EXTERNAL EAR DISEASES
BY DR. AMMAR MOHAMMED 2019
NON INFLAMMATORY
A-CONGENTIAL MALFORMMATION
1:MICROTIA
2: ANOTIA
3:ACESSORY AURICLE
4: PREAURICULAR SINUS
5:ATRESIA
6: Prominent ears
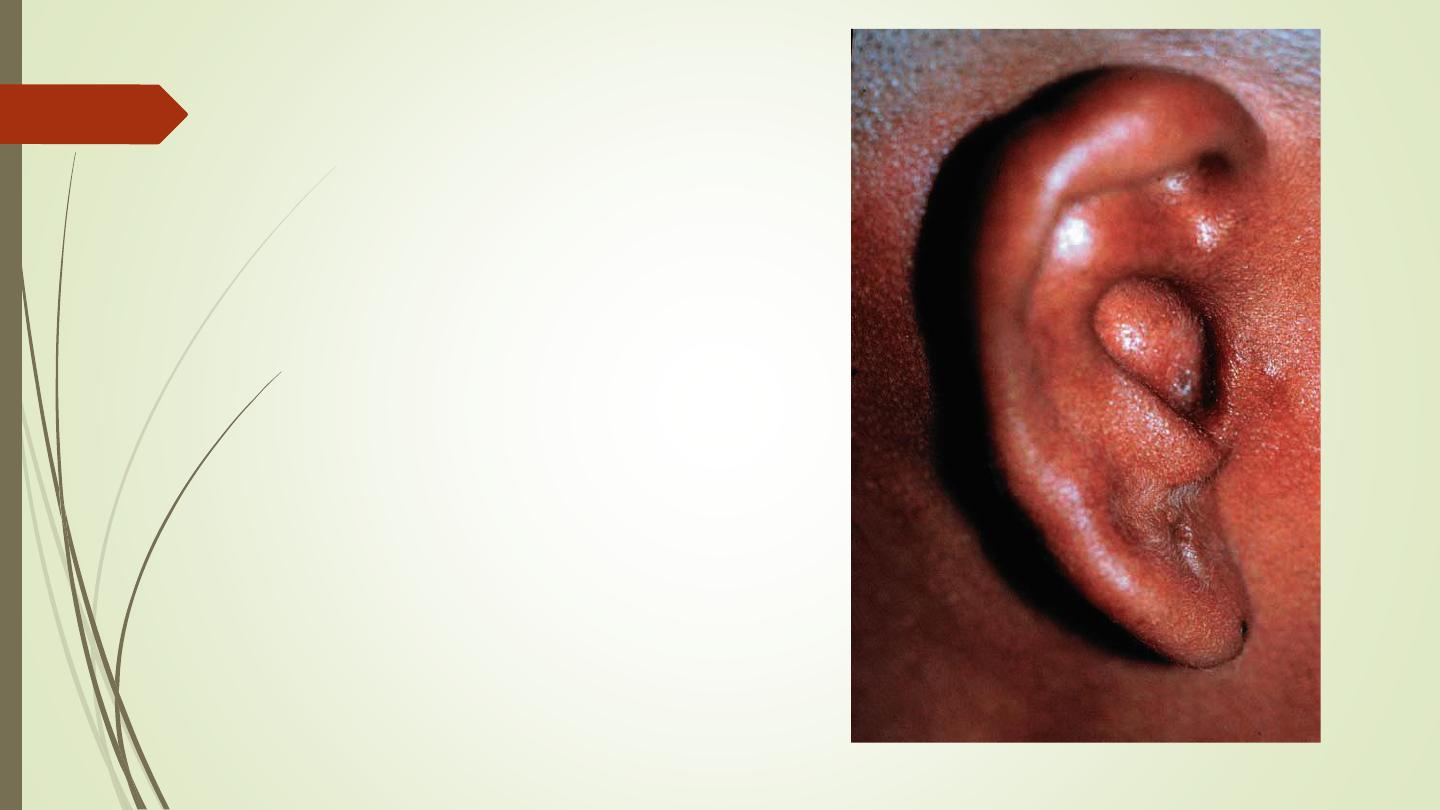
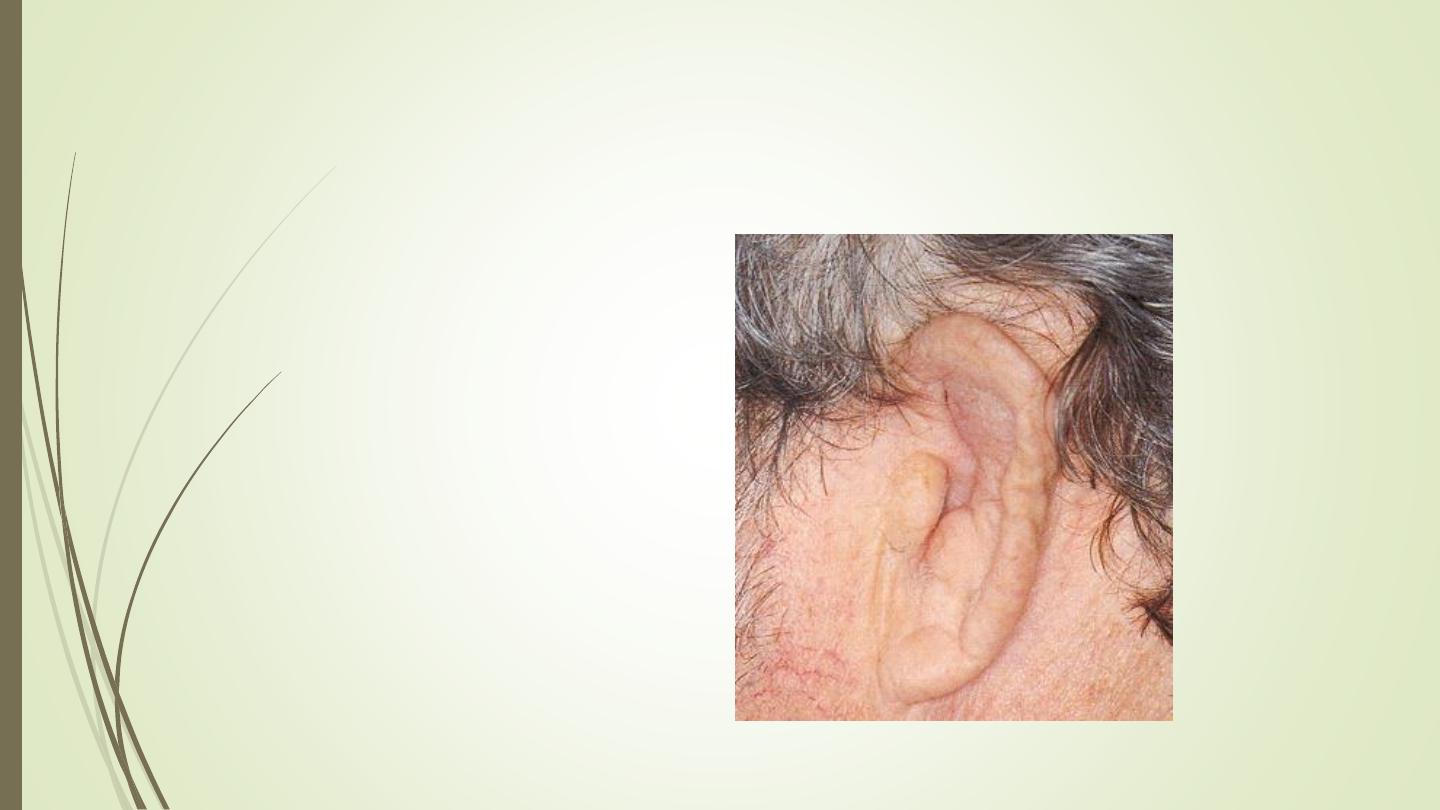
Microtia
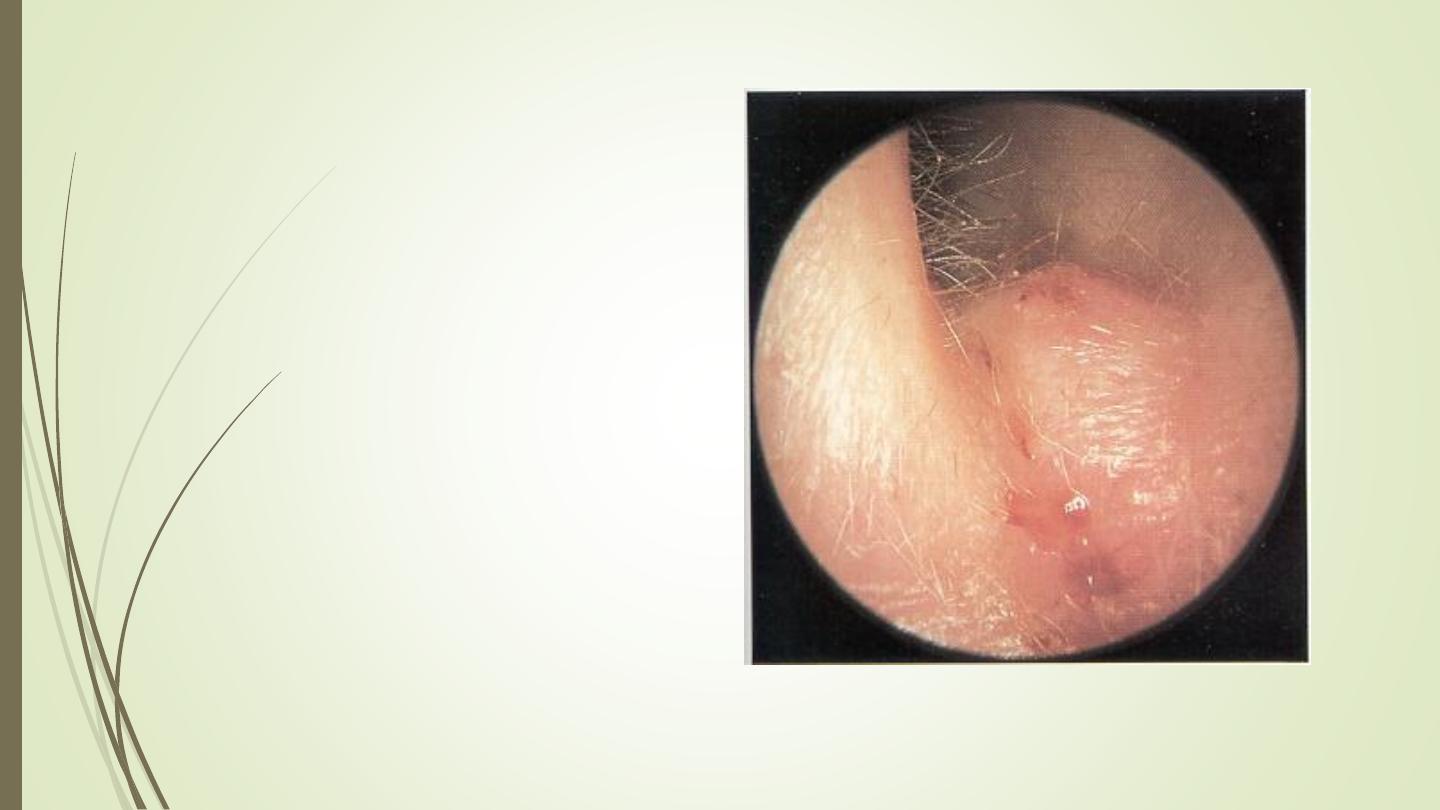
. This picture shows
microtia of the external ear.
This
congenital
