DISORDERS OF THE SPINE AND SPINAL CORD
INTRODUCTION
Anatomy:
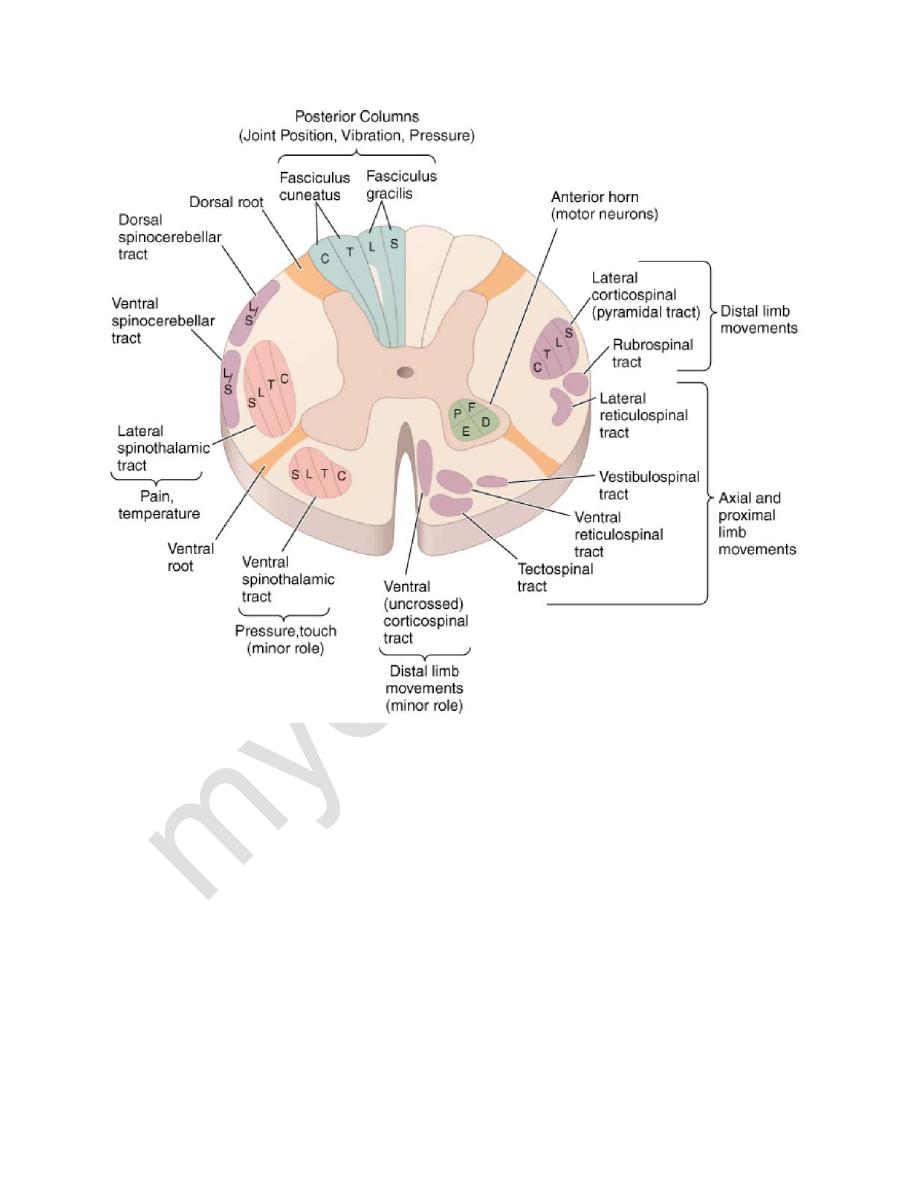
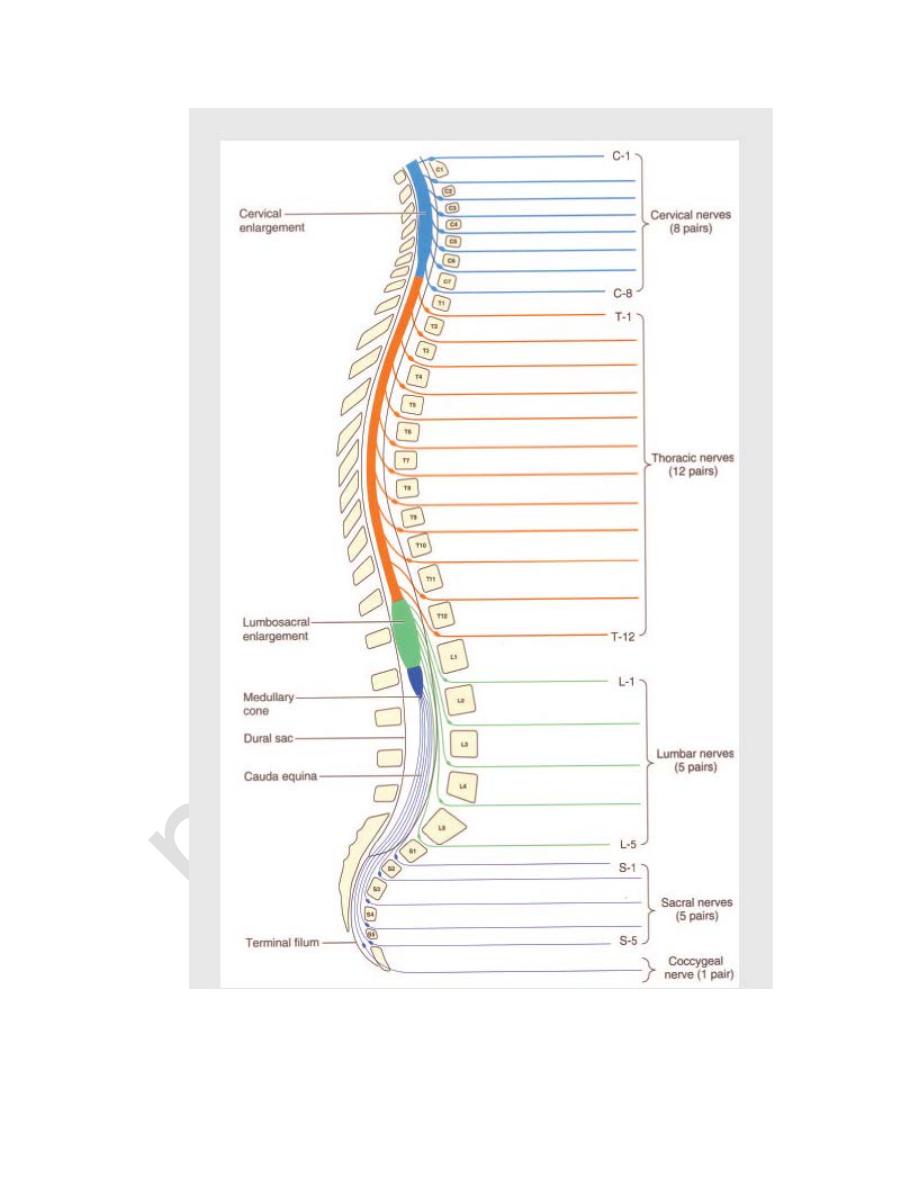
• Spinal cord is the component of the central nervous system that connects the
brain to the peripheral nerves.
• It contains:
a) in the white matter, fiber pathways leading from the brain to the
periphery and vice versa
b) In the gray matter, an intrinsic neuronal system; motor, somatosensory,
autonomic and interneurons.
• Anterior 2/3 of cord is supplied by anterior cerebral artery while posterior
1/3 is supplied by posterior cerebral artery.
Main Spinal Cord Syndromes:
1. Spinal cord transection syndrome: is the pattern of neurological deficits
resulting from damage of the entire cross-section of the spinal cord at some
level.
• It is traumatic, ischemic, infectious or inflammatory (transverse myelitis).
• The clinical features of the spinal cord transection syndrome are:
I.
there is a sensory level below which all modalities of sensation are
impaired
II.
Bilateral pyramidal tract dysfunction: spastic paraplegia, or, with cervical
lesions, spastic quadriplegia (immediately there may be usually flaccid
weakness “spinal shock”, which subsequently becomes spastic).
1
III.
sphincter dysfunction
2. Spinal cord hemisection syndrome
(Brown−Séquard syndrome)
• Caused by a compressing tumor or demyelination.
• Clinical features include:
I.
Ipsilateral paresis
II.
