• Line or band like shadows: all lines shadows within the lung are abnormal except
fissures and walls of large central bronchi:
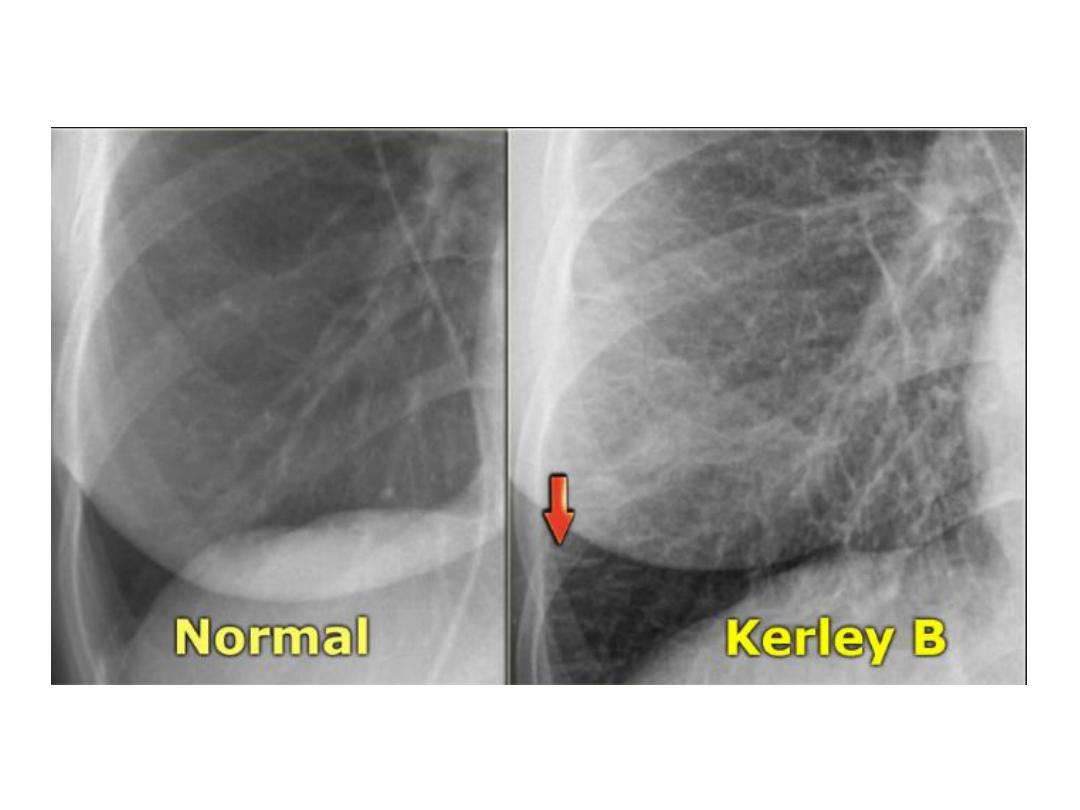
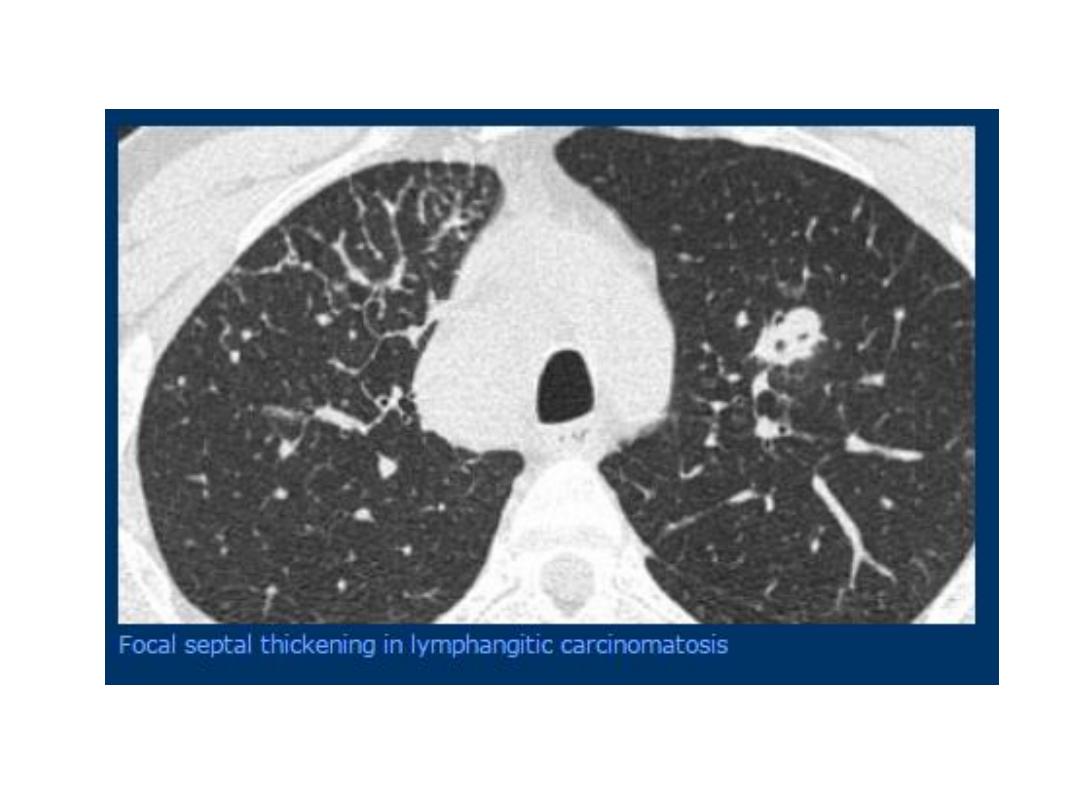
1- septal lines: the most important one.
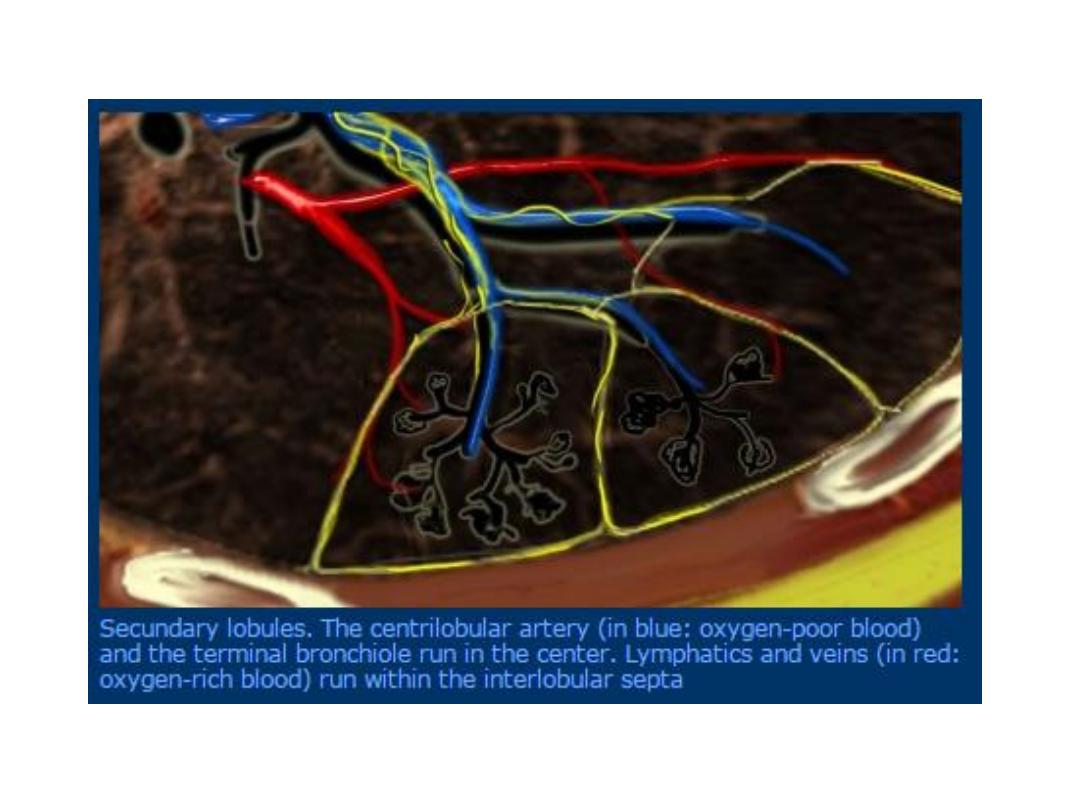
• Interlobular septa are connective tissue planes containing lymph vessels, are
normally invisible, only greatly thickened septa can be seen on CXR.
• Septal lines are much thinner than pulm. Blood vs.
• On plain CXR septal lines see: Karely B lines horizontal lines, never more than 2
cm in length, best seen at periphery of lung, unlike blood vs. often reach edge of
lung.
• mild thickening of minor interlobular septa are readily identified by CT.
