In diabetic patients fungal superinfection may develop

Culture and sensitivity of pus, if present and of blood
Treatment –Broad spectrum Intravenous antibiotics ,
and anti inflammatory
If abscess has formed – Incision and Drainage under
cover of antibiotics
Management

Treatment
• Hospital admission is mandatory, with urgent otolaryngological assessment and frequent
ophthalmic review. Paediatric specialist advice should be sought in the management of a
child, and a low threshold should be adopted for infectious disease specialist consultation.
• Delineation of the extent of erythema on the skin using a surgical marker may help in
judging progress.
• Antibiotics are given intravenously, with the specific drug depending on local sensitivities;
ceftazidime is a typical choice, supplemented by oral metronidazole to cover anaerobes.
Intravenous antibiotics should be continued until the patient has been apyrexial for 4 days,
followed by 1–3 weeks of oral treatment. • Monitoring of optic nerve function is performed
at least every 4 hours initially by testing VA, colour vision, light brightness appreciation and
pupillary reactions. Deterioration should prompt the consideration of surgical intervention.
• Surgery. Drainage of an orbital abscess should be considered at an early stage; drainage of
infected sinuses should be considered if there is a lack of response to antibiotics, or if there is
very severe sinus disease. Biopsy of inflammatory tissue may be performed for an atypical
clinical
picture.
Severe
optic
nerve
compression
may
warrant
an
emergency
canthotomy/cantholysis.

Cavernous sinus
thrombosis
Due to extension of
thrombosis from various
feeding vessels.
Source of infection
-Orbital veins - as in cases of septic lesion of
face, orbital cellulitis , infective condition of
face, mouth, nose, sinuses
-Furuncle of upper lip – dangerous area of face
-Metastatic infection or septic condition

Symptoms and Signs
Patient may present with symptoms and signs of Orbital cellulitis,
there is sever supra-orbital pain
Systemic features
– headache, fever ,altered sensorium, vomiting
and cerebral symptoms
Transference of symptoms and signs to other eye (bilateral orbital
cellulitis with which it may be confused is very rare clinical condition).
Mastoid edema and tenderness is present.

Emergency
Broad spectrum Intra Venous antibiotics
Anti coagulants
Neurophysicians to be consulted

Proptosis in children
1.Dermoid and epidermoid cyst
2.Capillary haemangioma
3.Optic nerve glioma
4.Rhabdomyosarcoma
5.Leukaemias
6.Metastatic neuroblastoma
7.Plexiform neurofibromatosis
8.Lymphomas

1. Graves disease.
2. Metastases – (of malignancy) from breast, lung, GIT.
3.Cavernous haemangiomas
4.Mucocele
5.Lymphoid tumors
6.Meningiomas

Types of Proptosis
- eye is pushed directly forwards – lesions situated in
optic nerve and central space
situated elsewhere in orbit pushes eye in opposite direction
as seen usually in congenital causes
– fast- as in cases of Rhabdomyosarcoma,
neuroblastoma, haemopoetic
as in cases of meningiomas
as in cases of carotid cavernous fistula
as in cases of orbital varicosity
