Biological and Biomechanical Aspects of Tooth Movement
Tooth movements can be divided into three types:
• Physiologic.
• Pathologic (Pathologic migration).
• Orthodontic.
The term physiologic tooth movement means primarily the slight tipping of the
functioning tooth in its socket and secondarily, the changes in tooth position that
occur in young persons during and after tooth eruption.
The minor changes in tooth position observed in growing persons and adults are
usually called tooth migration. These are generally associated with periodontal
breakdown or/and altered force levels in the dental arches.
Orthodontic teeth movement is based on the observation that if prolonged light
pressure is applied to a tooth, tooth movement will occur as the bone around the
tooth remodels. Bone is selectively removed in some areas and added in others. In
essence, the tooth moves through the bone carrying its attachment apparatus with
it, as the socket of the tooth migrates. Because the bony response is mediated by
the periodontal ligament (PDL), tooth movement is primarily a PDL phenomenon.
Theories of orthodontic tooth movement
1- Pressure tension theory.
2- Piezoelectric theory.
3- Hydrodynamic theory(blood flow theory).

Pressure tension theory: This is the simplest and the most widely
accepted, according to this theory, Whenever a tooth is subjected to an orthodontic
force, it results in areas of pressure and tension in PDL. The alveolar bone is
resorbed whenever the root causes compression of the periodontal ligament, i.e.
the pressure side. New alveolar bone is deposited whenever there is a stretching
force acting on the periodontal ligament fibers, i.e. the tension side.
Hydrodynamic theory (blood flow theory) : According to this theory,
tooth movement occurs as a result of alterations in fluid dynamics in the
periodontal ligament. When an orthodontic force is applied, it results in
compression of the periodontal ligament on the pressure side. The blood vessels in
this region also get compressed and this results in their stenosis. The blood vessels
beyond the stenosis balloon up, resulting in the formation of aneurysms. The
formation of aneurysms causes the blood gases to escape into the interstitial fluid
thereby creating a favorable environment for bone resorption.
Bone bending, piezoelectric or bioelectric theory: The deformation of the
crystal structure produces a flow of electric current as electrons are displaced from
one part of the crystal lattice to another. piezoelectric signal is created in response
to the force, The possible sources of electric current are: Collagen, hydroxyapatite
and Collagen hydroxyapatite interface.
When the force is applied on a tooth, the adjacent alveolar bone bends. the bends
in the bone cause small electrical charges which activate osteoblasts and
osteoclasts resulting in the resorption and deposition needed to move a tooth
through bone . Areas of concavity are associated with negative charge and cause
bone deposition. Areas of convexity are associated with positive charge and cause
bone resorption .

Pressure–Tension Effects in the Periodontal Ligament Space
sustained pressure against a tooth causes the tooth to shift position within the
PDL space, compressing the ligament in some areas while stretching it in others.
The mechanical effects on cells within the ligament cause the release of cytokines,
prostaglandins, and other chemical messengers. In addition, blood flow is
decreased where the PDL is compressed, while it is maintained or increased where
the PDL is under tension. These alterations in blood flow also quickly create
changes in the chemical environment. For instance, oxygen levels decrease on the
compressed area and carbon dioxide (CO2) levels increase, while the reverse
occurs on the tension side. These chemical changes, would stimulate cellular
differentiation and activity.
In essence, this view of tooth movement shows three stages:
(1) initial compression of tissues and alterations in blood flow associated with
pressure within the PDL,
(2) the formation and/ or release of chemical messengers.
(3) activation of osteoblasts and osteoclasts, leading to remodeling of alveolar
bone.
Phases of tooth movement
Three distinct but overlapping stages of tooth movement. They are:
• Initial phase
• Lag phase
• Post-lag phase.
Initial phase of tooth movement
Application of a force to the crown of a tooth leads to tooth movement within the
alveolus and initially a narrowing of the PDL, causing compression in limited areas
and by that changes vascular circulation and cell differentiation, this will occur
within a few hours of the application of the orthodontic force. The cells undergo
rupture and dissolution of the cell membrane leaves only isolated nuclei
(pyknosis) and this is the first indication of hyalinization. Precursor cells
(undifferentiated cells) along the alveolar bone wall differentiate into osteoclasts
and fibroblasts after 30 to 40 hours.