• Two imp. Causes of thickened interlobular septa:
pulm. Edema
and
lymphangitis
carcinomatosa
.
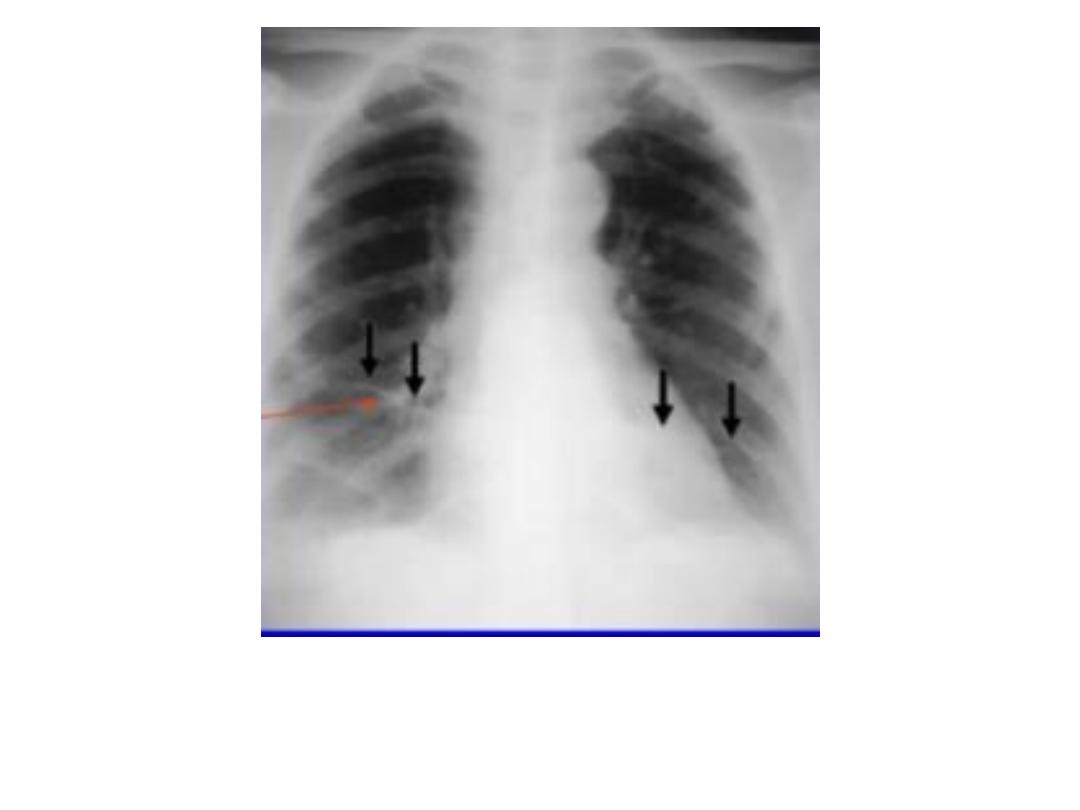
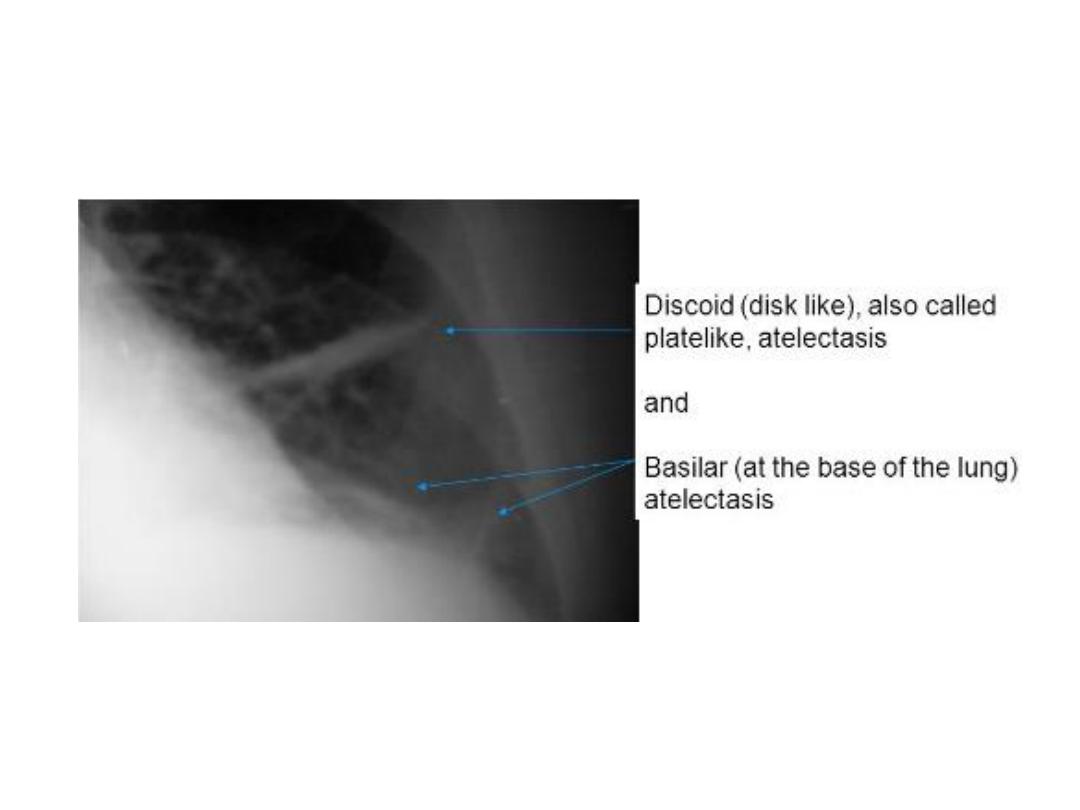
2- pleuropulmonary scars and linear(discoid) atelectasis: are common causes of line
and band like shadows.
• Linear scars are due to previous infection or infarction, usually reach the pl. and
often associated with visible pl. thickening.
• Linear(discoid) atelectasis: horizontally oriented bands or discs of collapse.
3- emphysematous bullae: bullae(blebs) : are air spaces devoid of blood vs., may be
rounded and traversed by thin line shadows, have few if any normal vs. within
them.
4- the pleural edge of pneumothorax: seen as line, approximately parallel with chest
wall, no lung vs. seen beyond pl. line.
