Host defense in the dentogingival area
Specific microorganisms responsible for periodontic disease include G.-ve facultative or anaerobic bacteria are predominant bacteria as;
• Porphyromonas gingivalis
• Aggregatibacter actinomycetemcomitans
(previouslyActinobacills actinomycetemcomitans)
3. Treponema denticola
4.Tannerella forsythia( previouslyBacteriod forsythus).
5.Fusobacterium nucleatum
6.Prevotella intermedia
7.Campylobacter rectus
8.Peptostreptococcus micros
9.Eikenella corrodens
To function as pathogen, the bacteria must :-colonize appropriate host tissue site & then cause destruction of host tissue in periodontitis.Invasion of bacteria or its products, later on cause direct & indirect tissue destruction( depend on virulence factor of the pathogen).
• Oral cavity with its micobiota represent an open growth system as nutrient & microorganisms can enter & remove by the actions of :--saliva flow-gingival fluid flow-chewing -oral health procedure-desquamation of epithelial cellOral cavity supply favorable conditions as; humidity,temperature ,pH,C02 and O2 .
Growth in Oral Cavity
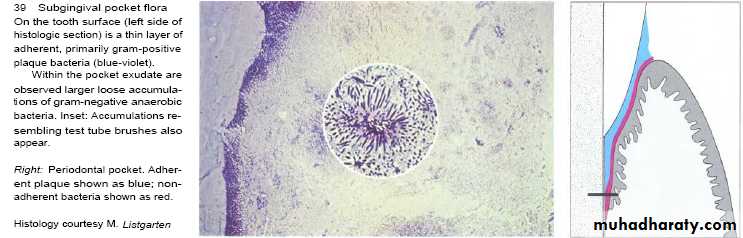
Some microorganisms are able to retained in pits & fissures or in between teeth.Gingival sulcus & perioodental pocket bathed in gingival fluid that flow outward from base of pocket so bacteria should attach to available surface (tooth ,root & preexisting plaque mass) to avoid displacement by fluid flow.
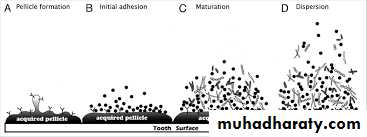
It provides: nutrients, buffer action, acidic conditions, fermentation products & remove inhibitory waste products.Salivary mucin induce lubrication of mucosa, water proofing ,interfere with bacterial adherence (epithelial receptor) ,mechanical cleansing of the exposed oral surface.Nevertheless saliva on tooth surface can form organic film (named acquired pellicle) that form solid ground for bacterial adherence & growth.
Saliva
Microorganisms carry –ve charge which tend to repel each other electro statically.Tooth surface also carries -ve charge that repel cells theAttractive (electrodynamics or vanderwaals) & repulsive forces allow separation from tooth surface producing a gap. This gap influence by ions(where acidic pH or increased concentration of cations) will decrease gap.
Bacterial adherence
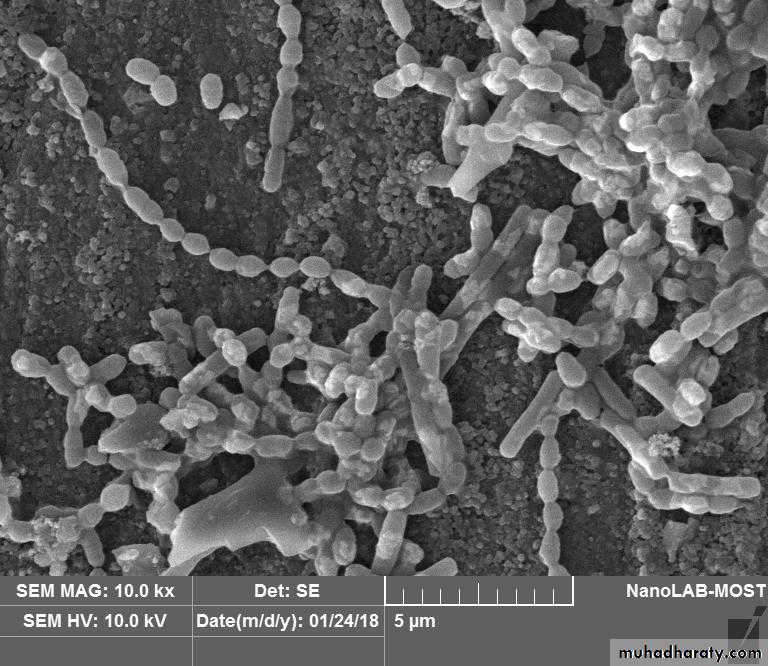
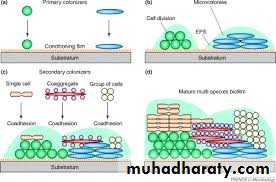
Microorganisms surrounded by highly hydrated matrices (glycocalyses) consist of regular array of rod-like glycoprotein appendages but mostly composed of matrix of polysaccharide(S.sanquis, S.mitis, S.salivarius & S.mutans synthesis it from dietary sucrose).Glycocalyx extend beyond highly charged surface & can bridge the gap.Other attractive forces like hydrogen bonding between glycocalyx & tooth surface.Also some bacteria have long appendages are called pili or fimbriae.
