
STROKE
DEFENITION
Stroke, or cerebrovascular accident, is defined by rapid onset (usually
over minutes) of a focal neurologic deficit that is attributable to a focal
cerebral vascular cause.
•
Stroke is divided into ischemic and hemorrhagic type.
•
Stroke is the third commonest cause of death in developed countries
after cancer and ischemic heart disease. The incidence of
cerebrovascular diseases increases with age and the number of
strokes is projected to increase as the elderly population grows.
stroke
Clinical classification of
1-Transient ischemic attack (TIA). This describes strokes in which
symptoms and signs resolve within 24 hours (most less than 1 hour).
2-Reversible Ischemic Neurological Deficit (RIND) Patients recover
without significant deficit, usually within a week or two.
3-Progressing stroke (or stroke in evolution). This describes a stroke in
which the focal neurological deficit worsens after the patient first
presents. Such worsening may be due to increasing volume of infarction,
haemorrhage or related oedema.
4-Completed stroke means the focal deficit has become maximal,
persists and is not progressing.
VASCULAR ANATOMY OF BRAIN
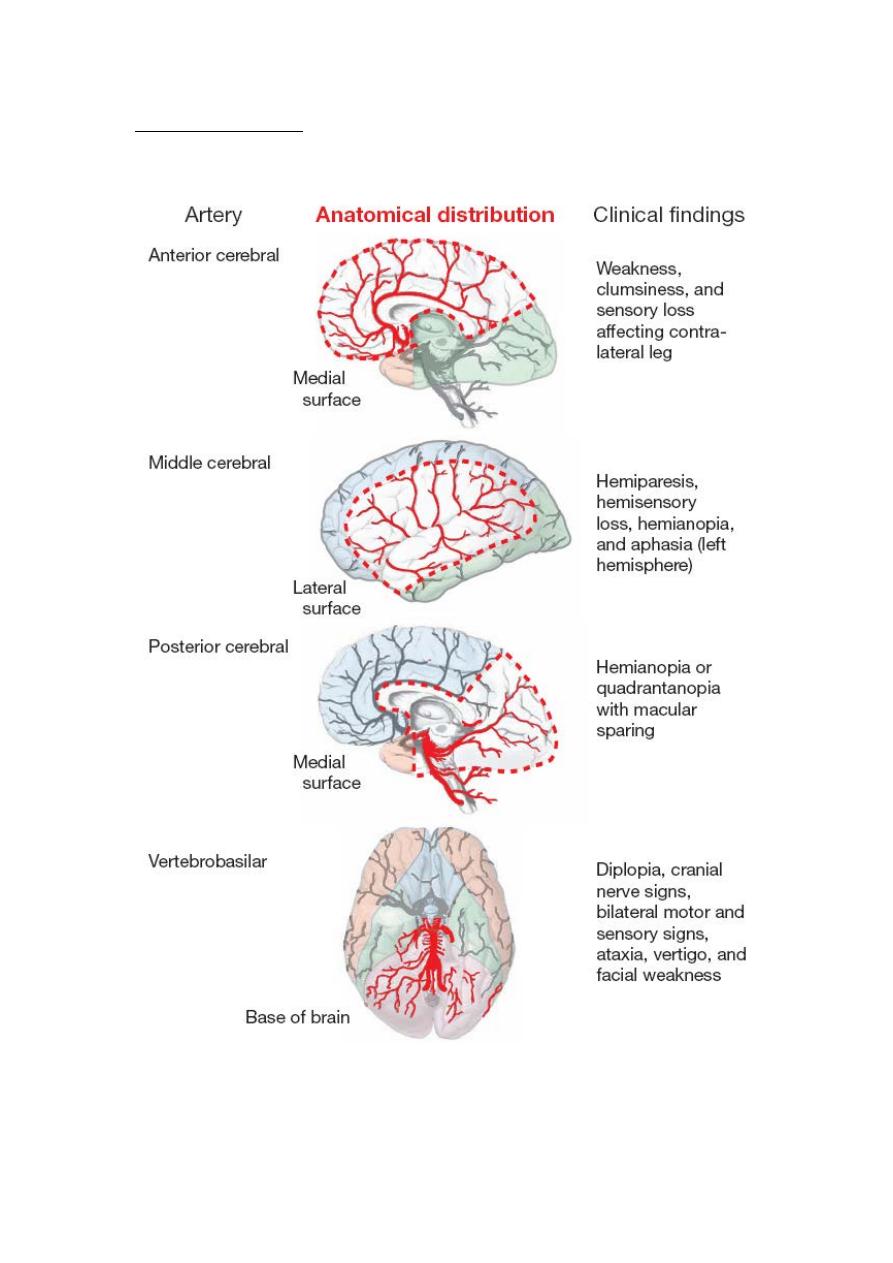
1-anterior circulation (carotid circulation)
Internal carotid artery gives off the anterior cerebral artery (ACA) and
middle cerebral artery (MCA).