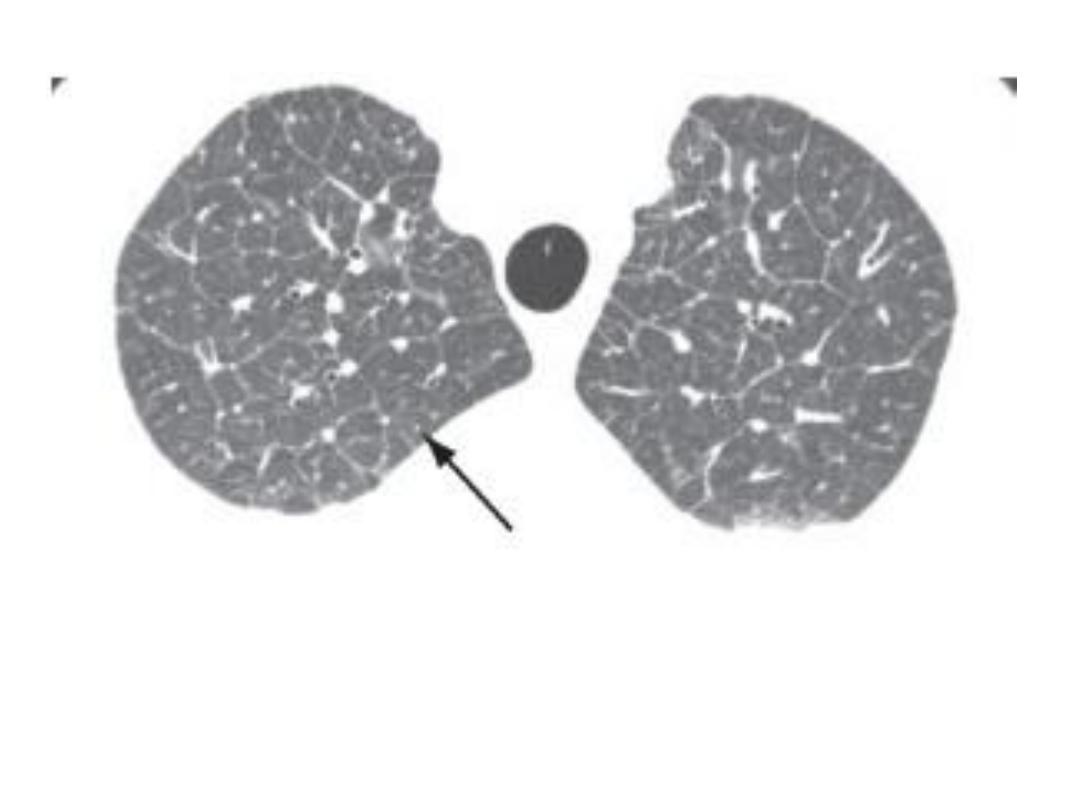
CT scan, thickening interlobular septa
Pulm. Scars in lung infarction
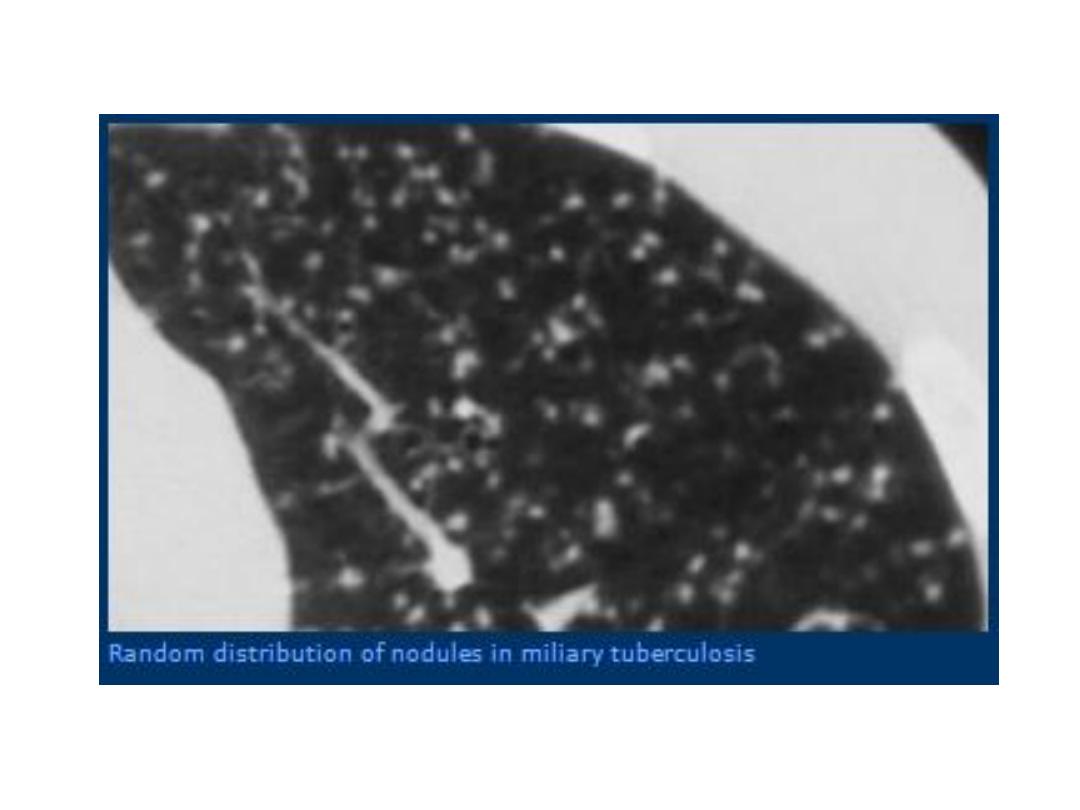
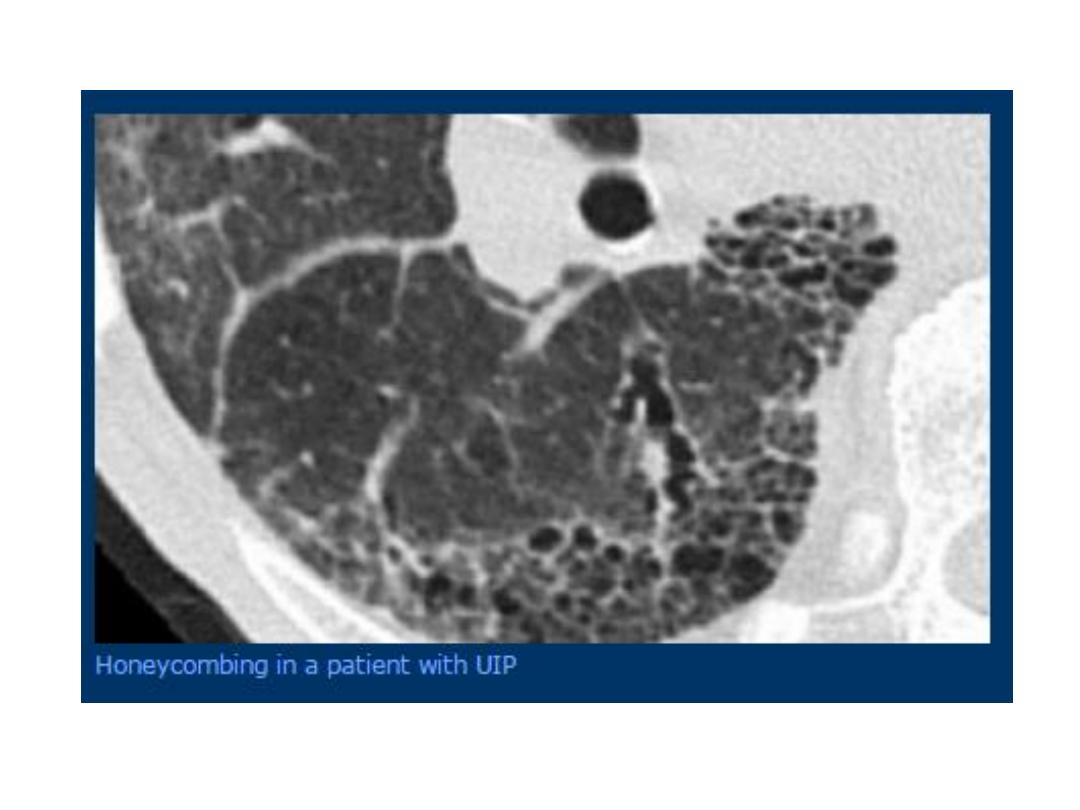
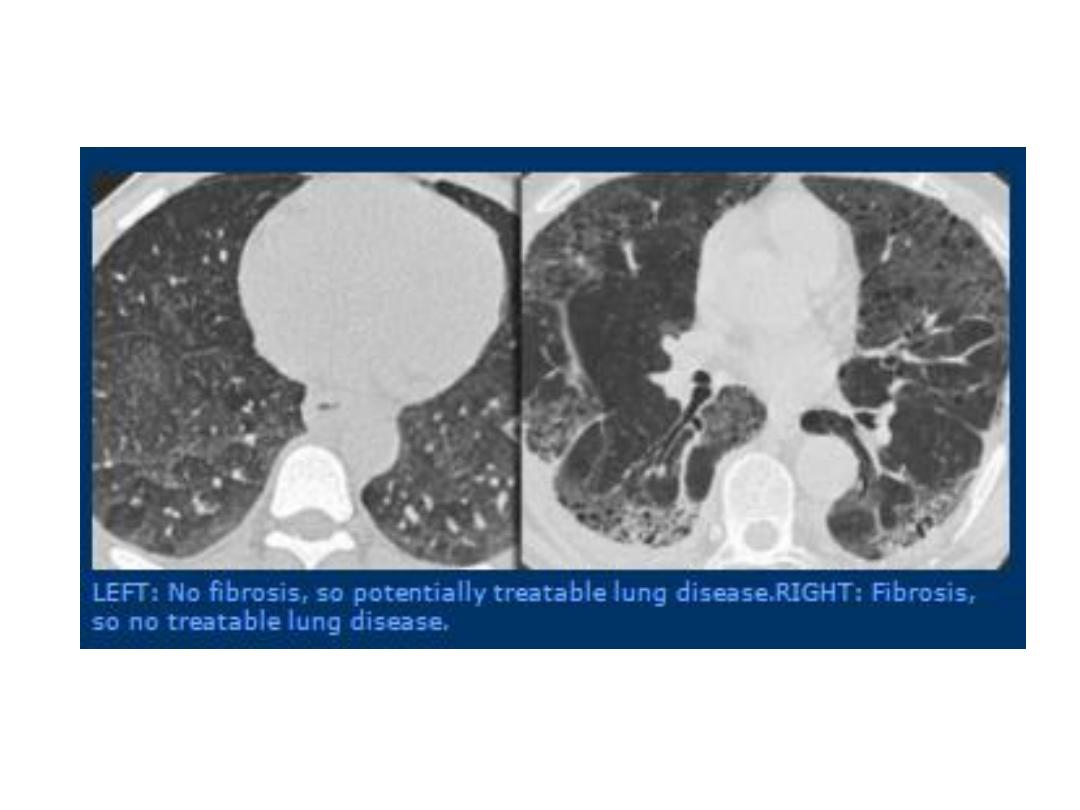
• Widespread small pulmonary shadows: CXR with widespread small(2-3) mm
pulm. Shadows often present a diagnostic problem, terms applied: mottling,
honeycomb, fine nodular, reticular and reticulonodular shadows.
• Nodular shadows: discrete small nodules
• Reticular shadows: net like pattern of small lines.