Hyalinization phase
At the pressure side, the degradation of the cells and vascular structures gives the
tissue a glasslike appearance under the light microscope, termed hyalinization,
represents a sterile necrotic area, characterized by: degeneration, elimination of
destroyed tissue, and establishment of a new tooth attachment.
hyalinization process stops when the adjacent alveolar bone has been removed by
osteoclastic bone resorption. The necrotic structures are removed, and the
hyalinized area repopulated by cells. The areas of the hyalinized compressed tissue
are eliminated by an invasion of cells and blood vessels from the undamaged PDL.
The hyalinized tissue is ingested by macrophages and is removed completely.
Lag phase
The lag phase is characterized by very little or no tooth movement. It is the phase
where the cellular components around the area of interest get activated to cause
tooth movement.
Post lag phase (Secondary phase of tooth movement)
The PDL space is now wider than before the start of the treatment and the tissue
under repair is rich in cells. On the pressure side, the osteoclastic bone resorption
continues with a direct bone resorption. The main feature is the deposition of new
bone on the alveolar surface from which the tooth is moving (the tension side). A
‘pre-bone’ protein matrix, or osteoid, is produced by osteoblasts on the tension
side. The periodontal fibers become embedded in the osteoid, which continuously
mineralizes to bone tissue in its deeper layer. The bone deposition on the
periodontal surface on the tension side is synchronous with the resorption process,
which occurs on the pressure side of the alveolar bone and tends to maintain the
dimension of the supporting bone tissue.
Mechanical aspects of tooth movement
Application of a force on the crown of the tooth results in tooth movement, which
depends on type, magnitude, direction and duration of the force.
Two different types of orthodontic forces exist: continuous and intermittent. Fixed
appliance systems are based on light continuous forces from an arch-wire.
However, a continuous force may be interrupted , when it is no longer active and
