Imaging of bone disease
1- plain x-ray
2-radio isotope
3- CT scan
4- MRI

PLAIN X-RAY
1-BONE DENSITY
2-PERIOSTEAL REACTION
3-CORTICAL THICKENING
4- ALTERATION IN TRABECULAR PATTERAN
5-ALTERATION IN THE SHAPE OF BONE
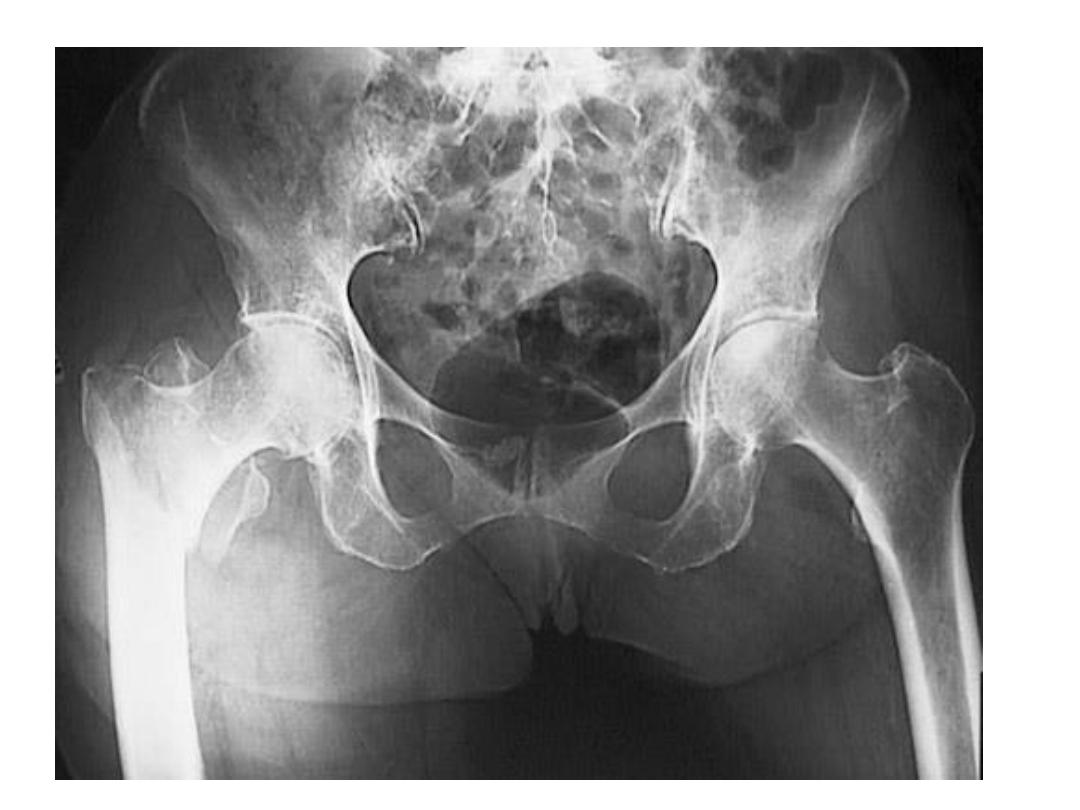
Decrease bone density
Generalized :
a-osteoporosis
b-osteomalacia and rickes
c-hyperparathyroidism,renal
osteodystrophy
d- mutiple myeloma
e-osteogensis imperfecta
Localized :
Fracture of one bone
Sudeck atrophy -sever osteoporosis
Increase bone density
a-osteopetrosis
b-myelosclerosis
c-sclerotic metastasis
d-paget s disease
e-prostatic metastasis
Periosteal reaction
Excess bone prodused by the
periosteum which occurs in response to
such condition
a-neoplasm
b-inflammation
c-trauma

