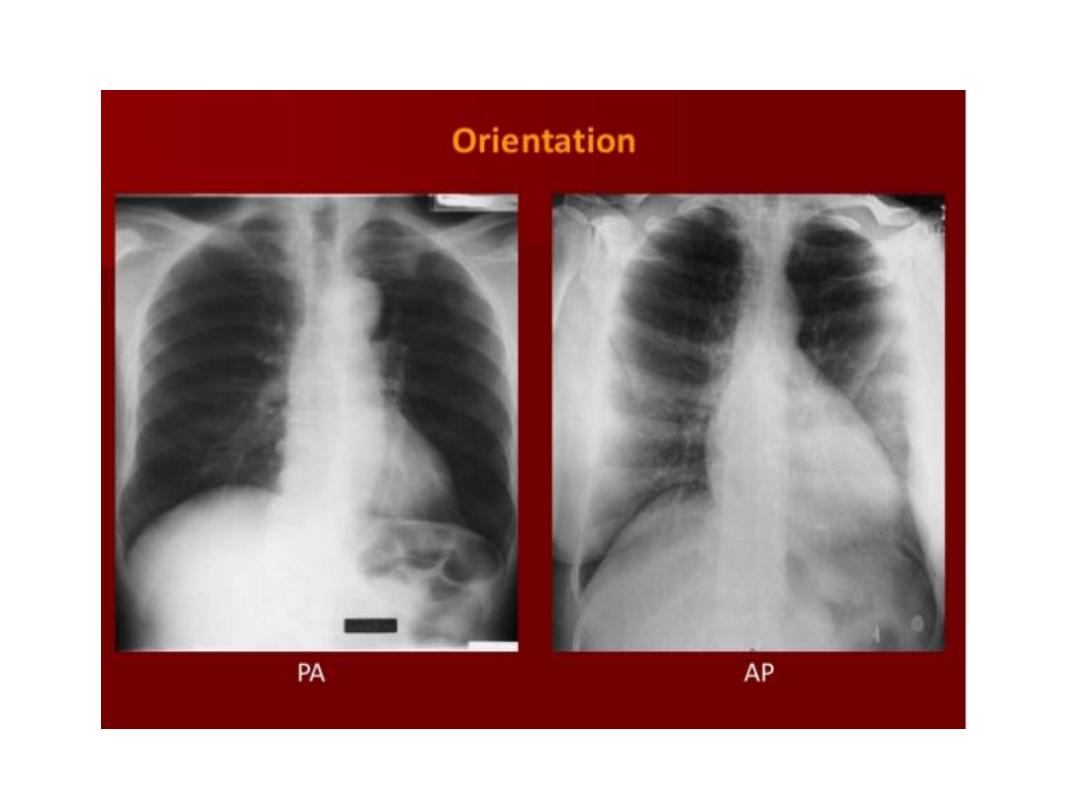
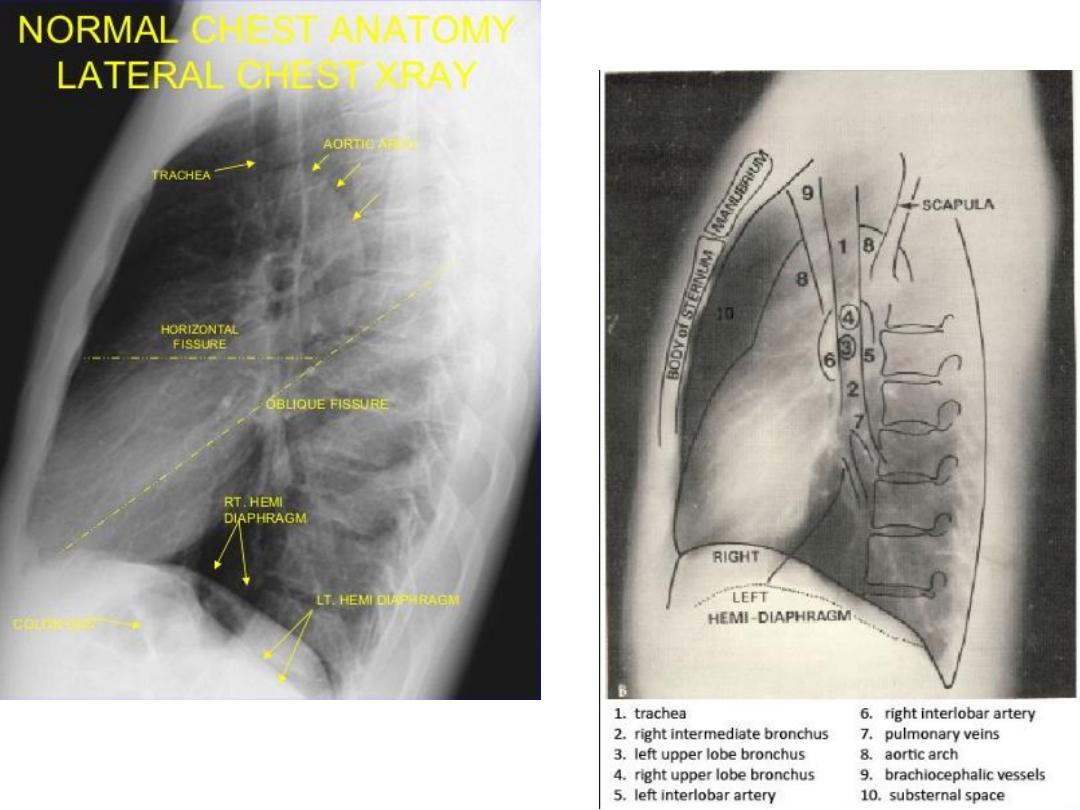
Routine CXR: is PA known as frontal view with optional lateral
view.
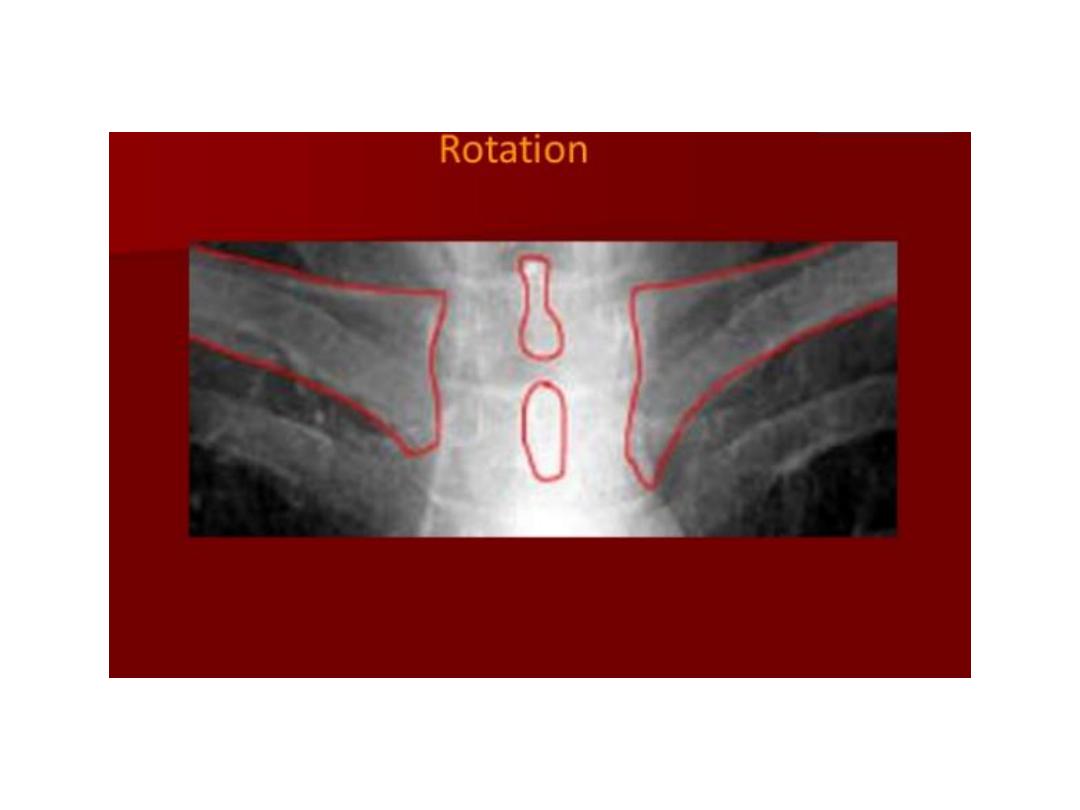
Both should exposed in full insp. And patient in upright position.
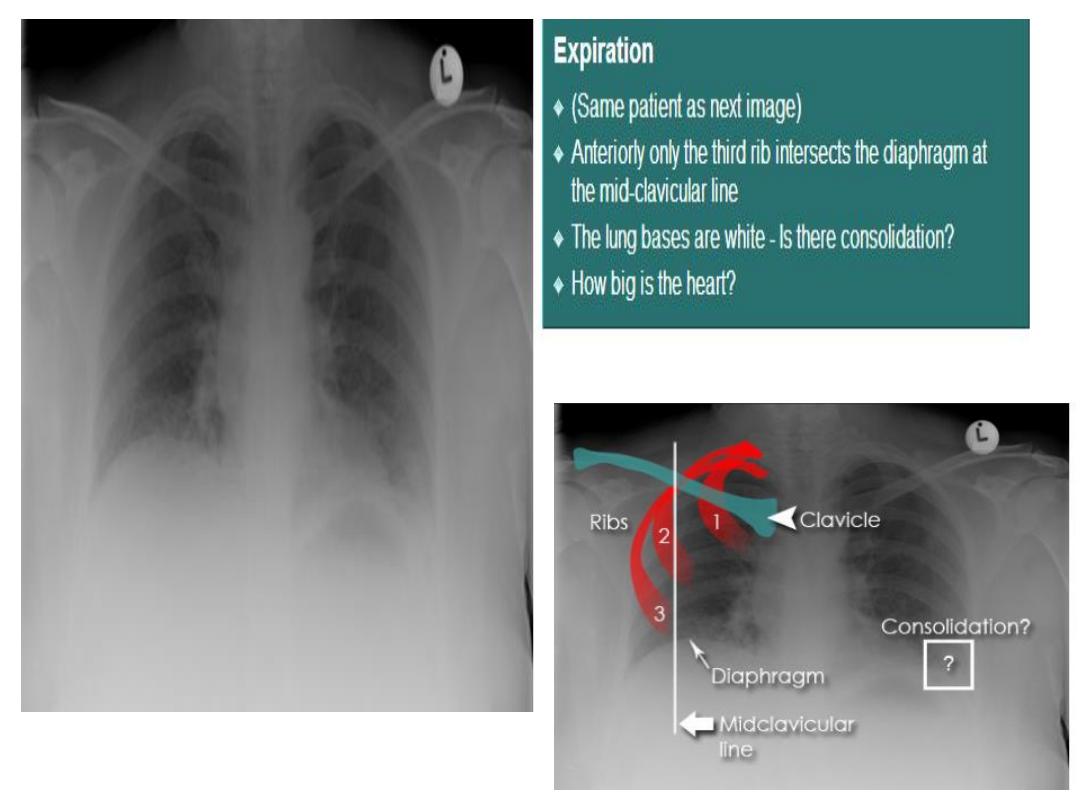
Films taken in exp. Are difficult to interpret because:
1- hazy lung base.