has to be reactivated. Such an interruption has certain advantages as the tissues are
given chance for reorganization, which is favorable for further tissue changes when
the force is again activated. An intermittent force acts during a short period and is
induced primarily by removable functional appliances.
The magnitude of forces is important for the tissue response. A light force over a
certain distance moves a tooth more rapidly and with fewer injuries to the
supporting tissues than a heavy force. The purpose of applying a light force is to
increase cellular activity and to prepare the tissues for further changes. Also it
results in less discomfort and pain to the patient. Unmyelinated nerve endings
persist in the hyalinised tissue, and are compressed during the initial stage.
The duration, is a more crucial factor than the magnitude of the force regarding
adverse tissue reactions Thus, a long treatment period in an aging bone structure
should be avoided.
The direction of forces will result in different kinds of tooth movements, often
presented in terms of tipping, torque, bodily, intrusion, extrusion and rotation.
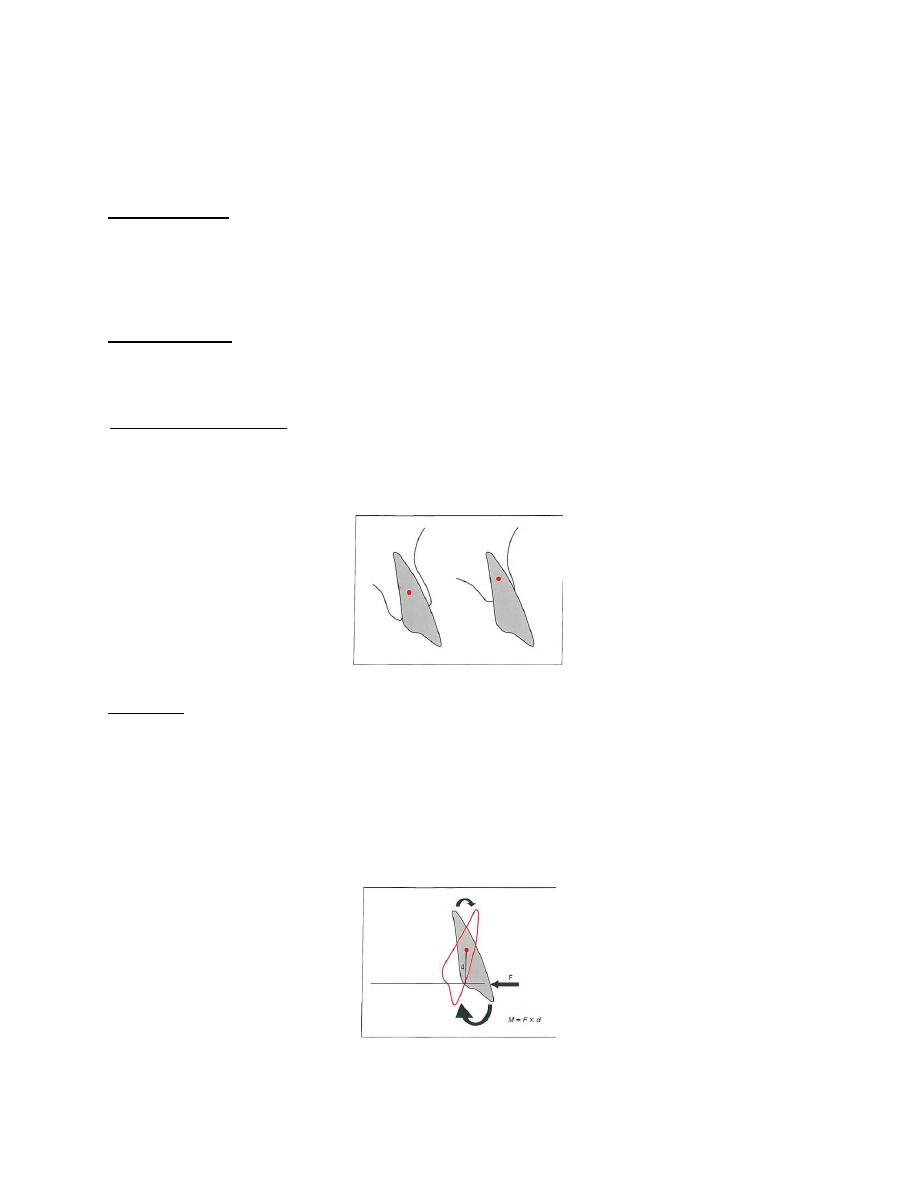
Center of resistance: a point at which resistance to movement can be concentrated.
The center of resistance is at the approximate midpoint of the embedded portion of
the root (halfway between the root apex and the crest of the alveolar bone).
Moment : a measure of the tendency to rotate an object around some point. If the
line of action of an applied force does not pass through the center of resistance, a
moment is necessarily created. Not only will the force tend to translate the object,
it also will tend to rotate the object around the center of resistance. This is
precisely the situation when a force is applied to the crown of a tooth.
Couple: two forces equal in magnitude and opposite in direction but not on the
same line. The result of applying two forces in this way is a pure moment. A
couple will produce pure rotation, spinning the object around its center of
resistance.
Center of rotation : the point around which rotation actually occurs when an object
is being moved.