Cortical thickening
Laying down of new bone ,there is no
separated lines or spicules of calcification as
seen in periosteal reaction
Causes:
1-chronic osteomylitis
2-healed trauma
3- response to chronic teroids
4- benign neoplasm
Alteration in the trabecular pttern
Reduction in number of trabeculae and alteration
in the remaining ones
a-osteoporosis :thick cortex ,long trabeculae
b-paget s disease:thick trabeculation in cortex and
medulla
c-haemolytic anemia :biconcave bone marrow

Alteration in the shape of the bone
a-achondoplasia
b-multiple stenosis
c-acromegaly
e-expnding bone tumor

osteoporosis
•
Due to defenciency of the protein matrix
•
Matrix reduced in quantity
•
Caueses:
•
1-idiopathic
•
2-cushing syndrome
•
3-postmenopausal

osteomalacia
Lack of calciumin the body tissue
With poor mineralization of osteoid
If this occurs before epiphyseal closure
It is called rickets while in adults it is called
osteomalacia



Periosteal Reactions
Benign
None
Solid
More aggressive or malignant
Lamellated or onion-skinning
Sunburst
Codman’s triangle
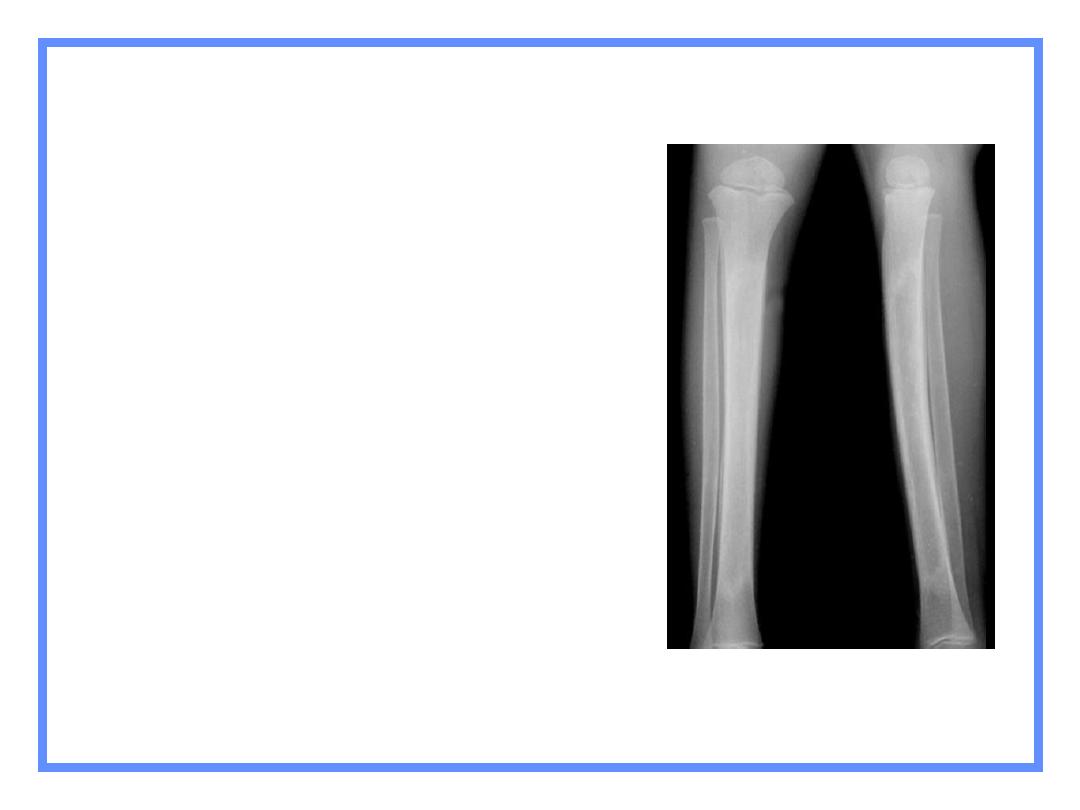
Chronic osteomyelitis
Benign
None
Solid
Aggressive/malignant
Onion-skinning
Sunburst
Codman’s triangle