2- heart shadow increase in size.
CXR approach:
1- trace the diaphragm: the upper surface of diaphragm should be
clearly visible from CPA to other, except when heart and
diaphragm in contact with diaphragm.
On good insp., the dome of rt. Hemidiaphragm at level of ant.
End of 6
th
rib.
The rt. Hemidiaphragm being up to 2.5 cm higher than the left.
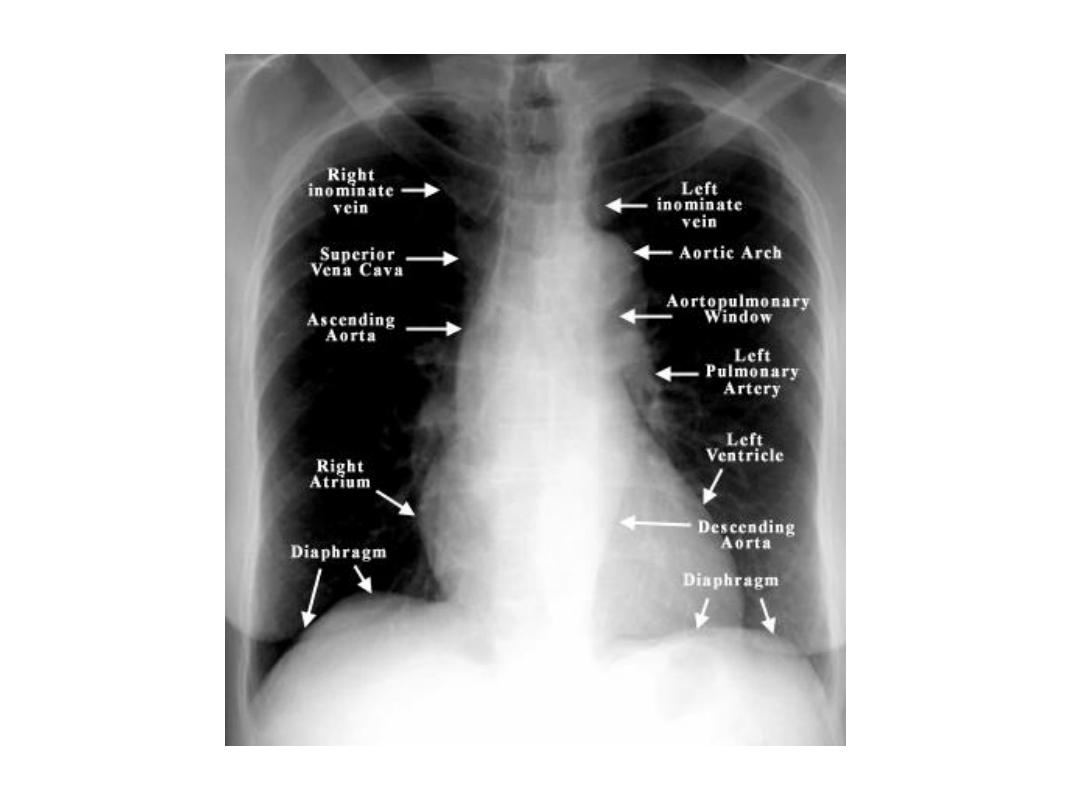
2- check the size and shape of heart.

3- check position of heart and mediastinum: normally trachea lies midway
or slightly to right of midpoint between medial end of clavicles.
One third of heart is on rt. Of midline and two thirds to left.
4- looks at mediastinum: the outline of heart and med. Should be clearly
seen except where the heart lies in contact with the diaphragm.
The rt. Sup. Med. Border is usually straightly or slightly curved.
Left sup. Med. Border is ill defined above aortic arch.
With increasing age the aorta elongates, lead to unfolding of aorta
because aorta fixed at aortic valve and diaphragm, lead to ascending
aorta deviate to rt., descending aorta deviate to left.
In young children the normal thymus is often clearly seen, with
characteristic sail shape, projecting to rt. Side med.
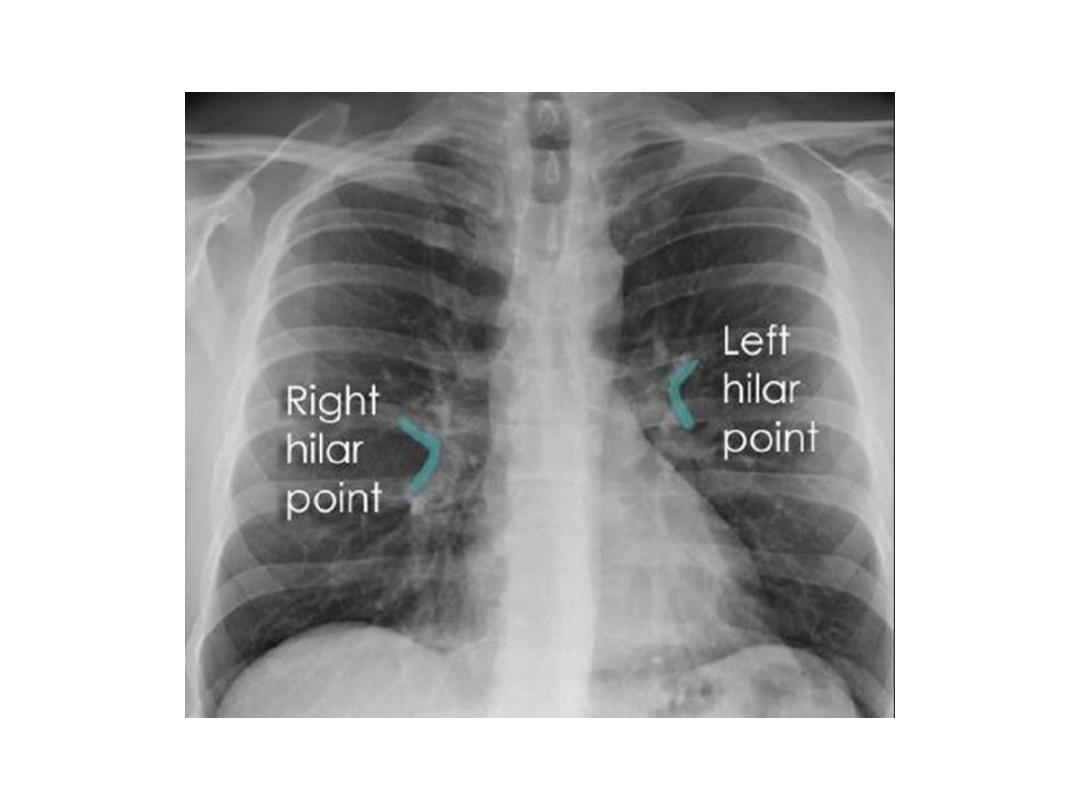
5- hilar shadows: represent the pulm. Arteries and veins.
Air within major bronchi can be recognizes, but walls not usually visible.
Hilar LNs normally too small to seen.
The left hilum usually slightly higher than rt. Side.

Unfolded aorta

6- examine the lungs: blood vessels, interlobar fissures, walls of certain larger
end on bronchi, are only identified within normal lung.
The fissures can only be seen if they lie along the line of X ray beam.
Usually only horizontal fissure, minor fissure, visible in frontal projection,
while oblique, major, fissure only seen on lateral view.
1% there is extra fissure as azygos fissure: during normal intrauterine
development, azygos vein migrates through the lung from chest wall to med.,
in those with azygos lobe, the vein fail to reach tracheobronchial angle and
lies within lower end of azygos fissure, this variant of no clinical significance.
Nipples are usually in 5
th
ant. Rib space.
On lateral view: reliable feature is that as go down the thoracic vertebral
bodies, each verteb. Body app. More lucent than above till reaching the
diaphragm.
7- check irregularity of ribs, clavicles and spine and examine soft tissue:
Bones of chest should checked for fractures and metastasis.
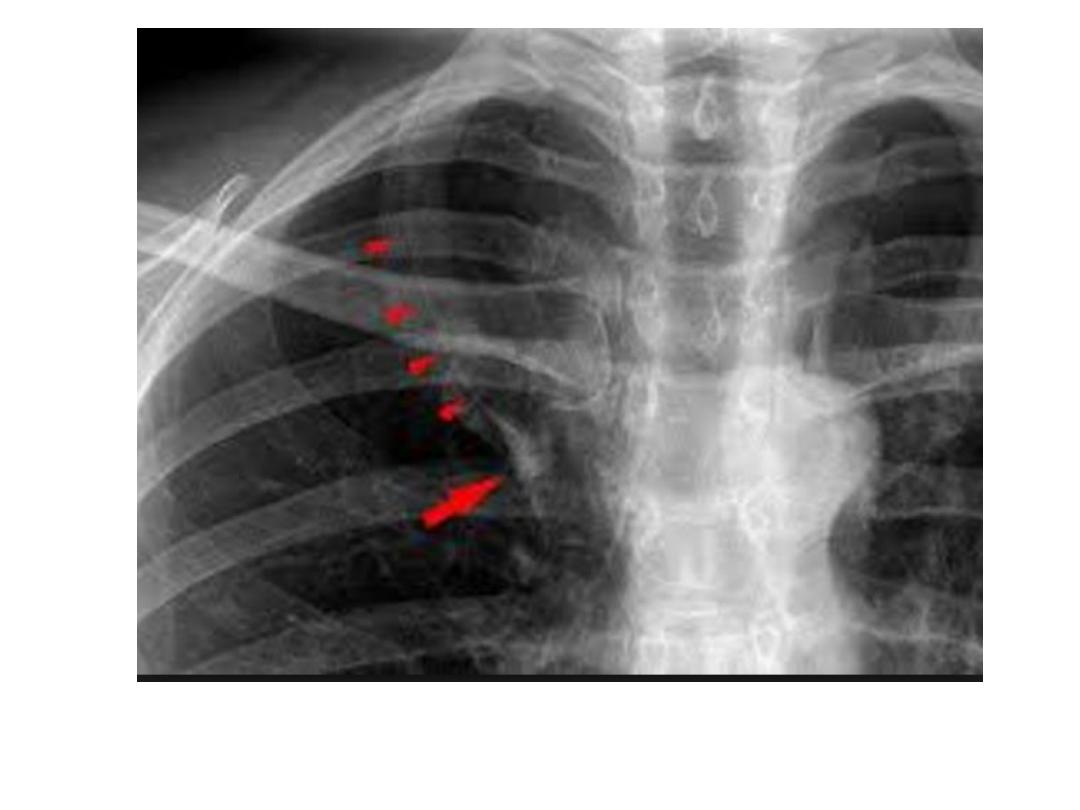
Rib notching should be noted as it may indicate coarctation of aorta.