anomaly
results
from
improper
development of first and
second branchial arches.
There is a small preauricular
skin tag present also.
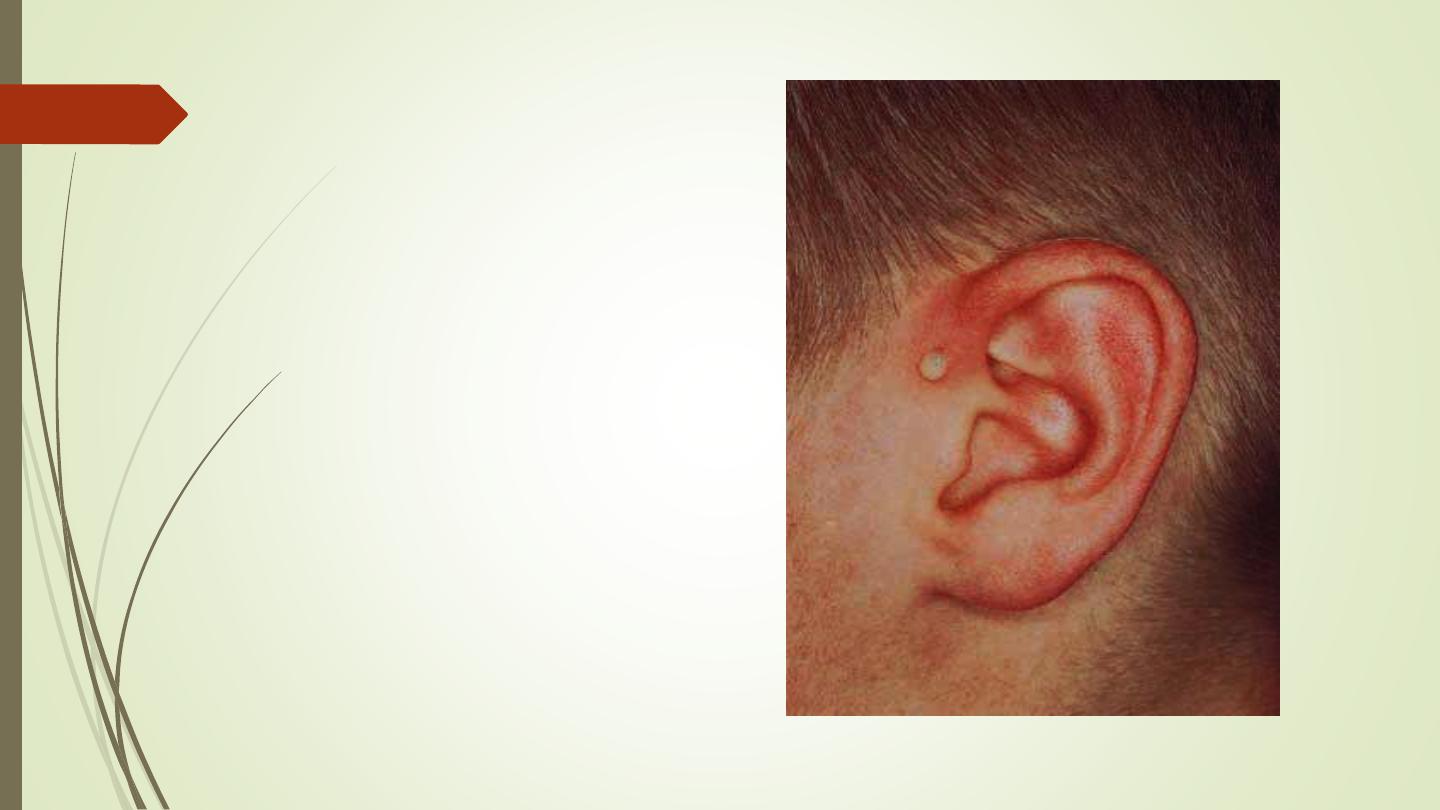
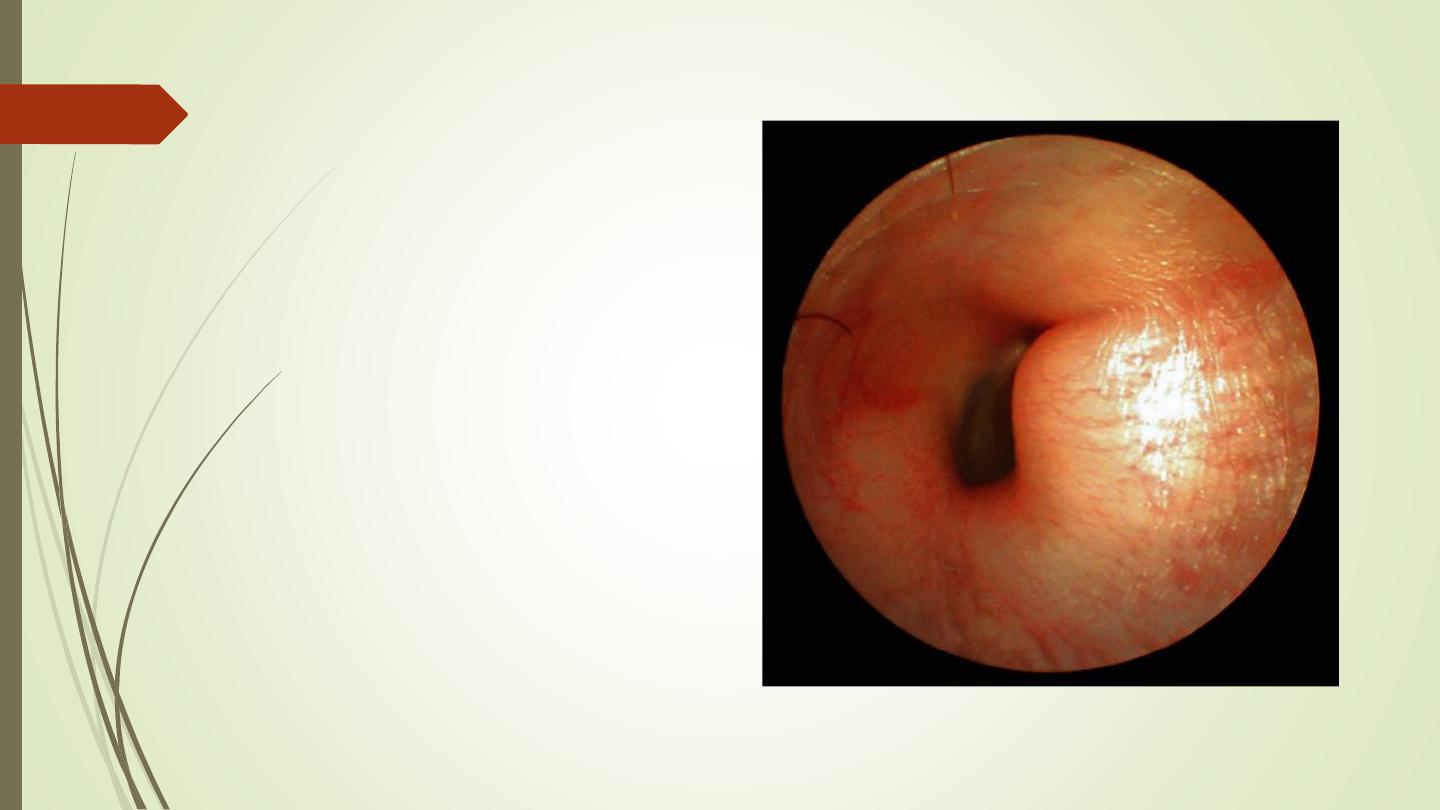
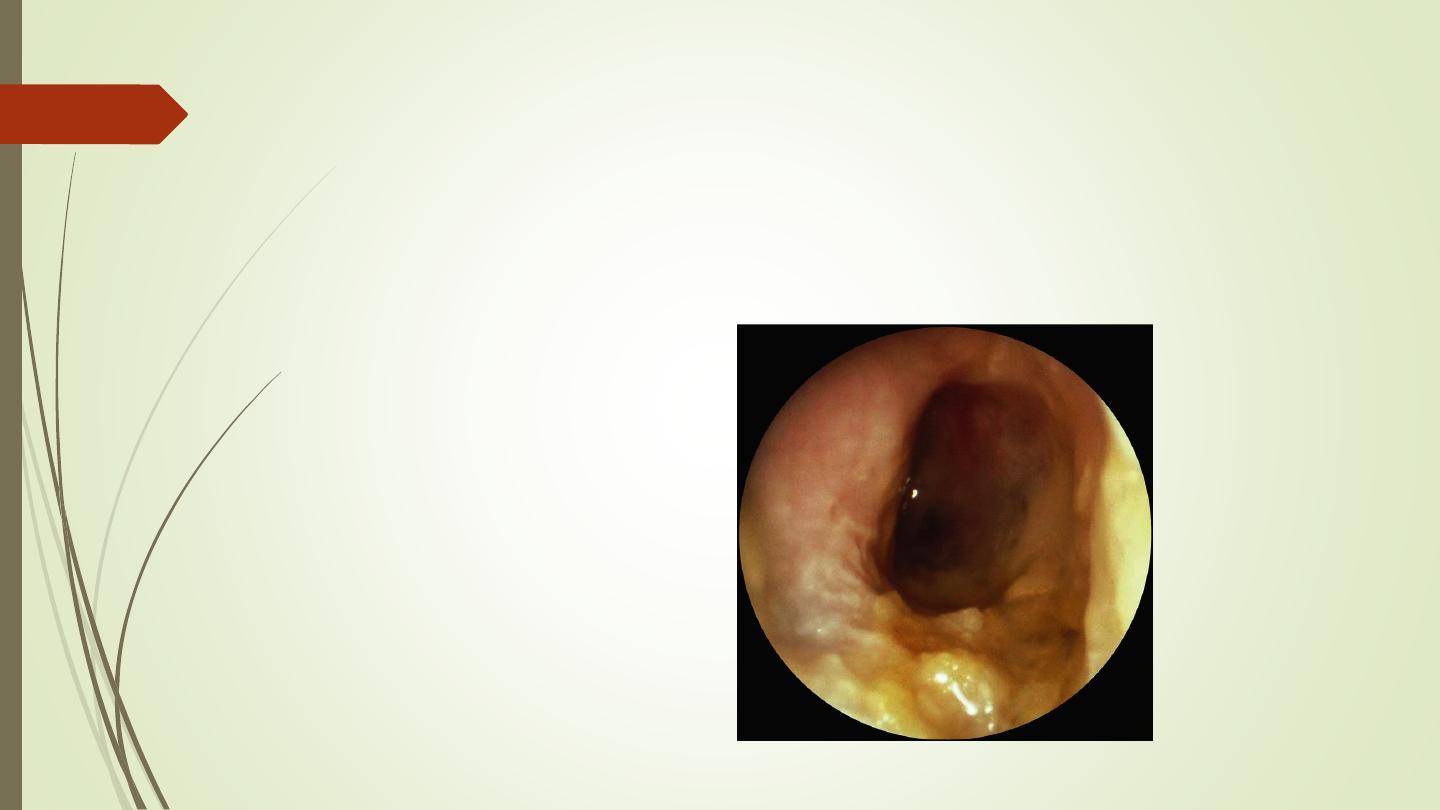
Atresia
of the external auditory
canal. This picture shows a
normal pinna with atresia
of the external ear canal.a