Periosteal Reactions
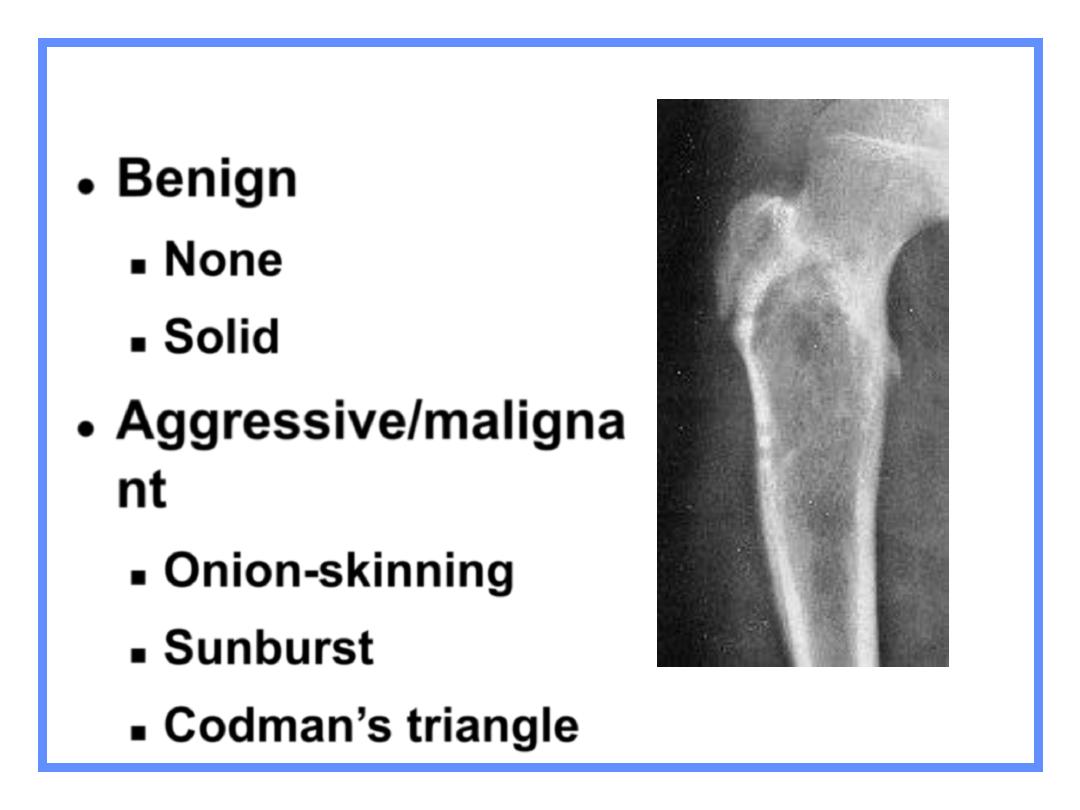
Benign
None
Solid
Aggressive/maligna
nt
Onion-skinning
Sunburst
Codman’s triangle
Periosteal Reactions
Ewing’s sarcoma
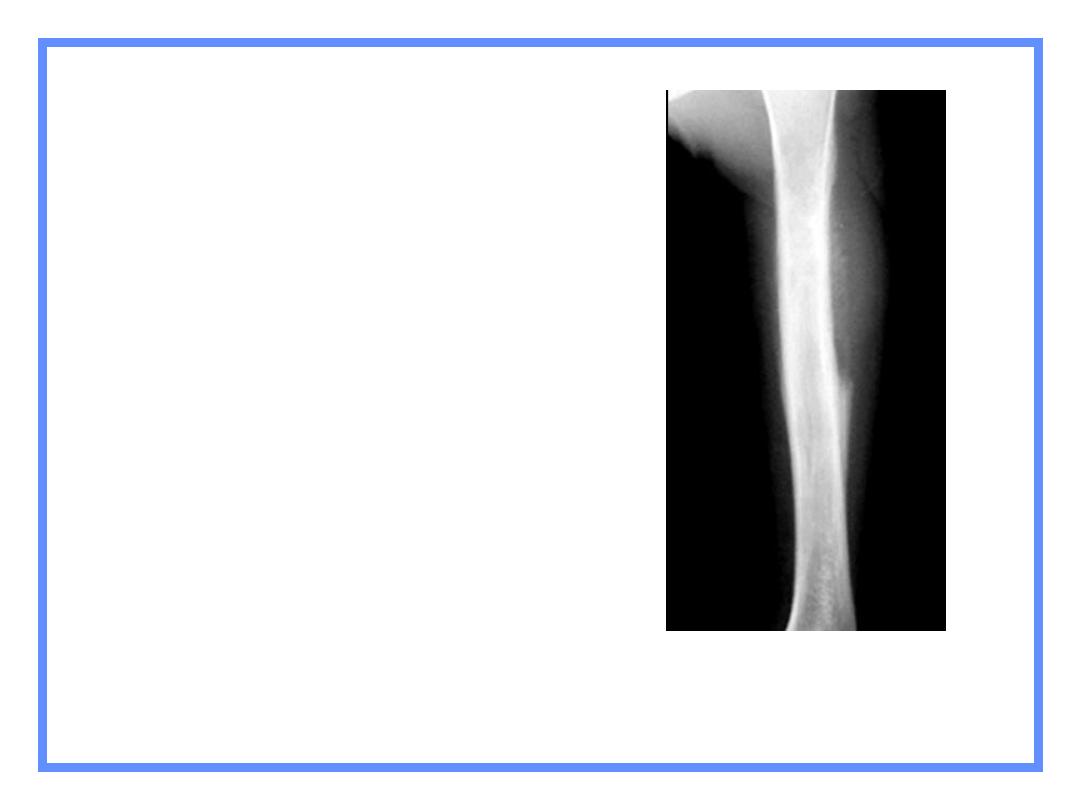
Ewing’s-Codman’s
triangle
Benign
None
Solid
Aggressive/maligna
nt
Onion-skinning
Sunburst
Codman’s triangle
Periosteal Reactions
Osteosarcoma
Benign
None
Solid
Aggressive/malignan
t
Onion-skinning
Sunburst
Codman’s triangle
Periosteal Reactions
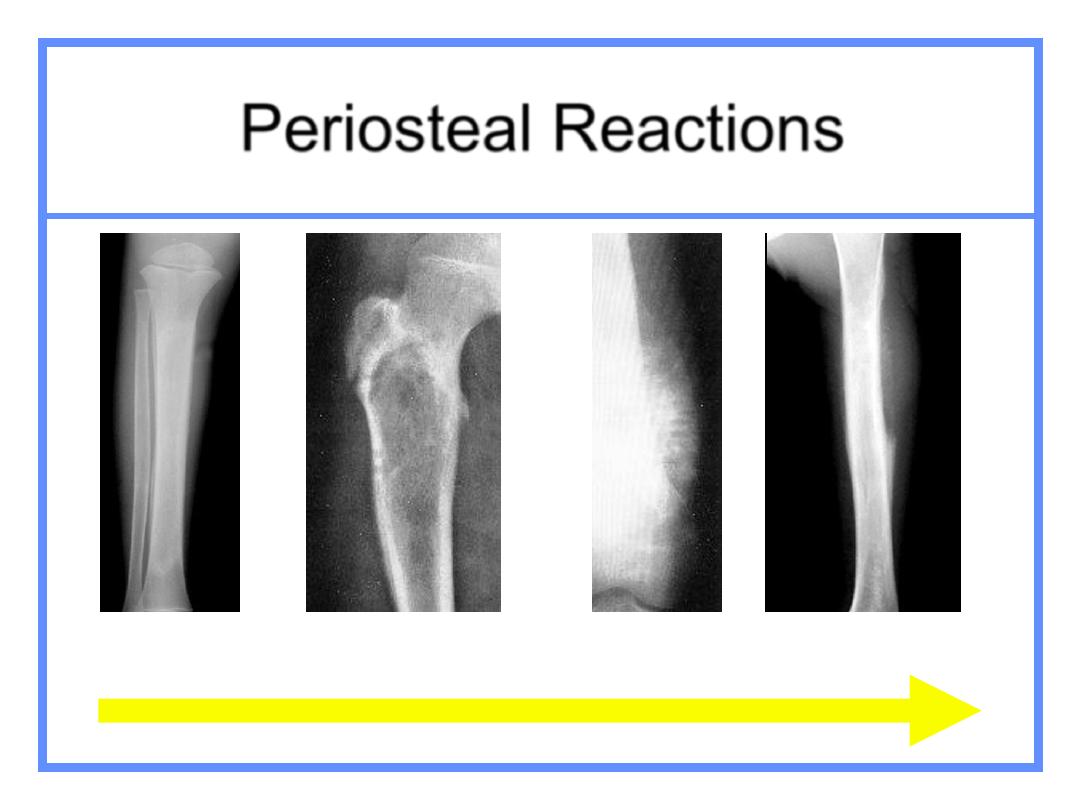
Periosteal Reactions
Solid
Lamellated
Codman’s
Sunburst
Less malignant
More malignant