• Reticulonodular shadows: when both mentioned patterns present.
• Look carefully at areas between ribs, where lung free of overlying shadows.
• The normal vs. pattern is a branching system which connect up in orderly way, vs.
are larger centrally and smaller peripherally.
• Vs. seen end on app. Small nodules, but no bigger than vs. in immediate vicinity and
their number correspond to expected number of vs. in that areas.
• No visible vs. in outer 1 – 2 cm of lung.
• Imp. Sign is that the abn. Shadows obscure the adjacent vs. and borders of med. And
diaph. May be less sharp than normal .
• When abn. Diffuse shadowing is present or suspected, the next step is high
resolution CT(HRCT): 1- to determine the precise pattern and distribution.
2-other abn. With in chest seen.
• Multiple ring shadows larger than 1 cm are diagnostic of bronchiectasis, which
dilated thick walled bronchi.

Nodular shadowing
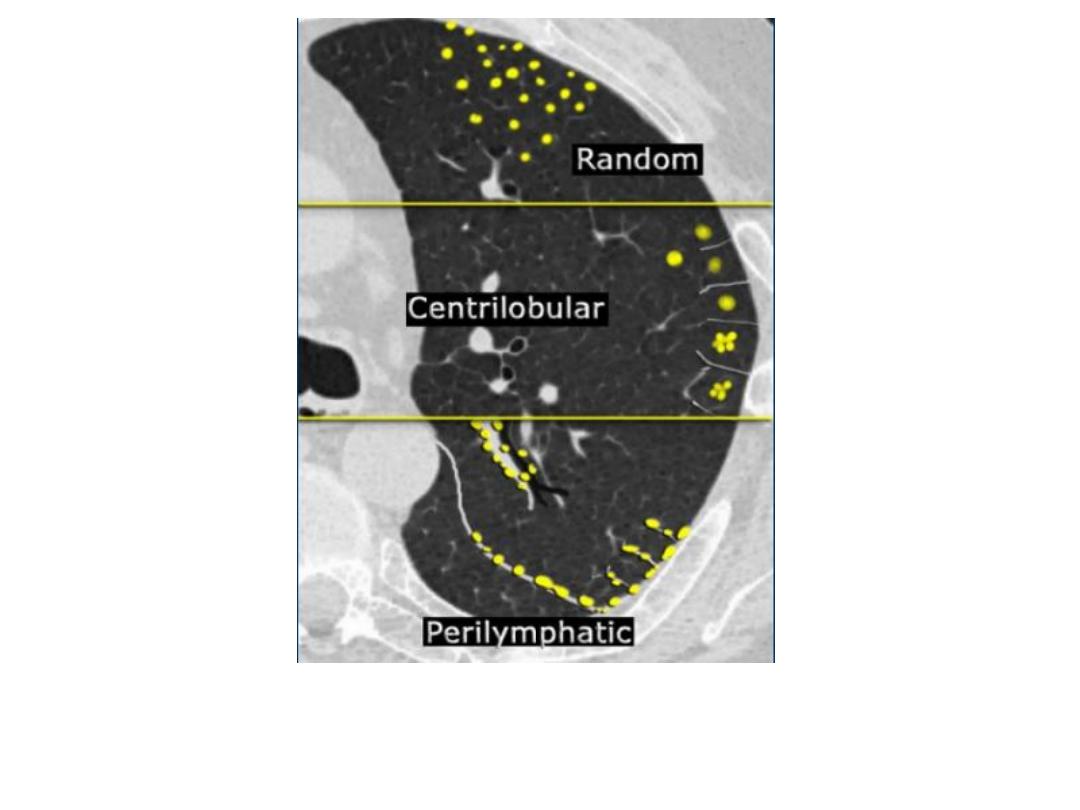
HRCT nodular shadowing

Bronchiectasis
• Increase transradiancy of the lungs : generalize increase
transradiancy of the lungs is one sign of emph.
• When only one hemithorax app. More transradiant than normal:
1- compensatory emph. : When a lobe or lung is collapsed or excised and
remaining lung expand to full the space.
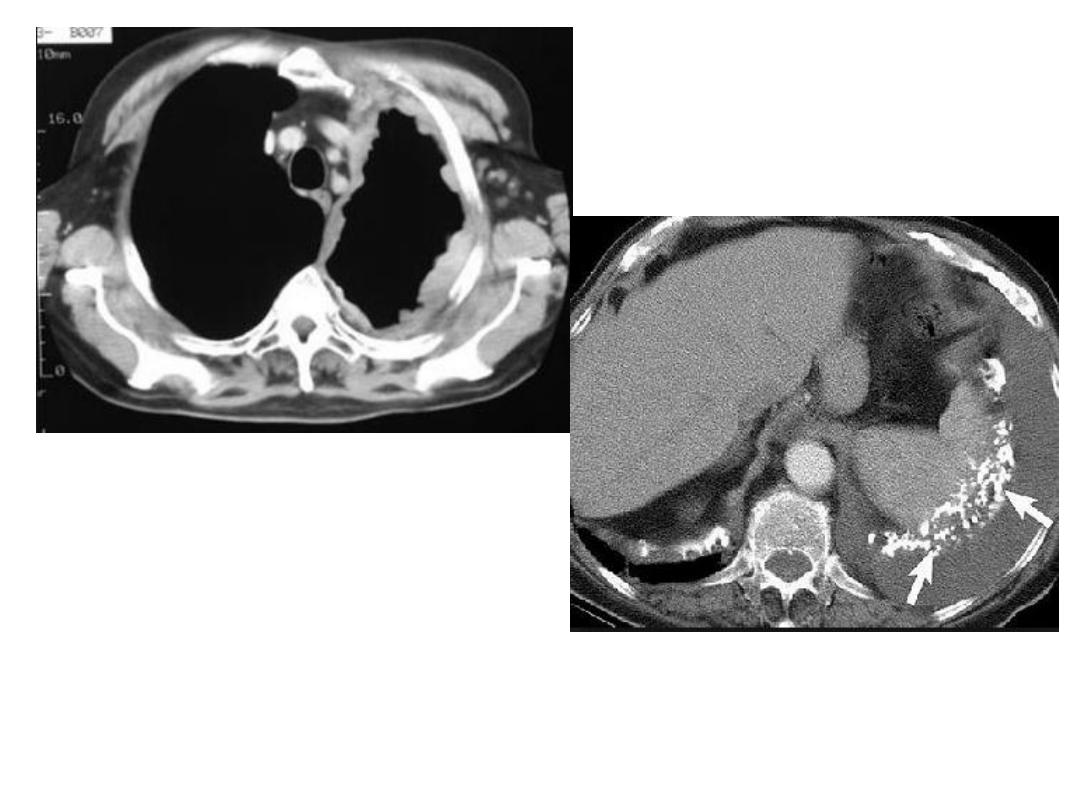
2- pneumothorax: Dx. depends on visualization of lung edge with air
peripheral to it, and the space not contain any vs.
3- reduction in chest wall soft tissues e.g. mastectomy .