conductive hearing loss would
be anticipated
because of the occluded ear
canal
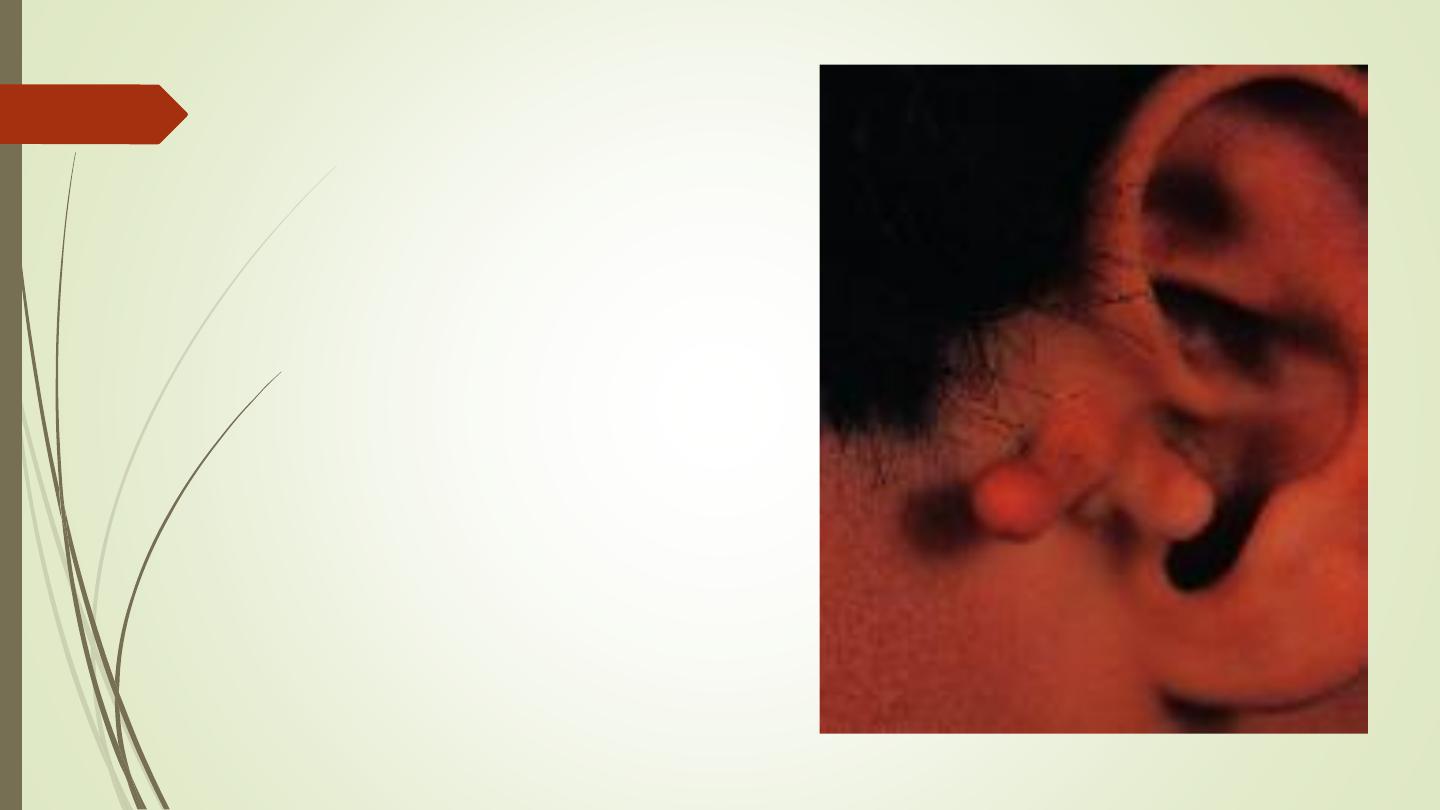
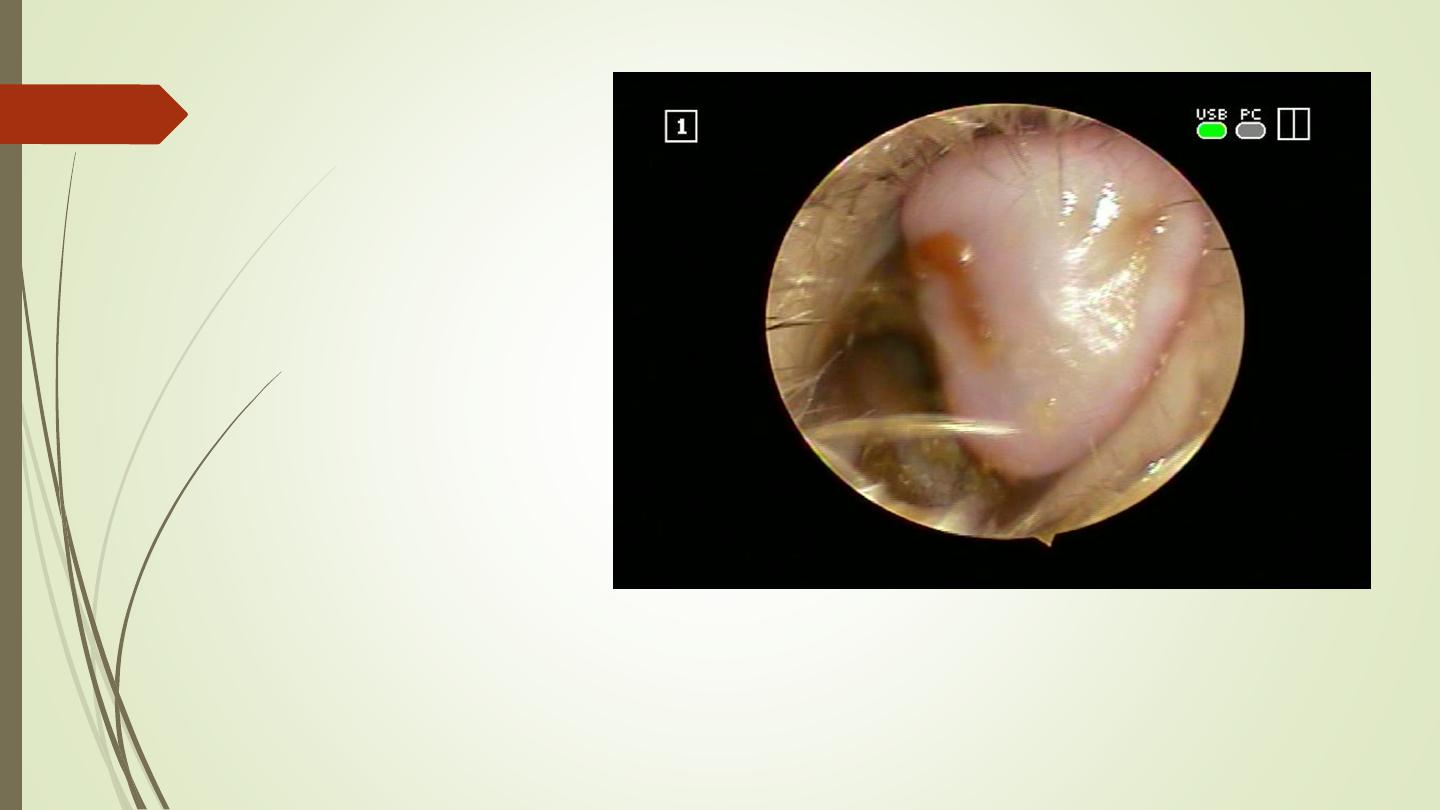
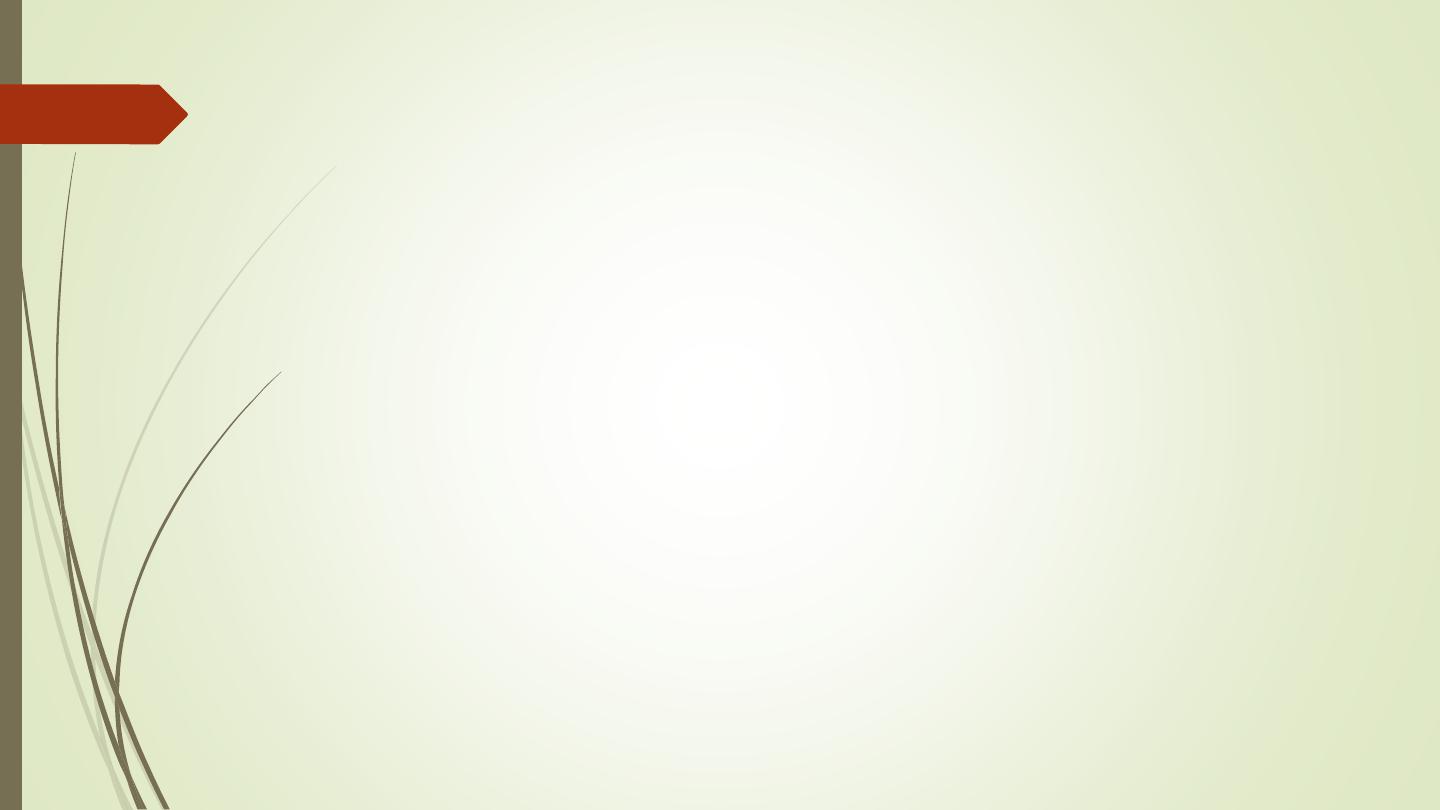
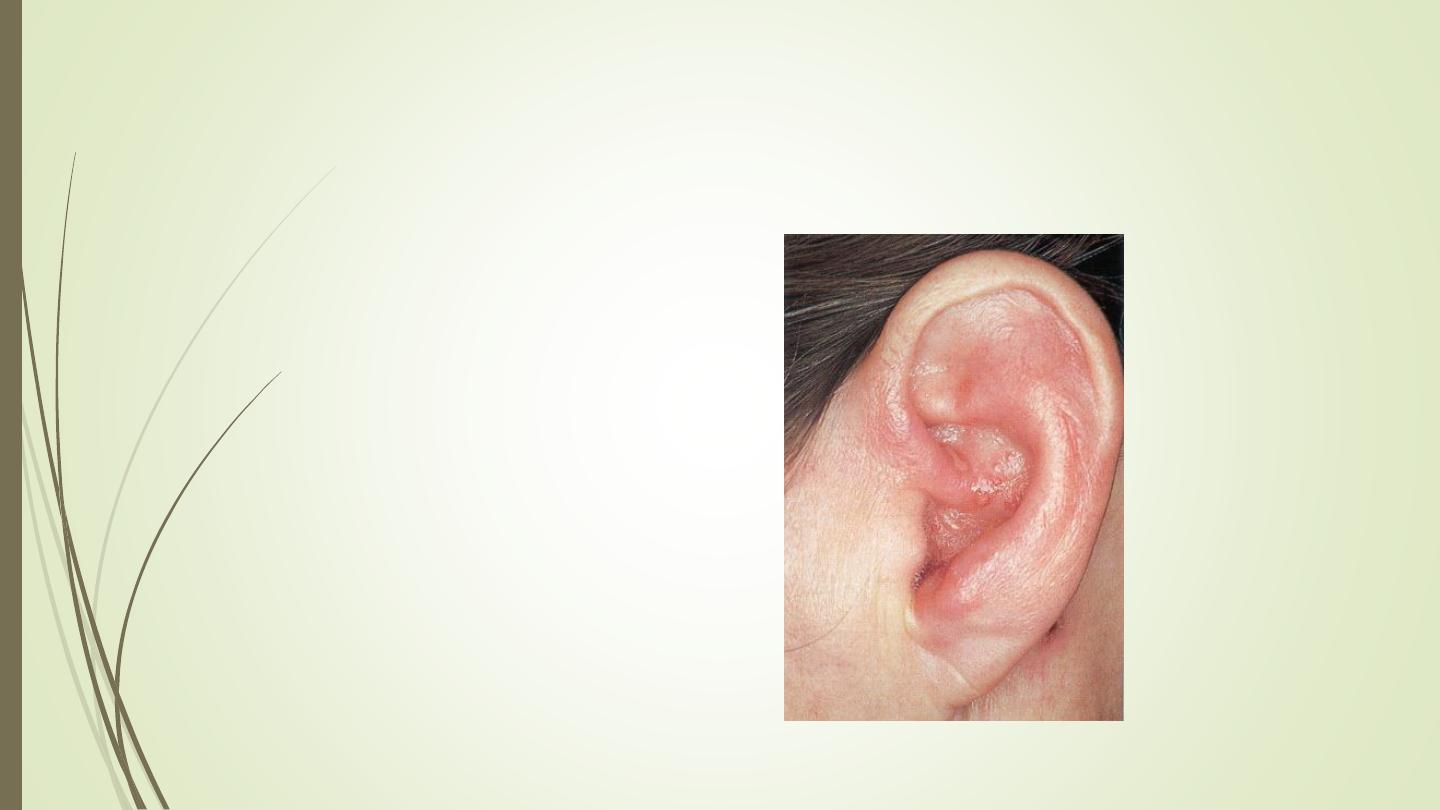
the preauricular cyst and/or
sinus tract
>>>a small fistula in
the skin anterior to the helix at
the upper tragus. A number of