Alteration in trabecular patteran
1-haemolytic anemia
2-paget s disease
3-marrow hyerplasia

CT SCAN
1-disc herniation
2-imaging of complex shapd bone
3- extend of bone tumors both within
bone and adjacent soft tissue

Radioisotope scanning
1-detecion of metastasis
2-detection of osteomylitis
3- to decide if an abnormality on
rdiograph no seen
4- other abnormalities

Infection of bone
• An invading organism may attack bone by direct invasion from
an infected wound, or from an infected joint, or it may gain
access by
haematogenous spread from distant foci, usually in the skin
• Haematogenous osteomyelitis usually occurs during the period
of growth, but all ages may be affected and cases are even found
in old
• age.
• In infants,
Streptococcus
usually causes osteomyelitis. In
• adults,
Staphylococcus is
more co
mmon

osteomyelitis
• In the
infant,
vessels penetrate the epiphyseal plate
in both directions. Metaphyscal infections can thus
pass to the epiphysis and then the joint. Acute
pyogenic arthritis is therefore a relatively
• common sequel of osteomyelitis in infants. The
periosteum in nfants is very loosely attached to
underlying bone.

osteomyelitis
• In
childhood,
between 2 and
1 6
years, few vessels
cross the epiphyseal
• plate though the periosteum is still relatively
loosely
• attached. The epiphysis and joint are thus less
frequently infected.
• The metaphyseal vessels terminate instead in
slow-flowing sinusoids
• which promote blood-borne infective change

osteomyelitis
• In the
adult,
after the epiphyseal plate has fused,
metaphyseal
• and epiphyseal vessels are again connected so
that septic arthritis
• can recur. Periostcum, however, is well hound
down and articular
• i nfections via a metaphyseal route are less
likely.