In female check that both breasts are present, if mastectomy: reduction in
soft tissue bulk leads to increase in transradiancy of that side of chest.
Azygos fissure

Nipple shadow
Rib notching coarctation of aorta

Female breast shadow

Left mastectomy
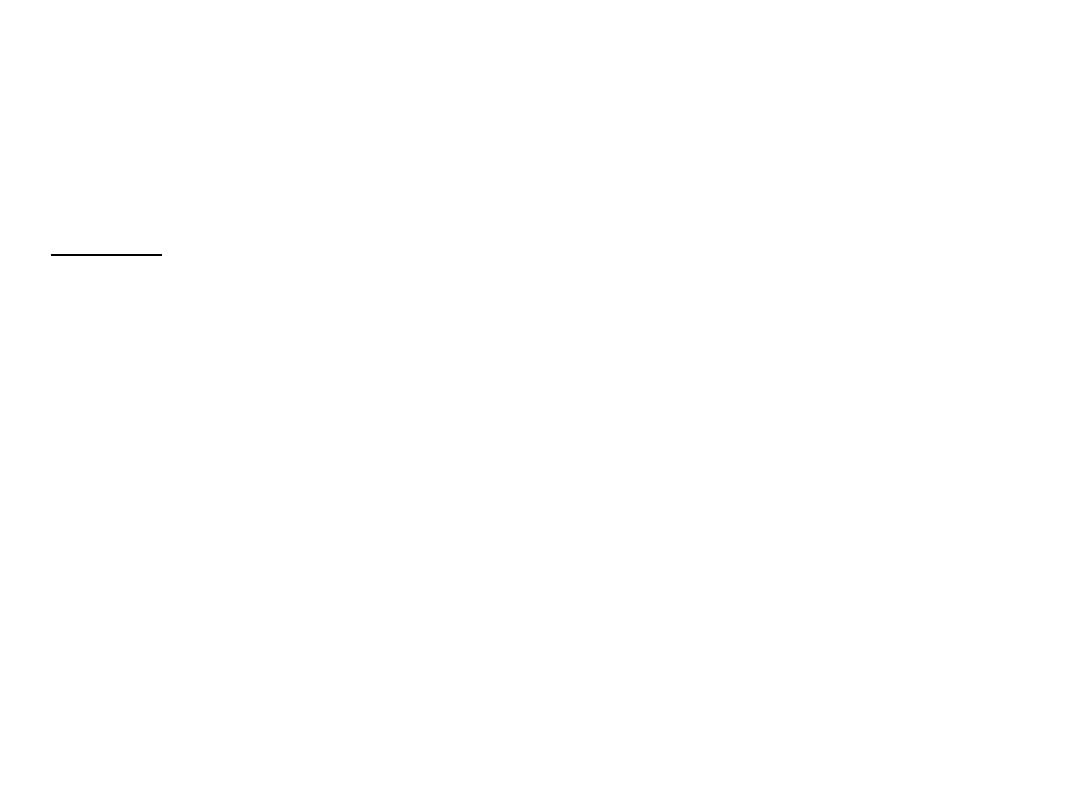
8- assess technical quality of the film: correctly exposed routine PA CXR is one
in which the ribs and spine behind the heart can be identified but lung not
overexposed.
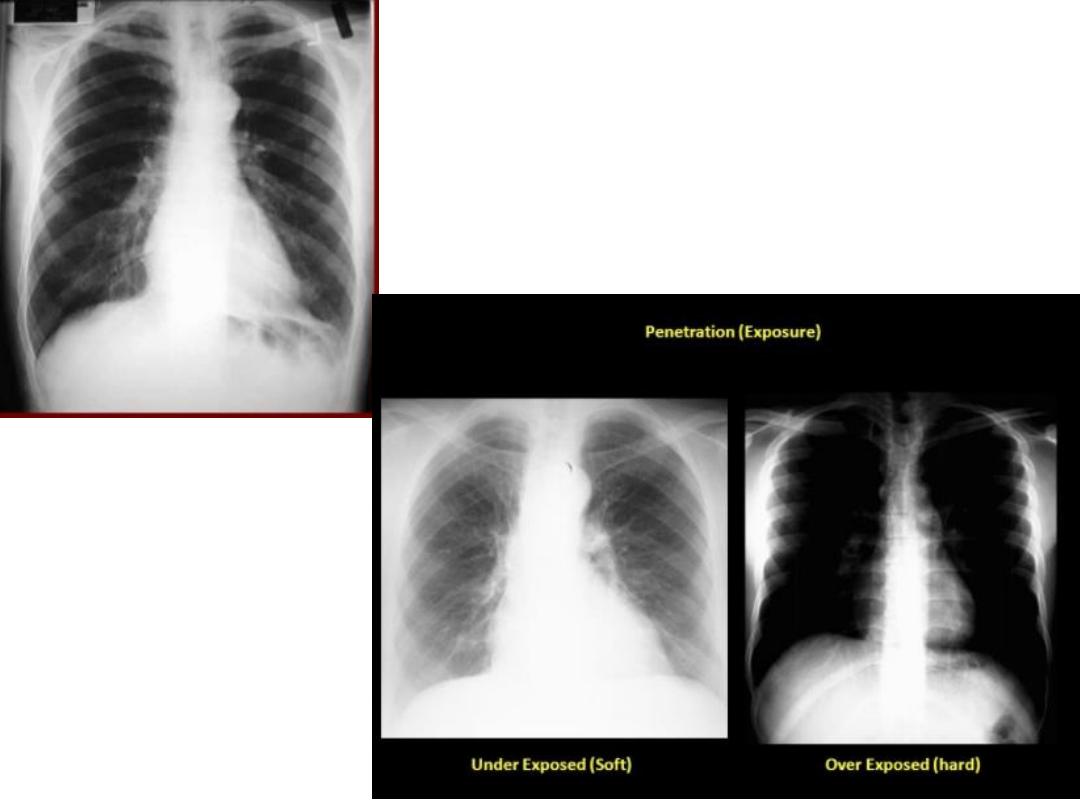
straight film is one where the medial ends of clavicles are equidistant from
thoracic verteb.
CT scan: IV CM part. Given when the purpose of examination is to visualize
med., hila or pulm. Vessels.
Images usually viewed at both lung and med. Windows.
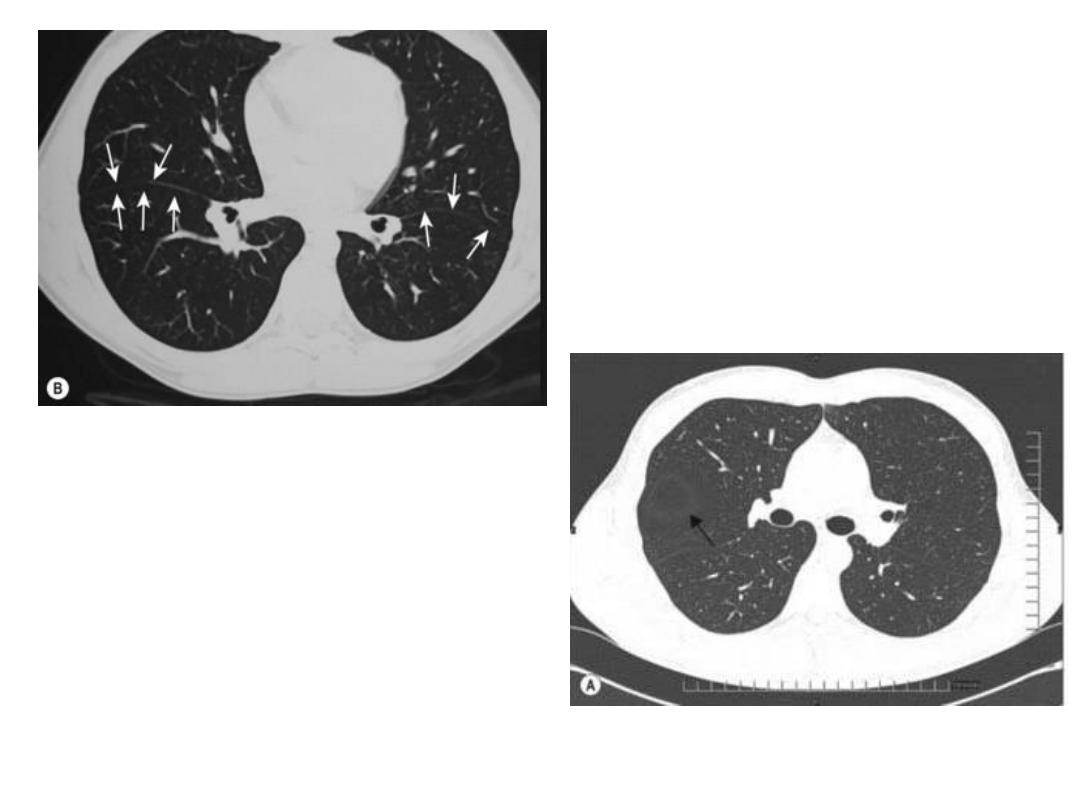
HRCT is thin section high spatial resolution CT, use for pulm. Parenchymal
dis. And bronchiectasis.