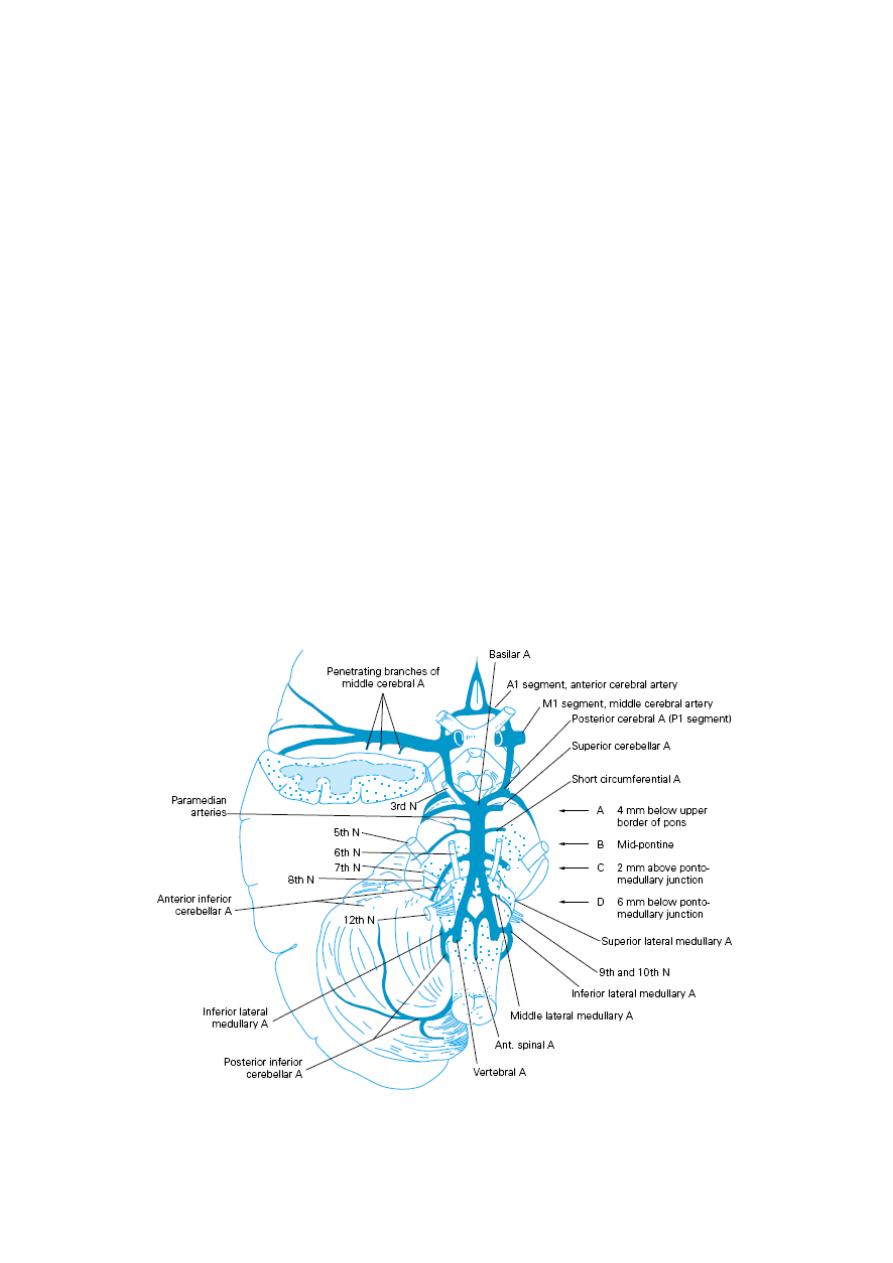
ACA supplies the medial surface of the hemisphere while MCA supplies
the lateral surface. ACAs of both sides are connected via the anterior
communicating artery.
2-posterior circulation (vertebrobasilar circulation)
Posterior circulation is composed of two vertebral arteries; they unite at
the pons to form the basilar artery.