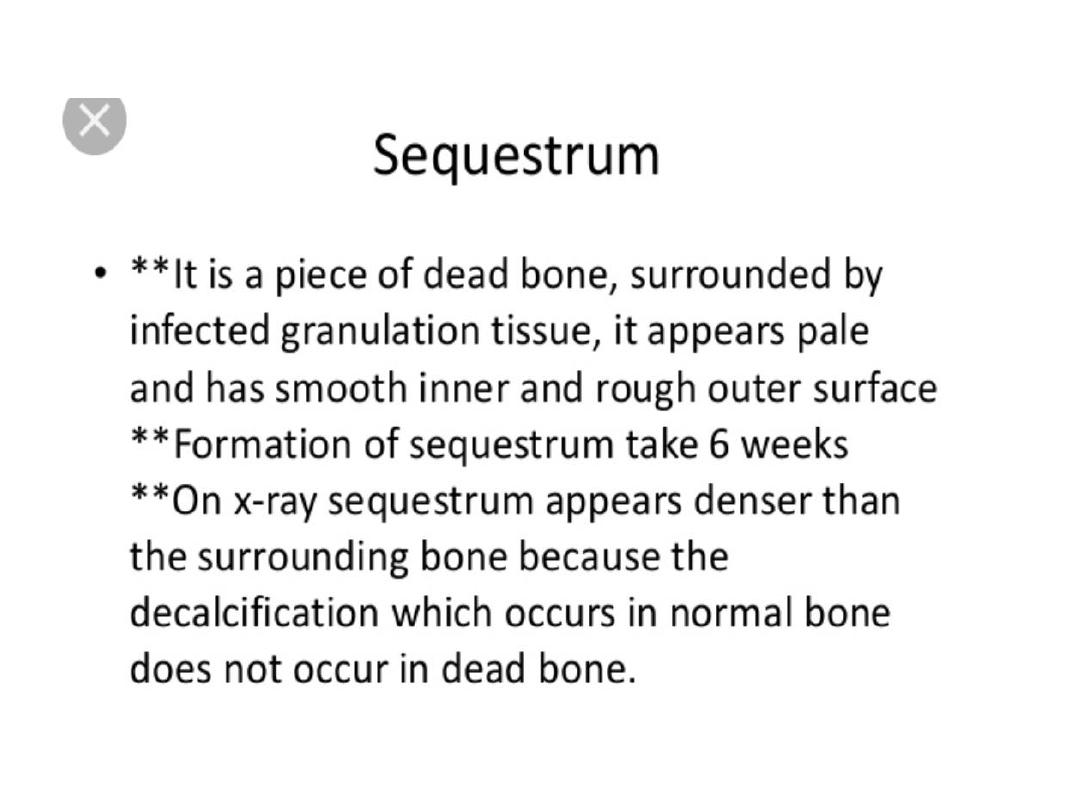
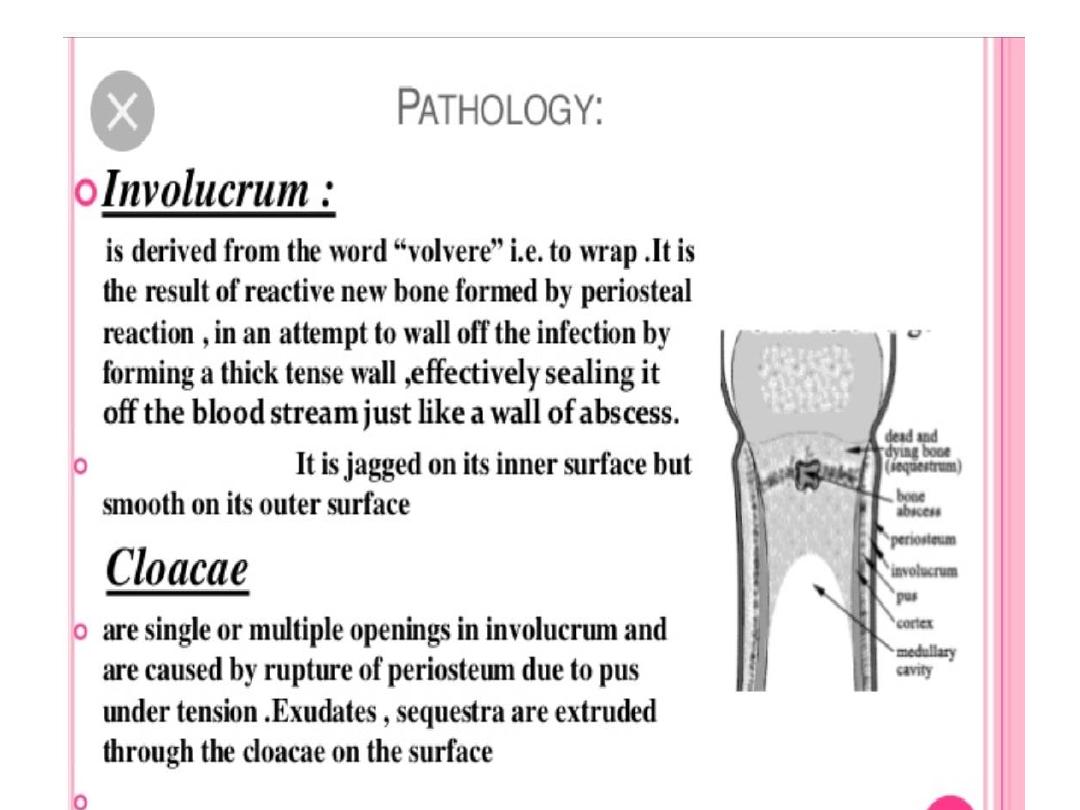
Osteomyelitis
• The formation of pus in the bone deprives local cortex and
• medulla of its blood supply.
• Dead bone is resorbed by
granulation tissue.
Pieces of dead
bone, especially if cortical or surrounded by ,
pus,
are not
resorbed and remain as
sequestra
.
• As sequestra are devitaliscd they remain denser than
surrounding vital bone, which becomes demineralised due to
hyperaemia and immobilisation.
• Absorption of sequestra is also facilitated by the presence of
• an
im'olucrum.
• The involucrum forms beneath vital periostcum •
which bas
been elevated by pus.
•
As periostcum is poorly attached in
nfants, involucrum
formation is greater and so is the resorption of dead bone, and
healing.