Optimal force levels for different tooth movements
Type of tooth movement Approximate force (grams)
Tipping 50–75
Bodily movement 100–150
Root uprighting (torque) 75–125
Extrusion 50–100
Intrusion 15–25
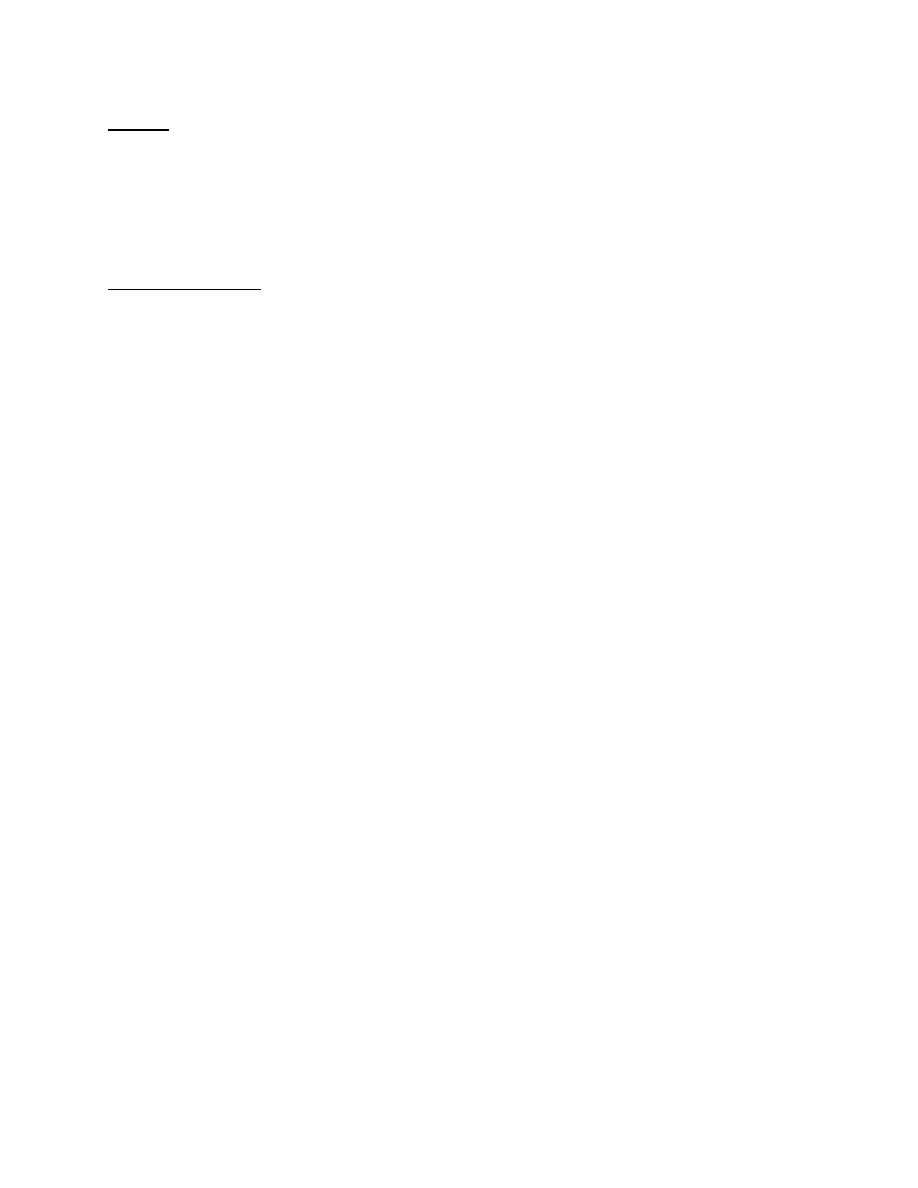
Types of orthodontic tooth movements
1- Tipping: Controlled and uncontrolled tipping,
Tipping is the easiest type of tooth movement. When a force is applied to a crown
of a tooth, the tooth tips around its center of rotation, located in the middle of the
root, close to its center of resistance. This force causes movements of the crown
and apex in opposite directions. This movement, is called uncontrolled tipping
(removable orthodontic appliances) and it is usually clinically undesirable.
While in controlled tipping center of rotation located near root apex lead to
movement of crown only with minimum apex movement (fixed orthodontic
appliances).