The short basilar artery divides into two posterior cerebral arteries
(PCA).
At the base of the brain
circle of Willis is formed by communication of
the anterior and posterior circulations via the posterior communicating
arteries, and communication of right and left circulations via the anterior
communicating artery.
Pathophysiology of ischemic stroke
•
Cerebral infarction is mostly due to thromboembolic disease
secondary to atherosclerosis in the major extracranial arteries
(carotid artery and aortic arch). About 20% of infarctions are due
to embolism from the heart (cardioembolic), and a further 20%
are due to intrinsic disease of small perforating vessels
(lenticulostriate arteries), producing so-called 'lacunar'
infarctions.
•
Acute occlusion of an intracranial vessel causes reduction in blood
flow to the brain region it supplies. The magnitude of flow
reduction is a function of collateral blood flow and this depends
on the site of occlusion. A fall in cerebral blood flow to zero
causes death of brain tissue within 4–10 min. (called infarction). If
blood flow is restored prior to a significant amount of cell death,
the patient may experience only transient symptoms, i.e., a TIA.
Tissue surrounding the core region of infarction is ischemic but
reversibly dysfunctional and is referred to as the ischemic
penumbra. The ischemic penumbras will eventually infarct if no
change in flow occurs.
•
Higher brain temperature, as might occur in fever, and higher
blood sugar have both been associated with a greater volume of
infarction for a given reduction in cerebral blood flow.
STROKE RISK FACTORS
modifiable
-
Non
•
Age ( more than 60)
•
Gender (male > female, except in the very young and very old)
•
Race (Afro-Caribbean > Asian > European)
•
Heredity
•
Previous vascular event, e.g. myocardial infarction, stroke or
peripheral embolism

Modifiable
•
High blood pressure
•
Heart disease (atrial fibrillation, heart failure, endocarditis)
•
Diabetes mellitus
•
Hyperlipidaemia
•
Smoking
•
Excess alcohol consumption
•
Polycythaemia
•
Oral contraceptives
•
Social deprivation
•
History of TIA or stroke
CLINICAL FEATURES
A- TIA
Clinical features of principal forms of TIA are:
1-Amaurosis fugax: is a sudden transient loss of vision in one eye for
more than a few seconds, described as a rapid fading of vision like a
curtain descending. It usually occurs from an embolus that becomes
stuck within a retinal arteriole.Then the embolus breaks up or passes,
flow is restored and vision returns quickly to normal. A TIA causing an
episode of amaurosis fugax is often the first clinical evidence of internal
carotid artery stenosis.
2-hemiparesis, hemianasthesia, aphasia
3-vertigo, diplopia.
completed stroke
-
B

PICA )
–
rior Cerebellar Artery
syndrome (Posterior Infe
Wallenberg
Due to lateral medullary ischemia resulting in weakness of ipsilateral
5th, 9th, 10th, Ipsilateral Horner's syndrome, ipsilateral cerebellar signs,
contra lateral spinothalamic sensory loss, vertigo and vomiting.
INVESTIGATION
1-imaging: Brain imaging with either CT or MRI should be performed in
all patients with stroke to confirm the diagnosis and exclude
intracerebral hemorrhage.
CT is the most practical and widely available method of imaging the
brain. It will demonstrate intracerebral haemorrhage within minutes of
stroke onset. However,
CT changes in cerebral infarction may be
completely absent or subtle and may take 24-48 hours to appear.
•
MRI diffusion weighted imaging (DWI) can detect ischaemia earlier
than CT.
•
MRI is more sensitive than CT in detecting strokes affecting the brain
stem and cerebellum.
2-Imaging blood vessels
Many ischemic strokes are caused by atherosclerotic thromboembolic
disease of the major extracranial vessels.
•
Carotid Doppler to show the degree of carotid stenosis.
•
MR angiography (MRA) or CT angiography.
3-Detecting a cardiac source of embolism:
Approximately 20% of ischemic strokes are thought to be due to
embolism from the heart. The most common causes of cardiac embolism
are atrial fibrillation, prosthetic heart valves, other valvular
abnormalities and recent myocardial infarction.
These can often be identified by clinical examination, ECG and
transthoracic or transoesophageal echocardiogram.
4-othe investigations: like lipid profile, CBP&ESR, FBS, B.urea, and
S.creatinine.