Ipsilateral loss of proprioception and vibration sense
III.
Contralateral loss of pain and temperature sensation
3. Central cord syndrome
• Is the classic presentation of syringomyelia but can also be due to an
intramedullary hemorrhage or tumor.
• In the cervical cord, the central cord syndrome produces arm weakness
out of proportion to leg weakness
• "Dissociated" sensory loss, signifying a loss of pain and temperature
sense in a cape distribution over the shoulders, lower neck, and upper
trunk in contrast to preservation of light touch, joint position, and
vibration sense in these regions.
4. Anterior Spinal Artery Syndrome
• Anterior spinal artery supplies the anterior two third of the cord.
• Infarction of the cord is generally the result of occlusion or diminished flow
in this artery.
• All spinal cord functions—motor, sensory (pain &temperature), and
autonomic—are lost below the level of the lesion, with the striking
exception of retained vibration and position
sensation (posterior column).
2
5. Cauda equina syndrome
• Results from compression of the nerve roots crossing through the
spinal canal below the conus medullaris, i. e., below the L1/2 level.
• It causes flaccid weakness and areflexia of the lower limb usually
asymmetrical.
• Impaired urination, defecation, and sexual function
• Impairment of all sensory modalities in multiple lumbar and/or sacral
dermatomes, usually most pronounced in the “saddle” area.