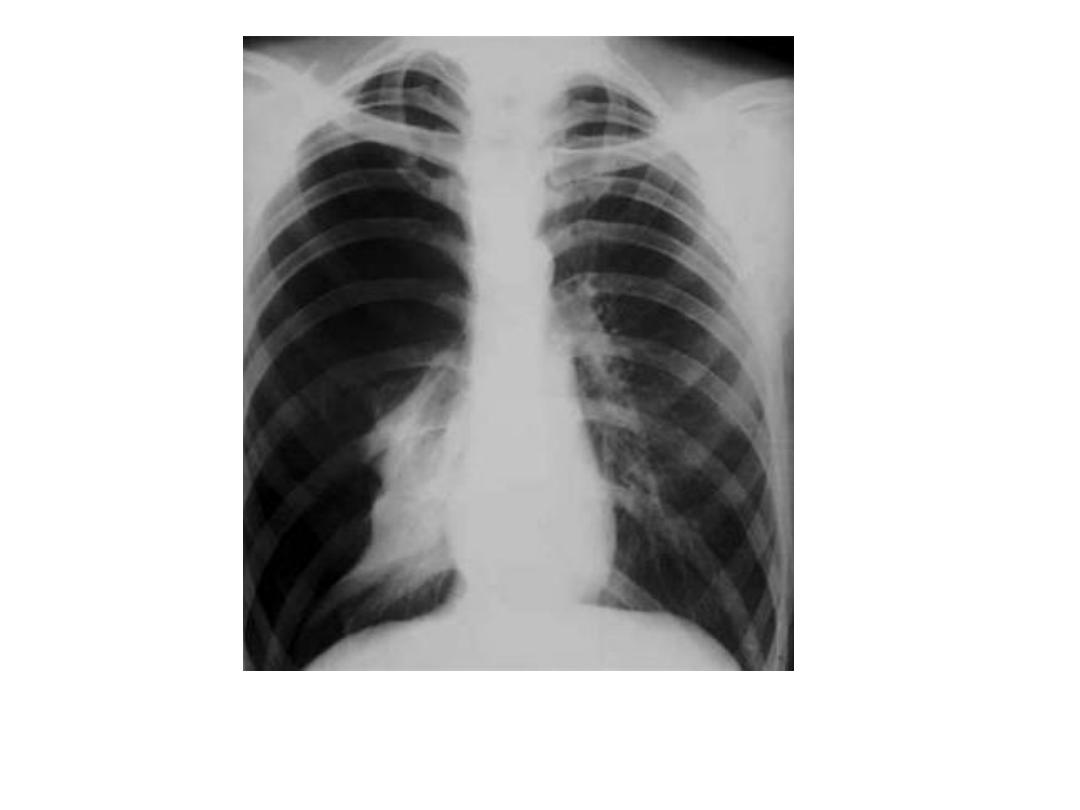
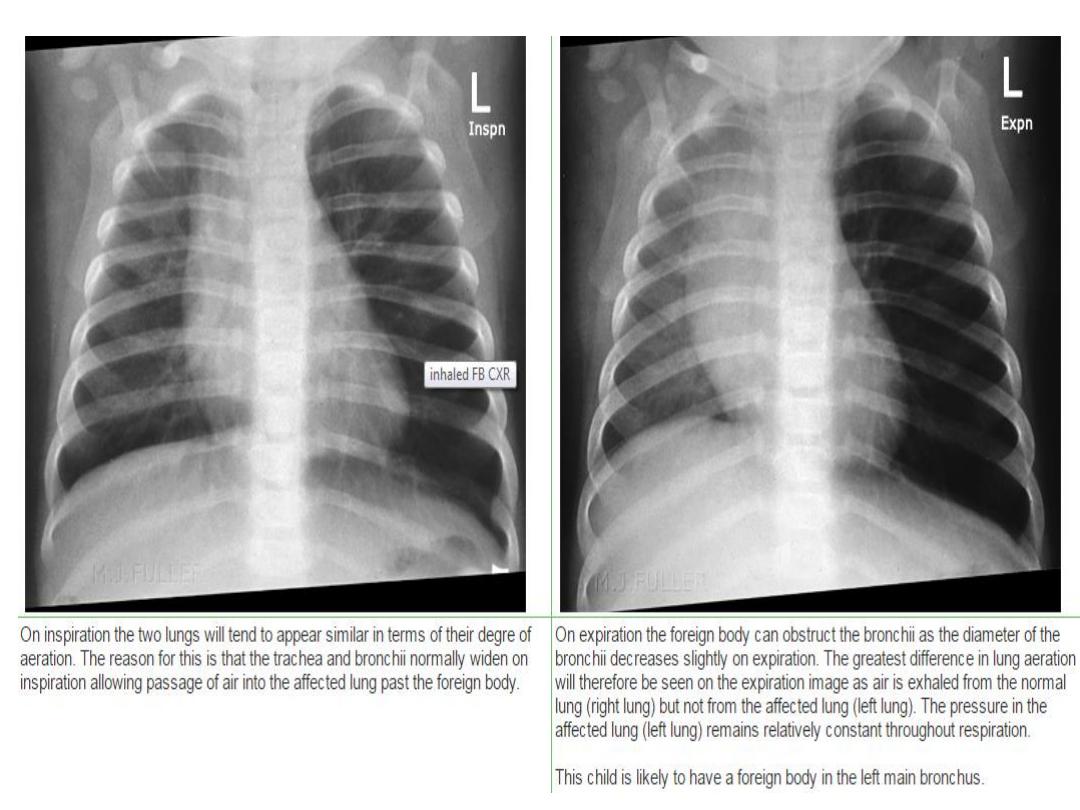
4- air trapping due to central obst. : most obst. Lesions in major bronchus
lead to lobar collapse, occasionally, part., when inhaled FB, a check-
valve mechanism may lead to air trapping.
• Inhaled FB are commonest in children, us. Lodged in major bronchus,
often CXR is normal, but sometimes the affected lung become abn.
Transradiant and heart is displaced to opposite side on expiration.
Pneumothorax

Left mastectomy
• Pleural effusion : it may lie free with in pl. cavity, in which fluid falls to most
dependant part of the pl. and assumes a shape dependant on thoracic cage and shape of
underlying lung.
• Pl. effusion may be loculated by pl. adhesions, although occurs in all types of effusion,
it is a particular feature of empyaema. Such loculations may be at periphery of lung or
with in fissures between the lobes.
• Loculated pl. effusion may simulate lung tumor on CXR.
• Causes: 1- infection: pl. effusion due to pneumonia (pn.) are on the whole small and pn.
Us.. The dominant feature on CXR.
• Large pl. effusion with pn. Often indicate empyaema.
• In some cases of TB, the pl. effusion is the only visible abn. And effusion may be large.
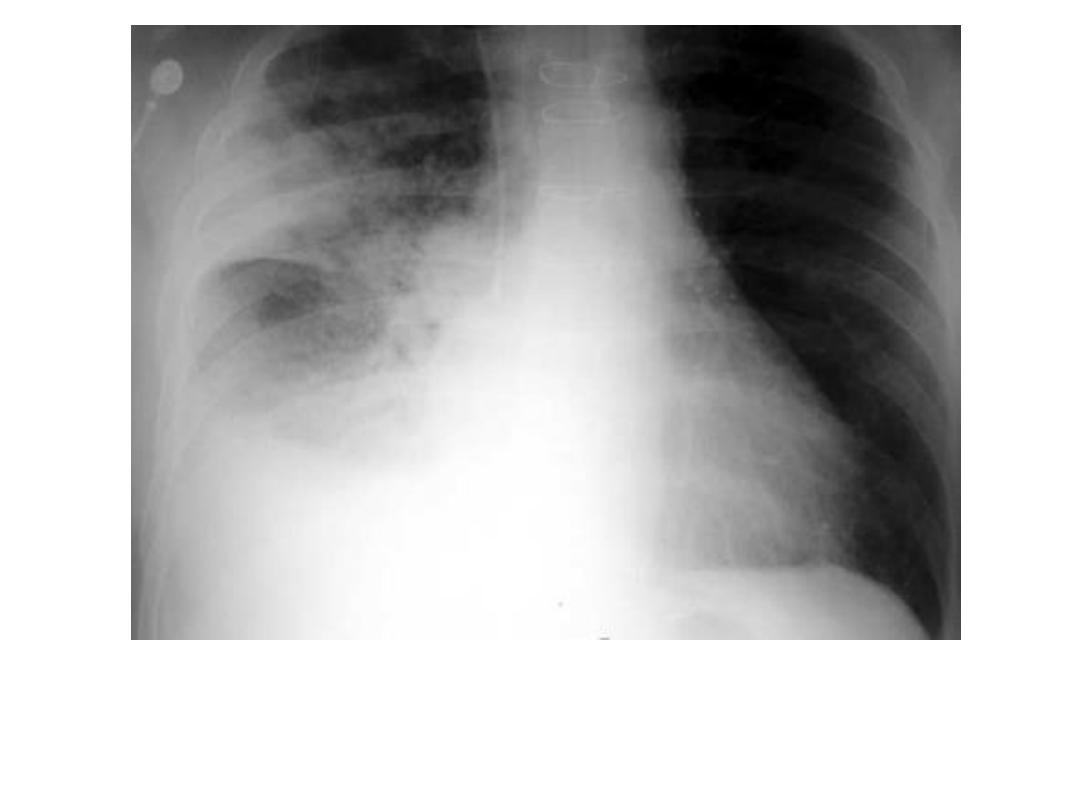
2- subphrenic abscess: nearly always accompanied by pl. effusion.
3- malignant neoplasm: pl. effusion seen with pl. metastasis, but unusual to see pl. deposits
themselves on plain CXR, but occasionally seen on CT, MRI or U/S as nodular masses
or mass like pl. thickening.
• Malignant effusion freq. large.
• If effusion due CA bronchus or malig. Mesothelioma, other signs of primary dis. Is us.
But not always evident.