Indications of CT chest:
1- presence and extent of med. Masses and other abn.: demonstrate LNs
enlargement
Determine likely nature of med. Abn.
Distinguish vascular from non vascular structure: e.g. mass from aneurysm.
CT allows fat to be recognized e.g.: Dx fatty tumors or excluding med.
Widening due to merely excess fat deposition.
Good penetration
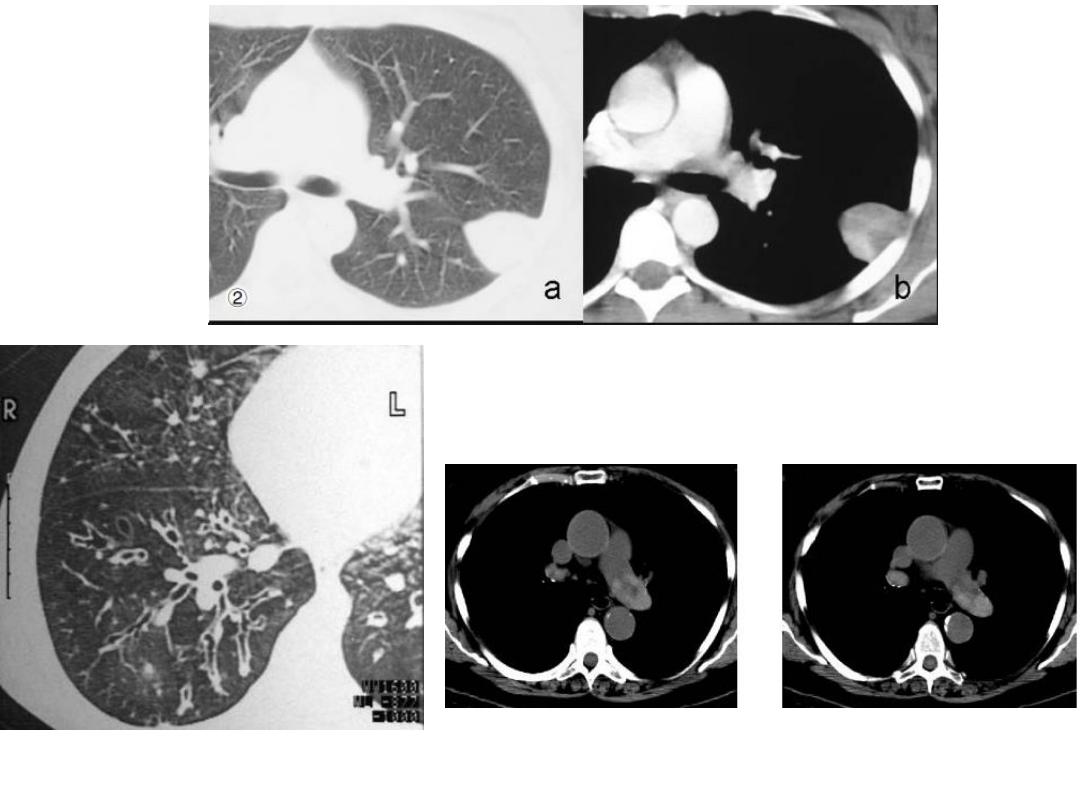
bronchiectasis
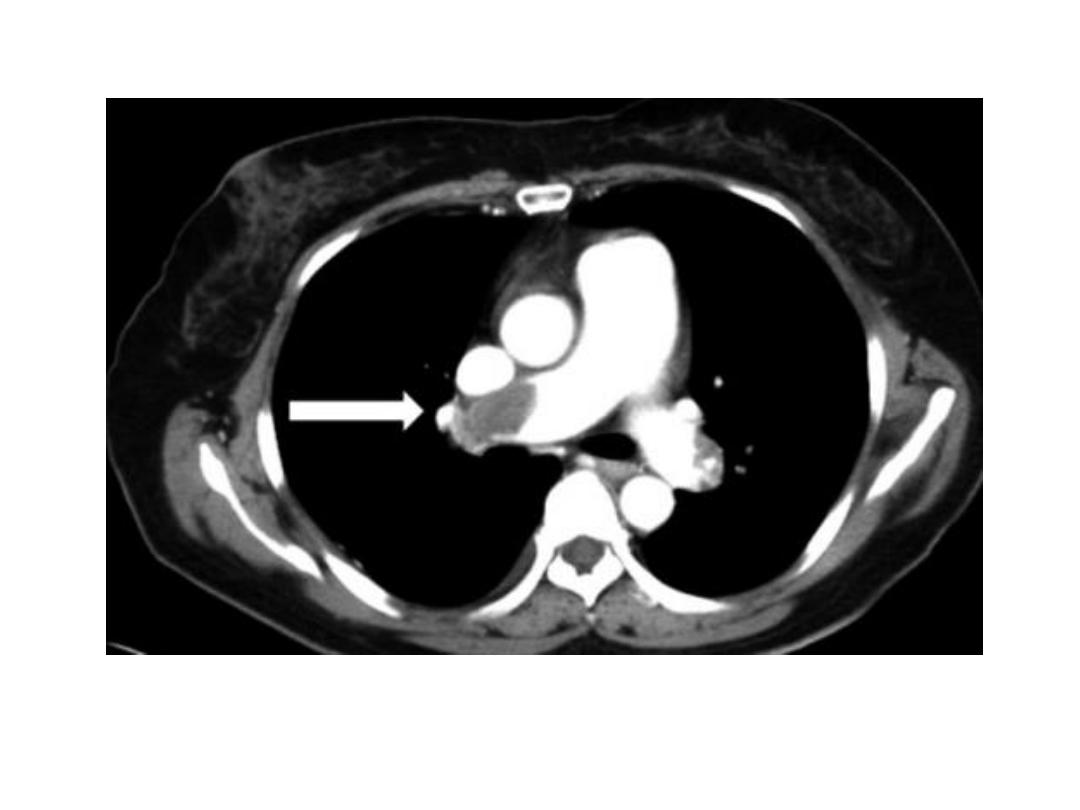
NECT with lt. pulm. A. thrombosis

2- Showing shape of intrapulmonary or pleural opacity, detecting calc. or
cavitation when plain CXR not conclusive.
3- localize opacity prior to biopsy.
4- demonstrating presence of dis. When abn. Uncertain or when CXR is
normal.
5- bronchiectasis.
6- diffuse pulm. Disease.
7- pulm. embolism.
Only structures seen normally in CT scan of chest are blood vs., fissures
and walls of bronchi(as on CXR).
Most metastasis and granulomas are located peripherally where blood
vs. are smallest.
Fissures seen as line or as avascular zone
MRI: very small role in chest, but increasingly large part in cardiac and
aortic dis.
Can be useful in lung CA when questions can not be answered by CT and
can show intraspinal Extensions of med. Neural tumors
Horizontal fissure
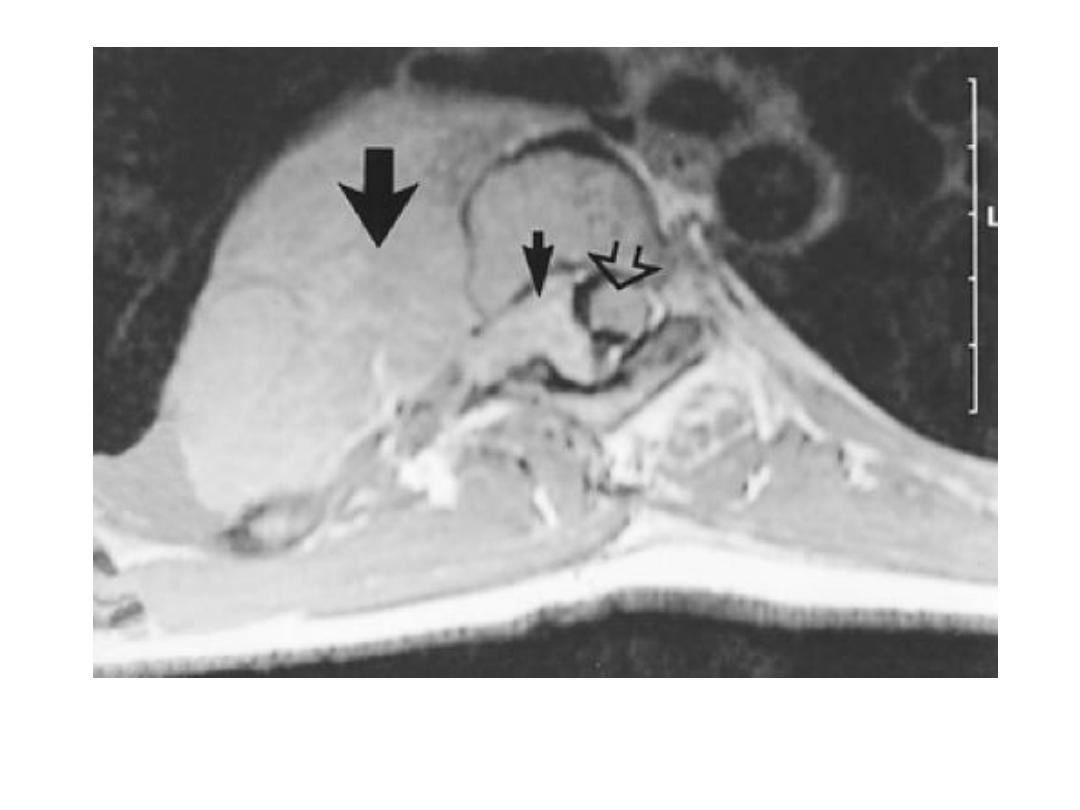
Intrathoracic
mass
intrasp.
portion
Sp. cord
Neurofibroma MRI with intrasp. Extension
Pulm. Emb.