• Patients usually have lower backache.
CAUSES OF SPINAL CORD DISORDERS (MYELOPATHIES)
1. Compressive (Herniated disc, neoplasm)
2. Vascular( AV malformation)
3. Inflammatory (multiple sclerosis, vasculitis)
4. Infectious (herpes)
5. Developmental (syringomyelia)
6. Metabolic (vitamin B12 deficiency)
3
4
5
SPECIFIC DISEASES
CERVICAL SPONDYLOSIS: is an osteoarthritic degenerative change of the
cervical spine.
Cervical spondylotic radiculopathy:
• Compression of a nerve root occurs when a disc prolapses laterally, which
may develop acutely or gradually .
• The patient complains of pain in the neck that may radiate in the distribution
of the affected nerve root. The neck movements may exacerbate pain.
• Paraesthesia and sensory loss may be found in the affected segment and
there may be lower motor neuron signs, including weakness, wasting and
reflex impairment.
• Investigations include
Plain X-rays, including lateral and oblique views
cervical spine MRI may be required.
Electrophysiological studies rarely add to the clinical examination.
• Conservative treatment with analgesics and physiotherapy results in
resolution of symptoms in the great majority of patients, but a few require
surgery in the form of foraminotomy or disc excision.
Cervical spondylotic myelopathy:
• Dorsomedial herniation of a disc and the development of transverse bony
bars or posterior osteophytes may result in pressure on the spinal cord.
• The onset is usually insidious and painless.
6
• Upper motor neuron signs develop in the limbs, with spasticity of the legs
usually appearing before the arms are involved.
• Sensory loss in the upper limbs is common, producing tingling, numbness
and proprioception loss in the hands, with progressive clumsiness.
• The neurological deficit usually progresses gradually and disturbance of
micturition is a very late feature.
• MRI of the cervical spine shows the site of compression.
• Management: Surgical procedures may arrest progression of disability but
may not result in neurological improvement.
LUMBO-SACRAL SPONDYLOSIS
Lumbar disc herniation
• Acute lumbar disc herniation is often precipitated by trauma, usually by
lifting heavy weights while the spine is flexed.
• The onset may be sudden or gradual.
• Repeated episodes of low back pain may precede sciatica by months or
years.
• Constant aching pain is felt in the lumbar region and may radiate to the
buttock, thigh, calf and foot.
• Pain is exacerbated by coughing or straining but may be relieved by lying
flat.
• Root pressure is suggested by limitation of flexion of the hip on the affected
side if the straight leg is raised (Lasègue's sign).
• The roots most frequently affected are S1, L5 and L4.
• MRI is the investigation of choice.
7
• Management :
Some 90% of patients with sciatica recover with conservative
treatment with analgesia and early mobilisation.
Avoid physical manoeuvres likely to strain the lumbar spine.
Surgery may have to be considered if there is no response to
conservative treatment or if progressive neurological deficits
develop, especially sphincter dysfunction.
Lumbar canal stenosis
• This is due to a congenital or acquired narrowing of the lumbar spinal canal.
• Patients, who are usually elderly, develop exercise-induced weakness and
paraesthesia in the legs (neurogenic claudication), but are quickly relieved
by a short period of rest.
• Weakness or sensory loss may only be apparent if the patient is examined
immediately after exercise.
• CT or MRI will demonstrate narrowing of the lumbar canal.
• Extensive lumbar laminectomy often results in complete relief of symptoms
and recovery of normal exercise tolerance.
SYRINGOMYELIA:
• Syringomyelia is a developmental cavitary expansion of the cervical cord
that is prone to enlarge and produce progressive myelopathy.
• Symptoms begin insidiously in adolescence or early adulthood.
8
• The classic presentation is a central cord syndrome consisting of a
dissociated sensory loss and areflexic weakness in the upper limbs.
• Horner's syndrome is also present.
• Extension of the syrinx into the medulla (syringobulbia), causes palatal or
vocal cord paralysis, dysarthria, horizontal or vertical nystagmus, episodic
dizziness, and tongue weakness.
SUBACUTE COMBINED DEGENERATION (VITAMIN B12
DEFECIENCY):
• It presents with subacute paresthesias in the hands and feet, loss of
vibration and position sensation, and a progressive spastic weakness.
• Loss of reflexes due to an associated peripheral neuropathy in a patient,
who also has Babinski signs, is an important diagnostic clue.
• Optic atrophy and irritability or other mental changes may be prominent
in advanced cases.
• Signs are generally symmetric and reflect predominant involvement of
the posterior and lateral tracts, including Romberg's sign.
• The diagnosis is confirmed by the finding of macrocytic red blood cells,
a low serum B12 concentration, elevated serum levels of homocysteine
and methylmalonic acid, and in uncertain cases a positive Schilling test.
• Treatment is by replacement therapy.
9