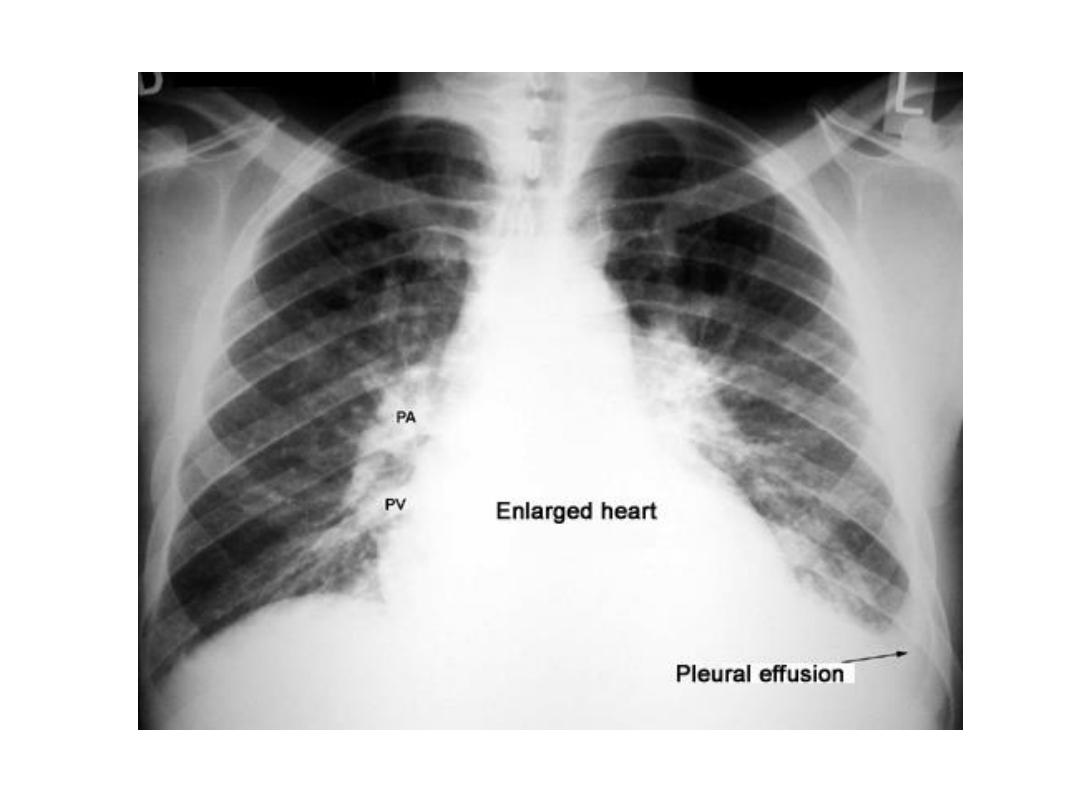
4- cardiac failure : small bilateral pl. effusion seen freq. in acute LVF. Larger pl. effusion
may se seen in longstanding CHF.
• The effusion us. Bilateral, often larger on the rt.
• Other signs of HF: alteration is size and shape of heart, pulm. Edema, signs of pulm.
Venous hypertension, are us. Visible.
5- pulmonary infarction : pulm. Emb. Cause pulm. Infarction may cause pl. effusion,
which us. Small ass. With shadow of pulm. I.
6- collagen vascular disease : pl. effusion either uni or bilateral, it may be the only abn.
Feature on CXR.
7- nephrotic syndrome, renal failure and ascities : are ass. With pl. effusion.
CXR findings : it is same whether the fluid exudate, transudate, pus or blood.
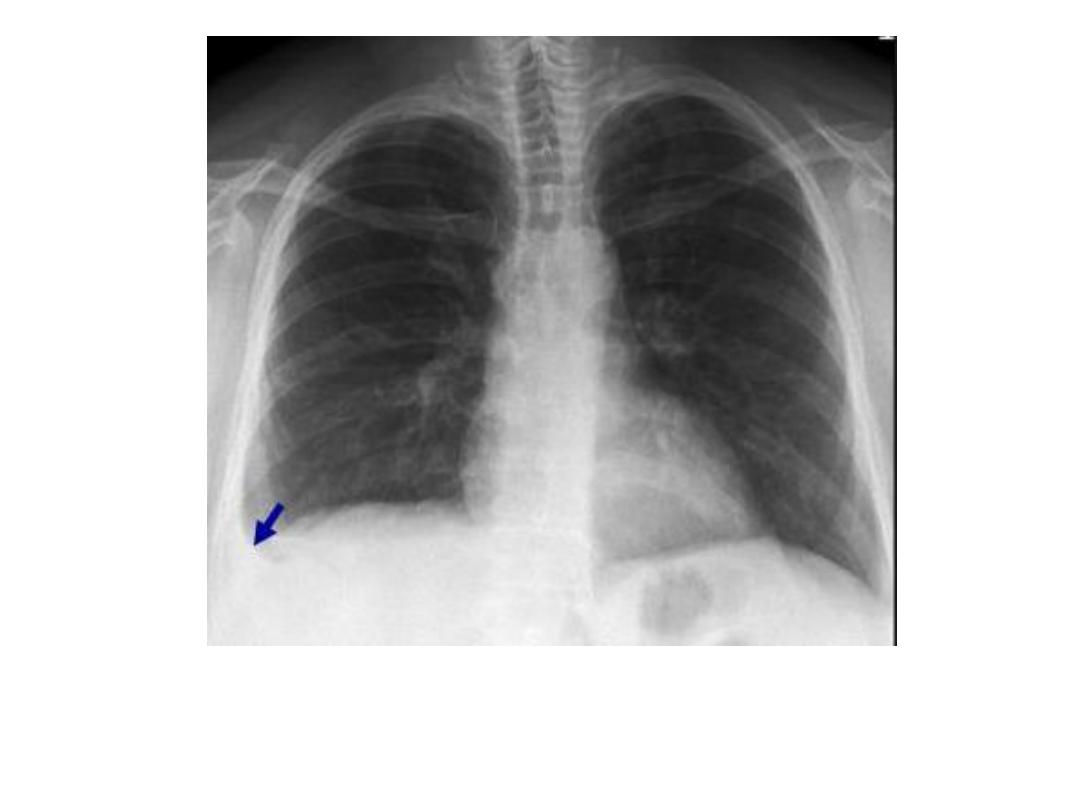
• Free pl. effusion: 1- entirely homogenous. 2- fluid collects in most dependant part of
pl. cavity and always fill in costophrenic angle(CPA). 3- us. Surrounds the lung and
higher laterally than medially. 4- large effusion may cause med. Shift to opposite side. 5-
very large effusion run over the top of the lung. 6- the smooth edge between the lung
and the fluid can be recognized on adeq. Penetrated film.
• S.T. even with large effusion , little or no fluid seen running up on chest wall, is often
known as subpulmonary pleural effusion : the upper border of the fluid is much the same
shape as normal diaphragm, but he peak of pseudodiaphragm is more lateral than
normal.
On ultrasound : it is simple method to determine whether there is pl. effusion or not.
• Pl. fluid can be recognized as transonic area between the lung and diaph. Or between the
chest wall and the lung.
• In empyaema we may be seen multiple echoes in the pl. fluid pus in the fluid.
• U/S is part. Useful in defining presence, size and shape of pl. collection loculated against
chest wall or diaph.
• U/S is convenient method of imaging control for pl. fluid aspiration or drainage.
On CT scan : pl. effusion us. Seen as homogenous fluid density between chest wall and
lung.
• It is part. Useful for showing loculated pl. effusion.
•
Fluid due to recent hemorrhage it will show high density blood.
•
Free pl. effusion move to dependant portion of the chest,
•
To differentiate ascities fro pl, effusion: pl. fluid collects outside diaph. Dome and can be seen post.
To portion of the diaph, that cover the bare area of the liver .
•
CT scan can be used to distinguish between lung abscess and empyaema.
•
CT can be used to direct the placement of drainage tubes.
•
Pleural thickening(fibrosis) : fibrotic pl. thickening (scarring) esp. in CPA may follow resolution
of pl. effusion, part. Following pl. infection or hemorrhage, or following asbestos related pl.
effusion .
•
Pl. scarring is nearly always much smaller in volume than original pl. effusion.
•
If can not differentiate pl. effusion from pl. thickening, U/S or CT scan us. Resolve the problem.
•
Localized plaques of pl. thickening along lateral chest wall commonly indicate asbestos exposure,
such plaques may show irregular calc.