people have only a punctum
here as an embryonic remnant
with no clinical problems.
If infected like this picture so
need>>> antibiotics.
If recurrent infection ocure >>>
surgical removal
Accessory lobules
These are commonly found anterior
to the tragus, and are
excised
for
cosmetic reasons
. A small nodule
of cartilage may be found
underlying these skin

Prominent ears.
the antihelix is either absent or
poorly formed
Treatment >>>pinnaplasty
B- hyperplastic
1:Exostoses
2; Osteoma
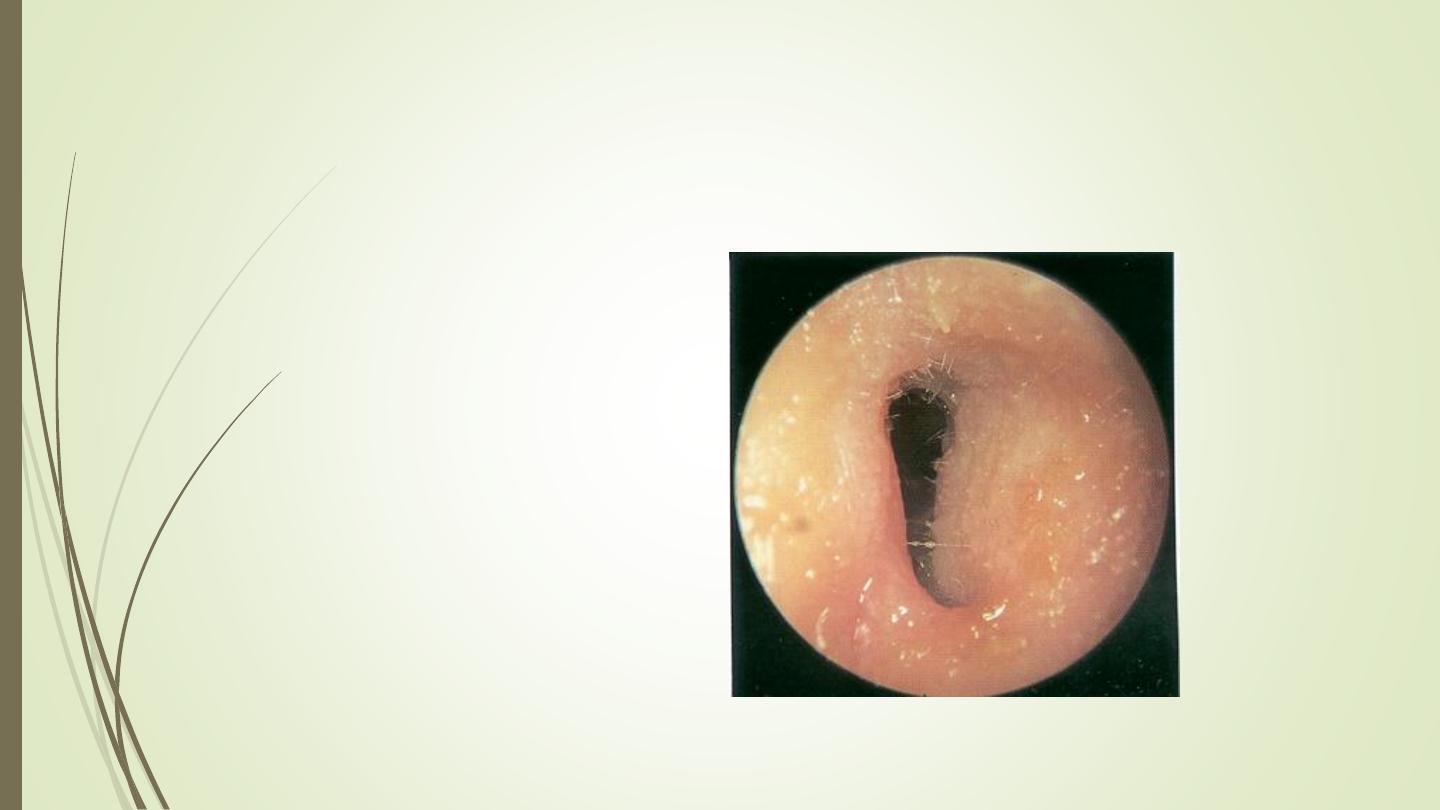
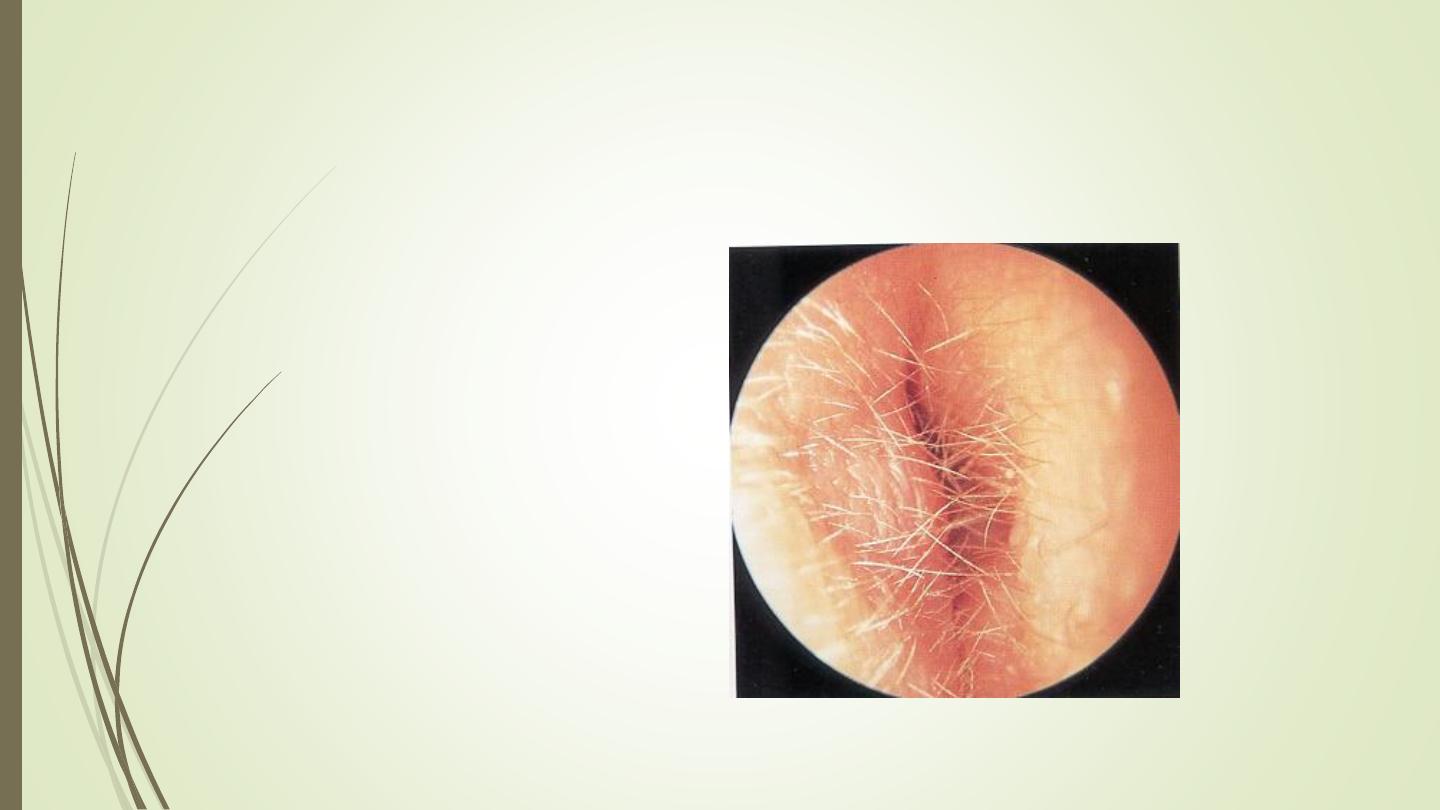
Exostosis
>>>Lamellar thickening of bone
of external ear canal
associated with cold water
exposure, generally seen in
swimmers
>>>They are bony, hard, and
usually remain small and
symptom free.