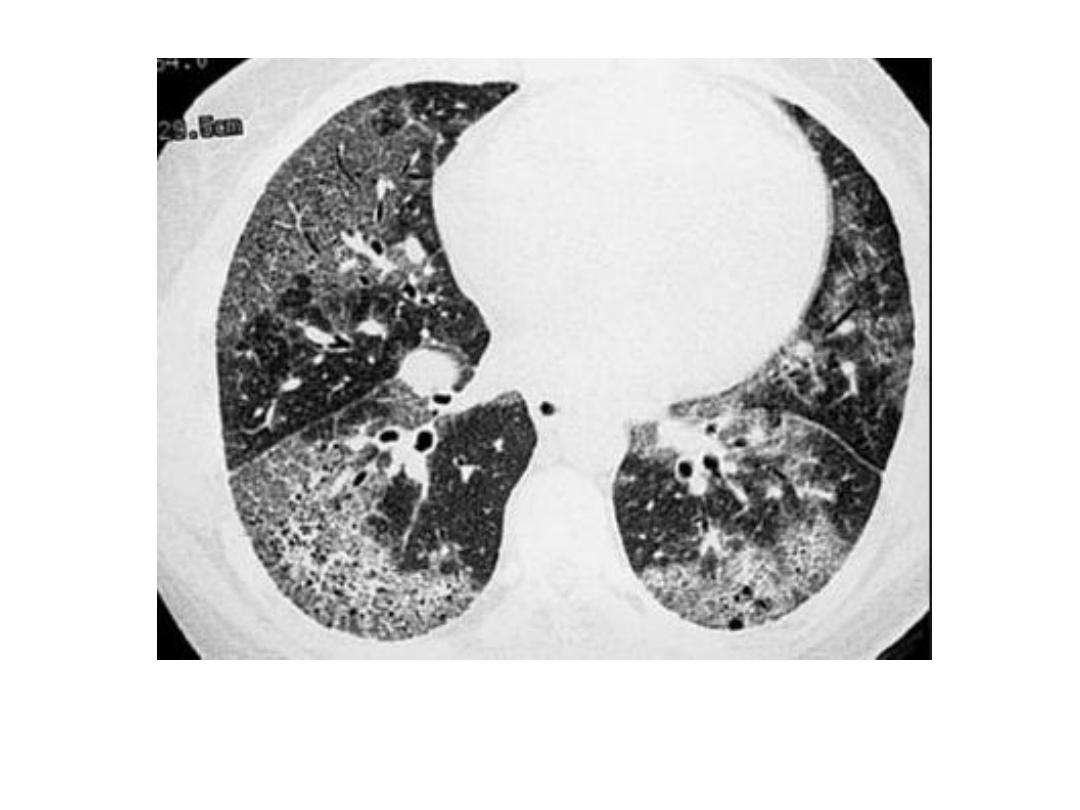
Interstial lung disease
Radionuclide imaging: the major indication is to diagnose or exclude pulm.
Emb., but this indication has been superceded by CT pulm. Angiography.
1- perfusion scan: use small particles labeled with
99m
TC inj. IV., are trapped in
pulm. Capillaries, accurately reflect blood flow.
2- ventilation scan: Patient inhales radioactive gases as Krypton – 81m.
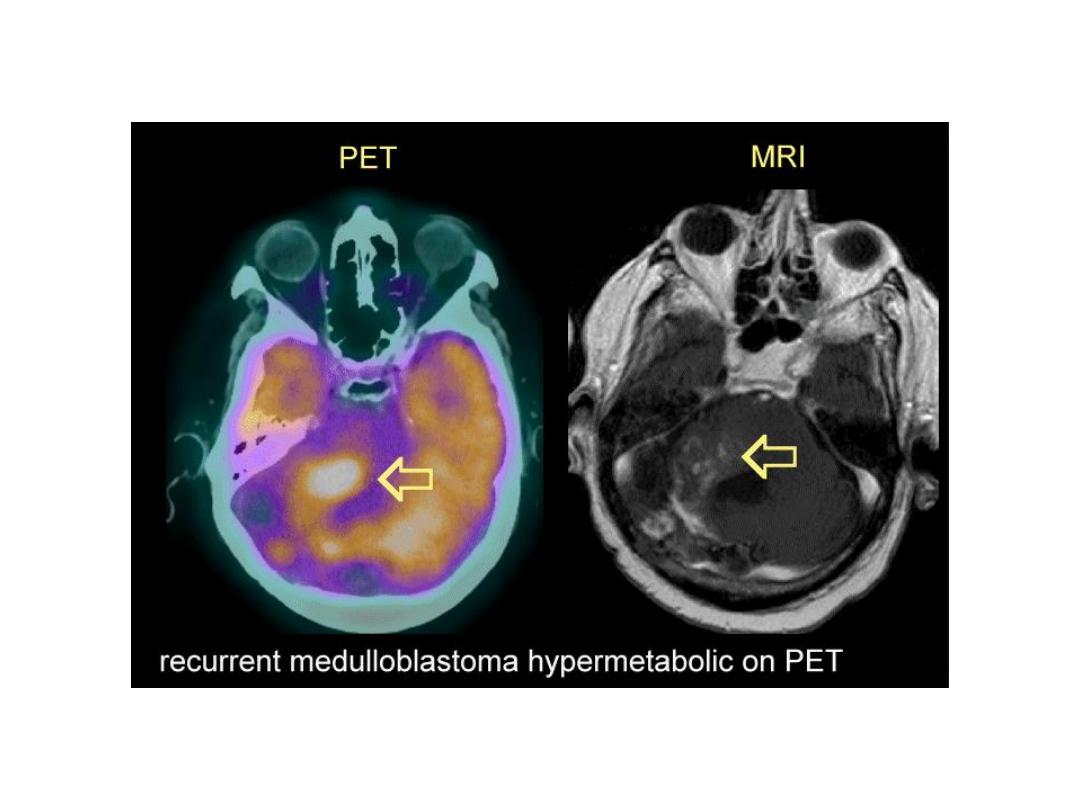
Positiron emission tomography(PET): Fluorodeoxyglucose(FDG) is taken by
number of tumors, and it is used to stage lung CA or lymphoma and
diagnose recurrent lung CA, diagnose malignant nature of SPN.
Unfortunately inflammatory conditions also conc. FDG, so it is not entirely
specific for neoplastic tissue.
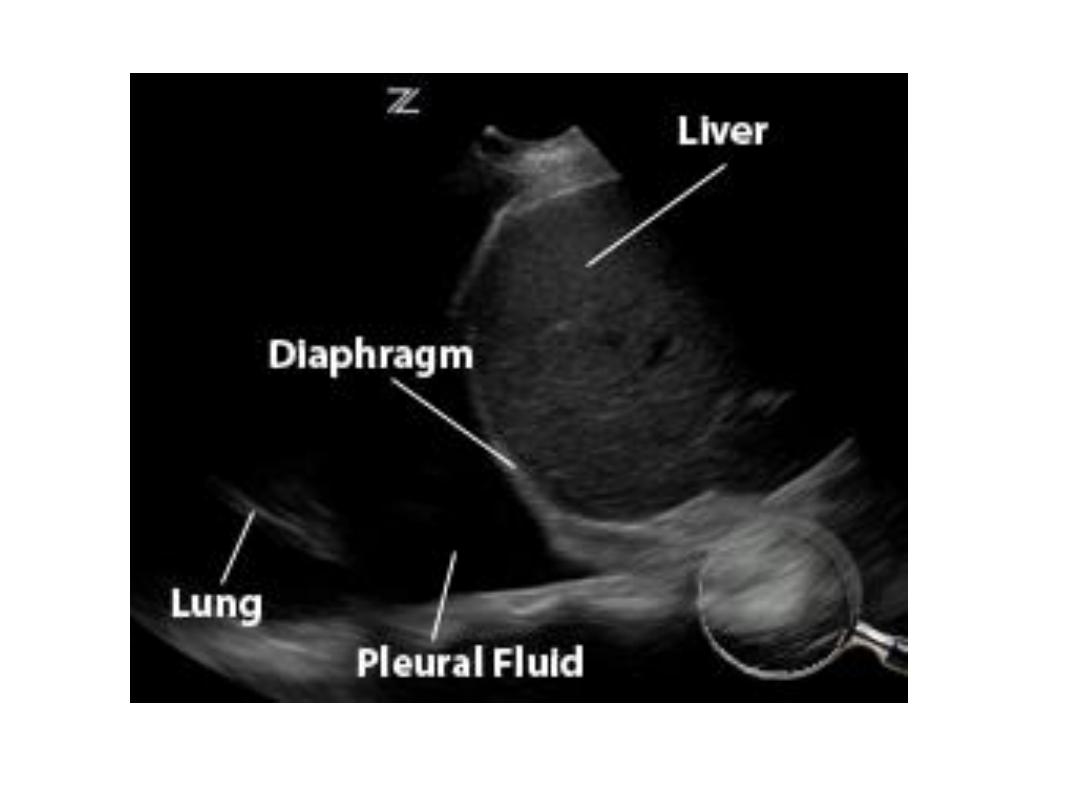
Ultrasound of chest: 1- confined to processes in contact with chest wall
notably pl. effusion, pl. masses, selected med. Masses.
2- guide needle to sample or drain pl. fluid
3- needle biopsy/ aspiration cytology of masses in contact with chest wall.
As U/S is absorbed by air in lung, so conventional U/S can not used to
evaluate processes deep to aerated lung tissue, but can possible to pass
small U/S probe through endoscope to visualize str. Immediate to
esophagus as para esoph. LNs and descending aorta.
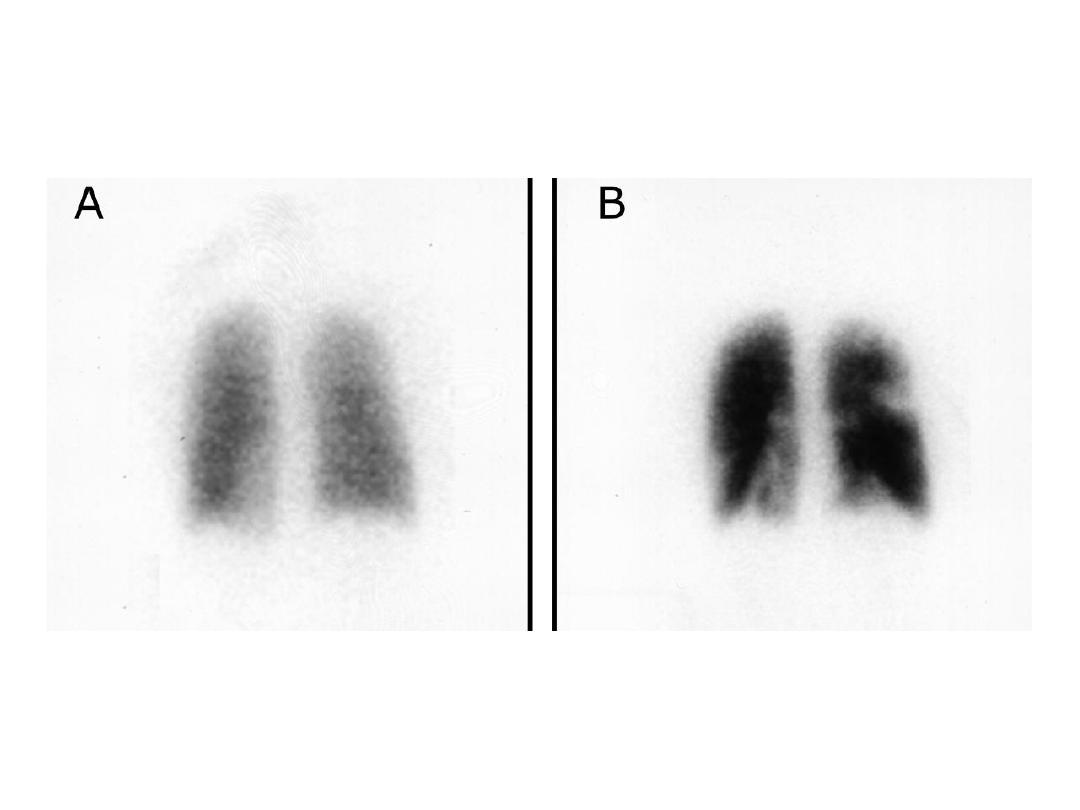
Vent.