•
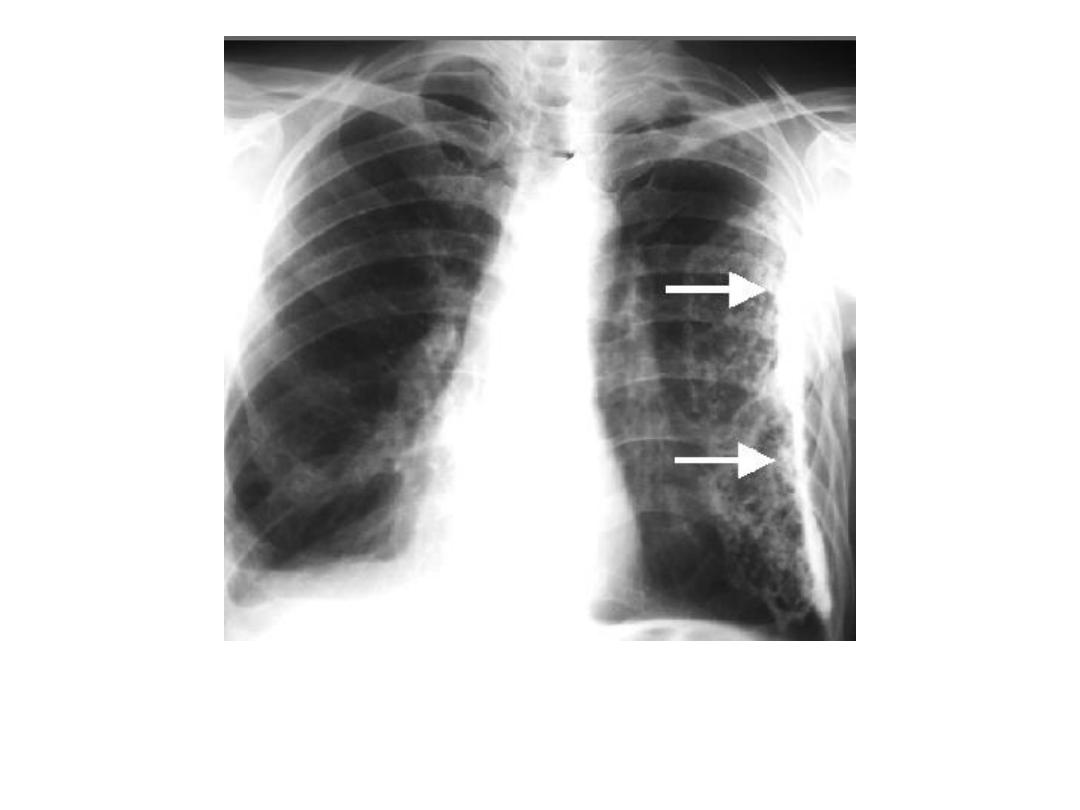
Pleural tumors : metastatic CA are the commonest pl. tu.
•
Primary pl tu. Such as Mesothelioma, are relatively uncommon.
•
Many patients with malignant mesoth. Give a Hx. Of asbestos exposure.
•
Pl. tu. Produce lobulated masses based on pl.
•
Malignant pl. tu., both primary(malignant Mesothelioma) and secondary, freq. cause pl. effusions,
which may obscure the tu. Itself.
•
The commonest feature of metastatic pl. tu. And some malig. Mesoth.: is a pl. effusion with no
visible mass on imaging.
•
Pleural calcification : irregular plaques of calc. may be seen with or without accompanying pl.
thickening.
•
Unilateral: are likely due to old empyaema(us. TB) or old haemothorax.
•
Bilateral: often related to asbestos exposure.
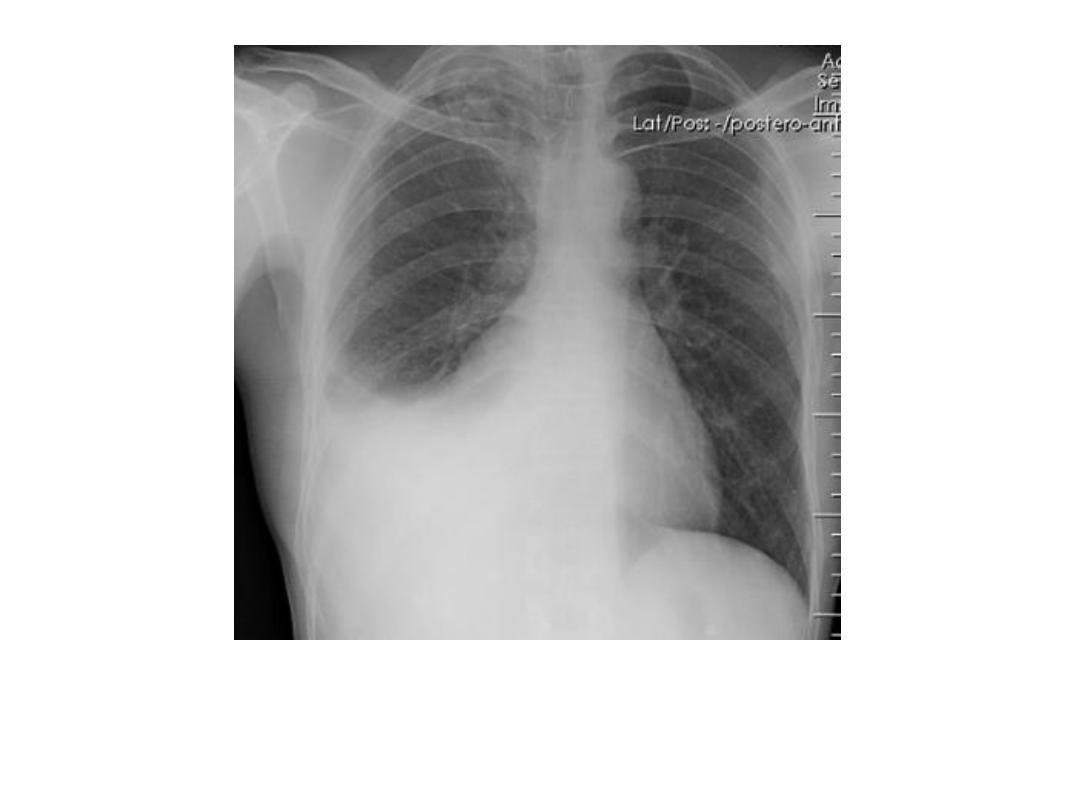
Pleural effusion
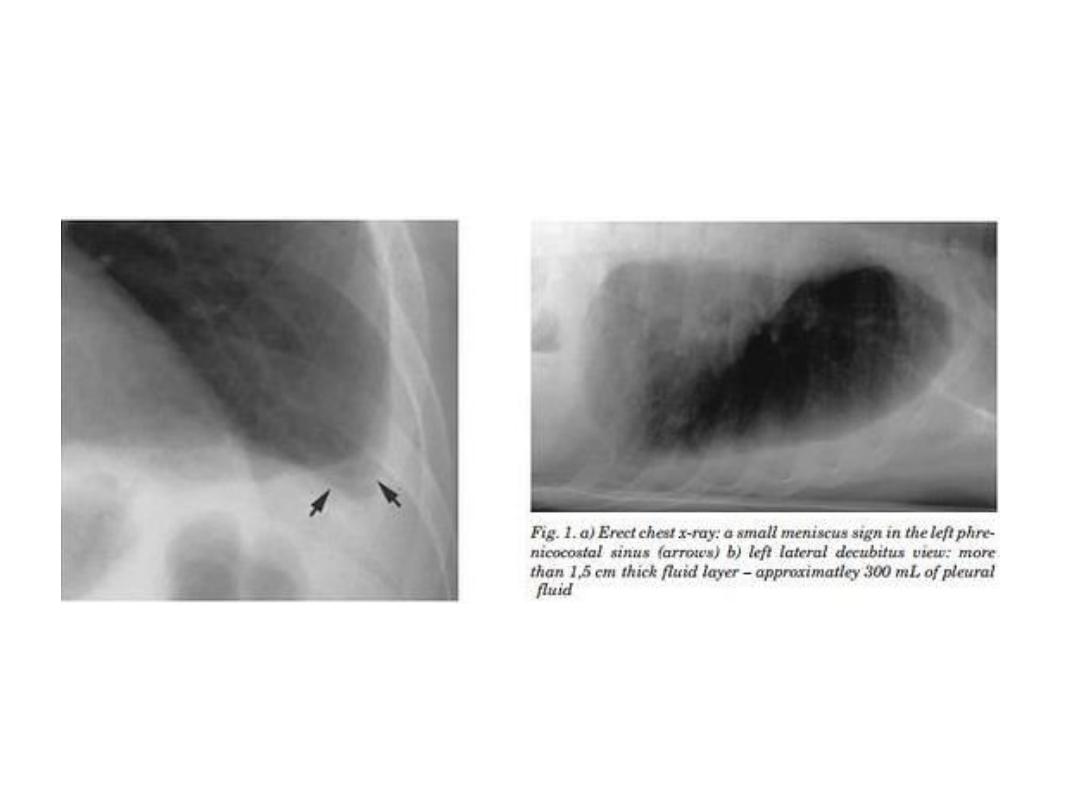
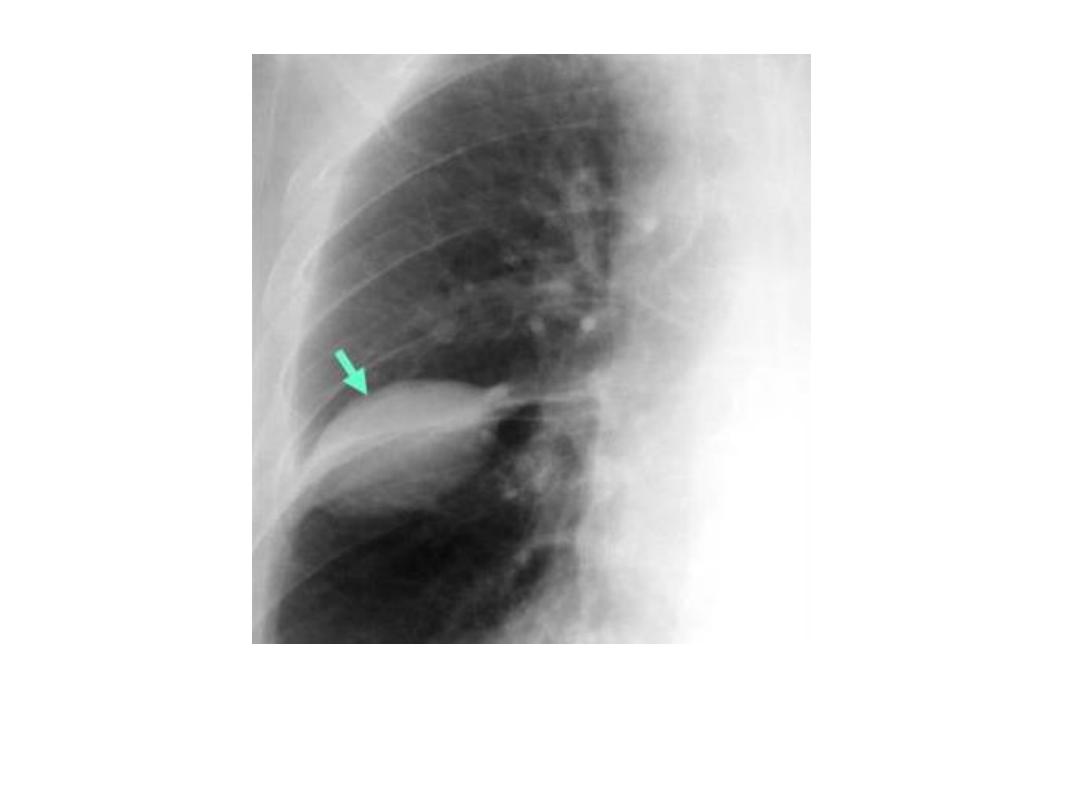
Loculated pl. effusion

Subphrenic abscess and rt. Pl. effusion
Rt. Pulm. Infarct and pl. effusion
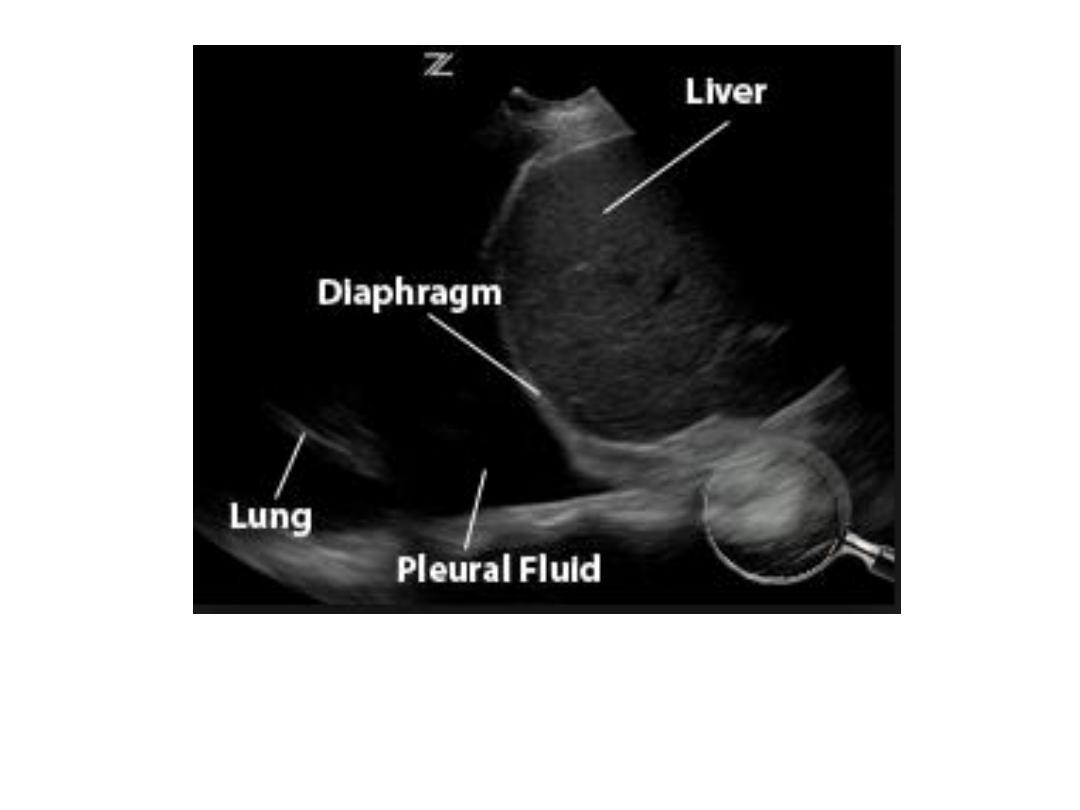
Ultrasound of pl. effusion
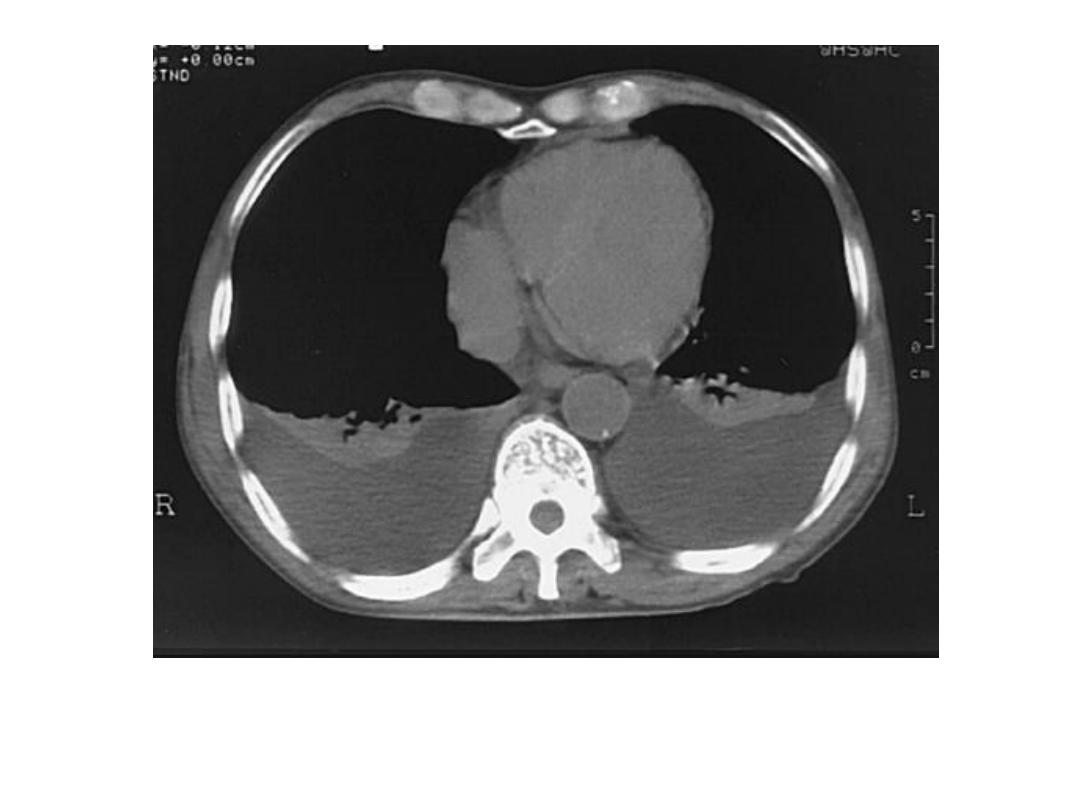
CT pl. effusion

CT of empyaema
Pleural thickening
Pleural calcification

Calcified pleural plaques
Mesothelioma