MANAGEMENT OF PATIENTS WITH STROKE
The aim of management
•
minimizing the volume of brain that is irreversibly damaged (saving
penumbra)
•
preventing complications
•
reducing the patient's disability and handicap through rehabilitation
•
reducing the risk of recurrent episodes
ACUTE STROKE MANAGEMENT
•
non-specific
1-ABC: maintain adequate airway to prevent aspiration, O
2
saturation
should be ≥ 95%, IV fluid for adequate hydration (isotonic saline or
glucose saline).
2-Nutrition: Consider nutritional supplements; start feeding via a
nasogastric tube in persistent dysphagia.
3-Blood pressure: Unless there is heart failure or renal failure, evidence
of hypertensive encephalopathy or aortic dissection, do not lower the
blood pressure in the first week since it will often return towards the
patient's normal level within the first few days.
4- Blood glucose: Hyperglycemia (≥200mg/dl) may increase infarct
volume, therefore use insulin but monitor closely to avoid hypoglycemia.
5-temperature: fever may increase infarct volume, so treat any cause
and give antipyretics early.
•
Specific treatment
1- Thrombolysis treatment:
Intravenous thrombolysis with recombinant tissue plasminogen
activator (rt-PA) – alteplase increases the risk of haemorrhagic
transformation of the cerebral infarct with potentially fatal results.
However, if given within 3-4.5 hours of symptom onset to highly
selected patients
, may improve overall outcome
2- After an acute persistent stroke, aspirin 300mg started within 48
hours of onset improves long-term outcome.It may be given by
rectal suppository or by nasogastric tube in dysphagic patients.
3- Heparin increases in the risk of both intracranial and extracranial
haemorrhage and does not result in better long-term outcomes.
Therefore it should not be used in the routine management of
acute stroke.
SECONDARY PREVENTION OF ISCHAEMIC STROKE
The average risk of a further stroke is 5-10% within the first week of a
stroke or TIA, perhaps 15% in the first year and 5% per year thereafter.
•
Patients with ischaemic events should be put on long-term
antiplatelet drugs (either aspirin 75-300 mg daily or clopidogrel 75
mg daily or a combination of aspirin and dipyridamole modified
release 12-hourly), and statins to lower cholesterol.
•
The risk of recurrence after both ischaemic and haemorrhagic strokes
can be reduced by blood pressure reduction.
•
For patients with cardioembolic cause the risk can be reduced by
about 60% by oral anticoagulation (warfarin) to achieve an INR of 2-3.
•
Carotid endarterectomy, angioplasty and stenting in patients with a
carotid territory ischemic stroke or TIA and 70-99% stenosis of the
carotid artery on the side of the brain lesion. Antiplatelet drugs are
used in carotid stenosis less than 70%.
COMPLICATIONS OF ACUTE STROKE
Complication
Prevention
Treatment
Chest infection
Nurse semi-erect
Antibiotics
Avoid aspiration
Physiotherapy
Epileptic seizures
Maintain cerebral
oxygenation
Anticonvulsants
Avoid metabolic disturbance
Deep venous
thrombosis/pulmonary
embolism
Maintain hydration
Early mobilization
Anti-embolism stockings
Heparin (for high-risk
patients only)
Anticoagulation (exclude
haemorrhagic stroke first)
Painful shoulder
Avoid traction injury
Physiotherapy
Shoulder/arm supports
Local corticosteroid
injections
Physiotherapy
Pressure sores
Frequent turning
Nursing care
Monitor pressure areas
Pressure-relieving mattress
Avoid urinary damage to skin
Urinary infection
Avoid catheterization if
possible
Antibiotics
Use penile sheath
Constipation
Appropriate laxatives and
diet
Depression and anxiety
Maintain positive attitude
and provide information
Antidepressants
SPECIFIC TYPES OF STROKE
LACUNAR STROKE
20% of cerebral infarctions are due to occlusion of small perforating
vessels (lenticulostriate arteries), producing so-called 'lacunar'
infarctions. Each of these small vessels can occlude either by
atherothrombotic disease at its origin or by the development of
lipohyalinotic thickening causing small infarcts that are referred to as
lacunes. Hypertension and age are the principal risk factors.
Lacunar syndromes are the followings:
1-Pure motor hemiparesis
2-pure sensory stroke (hemianasthesia)
3-ataxic hemiparesis
4-dysarthria and a clumsy hand or arm
•
Secondary prevention of lacunar stroke involves risk factor
modification, specifically reduction in blood pressure and antiplatelet
drugs.