Biofilm of Facklamia hominis an d Streptococcus mutans on Composite surfaces 10.00 kx
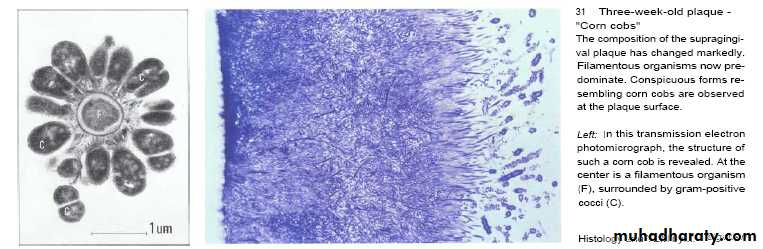
Pili can bridge the gap. Adhesins on pili & glycocalyx recognize specific receptor molecules on tooth surface which is proline-rich protein of pellicle (as done by Actinomycoses viscosus).Small irregularities of acquired pellicle allow adherence of microorganisms that start to grow & multiply to form colonies. On the other hand, secretory IgA & agglutinins surround the bacteria & prevent its adherence to tooth surface.Supragingivally, the aggregated microorganisms form a corncob structure while subgingivally,they form test tube brush design
CoaggregationMany species attach directly to host surfaces,while other species attach indirectly to that already attached bacteria.Bacterial attachment to tissue like adherence of Porphymonas gingivalis to epithelial & connective tissue component ,fibrinogen & fibronectin.Attachment of Treponema denticola to fibroblast through surface protein & attachment of Fusobacterium nucleatum to neutrophils through protein.
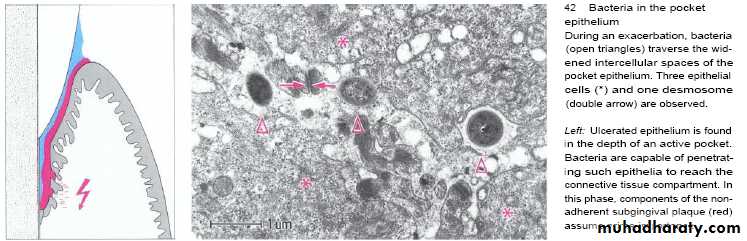
• Microorganisms(cocci,rods,filaments & spirochetes ) invade the host tissue could be detected in patients with NUG, advanced chronic periodontitis & aggressive periodontitis. Microorganisms can be been seen in gingival connective tissue & in proximity to alveolar bone enter through ulceration in the epithelium of gingival sulcus or pocket & observed in intercellular spaces of epithelial cells or directly through penetration of host epithelial or connective tissue cells like that done by Aggregatibacter actinomycetemcomitans (previouslyActinobacillus actinomycetemcomitans)& Porphmonas gingivalis.
Host Tissue Invasion
Invasion related to disease & it’s a key factor that distinguish between pathogenic from non pathogenic bacteria gram -ve species .Invasion can deliver toxic products & enzymes to the host tissues. The burst period in bacterial invasion enables the persistence of that species in periodontal pocket by providing a reservoir for recolonization. Supporting to this hypothesis , mechanical debridment alone is insufficient to eliminate Aggregatibacter actinomycetemcomitans (previouslyActinobacillus actinomycetemcomitans in patients with localized aggressive periodontitis, so it needs antibiotic cover.
Host Tissue Invasion
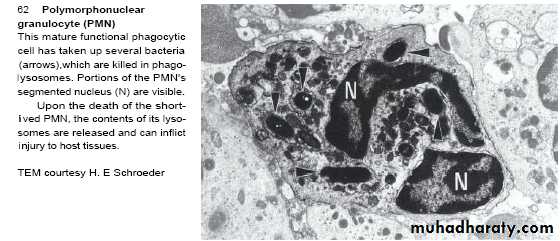
To survive in periodontal enviroment , the bacteria must evade host response by the following mechanisms;1-Antibodies-degrading proteases by specific microorganisms. 2- T.forsythia & Fusobacterium nucltium induce apoptosis, a form of cellular suicide in leukocytes.3- Bacterial products suppress the activity of or kill PNL & other leukocytes (leukotoxin & cytolethal toxin by A. actinomycetemcomitans). 4- The presence of pathogenic microorganisms stimulate production of interleukin-8, a proinflammatory chemokine that provides a signal for the recruitment of PNL to local sites.So, Porphymonas gingivalis can inhibit production of IL-8 by epithelial cell that enable microorganisms to evade PNL-mediated killing.5- T.denticola induce inhibition of superoxide production which induce bacterial killing.