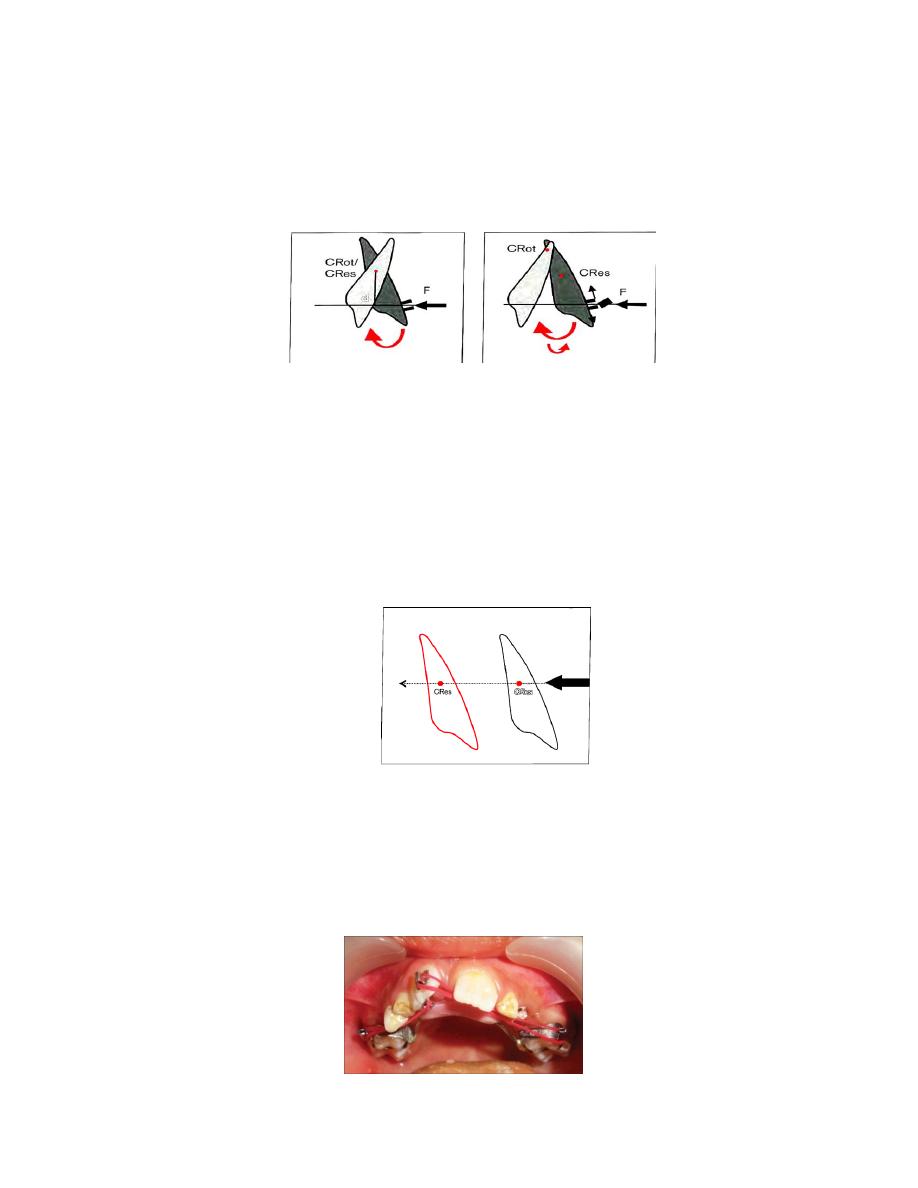
2- Translation (bodily movement),
translation of a tooth is the movement in a straight line of that tooth, without
changing the angle During translation, all the points on the tooth move the same
distance, and they therefore have the same velocity. A force having a line of action
passing through the center of resistance causes translation of the tooth. During
this movement, the center of resistance moves along the line of action of the force.
3-
Rotational movements: Rotation of the tooth around its long axis. To
achieve this type of tooth movement, the application of couple force is required
(forces from two opposite direction).
.
4-
Torque: Torque is a tipping movement of the root apex, It cannot be achieved
with removable orthodontic appliances (only fixed orthodontic appliances).