Perfusion
Diseases with normal CXR : serious resp. disease may have normal CXR,
sometimes only possible to detected abn. By compare with prev. Or later
examinations, e.g.:
1- obst. Air way dis. As asthma, emphysema.
2- small lesions: us. Impossible to see solitary lung mass or consolidation less than 1
cm.
Even 2 – 3 cm CA lung may very difficult to identify.
Endobronchial lesions as CA, can not dx. On routine films unless cause collapse or
consolidation.
3- pulm. Emb. Without infarction even with life threatening emb.
4- infections: as in patient with miliary TB.
5- diffuse pulm. Fibrosis
6- pleural abn.: as dry pleurisy.
Small pl. fluid may be impossible to dx. On PA and lateral films
7- med. Masses: plain CXR very insensitive to dx. Med. Masses, LNs, med. Fluid
collections.
Abn. Chest: if the abn. Surrounded on all sides by aerated lung, it must arise within
the lung.
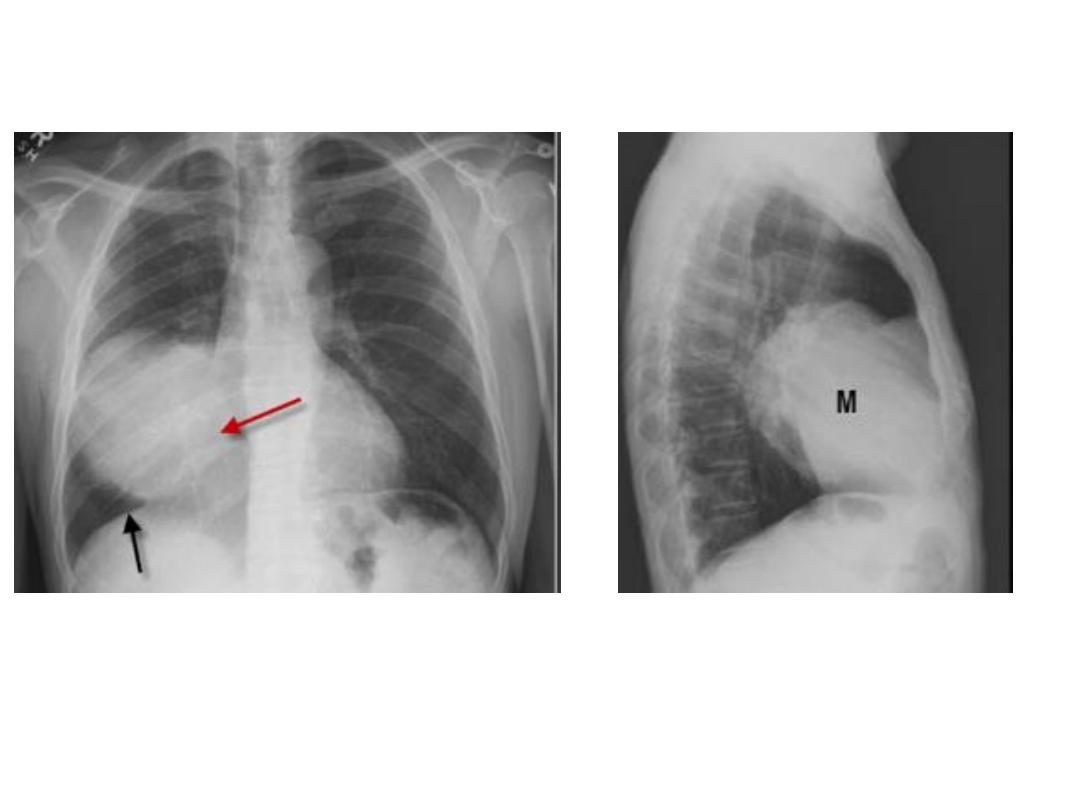
If the shadow has broad base, smooth convex border projecting into the lung, well
defined outline, so it is pl., extrapl. Or med. In origin.
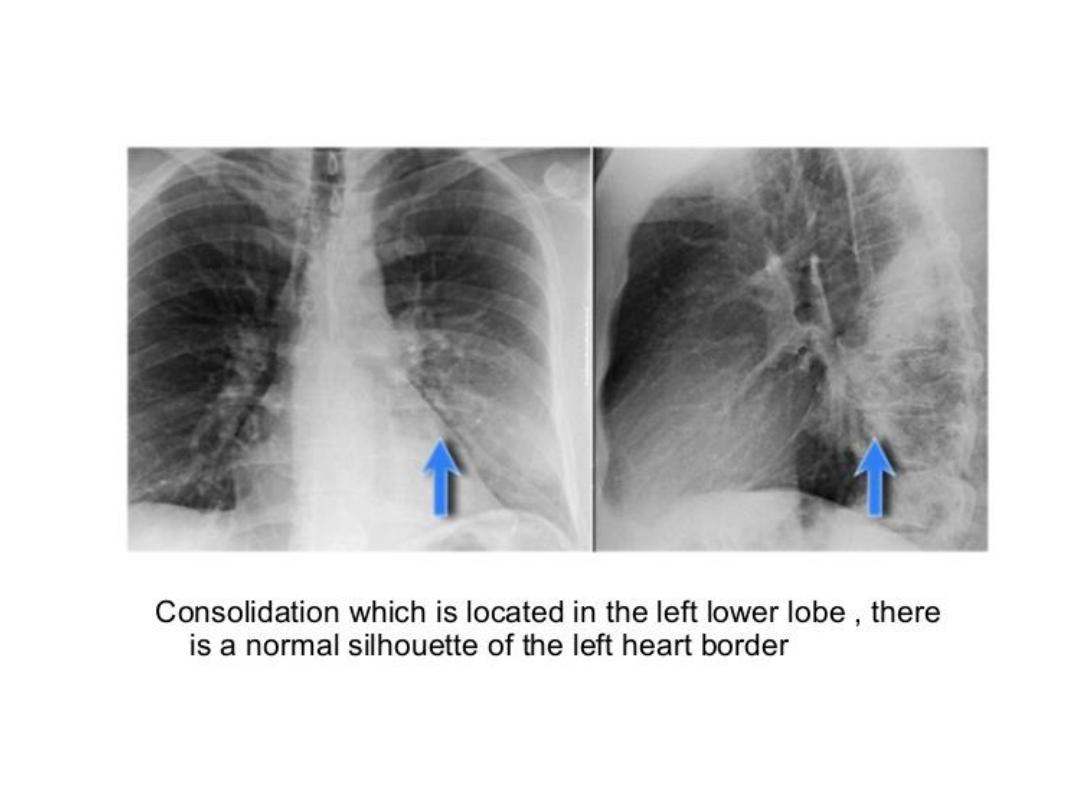
Silhouette sign: invaluable sign for localizing dis. From plain CXR.
Intrathoracic lesion touching heart, aorta or diaph. Obliterate their borders
It has two important applications:
1- localize shadow by observing which border is obliterated, e.g.: loss of heart border means the
shadow in ant. Half of the chest, loss of diaph. Outline indicate the dis. Of pl. or in lower lobes.
2- it makes possible on occasions to dx. Disorders as consolidation or collapse even when its
presence is uncertain, when it is in contact with med. Or diaph., losing their sharp outlines.
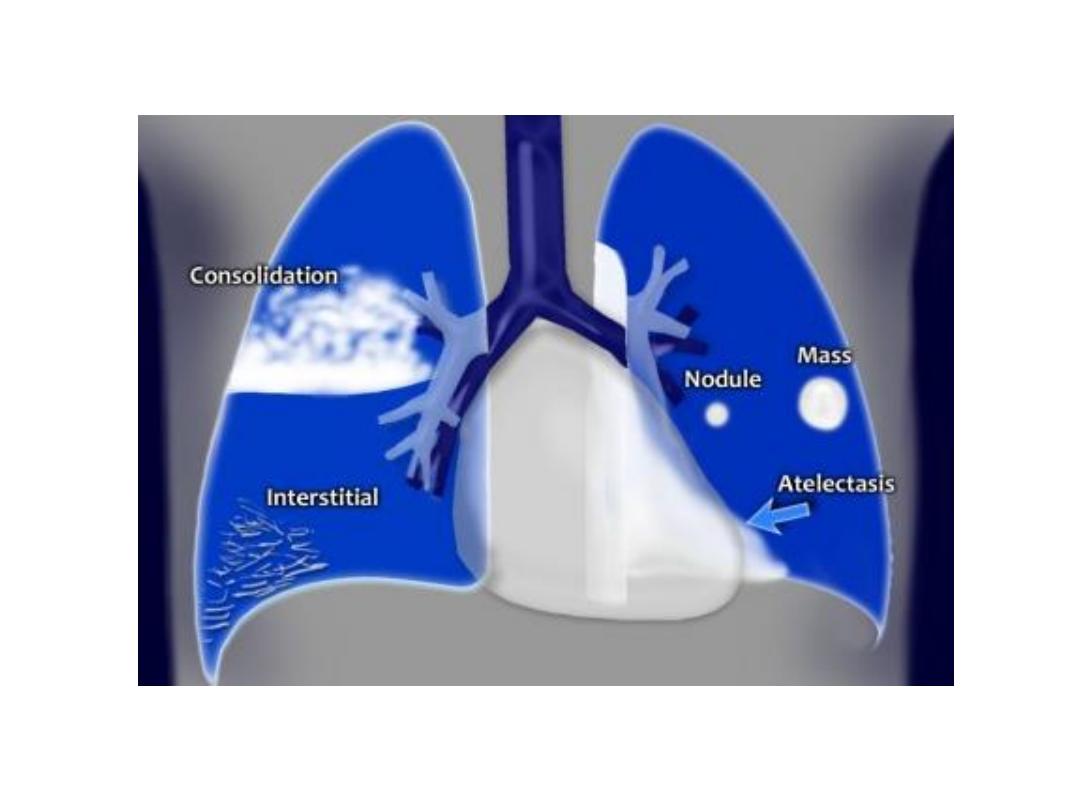
Radiological signs of lung dis. :
Air space filling: means replacement of air in alveoli by fluid or rarely by other materials.