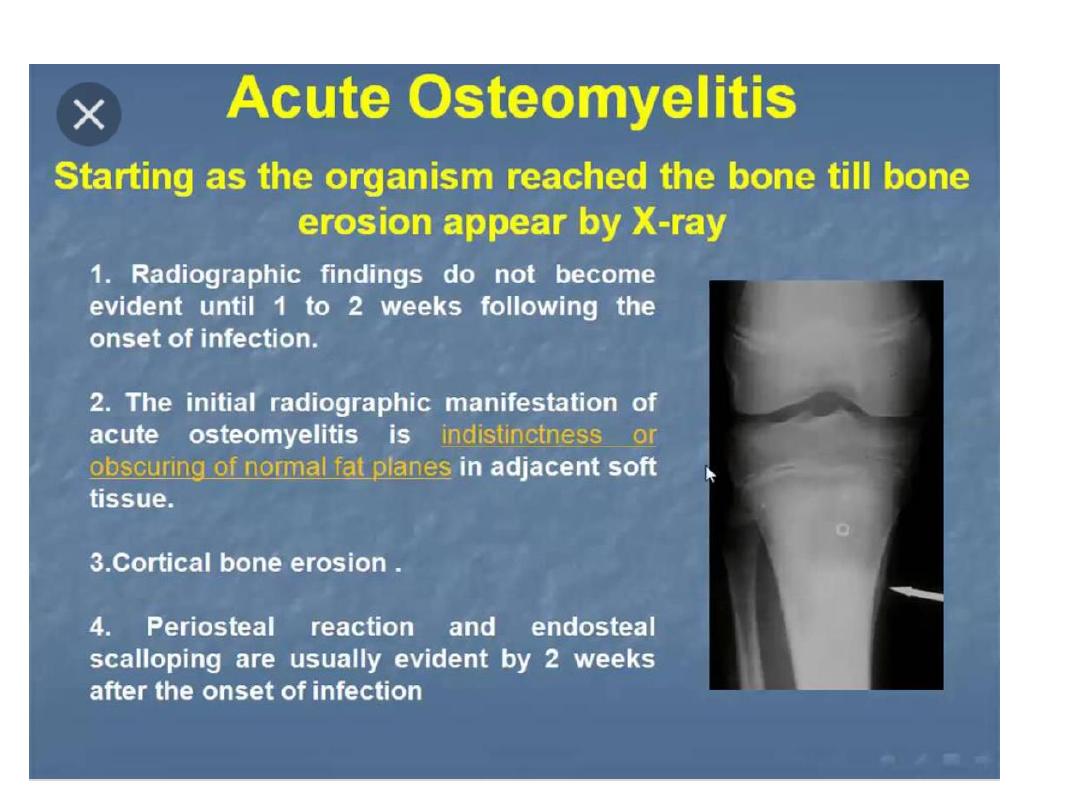
osteopmyelitis
• Acute osteomyelitis:
• 1-oedema
• 2-soft tissue swelling
• 3- bone destruction