>>>They do not require any
treatment unless they cause
canal stenosis, cerumen
impaction, or limited exposure
of the tympanic membrane .
>>>Treatment by surgery
Osteoma
Pedunculated bone
mass developing along
suture lines,
tympanosquamous,
tympanomastoid.,
Occluding osteoma may
require surgical removal.
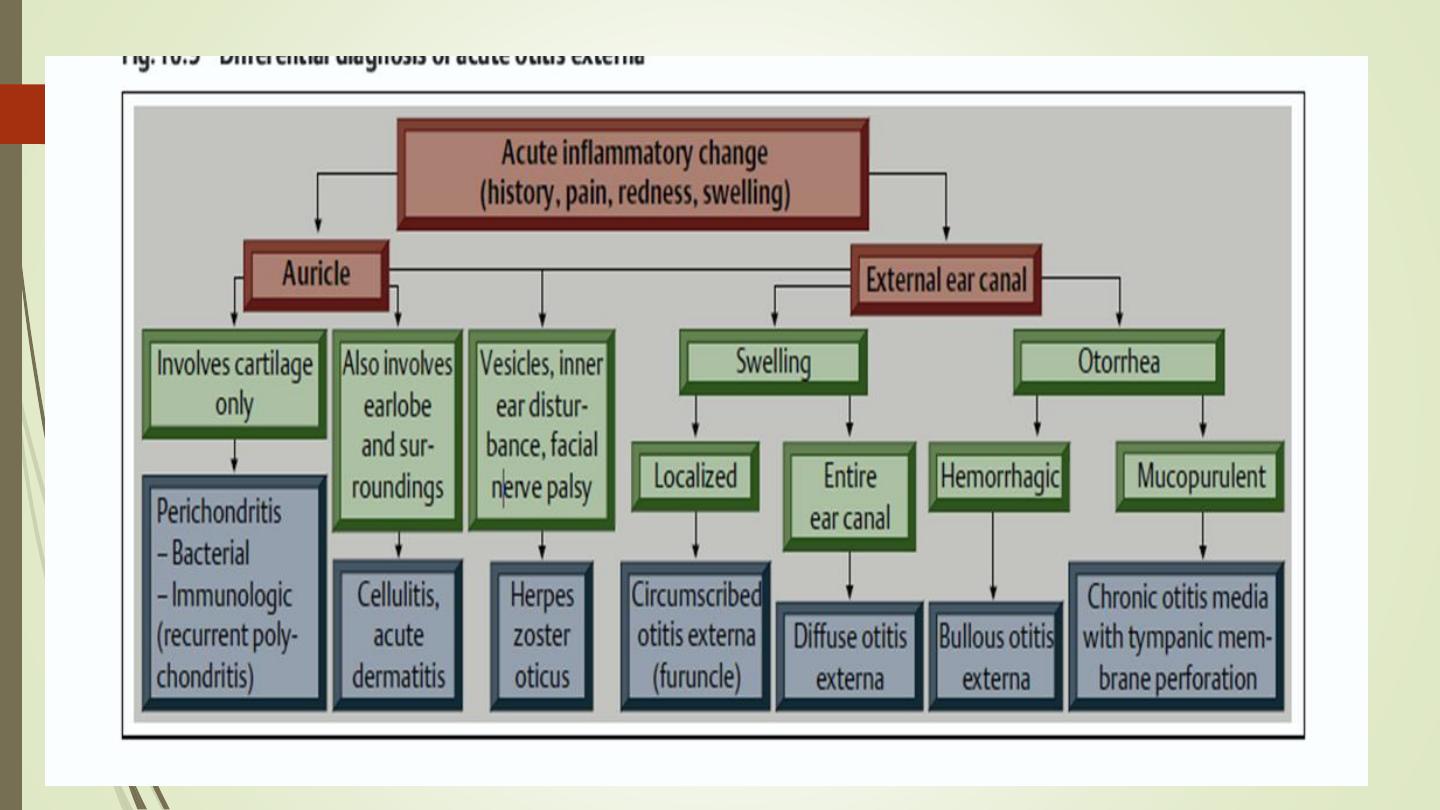
1- Acute localized otitis externa ((Furunculosis))
2-Acute diffused otitis externa
3- Otomycosis
4- External canal seborrheic dermatitis.
5- Perichondritis of the auricle
6- Malignant otitis externa
Inflammatory diseases of external ear
1- Acute localized otitis externa ((Furunculosis))
Acute localized infection
Lateral 1/3 of posterosuperior canal
Obstructed apopilosebaceous unit or glands
Pathogen: S. aureus
Symptoms
>>Localized pain
>>Pruritus
>>Hearing loss (if lesion occludes canal)
Furunculosis: Signs
Edema
Erythema
Tenderness
Occasional fluctuance
Furunculosis: Treatment
Local heat
Analgesics
Oral anti-staphylococcal antibiotics
Incision and drainage reserved for localized abscess
IV antibiotics for soft tissue extension
Acute Otitis Externa (AOE)
The most common infection occurs in humid climates, especially common
in the swimmers (swimmer’s ear, or tropical ear).
Precipitating factors:
Excessive sweating.
Absence of cerumen.
Narrow canal.
Alkaline pH.
Hearing aids
AOE: Mild to Moderate Stage
Progressive infection
Symptoms
Pain
Increased pruritus
Signs
Erythema
Increasing edema
Canal debris, discharge of
seropurulant material
AOE: Severe Stage
Severe pain, worse with
ear movement
Signs
Lumen obliteration
Purulent otorrhea
Involvement of periauricular
soft tissue
AOE: Treatment
Most common pathogens: P. aeruginosa and proteus
1- Frequent canal cleaning, a wick with a moderate amount of antibiotic or
antimycotic cream with steroid is inserted and left for 1–2 days. After the
oedema has been reduced, topical drying agents such as iodopovidone
should be applied.
2- Topical antibiotics
3-Pain control
4- Oral antibiotics are indicated only in cases of severe external otitis with
cellulitis or lymphadenitis, and always in diabetic patients.