It is done directly by bacterial products(ammonia ,volatile sulfur compounds, fatty acids & peptide ) that inhibit growth or alter metabolism of host cells . Baterial enzymes can degrad all host tissue & intermicrobial matrix molecules as proteolytic enzymes from Porphymonas gingivalis include trypsin-like enzyme that degrade collagen,fibronectin & antibodies. After tissue destruction,invasion into host can be facilitated e.g.collagenase,keratinase,phospholipase A, neuraminidase & sulfatase.
Microbial Mechanism of Host Tissue Damage
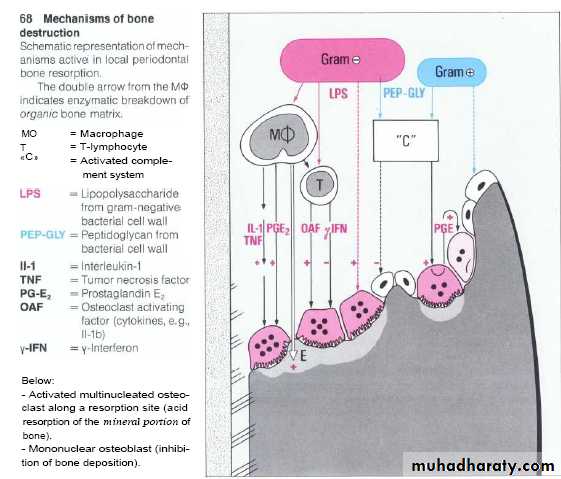
Indirect damage through release of host derived mediators(endogenous mediators) lead to stimulate bone resorption, activate or inhibit other host cells like release of IL-1 that stimulate neutrophils & macrophage,prostoglandin & IL-8.
Indirect Tissue damage
Lactoferrin ( iron binding protein) represents an important defense factor against bacterial injuries including those related to Streptococcus mutans and periodontopathic bacteria through its ability to decrease bacterial growth, biofilm development, iron overload, reactive oxygen formation and inflammatory processes. Lysosome (bacteriocidal effect); in saliva & PML work on veillonella & A. actinomyetemcomitans.
Defense mechanism by saliva
Bacteriocin (bacterial product) attack DNA.Peroxidase :-It convert H2O2 (produce by streptococcus) in presence of salivary thiocyanate into H2O& hypothiocyanite that is less toxic to epithelial cells & serve as feed-back inhibitor of H2O2 production, thiocyanate is toxic to microorganisms too. it inhibit the growth, respiration and metabolism of most species of oral bacteria.
Defense mechanism by saliva
Myeloperoxidase It is enzyme similar to salivary peroxidase released by leukocytes.It is bacteriocidal to actinobacillus & inhibit attachment of actinmyces to the tooth. Lactoperoxidaseoxidation of susceptible microorganisms.
Defense mechanism by saliva
Buffering It is done by bicarbonate & phosphate .Tooth integrity by minerals that assist in maturation & maintenance of the tooth ---remineralization of teeth.
Defense mechanism by saliva
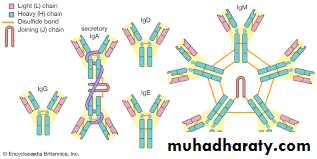
Saliva contain large amount of (IgG,IgM,IgA).Many salivary bacteria showed coated with secretary IgA that inhibit bacterial attachment to epithelial cell & tooth surface.Enzymes seen in saliva derived from salivary glands, microorganisms, leukocytes, oral tissue & ingested substance, its increase during periodontal disease.
Defense mechanism by saliva
Antiproteases that inhibit cathepsins (cysteine proteases),elastase & collagenaseCoagulation factors(factors,8,9,10 & hagman factor) that hasten blood coagulation & protect wounds from bacterial invasion.
Defense mechanism by saliva
Salivary mucin is not static, where the mucous takes a direct & constant course along specific routes toward esophagus. In this way ,microorganisms inoculated into mouth do not spread widely clearance time is about 30min. interruption occur by saliva as in Sjogrens syndrome or mouth breather.
Defense mechanism by saliva
Microorganisms can grow & multiply in dentogingival area by adherence. S.sanquis & S.mitis produce IgA protease antigenic shift & drift and change their surface characteristic.
Defense mechanism by saliva