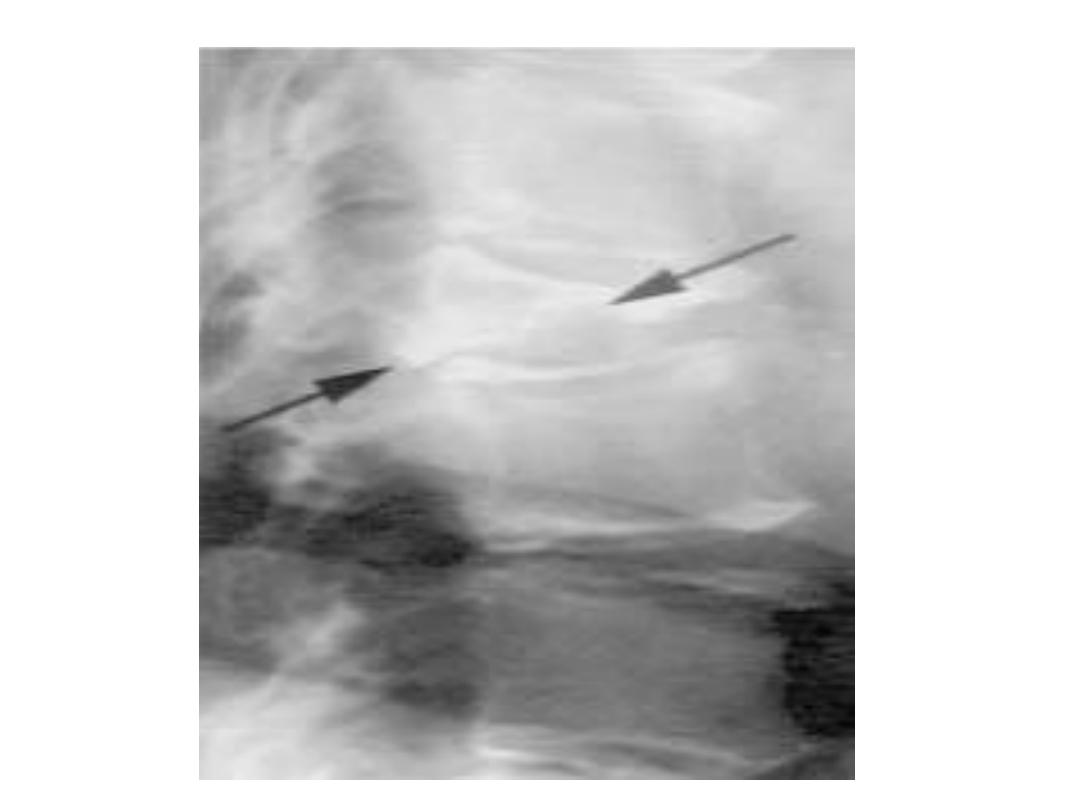
osteomyelitis
• Chronic osteomyelitis :The preliminary
radiograph :
• 1- There is cortical thickening
• 2- evidence of intramedullary cavitation and
angulation.
• 3-Linear calcified densities in the
• soft tissues may represent extruded sequestra.
•
4- sequestrum in bone

Chronic osteomyelitis
•
MR image shows
1- muscle wasting;
2-the deformity of the bone is again
demonstrated.
3-There is extensive increase in signal within the medulla,
indicating
•
a fluid collection.
•
4- A band of high signal can be seen extending from
•
the medulla superiorly, through the cortex laterally and into
the adjacent
•
soft tissues.
•
5-There is an effusion in the knee joint and oedema of the
subcutaneous
•
soft tissues.

osteomyelitis

Osteomyeltis
• I n areas of dead periostcum, defects in the
involucrum occur..
• These
cloacae
allow pus and sequestra to
escape, sometimes to the
• skin via a sinus. The track and its deep
connection to bone can then
• be demonstrated by sinograpby using water-
soluble contrast medium