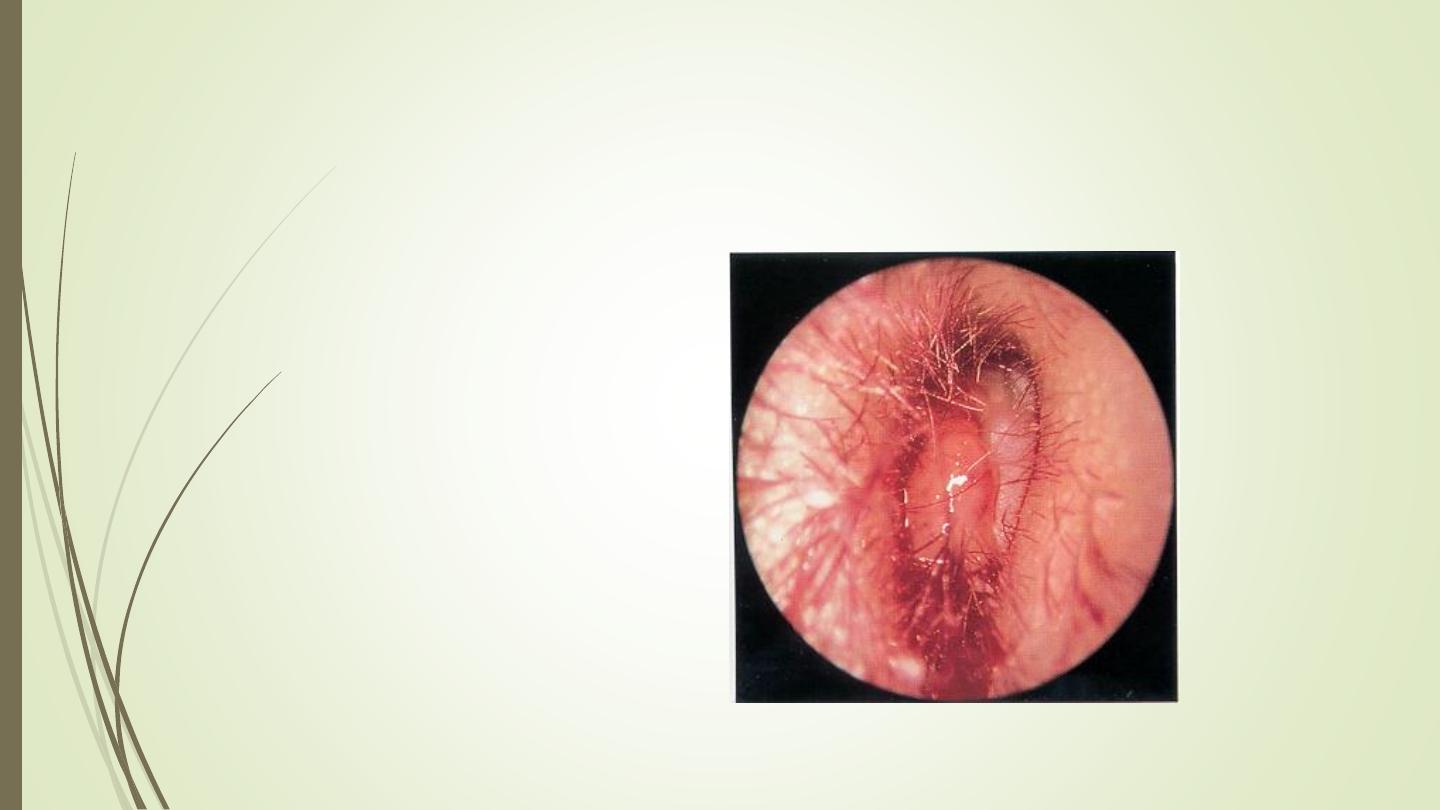
Otomycosis
Fungal infection of EAC skin
Primary or secondary
Most common organisms: Aspergillus and Candida
Otomycosis: Symptoms
Often indistinguishable from bacterial OE
Pruritus deep within the ear
Dull pain
Hearing loss (obstructive)
Tinnitus
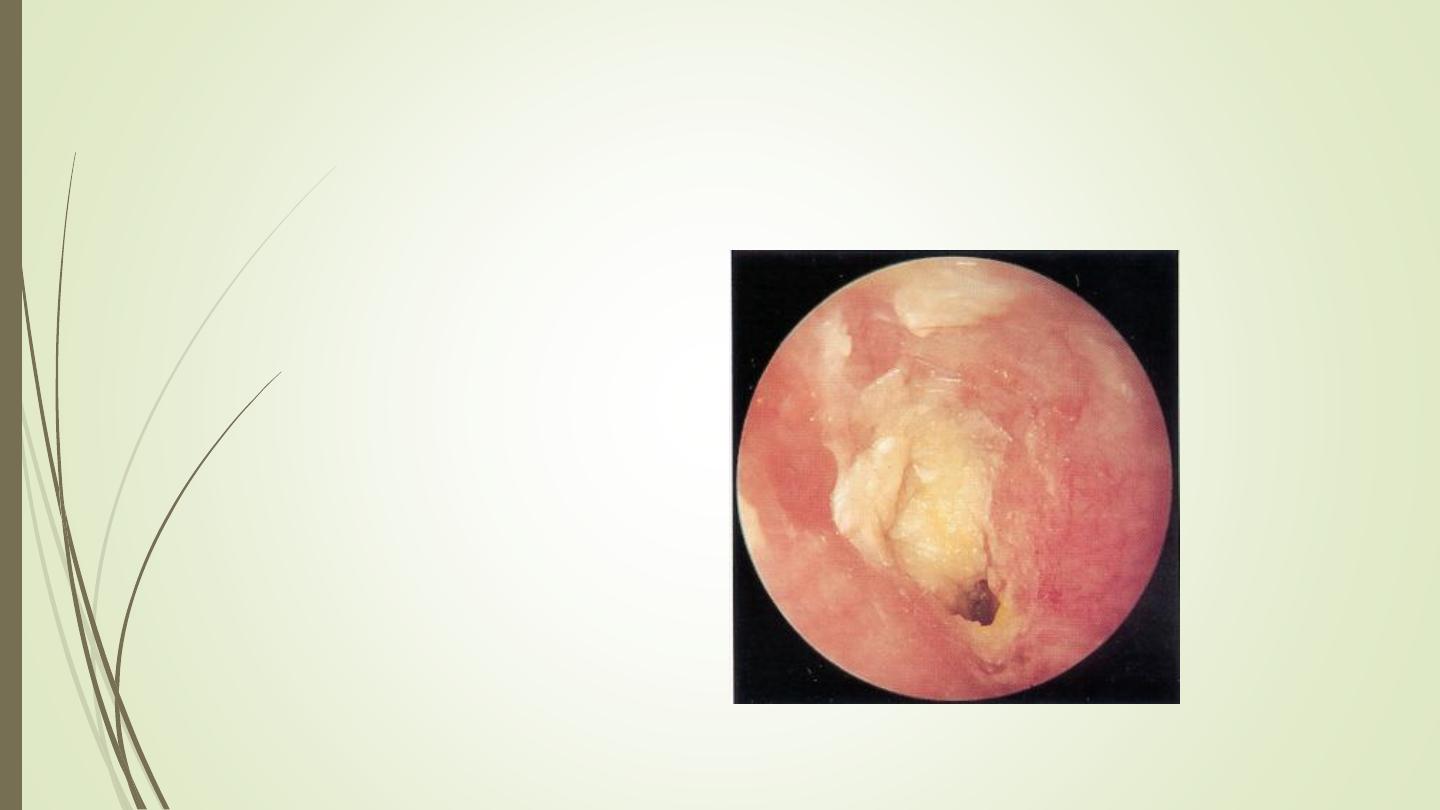
Otomycosis: Signs
Canal erythema
Mild edema
White, gray or black
fungal debris
Otomycosis: Treatment
Thorough cleaning and drying of canal
Treatment:
Avoid risk factors.
Keratolytic agents (2% salicylic acid in alcohol).
Fungicidal (nystatin, clotrimoxazole, gention violet)
Necrotizing External Otitis(NEO)
***Malignant OE***
Malignant because of the high mortality rate if the disease spreads outside
EAM.