The fluid either exudate : often called consolidation, or transudate: pulm. Edema.
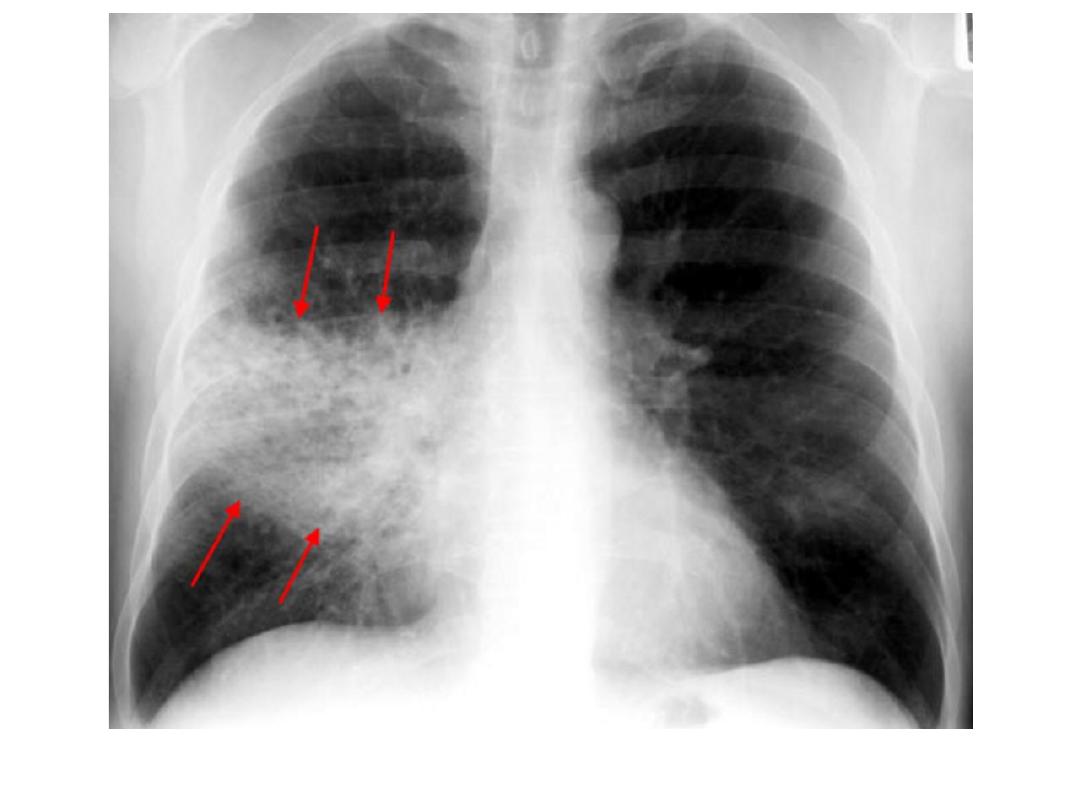
Signs of consolidation: 1- a shadow with ill defined borders except when in contact with fissure.
2- air bronchogram: if alveoli filled with fluid, the air within bronchi contrasts with fluid in adjacent
lung.
3- silhouette sign: i.e. loss of visualization of adjacent med. Or diaph. Outline.
Consolidation of a whole or majority of a lobe is virtually diagnostic of bacterial pneumonia.
Lobar consolidation produce opaque lobe except for air bronchogram.
Patchy consolidation: one or more patches of ill defined shadowing, is usually due to: pn.,
infarction, contusion, and immunological disorders.
Cavitation(abscess formation) : within consolidated areas in the lung may occur with many bact.
And fungal infections, occasionally in infarction and Wegener granulomatosis.
Abscess formation only recognizable once there is communication with bronchial tree, allowing
liquid Centre to coughed up and replaced by air, the air then seen as transradiancy within
consolidation, and air fluid level may be present.
CT is better and more sensitive than plain CXR for cavitation.
Rt. Ant. Med. Mass silhouette rt. Cardiac border
Pneumonia, with air bronchogram, partly ill defined, silhouette positive
bronchopneumonia
Cavity + air fluid level
CT lung cavity
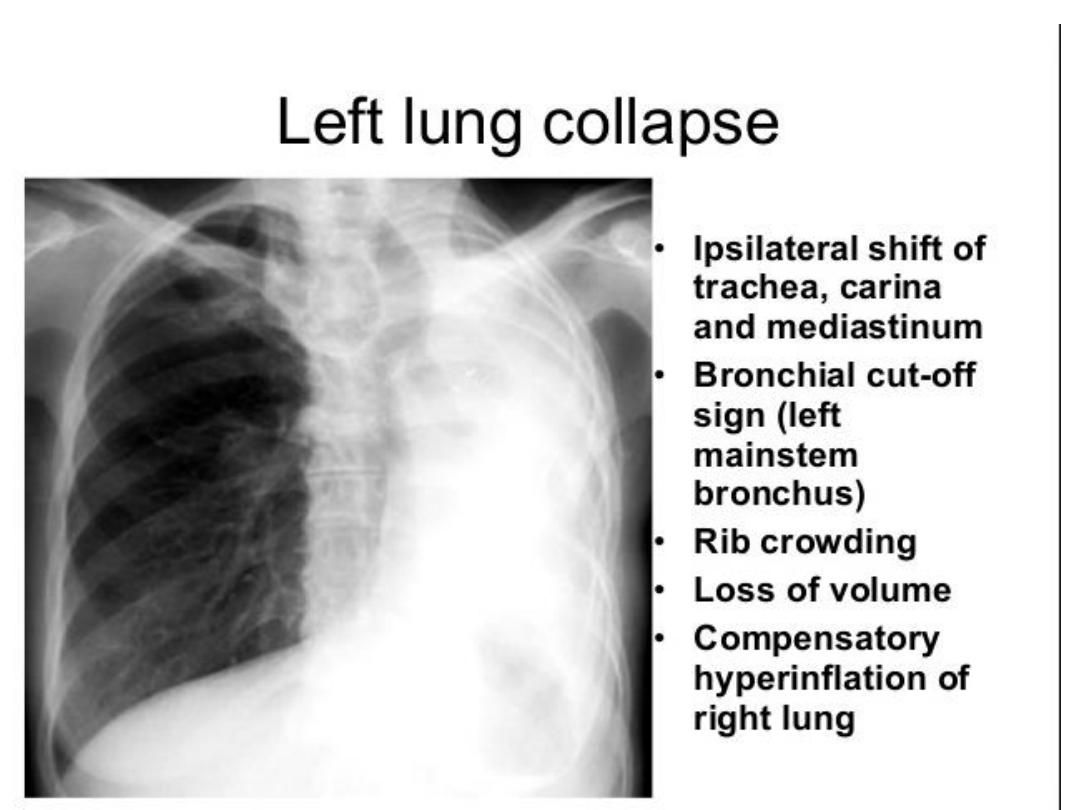
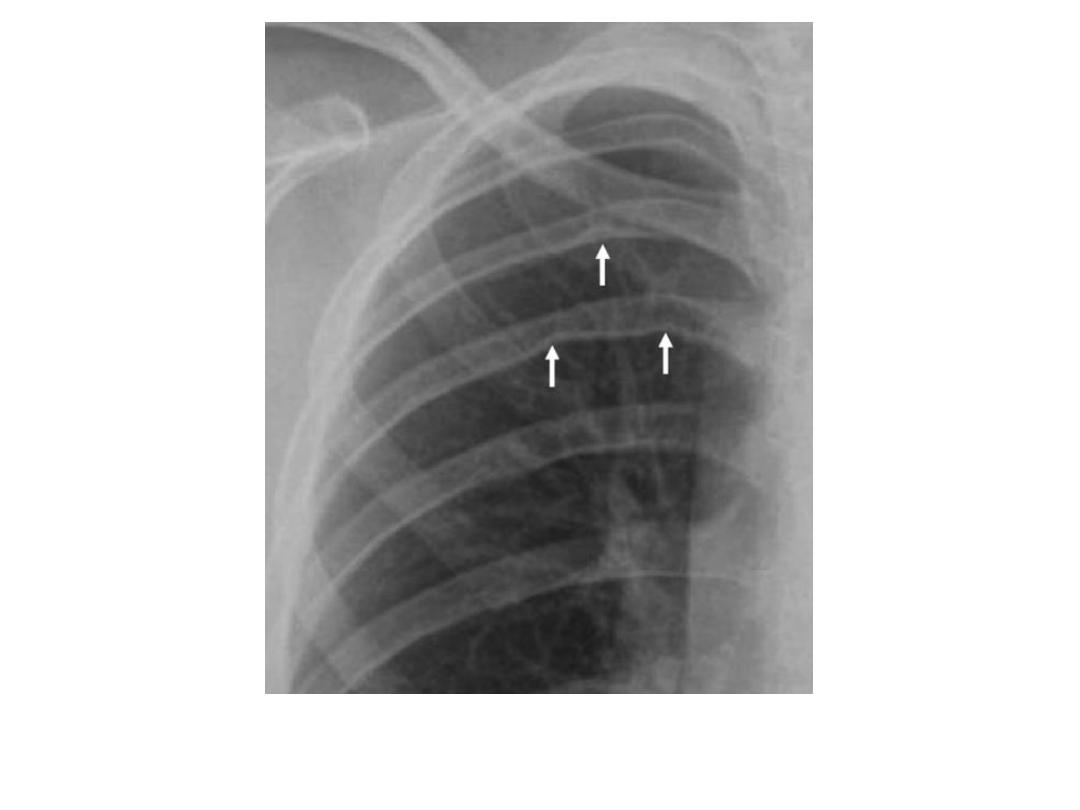
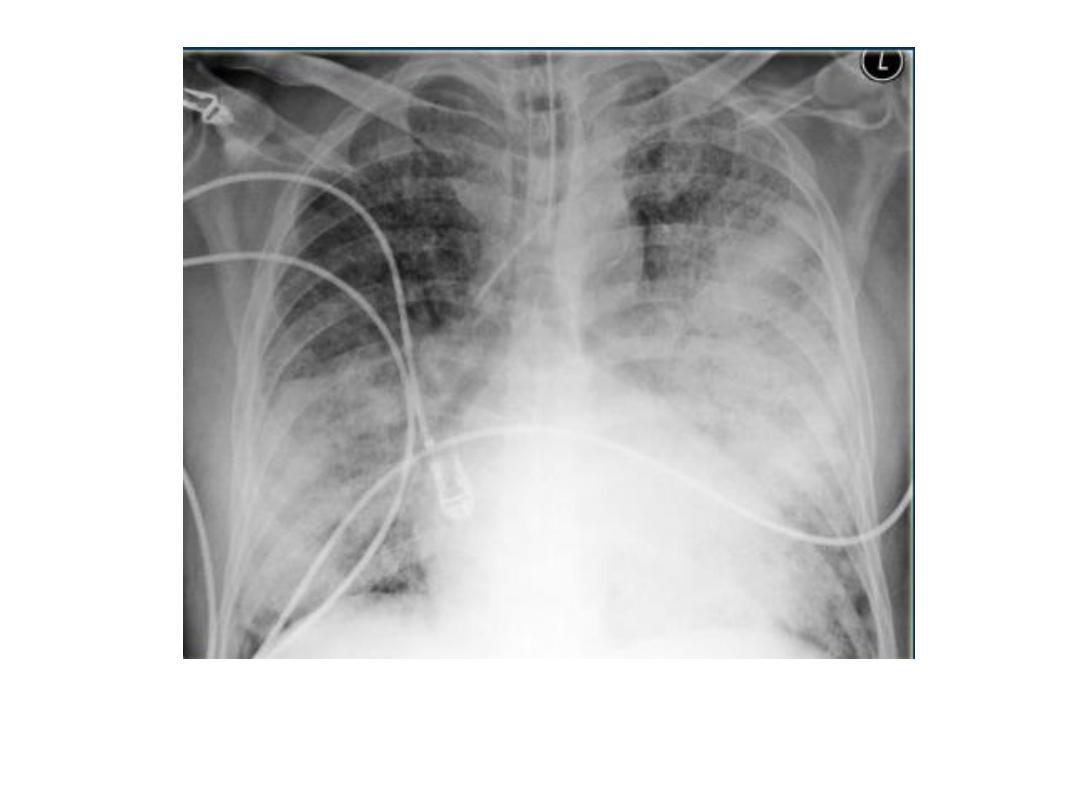
Pulmonary collapse(atelectasis): loss of volume of a lobe or lung, common causes: bronchial
obst., pneumothorax or pl. effusion, linear(discoid) atelectasis.
Collapse caused by bronchial obst.: occurs due to air can not get into the lung in sufficient amount