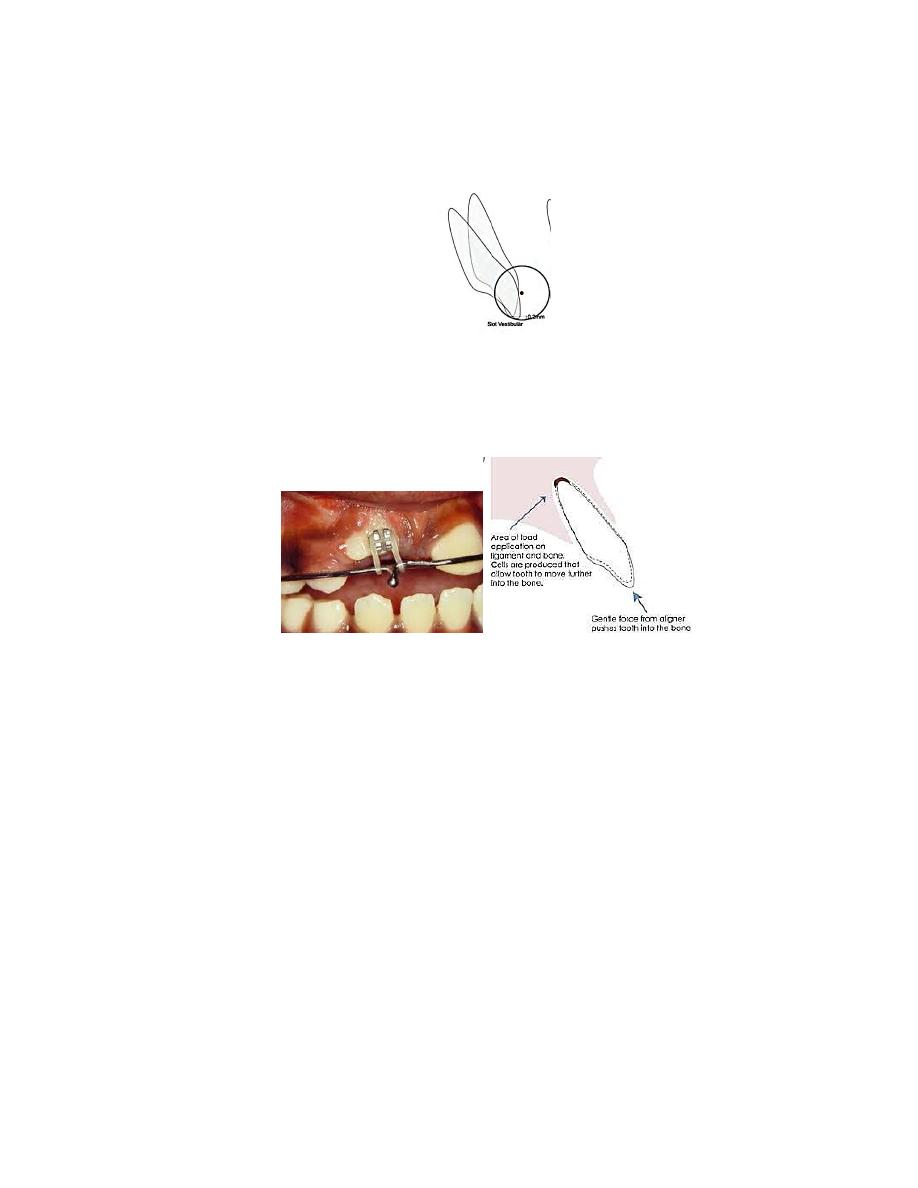
5- Intrusion and extrusion of teeth: vertical movement of individual tooth, or teeth
segments, requires some form of attachment onto the tooth surface on which the
force can act.
Retention Period an Relapse
After finishing of the orthodontic treatment, the retention period should start.
Retention prevents the teeth from returning to their original position of
malocclusion (relapse). Orthodontic correction will remain stable if the teeth are
aligned into a normal occlusion and provided with adequate retention.
The length of the retention period is controversial. Some recommend 2 to 5 years,
whereas others have suggested a minimum of 10 years or longer.

retention is necessary for three major reasons :
• The gingival and periodontal tissues are affected by orthodontic tooth movement
and require time for reorganization when the appliances are removed.
• The teeth may be in an inherently unstable position after the treatment, so soft
tissue pressures constantly produce a relapse tendency.
• Changes produced by growth may alter the orthodontic treatment result.
A relapse is defined as ‘a return towards pre-treatment conditions’, and hence is an
event of periodontal tissue reaction or dentofacial developmental changes.
Causes of relapse
1. Failure to remove the cause of malocclusion.
2. Incorrect diagnosis and failure to properly plan treatment.
3. Lack of normal cuspal interdigitation.
4. Arch expansion, laterally and/or anteriorly.
5. Incorrect arch size and harmony.
6. Incorrect axial inclinations.
7. Improper proximal contacts.