Typically seen in diabetics and immunocompromised patients
Pseudomonas aeruginosa is the usual cause
NEO: Symptoms
Poorly controlled diabetic with h/o OE
Deep-seated aural pain
Chronic otorrhea
Aural fullness
NEO: Signs
Inflammation and
granulation
Purulent secretions
Occluded canal and
obscured TM
Cranial nerve involvement
NEO: Treatment
Intravenous antibiotics for at least 4 weeks – with serial gallium scans
monthly
Local canal debridement until healed
Pain control
Use of topical agents controversial
Hyperbaric oxygen experimental
Surgical debridement for refractory cases
NEO: Mortality
Death rate essentially unchanged despite newer antibiotics (37% to 23%)
Higher with multiple cranial neuropathies (60%)
Recurrence not uncommon (9% to 27%)
May recur up to 12 months after treatment
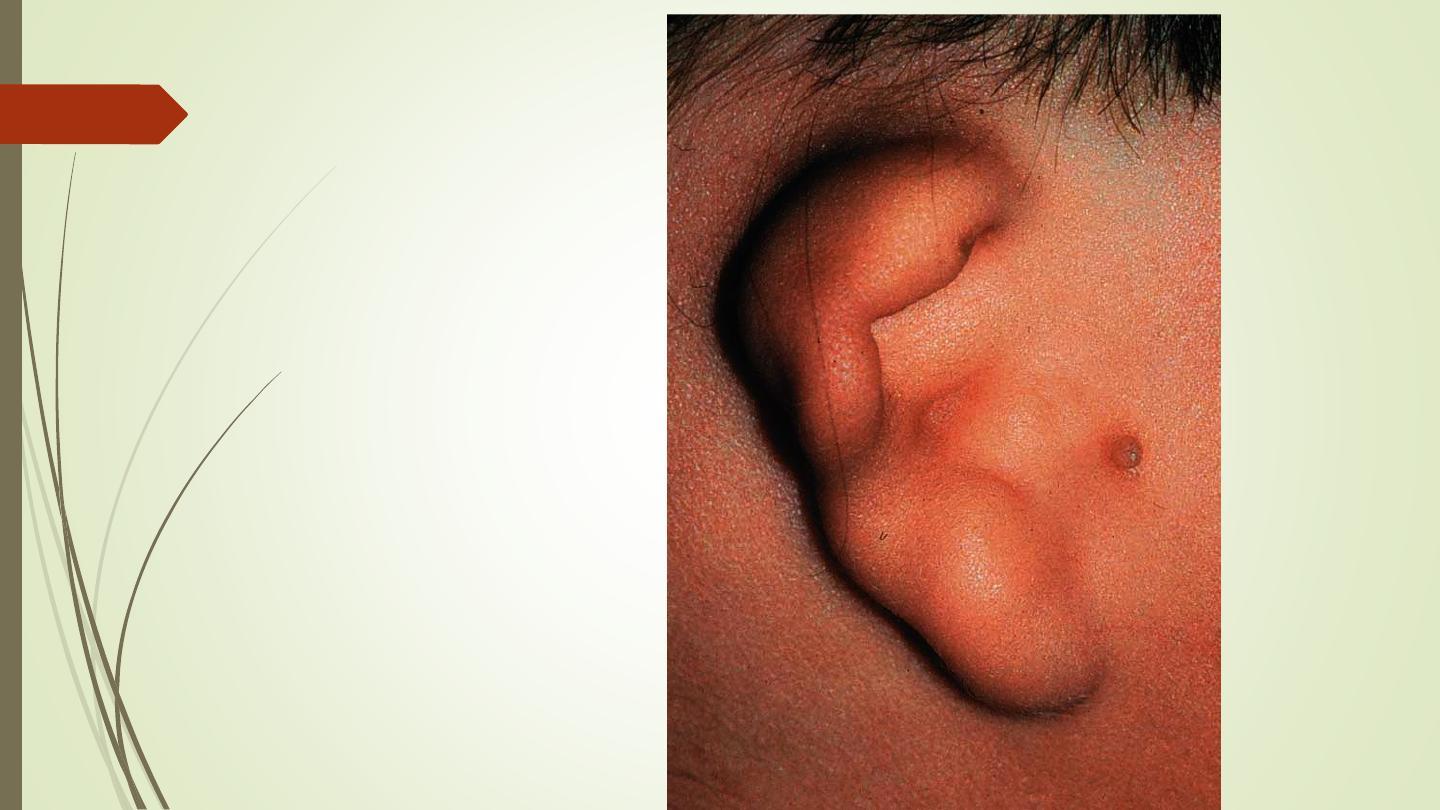
Perichondritis/Chondritis
Infection of perichondrium/cartilage
Result of trauma to auricle
May be spontaneous (in diabetics)
Symptoms
• Pain over auricle and deep in canal
• Pruritus
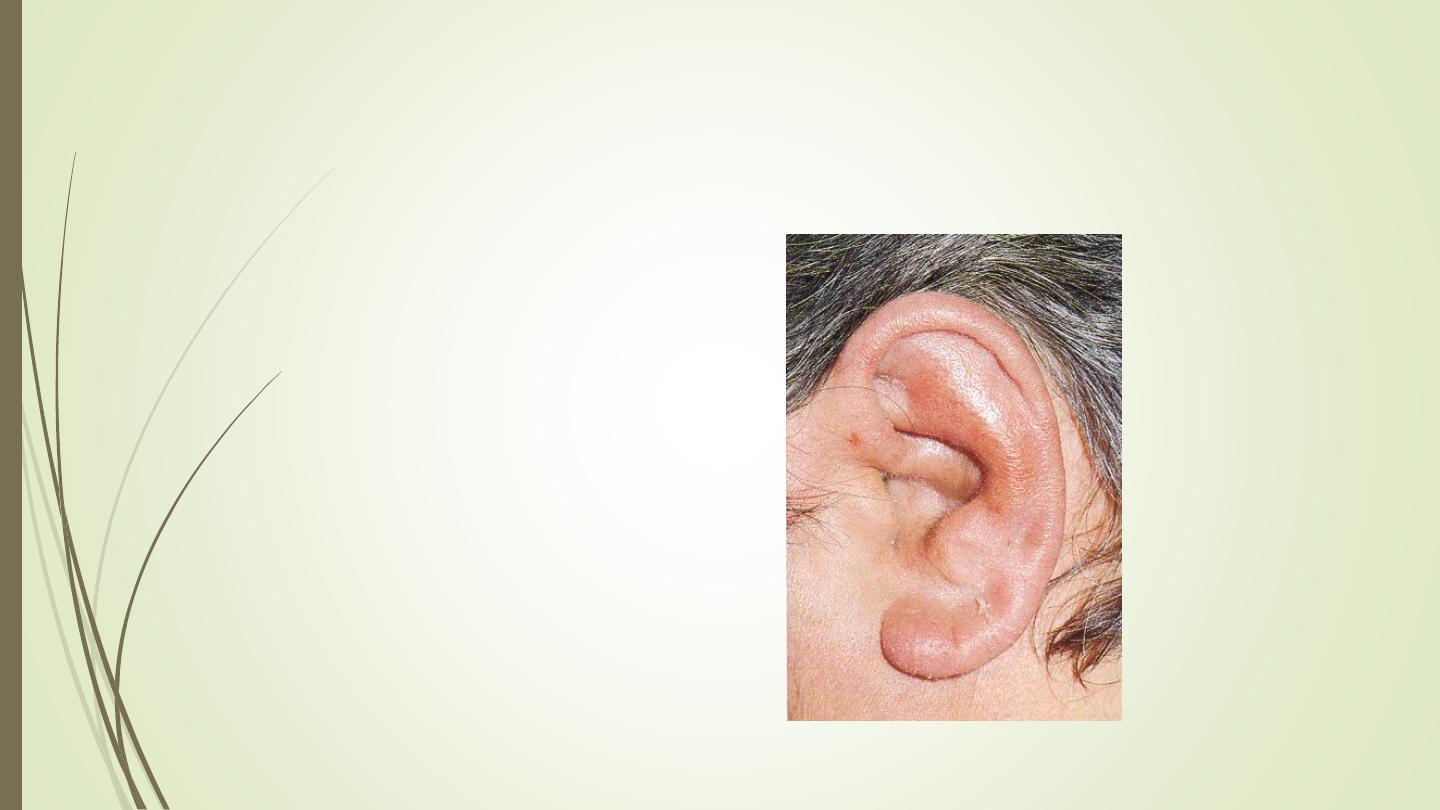
Perichondritis: Signs
Tender auricle
Induration
Edema
Advanced cases
Crusting & weeping
Involvement of soft tissues
Relapsing Polychondritis
Episodic and progressive inflammation of cartilages
Autoimmune etiology?
External ear, larynx, trachea, bronchi, and nose may be involved
Involvement of larynx and trachea causes increasing respiratory obstruction
Relapsing Polychondritis
Fever, pain
Swelling, erythema
Anemia, elevated ESR
Treat with oral
corticosteroids
Herpes Zoster Oticus
J. Ramsay Hunt described in 1907
Viral infection caused by varicella zoster
Infection along one or more cranial nerve dermatomes (shingles)
Ramsey Hunt syndrome: herpes zoster of the pinna with otalgia and facial
paralysis
Herpes Zoster Oticus: Symptoms
Early: burning pain in one
ear, headache, malaise
and fever
Late (3 to 7 days):
vesicles, facial paralysis
Herpes Zoster Oticus: Treatment
Corneal protection
Analgesics
Antivirals -Oral acyclovir_800mg x5 per day.