• Pneumothorax : the majority occur in young people with no obv. Cause, the
patients have small blebs or bullae at periphery of lungs which burst, occasionally is
due to: emphysema, trauma, certain cause of interstial pulm. Dis., pneumocystis
carinii pn., rarely metastasis.
• Radiologically: 1- there is line of pl. due to lung edge being separated from chest
wall, med. Or diaph. By air.
2- absence of vs. shadows outside this line, which is alone insufficient for dx., as may
be few, or no, visible vs. in emph. Bullae.
3- if pneumothorax is very large, the may be appreciable increase in density of
underlying lung.
• S.T. pneumothorax is more obv. On exp. Film.
• When we Dx. Pneumothorax, so next step to decide if it is tension type: see med.
Shift and flattening of inversion of the hemidiaph.
• Most tension pneumothorax is large due to underlying lung collapsed.
• Small pneumothorax can cause serious symptoms if underlying pulm. Reserve is
poor.
• Hydropneumothorax : pl. effusing in pl. cavity , haemopneumothorax: blood in pl.
cavity , &pyopneumothorax: pus in pl. cavity, are in presence of pneumothorax, the
Dx. Feature is air – fluid level.
• Some fluid is present in pl. cavity in most patients with pneumothorax, the amount
us. small.

pneumothorax

Tension pneumothorax

Hydropneumothorax