to replace the air absorbed from alveoli.
Signs of lobar collapse:
1- displacement of structures
2- shadow of collapsed lobe/ consolidation, almost invariably accompanies lobar collapse.
3- Silhouette sign: A- help to dx. Lobar collapse when resulting shadow is difficult to appreciated. B-
decide which lobe is collapsed.
Collapse of ant. Located lobes, upper and middle, obliterate portions of med. And heart outlines,
whereas collapse of lower lobes obscure diaph. And descending aorta.
commoner causes of lobar collapse: 1- bronchial wall lesions: us. Primary CA, occasionally others
as carcinoid.
2- Intraluminal occlusion: us. FB. Or retained mucus plugs, part. Postop., asthmatic or unconscious
pat., patient with artificial vent.
3- invasion or compression by adjacent malig. Tumors, rarely enlarged LNs.
When lobe collapse, the unabsorbed lobe(s) on the side of collapse undergo compensatory
expansion, the displaced fissure seen as well defined boundary to airless lobe, the med. And
diaph. May move towards collapsed lobe.
With collapse of whole one lung, the entire hemithorax is opaque, and there is substantial med.
And tracheal shift.
CT shows lobar collapse very well, but rarely necessary simply to dx. Collapsed lobe.
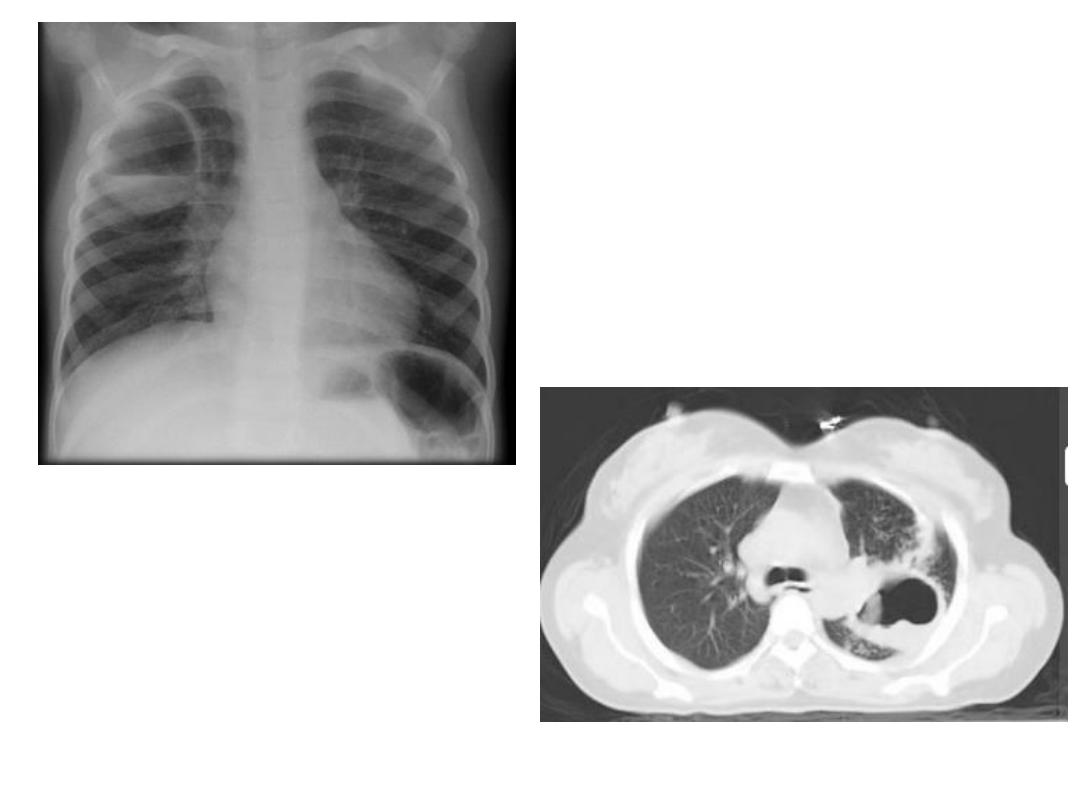
Collapse with pneumothorax or pl. effusion : presence of air or fluid in pl. cavity allows lung to
collapse.
Linear(discoid)atelectasis : is not secondary to bronchial obst., but due to hypoventilation,
commonest cause is postop. Or post traumatic pain. The result is horizontally oriented band or
disc of collapse
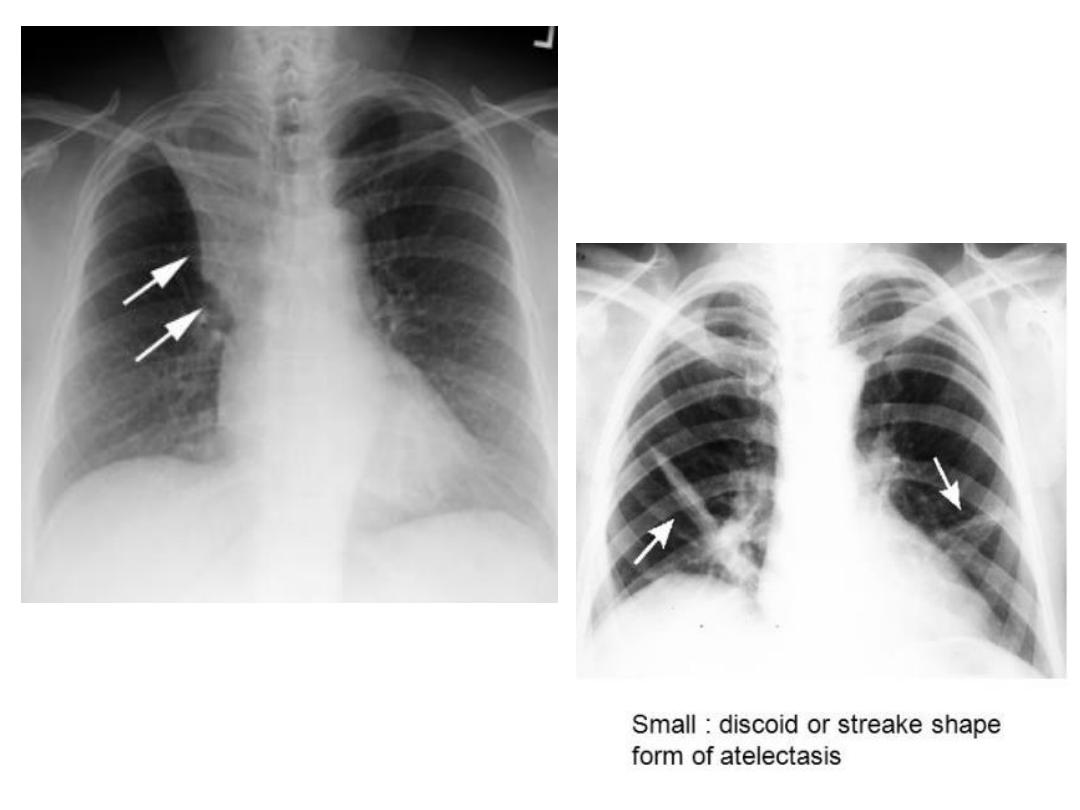
RUL collapse +Golden S sign